Abstract
Natural orifice translumenal endoscopic surgery (NOTES) has moved from the realm of laboratory experiments to the realm of human clinical trials. This paper reviews the spectrum of NOTES procedures currently available in the United States and worldwide. It also discusses the limitations and avenues for further development of these procedures, particularly those involving the transgastric approach.
Keywords: Natural orifice surgery, translumenal endoscopy, transvaginal, transgastric, transrectal
What Procedures Are Currently Being Performed and Where?
Natural orifice translumenal endoscopic surgery (NOTES) has clearly moved from an experimental laboratory technique to a technique that can be performed in a human environment. As of February 2012, more than 30 clinical trials involving NOTES were listed on ClinicalTrials.gov, and many of these trials had ongoing recruitment.1 A number of trials have been completed, and results should become available within the next year.1 With the support of the Society of American Gastrointestinal and Endoscopic Surgeons and the American Society for Gastrointestinal Endoscopy, the Natural Orifice Surgery Consortium for Assessment and Research (NOSCAR) is conducting a randomized multicenter trial comparing NOTES cholecystectomy (via the transgastric or transvaginal approach) with 4-port laparoscopic cholecystectomy; this trial is expected to be completed in Fall 2012.2 Other trials are investigating NOTES for appendectomy, hernia repair, cholecystectomy, sleeve gastrectomy, post—bariatric surgery gastric pouch reduction, pancreatic cancer staging, percutaneous endoscopic gastrostomy (PEG) rescue, and omental patch closure of perforated ulcers.3–9
In the United States, 5 medical centers are participating in the aforementioned NOSCAR trial. The highest volume of activity for this trial is on the East and West Coasts, with additional activity in Chicago, Illinois.2 The largest experience with transgastric peritoneoscopy in the United States has been in Ohio.9 Investigation of PEG rescue and assessment of NOTES closure for colonic diseases have also been completed in Ohio.1 A trial of transrectal resection of rectal cancer is currently being conducted in Massachusetts.10,11 Recruitment is currently open for studies assessing transvaginal sleeve gastrectomy in Southern California and transvaginal appendectomy in Connecticut.1,3 A trial examining translumenal omental closure of gastric and duodenal perforations is nearing completion in Minnesota.1
The international community is also very active, with the IMTN Registry reporting data from 362 patients in 2010.5 Surgeons and endoscopists from Brazil, Peru, Argentina, India, and other countries have compiled their results in this international registry. The highest volume of NOTES cholecystectomy (via transvaginal access) is being performed in Germany; here, the NOTES approach has clearly moved from an investigational procedure to a routine clinical option.6
The majority of reported procedures and trials utilize transvaginal access, with transgastric and transcolonic approaches being reported less frequently.
Why Is the Transvaginal Approach Being Used More Frequently Than the Transgastric Approach?
At the beginning of the last decade, NOTES rapidly evolved from a concept of advanced transgastric endos-copy to an experimental technique that garnered significant media attention.
The group of therapeutic endoscopists who developed the concept of NOTES had significant experience with transgastric drainage of pancreatic pseudocysts and debridement of pancreatic necrosis, most of which are found in a retrogastric position. For these advanced endoscopists, creating a gastrostomy using a combination of needle-knife puncture and wire-guided balloon dilation, followed by the placement of stents, was a matter of routine clinical practice. Following the balloon dilation, passage of the endoscope outside the gastric lumen was the logical next step.
The medical community took notice of this development when the gastrostomy was made at the anterior gastric wall, advancing the endoscope into the peritoneal cavity and, thus, into the realm of intra-abdominal surgical procedures.12,13 The anterior position of the gastrostomy brought both new opportunities and challenges.
Opportunities for the Transgastric Approach
Access to the abdominal cavity was now possible without making an abdominal wall incision. The advantages of avoiding the abdominal wall yet still being able to obtain access to the peritoneum were evident: There was no parietal pain, superficial wound infection, or hernia formation. The PEG rescue procedure reported by Marks and colleagues demonstrated that NOTES could be performed under conscious sedation in the monitored care setting, without the need for general anesthesia.7 Immediately, the most frequently performed abdominal operations (cholecystectomy, appendectomy, and hernia repair) were translated into the NOTES environment, first in the laboratory setting and then in the human setting.8,14–16
At the experimental stage, expectations were high that NOTES would facilitate the next revolution in minimally invasive approaches and possibly replace laparoscopy.13 However, attempting to replace the most frequently performed and successful laparoscopic procedures by developing the NOTES approach increased the number of challenges. These laparoscopic procedures were associated with a low risk of morbidity and a very low risk of mortality, which provided a high level of patient satisfaction.
Challenges of the Transgastric Approach
One of the major challenges of the NOTES transgastric approach was the safety of the gastrostomy closure.13 The posterior gastrostomy usually entered into a confined space that was often already sealed by a prior inflammatory process. Because the posterior gastrostomy decompressed the retrogastric fluid collection, communication with the gastric lumen was frequently a benefit rather than a problem. In contrast, the anterior gastrostomy enters a large space where ongoing communication with the gastric lumen is a problem. The experience with gastric perforations or anastomotic leaks—such as those in a gastric bypass operation with possible resultant mortality—makes the safety of the gastrostomy closure a pivotal procedural element. Intense investigation ensued surrounding the safety of different gastrostomy closure methods and devices. Although experimental data from porcine models supported the safety of the NOTES gastrostomy, anecdotal experience of peritonitis from a gastrostomy leak following transgastric cholecystectomy gave investigators pause.17–21
Another challenge involved the geometry of the abdomen, which made obtaining access to the gallbladder from the stomach quite difficult. Devices that attempted to overcome this spatial challenge proved to be costly for both developers and users. Transvaginal access appeared to provide the perfect solution to these problems for a number of reasons: Closure of the vaginal wall had been performed for more than 100 years, transvaginal access was routine in the gynecologic environment, and this approach would provide a straight route to the upper abdomen.22,23 In addition, rigid instrumentation could be used, which significantly decreased the technical skill level required. Transvaginal access with rigid instrumentation is the NOTES approach currently used in Germany.24
What Is the Current Role of the Transgastric Approach?
Transgastric access remains a viable option for translumenal endoscopy. As discussed before, pancreatic cancer staging and PEG rescue are both excellent opportunities to use transgastric access. At our own institution, we have utilized this route with good success for incision and drainage of pancreatic necrosis in the septic fluid phase, thus avoiding a large debilitating open abdomen for surgical necrosectomy. We used the transgastric approach when a patient with biliary pancreatitis became tachy-cardic, tachypneic, and febrile, with computed tomography findings that suggested infected necrosis with fluid collections. No abdominal compartment syndrome was present, and a laparotomy was not indicated at the time. After the transgastric endoscopic evacuation of malodorous fluid and debris from the lesser sac, the respiratory and hemodynamic situation of the patient improved within 24 hours. Continued treatment of the pancreatic necrosis was enabled by a repeat endoscopy, aided by nasojejunal feeding, nasotransgastric drainage and lavage, and percutaneous drainage and irrigation.
Furthermore, a patient with a chronic gastric perforation following experimental chemotherapy for pseudomyxoma underwent decompression of the mass, with resolution of a small bowel obstruction and hydronephrosis. We have also used the transgastric approach to facilitate perforated peptic ulcer closure in the stomach and duodenum. The existing opening was used to pass the endoscope, irrigate, and place the omental patch. For small perforations, the endoscopic tools served to facilitate fixation of the omental patch, which was technically easier than laparoscopic suturing.
Transesophageal (Submucosal Endoscopic Mucosal Flap) Approach
Transesophageal access using a submucosal tunnel is another well-studied NOTES approach. Animal experiments have revealed the ability to perform mediastino-scopy with lymph node biopsy, a technique that could be helpful in cancer staging and for difficult-to-diag-nose lung disorders.25–28 In the human environment, the submucosal endoscopic mucosal flap technique is successfully being used for the peroral endoscopic myotomy (POEM) procedure.29 To our knowledge, NOTES mediastinoscopy with lymph node biopsy or lymphadenectomy in humans has not yet been performed. Again, the concern regarding this procedure involves the possibility of developing a leak at the offset mediastinal entry site and fistula at a point of injury to the mucosal flap from inadvertent coagulation injury during the tunneling process.
Limitations to the Growth and Adoption of Natural Orifice Translumenal Endoscopic Surgery
As discussed above, the new techniques and technologies surrounding NOTES initially garnered high expectations and generated much media attention. Funding sources were made available for research, and industry partners were engaged in the development process but were careful not to cannibalize the laparoscopy market. The scientific community realized the need for additional tools and platforms, specifically those involving triangulation and retraction in the operative field. Energy, cutting, suturing, and stapling devices that were safe and flexible were also needed to drive the field forward. Although some of these needs were met, others did not materialize or were removed from the market.30–32 Mini-robotic concepts were introduced, as were robotically steered endoscopes, but neither of these advances are currently available on the market.33–35 The US Food and Drug Administration (FDA) played an active role in evaluating tools and procedures and weighing in with opinions. Parallel to the need for additional instrument development, the economic environment in the United States deteriorated and entered into a recession. This change was accompanied by a pullback of capital, and many start-up companies struggled, including companies dedicated to instrumentation for the facilitation of the next-generation endoscopic tool set, which significantly slowed the further development of NOTES.
In addition, due to the advanced endoscopic and spatial skills required for performing many of the NOTES procedures, the field of practitioners who could easily adopt the new techniques and technology did not appear to be very large. As an alternative approach to the no-scar concept, single-incision (single-port) laparoscopy instead gained traction. The same companies involved in NOTES development swiftly provided new instrumentation for this approach. The market for single-port laparoscopy is projected to encompass 25% of all laparoscopy procedures by 2014, with many more surgeons able to perform this approach than NOTES.
Somewhat surprisingly to the NOTES community, patients’ opinions regarding the NOTES approach also varied. Early surveys among young healthcare workers and students had suggested a high rate of acceptance of NOTES procedures, including those involving transvaginal access.36–39 Surgeons themselves were more hesitant to undergo the new procedures, although they were interested in performing them.40 More recent surveys from Switzerland, Australia, and the United States have revealed that women may be more interested in undergoing transvaginal gynecologic operations than general surgical operations.41,42 Overwhelming patient requests for new procedures—as seen with laparoscopic cholecystectomy in the early 1990s—has not been the driving force for further development of NOTES technology.
What Procedures Can Endoscopists Start Performing Immediately with Minimal Training?
One procedure that endoscopists can start performing immediately is PEG rescue. Using a NOTES technique, Marks and colleagues treated a patient with a dislodged PEG tube that had been recently placed.7 A Gastrografin study revealed that the tube was in the peritoneal cavity. The technique involved passing the endoscope through the existing gastrostomy site, inspecting and suctioning the peritoneal cavity, replacing a wire through the tube via the peritoneal cavity back in the gastric lumen, and repositioning the PEG tube. The technical skill involved was not significantly different from that needed to place the PEG tube in the first place. It is important to utilize carbon dioxide insufflation if pneumoperitoneum is expected and to observe the abdominal pressure closely. This procedure was performed at the patient’s bedside under conscious sedation.7 Alternatively, the patient would have required a general anesthetic agent and a laparoscopy or laparotomy to reposition the tube.
Additional avenues currently available are judiciously entering the peritoneal (or thoracic) cavity to interrogate selected fistulae or anastomotic leaks, possible irrigation, and closure by stenting, clipping, or suturing. The same can be done for iatrogenic perforations following endoscopic procedures. Transgastric lavage and drainage of pancreatic necrosis in a fluid phase with sepsis can have a dramatic benefit. The safety of performing a transgastric staging peritoneoscopy prior to a pancreaticoduodenectomy has also been extensively demonstrated.9
Of note, all of the staging peritoneoscopies have been performed in the operating room with the intention of performing a gastric anastomosis at the endoscopic gastrostomy site, thus avoiding endoscopic closure. Introduction of the submucosal endoscopic mucosal flap technique for safe offset access to the peritoneum may provide an expanded margin of safety and a larger operator pool.
What Procedures Can Minimally Invasive Surgeons Perform That Are New and Meet an Unmet Need?
Many minimally invasive surgeons also perform endo-scopy and PEG placement. They can immediately start using the technique outlined above, facilitated by the familiar environment of the peritoneal cavity, albeit with a different visuospatial orientation.
As with PEG rescue, a perforated ulcer has a preexisting gastric or duodenal hole. Perforated peptic ulcers continue to have a high mortality rate (15% at 30 days and 30% at 1 year).43 In addition to advanced age and preexisting disease, complications resulting from therapeutic interventions contribute to this high mortality rate.44 If suturing skills for laparoscopic closure are not available, using the endoscope as an adjunct to facilitate minimally invasive closure of the ulcer may be beneficial to the patient.43
Options to approximate and traverse esophageal atresias are actively being investigated in children. Once again, the endoluminal route may provide a less invasive approach, potentially resulting in faster recovery and better progress for these often ill children.45 Magnetic tools may be used to conveniently approximate tissues and facilitate anastomosis in this setting.
For colorectal procedures, visualization of the pelvic anatomy from the anal route is excellent compared to laparoscopic or open procedures. Laparoscopy for rectal resection is difficult and not widely available. Transanal rectal procedures are being investigated. Another option is using the transvaginal approach to reach the sigmoid and rectum; procedures have been performed using both of these routes.46,47 Combined procedures that involve vaginal hysterectomy and colectomy (eg, for treatment of Lynch syndrome) have been successfully performed at our institution.48
Expanding the Opportunities for Transvaginal Surgery
Transvaginal specimen extraction has been performed for large organs, such as the spleen, kidneys, and gallbladder with very large stones.49,50 Although many spleens can be morcellated to facilitate removal, abdominal incisions for kidney removal are associated with a risk of wound complications and hernia formation. The transvaginal route provides an alternative approach and has been successfully used, including for altruistic kidney donation.
Transvaginal tubal ligation appears to be of interest to patients; however, use of novel transuterine intratubal instrumentation, which eliminates the need for transgression of the vaginal wall, is an attractive alternative.
Next-Generation Endoscopes
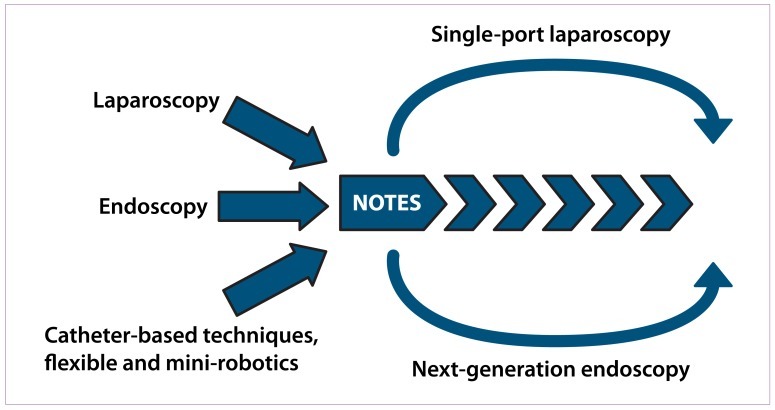
The evolution of NOTES and novel endolumenal techniques will be contingent on the development of the next-generation endoscope. Opportunities for advanced imaging technology, combined with multifunctional tools enabling retraction and triangulation within ergonomi-cally engineered and precise systems, will advance both intralumenal and translumenal endoscopic procedures (Figure 1). The surgical concept of “the eagle,” with its triangulation of eyes between 2 functional tools (eg, hands, laparoscopic tools, and robotic tools), has been juxtaposed with the endoscopic concept of “the snake,” with its in-line optics and tools and limited side trajectory. Based on a number of endoscopic prototypes—such as the Anubis scope (Storz), the EndoSamurai and R-scope (Olympus), the Direct Drive system (Boston Scientific), and the TransPort (USGI Medical)—the endoscope of the future may have octopus-like features. This configuration would combine the endoscopic ability to flexibly enter small spaces with the option of triangulation, again on a flexible basis. The most recent FDA-approved subunit of the da Vinci surgical robot is being used for single-port access, a first attempt at entering through a small space, followed by triangulation. Flexibility has not yet been achieved. A conceptual robot (Arachness) developed by the Imperial College of England Research Unit is small and modular and has the ability to assemble after entering a small space, all while targeting a lower consumer price than currently available.51
Figure 1.
Contributions, interactions, and possible future developments in interventional techniques.
NOTES=natural orifice translumenal endoscopic surgery.
Conclusion
A number of surgical interventions—such as those involving perforated ulcer disease, pancreatic necrosectomy, and esophageal atresia—continue to carry high morbidity and mortality rates, both in the short and long terms. Because of its avoidance of large abdominal or chest wall incisions, NOTES may offer a significant benefit in select situations. Competition with low-morbidity, low-mortality outpatient procedures may be ill-advised. The role of NOTES may not be realized in high-volume, high-revenue-generating procedures but in niches where significant patient benefit can still be realized. This role of NOTES will likely evolve over time.
References
- 1. Search: natural orifice surgery. ClinicalTrials.gov http://clinicaltrials.gov/ct2/results?term=Natural+orifice+surgery February 13, 2012
- 2.Articles/white papers/resources. NOSCAR. Natural Orifice Surgery Consortium for Assessment and Research. [February 13, 2012]. http://www.noscar.org/resources/
- 3.Solomon D, Lentz R, Duffy AJ, Bell RL, Roberts KE. Female sexual function after pure transvaginal appendectomy: a cohort study. J Gastrointest Surg. 2012;16:183–186. doi: 10.1007/s11605-011-1706-4. discussion 186-187. [DOI] [PubMed] [Google Scholar]
- 4.Horgan S, Cullen JP, Talamini MA, et al. Natural orifice surgery: initial clinical experience. SurgEndosc. 2009;23:1512–1518. doi: 10.1007/s00464-009-0428-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Zorron R, Palanivelu C, Galvao Neto MP, et al. International multicenter trial on clinical natural orifice surgery—NOTES IMTN study: preliminary results of 362 patients. SurgInnov. 2010;17:142–158. doi: 10.1177/1553350610370968. [DOI] [PubMed] [Google Scholar]
- 6.Lehmann KS, Ritz JP, Wibmer A, et al. The German registry for natural orifice translumenal endoscopic surgery: report of the first 551 patients. Ann Surg. 2010;252:263–270. doi: 10.1097/SLA.0b013e3181e6240f. [DOI] [PubMed] [Google Scholar]
- 7.Marks JM, Ponsky JL, Pearl JP, McGee MF. PEG “rescue”: a practical NOTES technique. Surg Endosc. 2007;21:816–819. doi: 10.1007/s00464-007-9361-2. [DOI] [PubMed] [Google Scholar]
- 8.Fischer LJ, Jacobsen G, Wong B, et al. NOTES laparoscopic-assisted transvaginal sleeve gastrectomy in humans—description of preliminary experience in the United States. Surg ObesRelat Dis. 2009;5:633–636. doi: 10.1016/j.soard.2009.04.015. [DOI] [PubMed] [Google Scholar]
- 9.Nau P, Anderson J, Yuh B, et al. Diagnostic transgastric endoscopic peritone-oscopy: extension of the initial human trial for staging of pancreatic head masses. Surg Endosc. 2010;24:1440–1446. doi: 10.1007/s00464-009-0797-4. [DOI] [PubMed] [Google Scholar]
- 10. Search: sylla and surgery. ClinicalTrials.gov http://clinicaltrials.gov/ct2/results?term=Sylla+AND+surgery February 13, 2012
- 11.Sylla P, Rattner DW, Delgado S, Lacy AM. NOTES transanal rectal cancer resection using transanal endoscopic microsurgery and laparoscopic assistance. Surg Endosc. 2010;24:1205–1210. doi: 10.1007/s00464-010-0965-6. [DOI] [PubMed] [Google Scholar]
- 12.Kalloo AN, Singh VK, Jagannath SB, et al. Flexible transgastric peritoneos-copy: a novel approach to diagnostic and therapeutic interventions in the peritoneal cavity. Gastrointest Endosc. 2004;60:114–117. doi: 10.1016/s0016-5107(04)01309-4. [DOI] [PubMed] [Google Scholar]
- 13.Rattner D, Kalloo A. ASGE/SAGES Working Group. ASGE/SAGES Working Group on Natural Orifice Translumenal Endoscopic Surgery. October 2005. Surg Endosc. 2006;20:329–333. doi: 10.1007/s00464-005-3006-0. [DOI] [PubMed] [Google Scholar]
- 14.Decarli LA, Zorron R, Branco A, et al. New hybrid approach for NOTES transvaginal cholecystectomy: preliminary clinical experience. SurgInnov. 2009;16:181–186. doi: 10.1177/1553350609339375. [DOI] [PubMed] [Google Scholar]
- 15.Michalik M, Orlowski M, Bobowicz M, Frask A, Trybull A. The first report on hybrid NOTES adjustable gastric banding in humans. Obes Surg. 2011;21:524–527. doi: 10.1007/s11695-010-0130-2. [DOI] [PubMed] [Google Scholar]
- 16.Salinas G, Saavedra L, Agurto H, et al. Early experience in human hybrid transgastric and transvaginal endoscopic cholecystectomy. Surg Endosc. 2010;24:1092–1098. doi: 10.1007/s00464-009-0733-7. [DOI] [PubMed] [Google Scholar]
- 17.Kantsevoy SV, Hu B, Jagannath SB, et al. Transgastric endoscopic splenec-tomy: is it possible? Surg Endosc. 2006;20:522–525. doi: 10.1007/s00464-005-0263-x. [DOI] [PubMed] [Google Scholar]
- 18.Kantsevoy SV, Jagannath SB, Niiyama H, et al. Endoscopic gastrojejunostomy with survival in a porcine model. Gastrointest Endosc. 2005;62:287–292. doi: 10.1016/s0016-5107(05)01565-8. [DOI] [PubMed] [Google Scholar]
- 19.Bergström M, Ikeda K, Swain P, Park PO. Transgastric anastomosis by using flexible endoscopy in a porcine model (with video) Gastrointest Endosc. 2006;63:307–312. doi: 10.1016/j.gie.2005.09.035. [DOI] [PubMed] [Google Scholar]
- 20.Park PO, Bergström M, Ikeda K, Fritscher-Ravens A, Swain P. Experimental studies of transgastric gallbladder surgery: cholecystectomy and cholecystogastric anastomosis (videos) Gastrointest Endosc. 2005;61:601–606. doi: 10.1016/s0016-5107(04)02774-9. [DOI] [PubMed] [Google Scholar]
- 21.Wagh MS, Merrifield BF, Thompson CC. Survival studies after endoscopic transgastric oophorectomy and tubectomy in a porcine model. Gastrointest Endosc. 2006;63:473–478. doi: 10.1016/j.gie.2005.06.045. [DOI] [PubMed] [Google Scholar]
- 22.Ott D. Die direkte Beleuchtung der Bauchhoehle, der Harnblase, des Dickdams and des Uterus zu diagnostischen und operativen Zwecken. Rev Med Techeque (Prague) 1901;2:27–29. [Google Scholar]
- 23.Shibahara H, Shimada K, Kikuchi K, et al. Major complications and outcomes of diagnostic and operative transvaginal hydrolaparoscopy. J Obstet Gynaecol Res. 2007;33:705–709. doi: 10.1111/j.1447-0756.2007.00636.x. [DOI] [PubMed] [Google Scholar]
- 24.Zornig C, Mofid H, Siemssen L, et al. Transvaginal NOTES hybrid cholecystectomy: feasibility results in 68 cases with mid-term follow-up. Endoscopy. 2009;41:391–394. doi: 10.1055/s-0029-1214644. [DOI] [PubMed] [Google Scholar]
- 25.Bonin EA, Moran E, Bingener J, Knipschield M, Gostout CJ. A comparative study of endoscopic full-thickness and partial-thickness myotomy using submuco-sal endoscopy with mucosal safety flap (SEMF) technique. Surg Endosc. doi: 10.1007/s00464-011-2105-3. 2012 Jan 19. Epub ahead of print. [DOI] [PubMed] [Google Scholar]
- 26.Sumiyama K, Gostout CJ, Rajan E, et al. Pilot study of transesophageal endoscopic epicardial coagulation by submucosal endoscopy with the mucosal flap safety valve technique. Gastrointest Endosc. 2008;67:497–501. doi: 10.1016/j.gie.2007.08.040. [DOI] [PubMed] [Google Scholar]
- 27.Fritscher-Ravens A, Cuming T, Olagbaiye F, et al. Endoscopic transesophageal vs. thoracoscopic removal of mediastinal lymph nodes: a prospective randomized trial in a long-term animal survival model. Endoscopy. 2011;43:1090–1096. doi: 10.1055/s-0030-1256768. [DOI] [PubMed] [Google Scholar]
- 28.Gee DW, Willingham FF, Lauwers GY, Brugge WR, Rattner DW. Natural orifice transesophageal mediastinoscopy and thoracoscopy: a survival series in swine. Surg Endosc. 2008;22:2117–2122. doi: 10.1007/s00464-008-0073-z. [DOI] [PubMed] [Google Scholar]
- 29.Inoue H, Tianle KM, Ikeda H, et al. Peroral endoscopic myotomy for esophageal achalasia: technique, indication, and outcomes. Thorac Surg Clin. 2011;21:519–525. doi: 10.1016/j.thorsurg.2011.08.005. [DOI] [PubMed] [Google Scholar]
- 30.Moran EA, Bingener J, Gostout CJ. Functional and comparative evaluation of flexible monopolar endoscopic scissors. Surg Endosc. 2010;24:1769–1773. doi: 10.1007/s00464-009-0855-y. [DOI] [PubMed] [Google Scholar]
- 31.Moran EA, Gostout CJ, Bingener J. Preliminary performance of a flexible cap and catheter-based endoscopic suturing system. Gastrointest Endosc. 2009;69:1375–1383. doi: 10.1016/j.gie.2009.01.032. [DOI] [PubMed] [Google Scholar]
- 32.Kratt T, Küper M, Traub F, et al. Feasibility study for secure closure of natural orifice transluminal endoscopic surgery gastrotomies by using over-the-scope clips. Gastrointest Endosc. 2008;68:993–996. doi: 10.1016/j.gie.2008.06.057. [DOI] [PubMed] [Google Scholar]
- 33.Tiwari MM, Reynoso JF, Lehman AC, Tsang AW, Farritor SM, Oleynikov D. In vivo miniature robots for natural orifice surgery: state of the art and future perspectives. WorldJ Gastrointest Surg. 2010;2:217–223. doi: 10.4240/wjgs.v2.i6.217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Solovitch S. NeoGuide Systems ready with a new strategy, $43M later Silicon Valley/San Jose Business Journal January 13, 2008 http://www.bizjournals.com/sanjose/stories/2008/01/14/story7.html?page=all February 13, 2012
- 35. NeoGuide Systems. CrunchBase. http://www.crunchbase.com/company/neoguide-systems February 17, 2012
- 36.Omana JJ, Mistry S, Herron D, Kini S. Perception of NOTES among health care workers and medical students. Surg Innov. 2010;17:63–68. doi: 10.1177/1553350609360977. [DOI] [PubMed] [Google Scholar]
- 37.Peterson CY, Ramamoorthy S, Andrews B, Horgan S, Talamini M, Chock A. Women’s positive perception of transvaginal NOTES surgery. Surg Endosc. 2009;23:1770–1774. doi: 10.1007/s00464-008-0206-4. [DOI] [PubMed] [Google Scholar]
- 38.Swanstrom LL, Volckmann E, Hungness E, Soper NJ. Patient attitudes and expectations regarding natural orifice translumenal endoscopic surgery. Surg Endosc. 2009;23:1519–1525. doi: 10.1007/s00464-009-0431-5. [DOI] [PubMed] [Google Scholar]
- 39.Varadarajulu S, Tamhane A, Drelichman ER. Patient perception of natural orifice transluminal endoscopic surgery as a technique for cholecystectomy. Gas- trointest Endosc. 2008;67:854–860. doi: 10.1016/j.gie.2007.09.053. [DOI] [PubMed] [Google Scholar]
- 40.Volckmann ET, Hungness ES, Soper NJ, Swanstrom LL. Surgeon perceptions of natural orifice translumenal endoscopic surgery (NOTES) J Gastrointest Surg. 2009;13:1401–1410. doi: 10.1007/s11605-009-0921-8. [DOI] [PubMed] [Google Scholar]
- 41.Strickland AD, Norwood MG, Behnia-Willison F, Olakkengil SA, Hewett PJ. Transvaginal natural orifice translumenal endoscopic surgery (NOTES): a survey of women’s views on a new technique. Surg Endosc. 2010;24:2424–2431. doi: 10.1007/s00464-010-0968-3. [DOI] [PubMed] [Google Scholar]
- 42.Bingener J, Sloan JA, Ghosh K, McConico A, Mariani A. Qualitative and quantitative analysis of women’s perceptions of transvaginal surgery. Surg Endosc. 2012;26:998–1004. doi: 10.1007/s00464-011-1984-7. [DOI] [PubMed] [Google Scholar]
- 43.Bonin EA, Moran E, Gostout CJ, McConico AL, Zielinski M, Bingener J. Natural orifice transluminal endoscopic surgery for patients with perforated peptic ulcer. Surg Endosc. doi: 10.1007/s00464-011-2063-9. 2011 Dec 17. Epub ahead of print. [DOI] [PubMed] [Google Scholar]
- 44.Imhof M, Epstein S, Ohmann C, Röher HD. Duration of survival after peptic ulcer perforation. WorldJ Surg. 2008;32:408–412. doi: 10.1007/s00268-007-9370-2. [DOI] [PubMed] [Google Scholar]
- 45.Blatnik JA, Ponsky TA. Advances in minimally invasive surgery in pediatrics. Curr Gastroenterol Rep. 2010;12:211–214. doi: 10.1007/s11894-010-0109-0. [DOI] [PubMed] [Google Scholar]
- 46.Lacy AM, Delgado S, Rojas OA, Almenara R, Blasi A, Llach J. MA-NOS radical sigmoidectomy: report of a transvaginal resection in the human. Surg Endosc. 2008;22:1717–1723. doi: 10.1007/s00464-008-9956-2. [DOI] [PubMed] [Google Scholar]
- 47.Sanchez JE, Rasheid SH, Krieger BR, Frattini JC, Marcet JE. Laparosco-pic-assisted transvaginal approach for sigmoidectomy and rectocolpopexy. JSLS. 2009;13:217–220. [PMC free article] [PubMed] [Google Scholar]
- 48.Dozois EJ, Larson DW, Dowdy SC, Poola VP, Holubar SD, Cima RR. Transvaginal colonic extraction following combined hysterectomy and laparoscopic total colectomy: a natural orifice approach. Tech Coloproctol. 2008;12:251–254. doi: 10.1007/s10151-008-0428-4. [DOI] [PubMed] [Google Scholar]
- 49.Kaouk JH, Haber GP, Goel RK, et al. Pure natural orifice translumenal endoscopic surgery (NOTES) transvaginal nephrectomy. Eur Urol. 2010;57:723–726. doi: 10.1016/j.eururo.2009.10.027. [DOI] [PubMed] [Google Scholar]
- 50.Targarona EM, Gomez C, Rovira R, et al. NOTES-assisted transvaginal sple-nectomy: the next step in the minimally invasive approach to the spleen. Surg Innov. 2009;16:218–222. doi: 10.1177/1553350609345488. [DOI] [PubMed] [Google Scholar]
- 51.Cuschieri A. The Arachness system. Late-breaking technology session. Presented at the Scientific Session of the Society of American Gastrointestinal and Endoscopic Surgeons (SAGES); April 14-17, 2010; National Harbor, Maryland.