Abstract
Objective
To examine the acculturation-health relationship between acculturation and biomarkers of the metabolic syndrome.
Methods
Cross-sectional sample data of 1,781 Mexican Americans (60-years and older) from northern California were analyzed. Biomarkers (waist circumference, blood pressure, fasting plasma glucose, triglycerides and high-density lipids) were used to construct the metabolic syndrome outcome variable using American Heart Association criteria. The Acculturation Rating Scale for Mexican Americans-II score was the primary predictor.
Results
US- and foreign-born respondents did not differ significantly in their metabolic risk profile. Nearly half of the sample (45.6%) met AHA criteria for the metabolic syndrome biomarkers, and the two nativity groups were not statistically distinct (χ2 = 0.26; P= 0.61). Higher acculturation scores were significantly lower risk for the metabolic syndrome for foreign-born, but not US-born Mexican Americans.
Discussion
Immigrant health advantages over US-born Mexican Americans were not evident in older adulthood. Among older foreign-born Mexican Americans, higher acculturation was associated with lower metabolic syndrome risk, which suggests that the prevailing acculturative stress hypothesis may not apply to older adults. Any negative relationship between acculturation and health found in younger adults appears to have yielded to different developmental healthcare influences in later adulthood. We conclude that examining the cultural and developmental aspects of acculturation may help better our understanding of the health and aging of Mexican Americans.
INTRODUCTION
The Latino health paradox asserts that, despite experiencing disproportionate exposure to purported risk factors for excess morbidity and mortality associated with low socioeconomic position, Mexican American immigrants, generally have more favorable health outcomes compared to Mexican Americans born in the United States (US-born) and non-Latino Whites (Markides & Coreil, 1986). Furthermore, the longer these healthy immigrants resided in the United States and acculturated, the more likely they were to report deterioration in health status indicators compared to recent immigrants (Antecol & Bedard, 2006).
To explain immigrant health deterioration, Rogler and colleagues described “acculturation as an exogenous force shaping the conditions for the rise to psychological distress”(Rogler, Cortes, & Malgady, 1991). This phenomenon was later called the “acculturative stress” hypothesis and widely used in mental health studies and generalized to an array of other health outcomes research with Latino populations. However acculturation stress models have important limitations in health research because they confound cultural change effects on health behaviors with pathology, they are not temporally specific and thus, inconsistent with developmental models of health. We offered the alternative “acculturation-health” hypothesis; to emphasize that health outcomes are instead conditional on multiple life-course contingencies that vary in importance as determinants over the lifespan (González et al., 2009). The acculturation-health temporal relationships can range from negative to positive during the lifespan of an individual. Acculturation stress assumes a cumulative, dose-response negatively linear association between acculturation and health. Acculturation-health involves interactions between endogenous (within-person) and exogenous (extra-person) factors that may affect health differentially over the life-course.
The proposed acculturation-health model assumes that there are multiple points in the life-course that are critical for improving health and lowering the risk of “weathering effects” seen in minority aging (Geronimus, 1992). Carefully focused research could lead to timely and effective interventions that improve health outcomes across the life-course. The assumption of a constant acculturation-health relationship that is generally negative leading to declines in Mexican American health is limiting because it is overly deterministic, and restricts opportunities for identifying determinants of long-range outcomes and life-course stages when they are most consequential. While we can assume that living in a new society introduces behavioral, social and environmental changes that may negatively influence health, there may be benefits as well, such as learning new occupational skills, greater exposure to public health information, and use of preventive medicine. Nevertheless, it is unclear how these changes are expressed in the health of older Mexican Americans in the long run.
Negative aspects of the acculturation-health relationship dominate current thinking about Mexican American health, especially regarding acculturation-related changes in risk behaviors such as diet, exercise, and substance abuse (Morales, Lara, Kington, Valdez, & Escarce, 2002). However, most of this evidence comes from studies with younger Latinos (Lara, Gamboa, Kahramanian, Morales, & Bautista, 2005). If the acculturation–health association is conditional and predicated on various endogenous and exogenous life-course factors, recent work among older adults may better inform us about the long-term acculturation-health relationship. Among older Mexican Americans and in contrast to younger adults, the relationship between acculturation and health appears positive from extant studies (González et al., 2009; González, Haan, & Hinton, 2001; Markides, Eschbach, Ray, & Peek, 2007). A limitation to much of the work on acculturation and health, including older Mexican Americans, is that outcomes are largely based on self-rated health status that reportedly can be influenced by cultural biases (Finch, Hummer, Reindl, & Vega, 2002). Secondly, most studies use proxy measures of acculturation (e.g., years of US residency), which provides little information on variations in cultural and behavioral patterns associated with acculturation (González et al., 2009).
One study purpose was to examine if the “healthy immigrant” phenomenon persisted among older Mexican Americans by examining a cluster of biological markers associated with the metabolic syndrome. Secondly, we sought to evaluate the relationship between biomarkers of the metabolic syndrome and a measure of acculturation that provides information on variations in cultural and behavioral patterns. For this, we used a large sample of older Mexican Americans. Based on previous work (Eschbach, Al-Snih, Markides, & Goodwin, 2007; González et al., 2001; Haan et al., 2003; Markides et al., 2007), we expected that rates of the metabolic syndrome between US-born and foreign-born Mexican Americans would not differ. Secondly, we expected that higher acculturation would be associated with lower odds of the metabolic syndrome among foreign-born older Mexican Americans. Thirdly, we examined the relationship between biomarkers and acculturation while including potentially moderating factors of socioeconomic position and health insurance (Adler et al., 1994; Andersen & Newman, 1973; Crimmins, Hayward, & Seeman, 2004). Finally, we examined the metabolic syndrome among older Mexican Americans in the context of comparing the prevailing “acculturative stress” hypothesis and “acculturation-health” hypothesis, which assumes multiple points in the life-course that are critical for improving health, to understand their utility for the study of health.
METHODS
Study Participants
Participants are from the Sacramento Area Latino Study on Aging (SALSA), which is a prospective cohort study of older Latinos living in Sacramento valley of northern California. The study was approved by the IRBs of the University of Michigan and of the University of California, Davis. Analyses for this report were approved by the Human Investigation Committee of Wayne State University. All SALSA participants were 60 years or older and self-designated as Latino (85.6% Mexican origin). The methods of enumeration and recruitment procedures have been previously published and produced a sample that was representative of older Latinos residing in the targeted areas (Haan et al., 2003). Briefly, surveys were conducted by bilingual/bicultural technicians in the participants’ homes to obtain demographic, health, and functional status information. Survey instruments were translated from English to Spanish and then back-translated to English to ensure the accuracy of the translations. The total baseline year (1998/1999) sample of the SALSA was 1,781 participants. In this study, we focused on participants with valid baseline biomarker data.
Biomarker Outcome Measures
Cross-sectional data for these analyses came from the SALSA baseline year (1998/1999). During in-home, face-to-face interviews, study participants underwent a clinical assessment that included anthropometry, fasting blood draw, and blood pressure. High-density lipids, triglycerides, and glucose levels were assayed from fasting blood samples. Waist circumference measurements (cm) were taken at umbilicus level at mid-respiration with the participant standing erect. Systolic and diastolic blood pressure (mmHg) was measured using a standard arm cuff.
We used the American Heart Association (AHA) criteria to define the metabolic syndrome and identify study participants who met these guidelines.(Grundy et al., 2005) The six AHA metabolic syndrome criteria were examined recoded. Following AHA guidelines, we applied gender specific dichotomization to all six criteria with values exceeding threshold levels that were assigned a value 1, to indicate the criterion was met, and all other valid values assigned a 0. AHA metabolic syndrome criteria are shown in Table 2. A hypertension criterion was generated based on values meeting criterion for either systolic or diastolic risk classified at or above criterion levels. Further, an additive risk scale (count) was created by summing total scores (range 0–5) based on the five dichotomous variables indicating criteria were met. To create our metabolic syndrome indicator, we applied AHA criteria to categorize the summed scores three or more on our additive scale as meeting metabolic syndrome criteria with all other lesser values assigned to the reference group.
Table 2.
American Heart Association criteria for metabolic syndrome risk factors
| Males | Females | |
|---|---|---|
| High density lipids (mg/dL) | ≤ 40 | ≤ 50 |
| Triglycerides (mg/dL) | ≥ 150 | ≥ 150 |
| Systolic blood pressure (Hg) | ≥ 130 | ≥ 130 |
| Diastolic blood pressure | ≥ 85 | ≥ 85 |
| Waist circumference (inches) | ≥ 40 | ≥ 35 |
| Fasting plasma glucose (mg/dL) | ≥ 100 | ≥ 100 |
Acculturation
The primary predictor variable of interest was acculturation. To assess acculturation, we used the revised Acculturation Rating Scale for Mexican Americans-II (ARSMA-II; (Cuellar, Arnold, & Maldonado, 1995). Briefly, the ARSMA is a series of seventeen Likert-type self-ratings on cultural practices, such as language and media use and social network contacts. The Likert-type ratings were then summed across items (range=17–70).
Statistical Approach
First, sample estimates describing demographic and socioeconomic characteristics including age (continuous), sex (female; male), nativity (foreign-born; US-born), education (four categories: less than high school, high school degree, some college and college or more), monthly household income (five categories: less than $1,000, $1,000–$1,499, $1,500–$1,999, $2,000–$2,499 and $2,500 or more), home ownership (own home or not) and health insurance coverage (insured or not insured) were calculated. Second, prevalence for the six metabolic syndrome AHA criteria (Table 2) was estimated. These prevalence estimates were further disaggregated by nativity. Metabolic syndrome was coded as a dichotomous variable. Third, logistic regression models were used to estimate the relationship between the metabolic syndrome acculturation and nativity. Of particular interest were the differential effects of acculturation on metabolic syndrome across nativity groups, which were captured using a multiplicative interaction term created between acculturation and nativity. Secondly, the multivariate models were used to examine the moderating effects of 1) socioeconomic indicators and 2) health insurance coverage. Both models were age and sex adjusted. The Stata statistical package (Release 10.1) was used for all of the analyses in this study (StataCorp, 2008).
RESULTS
Table 1 shows selected demographic and socioeconomic indicators for the overall SALSA sample and disaggregated by US-born foreign-born groups. Over 85% of the SALSA sample was of Mexican origin, and the remainder were Central and South American, which is consistent with 2000 US Census estimates for California (Census, 2000). We used the term Mexican American since this is the prevailing Latin American culture of the Sacramento Valley and the number of Central Americans was very small. The sample was evenly split between US- and foreign-born groups (Table 1). The foreign-born sample had significantly lower levels of education and household income, were significantly less likely to own their home, and significantly less likely to have health insurance coverage compared to their US-born counterparts.
Table 1.
Demographic characteristics of a sample of older Latinos (aged 60-years or older) from the Sacramento Area Latino Study on Aging (SALSA).
| Overall (n=1789) |
US-born (n=871) |
Foreign-born (n=908) |
|
|---|---|---|---|
| Age (Years), mean (SE) | 70.7 (0.2) | 70.1 (0.2) | 71.2 (0.3) |
| Sex, % (SE) | |||
| Female | 58.2 (1.2) | 56.5 (1.7) | 59.8 (1.6) |
| Male | 41.8 (1.2) | 43.5 (1.7) | 40.2 (1.6) |
| Nativity, % (SE) | |||
| US-born | 49.3 (1.2) | -- | -- |
| Foreign-born | 50.7 (1.2) | -- | -- |
| Education (Years), % (SE) | |||
| Less than High School | 70.6 (1.1) | 54.8 (1.7) | 86.0 (1.2) |
| High school | 12.8 (0.8) | 19.2 (1.3) | 6.5 (0.8) |
| Some college | 10.3 (0.7) | 16.2 (1.3) | 4.6 (0.7) |
| College or more | 6.3 (0.6) | 9.9 (1.0) | 2.8 (0.6) |
| Household Income (US Dollars/month), % (SE) | |||
| Less than $1,000 | 44.8 (1.2) | 30.0 (1.6) | 59.3 (1.7) |
| $1,000–$1,499 | 20.3 (1.0) | 19.0 (1.3) | 21.7 (1.4) |
| $1,500–$1,999 | 11.4 (0.8) | 14.3 (1.2) | 8.6 (0.9) |
| $2,000–$2,499 | 9.3 (0.7) | 13.4 (1.2) | 5.4 (0.8) |
| $2.500 or more | 14.1 (0.8) | 23.4 (1.4) | 5.1(0.7) |
| Home ownership, % (SE) | |||
| Other | 32.9 (1.1) | 22.3 (1.4) | 43.2 (1.7) |
| Own home | 67.1 (1.1) | 77.7 (1.4) | 56.8 (1.7) |
| Insurance, % (SE) | |||
| Not Insured | 9.2 (0.7) | 2.6 (0.5) | 15.6 (1.2) |
| Insured | 90.8 (0.7) | 97.4 (0.5) | 84.4 (1.2) |
Metabolic Syndrome
The US- and foreign-born samples were evenly matched on each of the AHA metabolic syndrome criteria. With the exception of hyperglycemia, US- and foreign-born respondents did not differ significantly in their metabolic risk profile. Nearly half of the sample (45.6%) met AHA criteria for the metabolic syndrome and the two nativity groups were not statistically distinct (χ2 = 0.26; P= 0.61).
Metabolic Syndrome, Acculturation and Nativity
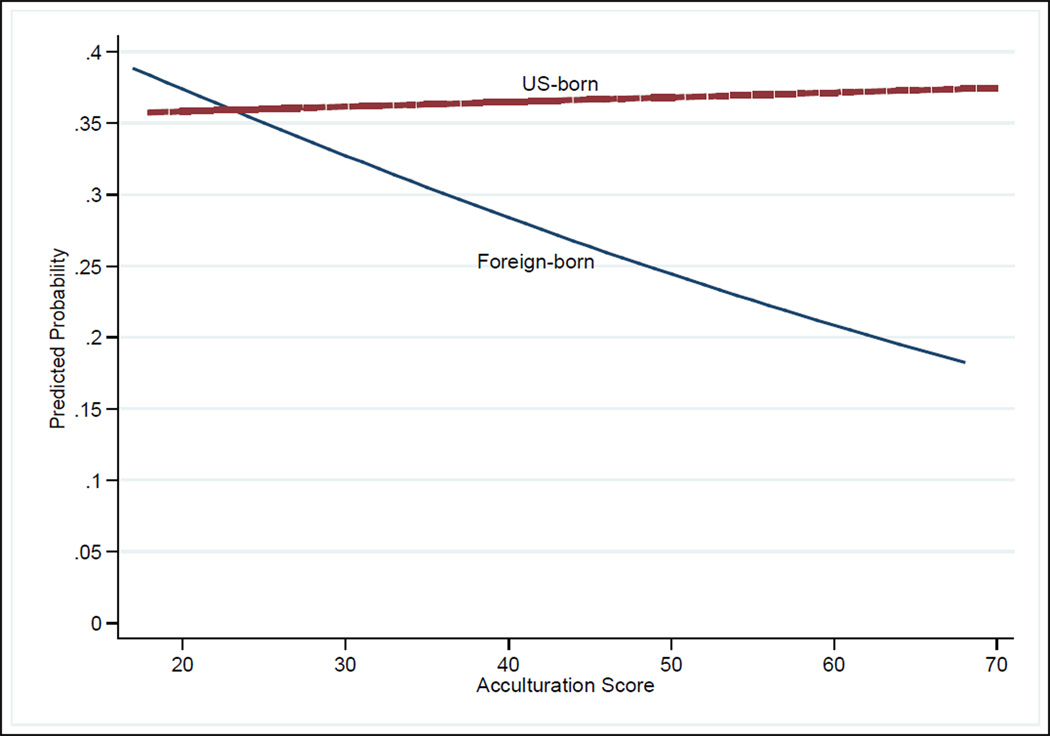
Higher ARSMA-II scores indicating more acculturation were associated with significantly decreased odds of the metabolic syndrome (Table 4, Model 1). Of particular interest were the differential effects of acculturation on metabolic syndrome across nativity groups, which were captured in a multiplicative interaction term created between acculturation and nativity. The interaction term was significant, indicating that the effect of acculturation on the odds of metabolic syndrome varied by nativity (P=0.045). The non-significant effect of nativity on metabolic syndrome, indicated at the bivariate level above, was reproduced using our multivariate results. When socioeconomic factors were introduced in Model 2, the effect (OR) of acculturation on metabolic syndrome was slightly moderated. Accounting for the socioeconomic indicators also had a moderating effect on the statistical significance of the interaction term (P=0.053). In Model 2, socioeconomic factors slightly moderated the relationship between metabolic syndrome and ARSMA-II scores. This indicates that while acculturation plays an important predictive role for foreign-born respondents, the effect of acculturation among US-born respondents is only marginally significant. The predicted probabilities of the metabolic syndrome by nativity groups across acculturation scores are plotted in Figure 1. Among the socioeconomic indicators considered, only the two middle-household income categories were significantly associated with lower odds of the metabolic syndrome relative to the lowest income group.
Table 4.
Predictors of Metabolic Syndrome using American Heart Association criteria using sample of older Latinos (aged 60-years or older) from the Sacramento Area Latino Study on Aging (SALSA).
| Model 1 | Model 2 | |||
|---|---|---|---|---|
| OR | 95 % CI | OR | 95 % CI | |
| Nativity | ||||
| Foreign-born | 1.00 | -- | 1.00 | -- |
| US-born | 0.61 | 0.26–1.42 | 0.60 | 0.26–1.43 |
| Acculturation | 0.97*** | 0.96–0.99 | 0.98** | 0.96–1.00 |
| Interaction | ||||
| US-born×Acculturation | 1.02** | 1.00–1.04 | 1.02* | 0.99–1.04 |
| Age | 0.99 | 0.98–1.01 | 0.99 | 0.97–1.00 |
| Sex | ||||
| Female | 1.00 | -- | 1.00 | -- |
| Male | 0.62*** | 0.51–0.76 | 0.65*** | 0.53–0.81 |
| Education | ||||
| Less than High School | 1.00 | -- | ||
| High school | 0.82 | 0.58–1.15 | ||
| Some college | 0.99 | 0.68–1.43 | ||
| College or more | 0.84 | 0.53–1.34 | ||
| Household Income (US Dollars/month) | ||||
| Less than $1,000 | 1.00 | -- | ||
| $1,000–1,499 | 0.84 | 0.63–1.13 | ||
| $1,500–$1,999 | 0.69** | 0.47–1.00 | ||
| $2,000–2,499 | 0.68* | 0.45–1.02 | ||
| $2,500 or more | 0.84 | 0.56–1.25 | ||
| Home Ownership | ||||
| Other | 1.00 | -- | ||
| Own Home | 0.98 | 0.76–1.27 | ||
| Insurance | ||||
| Not Insured | 1.00 | -- | ||
| Insured | 1.19 | 0.82–1.73 | ||
P≤ 0.01
P≤ 0.05
P≤ 0.10
Figure 1.
Predicted probability of Metabolic Syndrome using American Heart Association criteria using sample of older Latinos (aged 60 years or older) from the Sacramento Area Latino Study on Aging (SALSA).
DISCUSSION
Two main findings emerged from our study. First, we found no metabolic syndrome biomarker evidence of healthy immigrant advantages over US-born Mexican Americans. Secondly, higher acculturation was associated with lower risk for meeting AHA criteria for the metabolic syndrome among foreign-born Mexican Americans. Our findings are consistent with previous work demonstrating healthy immigrant advantages may not endure into older age and that acculturation is positively related with health (Crimmins, Kim, Alley, Karlamangla, & Seeman, 2007; González et al., 2009) The findings herein extend previous work based on self-reported functional health and proxies of acculturation with biomarkers and an acculturation measure that better characterizes cultural nuances. This study supports the acculturation-health hypothesis in that it accounted for a positive relationship between acculturation and health as opposed to a strictly negative and deleterious relationship that would be expected from the prevailing acculturative stress hypothesis. Finally, our findings are consistent with our hypothesis that the acculturation-health relationship is non-linear over the lifecourse; however, longitudinal information is needed to determine important developmental periods when health can be favorably modified.
To our knowledge, this is the first study to examine the relationship between acculturation and biomarkers associated with a specific health outcome. Our study is consistent with Crimmins and colleagues (2007) work showing no healthy immigrant biomarker profile advantages over non-Latino Whites (Crimmins et al., 2007). Our study extends Crimmins and colleagues work by examining the relationship between acculturation and a cluster of biomarkers associated with a specific and well defined medical syndrome. In addition, we were able to apply a theoretical framework for testing competing hypotheses on the relationship between acculturation and health. The results support the acculturation-health hypothesis and demonstrate its utility in understanding the complex relationship between acculturation and health in later adulthood.
There is evidence that immigrants lose their health advantages and converge with US-born Latinos after 15-years post-migration (Alderete, Vega, Kolody, & Aguilar-Gaxiola, 2000; Antecol & Bedard, 2006). Those observation suggest that acculturative stress would continuously exert deleterious effects on immigrant health. Beyond 15-years, the long-term acculturation-health relationship is not well known. Our findings suggest that the trajectory of the long-term acculturation-health relationship may deflect positively at some point after 15-years; however, precisely when this change or series of changes occurs could not be addressed in this study and remains known. Furthermore, the influential factor or factors affecting changes in the acculturation-health relationship are poorly understood. We hypothesized that those factors enabling better healthcare access would explain the positive association between acculturation and health; however, the healthcare access enabling factors that we examined inadequately explained this relationship. This is consistent with previous work and suggests that other factors may be operating to affect the trajectory of the acculturation-health relationship (González et al., 2009). Some influential factors that could affect the acculturation-health relationship may include a full spectrum of environmental conditions (i.e., toxic exposures), goods and services including improved communication with healthcare providers and other agents, better access to healthcare information (e.g., internet resources) and comprehension of that information (e.g., public health messages and medical prescriptions), healthier and safer neighborhood environmental conditions (for the individual and family), and less physiological and psychological stress associated with life as a minority in the US in a lowest socioeconomic position (González, Vega, & Tarraf, 2010). We are not suggesting that acculturation is a cure for all ills affecting Mexican Americans. Indeed, acculturation comes at costs to one’s cultural identity that may also affect the family and distance from family ties in Mexico. Instead, we posit that in the balance, positive aspects of acculturation may outweigh any negative factors relative to health, particularly in the later years of life when health needs change and are often more apparent. From developmental and public health perspectives, identifying deleterious and protective factors affecting health and important periods may prove valuable in improving health and reducing the disease burden for this important population over the lifecourse.
Study limitations
There are several caveats to consider when interpreting the results of our study. First, we relied on cross-sectional data, which is not informative about the time-varying factors influencing health. Furthermore, we examined a small set of factors that could influence the acculturation-health relationship and other unexamined factors may be more influential than those selected for this study. We did not examine return migration; however, our previous work with this sample indicates that the influence of return migration is not substantial (Patel, Eschbach, Ray, & Markides, 2004).
Conclusions
Immigrant health advantages over US-born Mexican Americans are not evident in older adulthood. Among older immigrant Mexican Americans, higher acculturation was associated with lower metabolic syndrome risk. Any negative relationship between acculturation and health found in younger adults may yield to different developmental healthcare influences in later adulthood. Our findings showed that the relationship between acculturation and health is complex and varies not only by nativity, but also developmentally. We conclude that examining the cultural and developmental aspects of acculturation may help better our understanding of the health and aging of Mexican Americans.
Table 3.
Older Mexican American Prevalence estimates of Metabolic Syndrome using American Heart Association criteria.
| Overall | US-born | Foreign-born | ||||
|---|---|---|---|---|---|---|
| % | SE | % | se | % | se | |
| High density lipids | 33.0 | 1.2 | 32.1 | 1.6 | 34.0 | 1.7 |
| Triglycerides | 53.6 | 1.2 | 55.4 | 1.7 | 51.7 | 1.8 |
| Systolic blood pressure | 65.0 | 1.2 | 63.9 | 1.7 | 66.1 | 1.7 |
| Diastolic blood pressure | 19.9 | 1.0 | 20.8 | 1.4 | 19.0 | 1.4 |
| Waist circumference | 51.3 | 1.2 | 51.5 | 1.8 | 51.0 | 1.7 |
| Fasting plasma glucose | 34.2 | 1.2 | 37.5 | 1.7 | 31.0 | 1.6 |
| Metabolic Syndrome | 45.6 | 1.2 | 46.3 | 1.8 | 45.0 | 1.8 |
Acknowledgments
Funding/Support:
Drs. González and Tarraf are supported by the NIMH MH 84994 and NHLBI HC 65233.
Dr. Haan is supported by NIA (R01) AG12975 and (R03) AG33751, and DK60753.
Role of Funding Source: This work was supported by the National Institutes of Health, National Institute of Mental Health, National Heart Lung Blood Institute and the National Institute on Aging. Its contents are solely the responsibility of the authors and do not necessarily represent the official views of the NIH.
Footnotes
Financial Disclosures: The authors report no conflicts of interest that could inappropriately influence, or be perceived to influence, this work.
REFERENCES
- Adler NE, Boyce T, Chesney MA, Cohen S, Folkman S, Kahn RL, et al. Socioeconomic status and health. The challenge of the gradient. American Psychologist. 1994;49(1):15–24. doi: 10.1037//0003-066x.49.1.15. [DOI] [PubMed] [Google Scholar]
- Alderete E, Vega WA, Kolody B, Aguilar-Gaxiola S. Lifetime prevalence of and risk factors for psychiatric disorders among Mexican migrant farmworkers in California. American Journal of Public Health. 2000;90(4):608–614. doi: 10.2105/ajph.90.4.608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Andersen R, Newman J. Societal and individual determinants of medical care utilization. Milbank Memorial Fund Quarterly. 1973;51:95–124. [PubMed] [Google Scholar]
- Antecol H, Bedard K. Unhealthy assimilation: why do immigrants converge to American health status levels? Demography. 2006;43(2):337–360. doi: 10.1353/dem.2006.0011. [DOI] [PubMed] [Google Scholar]
- Census, U.S. American FactFinder. 2000 from http://www.census.gov/
- Crimmins EM, Hayward MD, Seeman TE. Race/Ethnicity, Socioeconomic Status, and Health. In: Anderson NB, Bulatao RA, Cohen B, editors. Critical Perspectives on Racial and Ethnic Differences in Late Life. Washington, DC: The National Academies Press; 2004. pp. 310–352. [Google Scholar]
- Crimmins EM, Kim JK, Alley DE, Karlamangla A, Seeman T. Hispanic paradox in biological risk profiles. Am J Public Health. 2007;97(7):1305–1310. doi: 10.2105/AJPH.2006.091892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cuellar I, Arnold B, Maldonado R. Acculturation Rating Scale for Mexican Americans-II: A revision of the original ARSMA Scale. Hispanic Journal of Behavioral Sciences. 1995;17(3):275–304. [Google Scholar]
- Eschbach K, Al-Snih S, Markides KS, Goodwin JS. Disability and Active Life Expectancy of Older US- and Foreign-born Mexican Americans. In: Angel JL, Whitfield KE, editors. The Health of Aging Hispanics: The Mexican-Origing Population. New York: Springer; 2007. pp. 40–49. [Google Scholar]
- Finch BK, Hummer RA, Reindl M, Vega WA. Validity of self-rated health among Latino(a)s. Am J Epidemiol. 2002;155(8):755–759. doi: 10.1093/aje/155.8.755. [DOI] [PubMed] [Google Scholar]
- Geronimus AT. The weathering hypothesis and the health of African-American women and infants: evidence and speculations. Ethn Dis. 1992;2(3):207–221. [PubMed] [Google Scholar]
- González HM, Ceballos M, Tarraf W, West BT, Bowen ME, Vega WA. The Health of Older Mexican Americans in the Long Run. American Journal of Public Health. 2009;10(99):1879–1885. doi: 10.2105/AJPH.2008.133744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- González HM, Haan MN, Hinton L. Acculturation and the prevalence of depression in older Mexican Americans: baseline results of the Sacramento Area Latino Study on Aging. Journal of the American Geriatrics Society. 2001;49(7):948–953. doi: 10.1046/j.1532-5415.2001.49186.x. [DOI] [PubMed] [Google Scholar]
- González HM, Vega WA, Tarraf W. Health Care Quality Perceptions among Foreign-Born Latinos and the Importance of Speaking the Same Language. The Journal of the American Board of Family Medicine. 2010;23(6):745–752. doi: 10.3122/jabfm.2010.06.090264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grundy SM, Cleeman JI, Daniels SR, Donato KA, Eckel RH, Franklin BA, et al. Diagnosis and Management of the Metabolic Syndrome: An American Heart Association/National Heart, Lung, and Blood Institute Scientific Statement: Executive Summary. Circulation. 2005;112(17):e285–e290. doi: 10.1161/CIRCULATIONAHA.105.169404. [DOI] [PubMed] [Google Scholar]
- Haan MN, Mungas DM, González HM, Ortiz TA, Acharya A, Jagust WJ. Prevalence of dementia in older Latinos: the influence of type 2 diabetes mellitus, stroke and genetic factors. Journal of the American Geriatrics Society. 2003;51(2):169–177. doi: 10.1046/j.1532-5415.2003.51054.x. [DOI] [PubMed] [Google Scholar]
- Lara M, Gamboa C, Kahramanian MI, Morales LS, Bautista DE. Acculturation and Latino health in the United States: a review of the literature and its sociopolitical context. Annu Rev Public Health. 2005;26:367–397. doi: 10.1146/annurev.publhealth.26.021304.144615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Markides KS, Coreil J. The health of Hispanics in the southwestern United States: an epidemiologic paradox. Public Health Rep. 1986;101(3):253–265. [PMC free article] [PubMed] [Google Scholar]
- Markides KS, Eschbach K, Ray LA, Peek MK. Census Disability Rates Among Older People by Race/Ethnicity and Type of Hispanic Origin. In: Angel JL, Whitfield KE, editors. The Health of Aging Hispanics: The Mexican-Origing Population. New York: Springer; 2007. [Google Scholar]
- Morales LS, Lara M, Kington RS, Valdez RO, Escarce JJ. Socioeconomic, cultural, and behavioral factors affecting Hispanic health outcomes. J Health Care Poor Underserved. 2002;13(4):477–503. doi: 10.1177/104920802237532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patel KV, Eschbach K, Ray LA, Markides KS. Evaluation of mortality data for older Mexican Americans: implications for the Hispanic paradox. Am J Epidemiol. 2004;159(7):707–715. doi: 10.1093/aje/kwh089. [DOI] [PubMed] [Google Scholar]
- Rogler LH, Cortes DE, Malgady RG. Acculturation and mental health status among Hispanics: Convergence and new directions for research. American Psychologist. 1991;46(6):585–597. doi: 10.1037//0003-066x.46.6.585. [DOI] [PubMed] [Google Scholar]
- StataCorp. College Station, TX; 2008. Stata Statistical Software (Release 10.1) [Google Scholar]