Abstract
The objective of the study is to evaluate patients' quality of life (QOL) after endoscopic resection of skull base tumors. We estimated the QOL of 41 patients who underwent surgery for removal of skull base tumors via the expanded endonasal approach (EEA). The Anterior Skull Base Surgery Questionnaire (ASBS-Q), a multidimensional, disease-specific instrument containing 36 items was used. The rate of meningitis and cerebrospinal fluid leak was 1.4 and 0%, respectively. There was one case of uniocular visual impairment. The internal consistency of the instrument had a correlation coefficient (α-Cronbach score) of 0.8 to 0.92. Of 41 patients, 30 (75%) reported improvement or no change in overall QOL. Improved scores were reported in the physical function domain and worse scores in the specific symptoms domain. The most significant predictor of poor QOL was female gender, which led to a significant decrease in scores of all domains. Site of surgery, histology, age and comorbidity were not significant predictors of outcome. This paper further validates the use of the ASBS-Q for patients undergoing endoscopic skull base resection. The overall QOL of patients following endoscopic extirpation of skull base tumors is good. Female patients experience a significant decline in QOL compared with males.
Keywords: quality of life, endoscopy, morbidity, skull base, sinuses, craniofacial
There has been an increasing acknowledgment of the importance of topics addressing the quality of life (QOL) of patients with cancer. QOL is assessed in an effort to improve treatment modalities, to promote restoration of the patient's daily function, and to accelerate his return to normal life. Estimation of the influence of specific surgical procedures on QOL can serve as a means by which the most appropriate surgical approach can be selected for a given patient, especially when no single modality has a clear survival advantage over the others. Detailed understanding of the different aspects of QOL may help surgeons improve assessment and management of patients, identify possible obstacle as early as possible during follow-up, and guide the choices of medical interventions.1 Furthermore, early access of patients to detailed information about their disease can yield better adjustment to an imminent medical condition. A multidimensional evaluation of QOL involves retrieving information on the physical, emotional, social, and economical aspects of the patient's lifestyle, as well as on specific symptoms associated with their disease. Valid interpretation of the data requires disease-specific instruments, which cover the morbidity associated with the site of cancer and its treatment.2
The technical development of endonasal surgery has had a major positive impact on the management of patients with lesions involving paranasal sinuses, anterior cranial fossa, sella, and clivus.3 This procedure may, however, carry a considerable risk and serious morbidity. The expanded endonasal approach (EEA) was developed for the extirpation of anterior and middle skull base neoplasms.4 Although subsequent reports have established it as being effective for the removal of both benign and malignant tumors,5 tumor control should not be the only goal of patient care. During the last decade, numerous studies have assessed QOL issues in patients with skull base tumors,6,7 however there is little information data on the physical and psychological sequela of endoscopic skull base surgery in general and on the EEA specifically.
The aim of this study was to assess the influence of endoscopic surgery for extirpation of skull base tumors on patients' QOL. Since skull base surgery differs from other head and neck procedures, the psychological, social and physical well being of this group of patients were assessed using a disease-specific multidimensional questionnaire.8
Materials and Methods
This study is based on a review of the hospital charts of 41 patients operated between 2008 and 2010 for extirpation of skull base tumors at our institution. All operations were performed via the EEA and performed by the same interdisciplinary team. All the candidates who agreed to fill out a QOL questionnaire also gave a full medical history and underwent a physical examination on the same day. The demographic data of the patients are shown in Table 1. Comorbidity was defined according to the Charlson Comorbidity Index. An independent physician conducted all the interviews to avoid any bias that could stem from surgeon–patient interaction.
Table 1. Demographic Characterization of the Patients.
| Demographic Features | n (%) | |
|---|---|---|
| Gender | Male | 23 (57) |
| Female | 18 (43) | |
| Age (y) | <60 | 24 (58) |
| >60 | 17 (42) | |
| Mean | 55 ± 17 | |
| Comorbiditya | Yes | 9 (29) |
| No | 32 (71) | |
| Radiotherapy | Yes | 4 (10) |
| No | 37 (90) | |
| Months after surgery | 6–12 | 16 (39) |
| >24 | 25 (61) | |
| Histology type | Malignant | 35 (85) |
| Benign | 6 (15) |
Myocardial infarction; chronic lung disease; heart failure, peripheral vascular disease, cerebrovascular accident, liver dysfunction, chronic renal failure, diabetes mellitus, other malignancies.
The patients were at least 18 years old, were able to read and write, had no severe psychopathological or cognitive impairment, and gave their informed consent to participate in this survey. All patients have been operated on >6 months before study entry. The study was approved by the Institution Review Board.
We used the anterior skull base surgery questionnaire (ASBS-Q) whose development, reliability, and validity were described elsewhere.2,9 Six relevant domains were identified by factor analysis: role of performance, physical function, vitality, pain, specific symptoms, and impact upon emotions. Internal consistency of each of the six domains was evaluated using Cronbach's α coefficient.
All the questions were constructed to detect differences in QOL between the preoperative and postoperative periods. The answers were given on an ordinal scale with five levels for indicating any QOL change since the presurgical QOL. All the questions had an identical level of importance. For example, question number 8 was: “How would you define your general performance now relative to the period before the operation? (1) Much worse; (2) Slightly worse; (3) No change; (4) Slightly better; (5) Much better.” To help control for response bias, some of the answers ranged from “large improvement” to “large deterioration” or vice versa. The surgical technique, complications, and outcome have been described in detail elsewhere.10
Statistical Methods
Student's t-test, Spearman correlation coefficient, Cronbach's α coefficient, and the Mann–Whitney U-test were applied as appropriate. A probability of less than 0.05 was considered significant. To assess the impact of the various clinical and demographic variables on patient QOL, we used the Ryan-Einot-Gabriel-Welsch multiple-range test that was employed to determine significant differences between pairs of groups. Multiple comparisons for the adjusted means were also performed, using the studentized maximum modulus method.
Results
Seventy patients operated by us were eligible for enrollment in this study. The response rate for completing the questionnaire, after excluding the patients who died, who were lost to follow-up and who were operated <6 months before the study was activated, was 64% (41/64 patients). The demographic characteristics of these patients are shown in Table 1.
Two patients suffered major complications that included meningitis (n = 1) and uniocular visual impairment (n = 1). There were no cases of cerebrospinal fluid leak, or tension pneumocephalus. The study population was divided into subgroups according to age, gender, type of surgery (pituitary, nonpituitary), type of tumor (benign, malignant), primary anatomical area (cribriform, planum, sella, clivus or maxilla) and comorbidity.
We first assessed the reliability of the questionnaire by measuring the reproducibility of pairs of similar questions in each domain. The internal consistency of each domain was evaluated using an α-Cronbach value, and the scores for each domain showed high internal reliability of the questions in each domain (ranging from 0.8 to 0.92, p <0.001) (Table 2).
Table 2. Internal Consistency of the Questionnaire.
| α-Cronbach | Mean | Standard Deviation | |
|---|---|---|---|
| General performance | 0.81 | 2.86 | 0.69 |
| Physical function | 0.9 | 3.03 | 1 |
| Vitality | 0.92 | 2.83 | 0.88 |
| Pain | 0.91 | 3 | 1 |
| Specific symptoms | 0.8 | 2.78 | 0.75 |
| Impact on emotions | 0.88 | 2.97 | 0.89 |
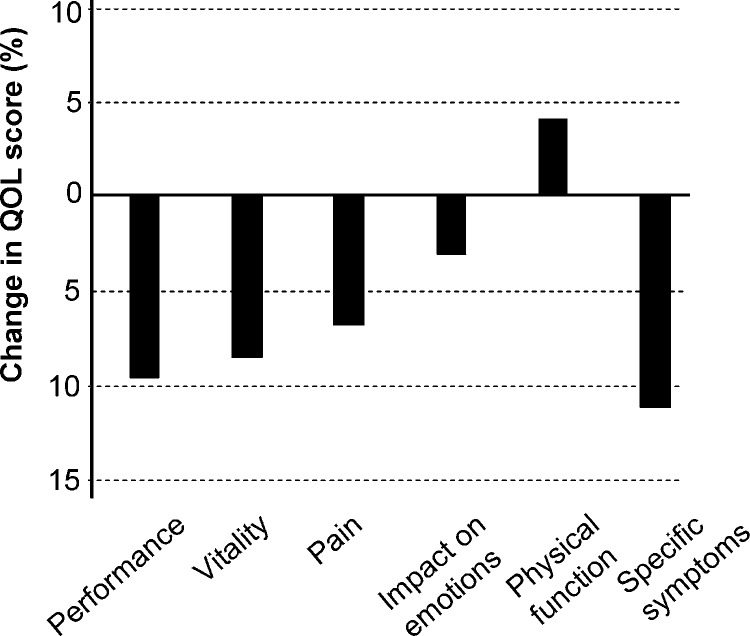
To obtain estimates on the influence of the EEA on various aspects of QOL, each patient was asked to answer 36 questions related to six distinct domains: general performance, physical function, vitality, pain, specific symptoms, and impact on emotions. The results are summarized in Fig. 1. There was a less than 12% reduction in QOL scores in most of the domains and a 4% improvement in the physical function domain.
Figure 1.
The effect of endoscopic surgery on selected quality of life domains. The graph shows changes of scores after surgery (in %), relative to the time prior to the operation.
The study population was further divided into subgroups according to demographic and clinical characteristics to predict which of them may have experienced a deterioration of QOL after surgery (Table 3). The female patients reported significantly lower scores than the males in all domains with the exception of specific symptoms (p <0.01). Whereas the male patients reported an improvement of up to 18% in the general performance, physical function, vitality, pain, and impact on emotions domains, the female patients reported an up to 18 to 32% reduction in those scores. There were no significant differences in the scores of the other subgroups (Table 3). The results of further analysis of any association with the primary resected area (cribriform, planum, sella, clivus and maxilla) and QOL score showed no significant difference in the QOL scores according to the primary area of surgery (data not shown).
Table 3. Association of Demographic and Clinical Variants with Selected Quality of Life Domains.
| Variant | Role of Performance | Physical Function | Vitality | Pain | Specific Symptoms | Impact on Emotions | Overall | |
|---|---|---|---|---|---|---|---|---|
| Total | n = 41 | 2.86 | 3.03 | 2.83 | 2.85 | 2.78 | 2.97 | 2.86 |
| Age (y) | ≤60 | 2.80 | 3.28 | 2.87 | 3.08 | 2.79 | 3.16 | 3.00 |
| >60 | 2.86 | 2.75 | 2.78 | 2.60 | 2.77 | 2.76 | 2.75 | |
| Pathology | Benign | 3.00 | 3.00 | 2.84 | 2.86 | 2.73 | 3.02 | 2.89 |
| Malignant | 2.37 | 3.43 | 3.08 | 3.20 | 3.23 | 3.08 | 3.06 | |
| Months after surgery | 6–12 | 2.7 | 3.04 | 2.90 | 2.89 | 2.71 | 3.00 | 2.87 |
| >12 | 2.4 | 3.02 | 2.79 | 2.83 | 2.72 | 2.96 | 2.79 | |
| Radiotherapy | No | 2.84 | 2.98 | 2.84 | 2.86 | 2.76 | 3.03 | 2.88 |
| Yes | 2.73 | 3.61 | 3.08 | 3.25 | 2.89 | 2.85 | 3.07 | |
| Type of surgery | Nonpituitary | 2.89 | 3.2 | 2.78 | 2.98 | 2.83 | 2.91 | 2.93 |
| Pituitary | 3.01 | 2.84 | 2.92 | 2.73 | 2.72 | 2.88 | 2.85 | |
| Gender | Female | 2.63a | 2.65a | 2.49b | 2.35b | 2.60 | 2.55a | 2.85a |
| Male | 3.06a | 3.34a | 3.15b | 3.30b | 2.94 | 3.34a | 3.2a | |
| Recurrent surgery | No | 2.84 | 2.96 | 2.74 | 2.75 | 2.63 | 2.89 | 2.80 |
| Yes | 2.84 | 3.13 | 2.97 | 3.05 | 2.95 | 3.10 | 3.01 | |
| Comorbidityc | No | 2.89 | 3.09 | 2.81 | 2.87 | 2.76 | 3.01 | 2.90 |
| Yes | 3.04 | 3.36 | 3.35 | 3.55 | 3.04 | 3.33 | 3.28 |
p <0.05.
p <0.01.
Myocardial infarction; chronic lung disease; heart failure, peripheral vascular disease, cerebrovascular accident, liver dysfunction, chronic renal failure, diabetes mellitus, other malignancies.
As for the impact of surgery on the specific symptoms domain, 19 patients (46%) reported that they had impaired sense of smell, 12 (29%) had loss of appetite, 20 (49%) had recurrent nasal secretion, 10 (24%) had epiphora, and 13 (32%) developed visual disturbances as a result of the operation. Fourteen patients (34%) reported that the operation interfered with their social activity, 14 (34%) reported impaired performance at work, 12 (29%) felt limited in their nonprofessional activities since their operation, and 13 (32%) reported that the operation had a deleterious effect on their family life.
Discussion
The effectiveness of endonasal surgical techniques for extirpation of anterior skull base tumors had been established during the past decade, however, there are sparse data on the impact of surgery on the patient's QOL. Surgical procedures for resection of neoplasms of the anterior skull base can carry significant morbidity.11 We had previously found that 44% of the patients are likely to suffer from anosmia following open anterior skull base surgery.12 Other significant factors that influence functional outcome include nasal secretions, mucocele, and visual disturbances.13 In this study, we retrospectively evaluated the influence of endoscopic skull base surgery on patients QOL.
Since the currently available instruments for estimating the QOL in patients with head and neck cancer are not designed for endonasal skull base surgeries, we used a disease-specific instrument initially designed for open anterior skull base surgery which was validated with standard psychometric criteria. The same instrument had been evaluated and validated for application to patients who had undergone endonasal surgery.14
The overall results showed that endoscopic resection of tumors of the anterior and middle skull base preserves health-related QOL measures in most patients. Most of our patients reported that the surgical procedure either improved or did not interfere with their overall QOL. The relatively good scores recorded in the general performance, pain, and specific symptoms domains further demonstrated the moderate negative impact of surgery on different aspects of QOL.
Most of the studies on QOL after anterior skull base surgery were performed on patients operated through open approaches.15 In a recent prospective study, Abergel et al showed that patients undergoing open skull base surgery have reduced QOL scores at 6 months after surgery, and that this was followed by an improvement in their QOL 6 months later.12 In a recent prospective study, Pant et al showed stability of the QOL scores 6 months after endoscopic skull base surgery.14 In agreement with these results, we also found stability of the QOL scores >6 months after surgery (Table 3). Nevertheless, variability in the postoperative period remains an important limitation of our study.
We found differences in QOL scores between male and female patients. It is conceivable that dissimilarity in patients' expectations or distinct coping mechanisms may have contributed to the differences in QOL between the sexes.16 The high internal consistency score within each domain serves to further validate the instrument for use in endoscopic surgery. Unlike our previous results on patients undergoing open skull base surgery, we did not detect significant changes in QOL due to radiation therapy, malignant histology, or age. Pant et al recently used the ASBS-Q instrument for estimating the QOL scores of patients undergoing endoscopic skull base surgery.14 By 3 months after surgery, most of their patients reported a mean score of >4.0 of 5 in most domains. They reported higher scores among patients undergoing a transsellar approach compared with those who underwent nontranssellar approaches. They also noted significant improvement in the sinonasal morbidity score (using the SNOT-22 questionnaire) within the first 6 months after surgery. The effects of sex, pituitary versus nonpituitary tumors, histology, anatomical compartments, or age on QOL were not estimated.
Cronbach's α is commonly used as a measure of the internal consistency and reliability of a test score for a sample of examinees.17 The α score varies from 0 to 1 and a score of 0.70 or higher is considered to be predictive of the reliability of the questionnaire.2 In this study, we found α-Cornbach values of 0.69 to 1 with most values being ≥0.75 for each domain, suggesting a good reliability of the ASBS-Q instrument in studying patients undergoing endoscopic skull base surgery.
Our study involves a group of patients operated by the same group of surgeons. Therefore, our results are applicable to these patients, and generalizing them to define the impact of various other endonasal approaches to the skull base on QOL is not possible. A main limitation of our current study is that it involves a relatively small group of patients with different types of neoplasms. It is conceivable that some of the demographic and clinical variables that were tested here did not reach statistical significance due to the small sample size of our cohort. Further prospective, multicenter studies are required to more accurately assess the QOL characteristics of patients with various anterior skull base tumors who undergo surgical modalities that have no clear survival advantage.18 Without such a level of evidence, one cannot assume a superiority of one surgical procedure over the other. For these reasons, QOL assessments should be included as a regular criteria for assessing the success of treatment, especially when the treatment modality is newly introduced.
Conclusion
The study further validates the use of the ASBS-Q instrument in patients undergoing endoscopic skull base operations. The overall QOL of most patients after endoscopic skull base tumor resection can be classified as good. The questionnaire's items relating to sinonasal morbidity had the worse impact on patients' QOL. Female patients had worse overall QOL scores than males.
Acknowledgments
This research was supported by the Legacy Heritage Biomedical Science Partnership Program of the Israel Science Foundation (No. 1680/08), the Israel Cancer Association (grant donated by Ellen and Emanuel Kronitz in memory of Dr Leon Kronitz, No. 20090068), the Israeli Ministry of Health (No. 3–7355), the Weizmann Institute - Sourasky Medical Center Joint Grant, the Tel Aviv Sourasky Intramural Grant, and by a grant from the US–Israel Binational Science Foundation (No. 2007312) to Z.G. Esther Eshkol is thanked for the editorial assistance.
References
- 1.Gil Z, Fliss D M. Quality of life in patients with skull base tumors: current status and future challenges. Skull Base. 2010;20(1):11–18. doi: 10.1055/s-0029-1242979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Gil Z, Abergel A, Spektor S, Shabtai E, Khafif A, Fliss D M. Development of a cancer-specific anterior skull base quality-of-life questionnaire. J Neurosurg. 2004;100(5):813–819. doi: 10.3171/jns.2004.100.5.0813. [DOI] [PubMed] [Google Scholar]
- 3.Gil Z, Fliss D M. Contemporary management of head and neck cancers. Isr Med Assoc J. 2009;11(5):296–300. [PubMed] [Google Scholar]
- 4.Snyderman C H, Kassam A B, Carrau R, Mintz A. Endoscopic Reconstruction of Cranial Base Defects following Endonasal Skull Base Surgery. Skull Base. 2007;17(1):73–78. doi: 10.1055/s-2006-959337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wasserzug O, Margalit N, Weizman N, Fliss D M, Gil Z. Utility of a three-dimensional endoscopic system in skull base surgery. Skull Base. 2010;20(4):223–228. doi: 10.1055/s-0030-1247630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Witgert M E, Veramonti T, Hanna E. Instruments for estimation of health-related quality of life in patients with skull base neoplasms. Skull Base. 2010;20(1):5–10. doi: 10.1055/s-0029-1242978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hanna E, DeMonte F, Ibrahim S, Roberts D, Levine N, Kupferman M. Endoscopic resection of sinonasal cancers with and without craniotomy: oncologic results. Arch Otolaryngol Head Neck Surg. 2009;135(12):1219–1224. doi: 10.1001/archoto.2009.173. [DOI] [PubMed] [Google Scholar]
- 8.Gil Z, Abergel A, Spektor S. et al. Quality of life following surgery for anterior skull base tumors. Arch Otolaryngol Head Neck Surg. 2003;129(12):1303–1309. doi: 10.1001/archotol.129.12.1303. [DOI] [PubMed] [Google Scholar]
- 9.Gil Z, Abergel A, Spektor S, Khafif A, Fliss D M. Patient, caregiver, and surgeon perceptions of quality of life following anterior skull base surgery. Arch Otolaryngol Head Neck Surg. 2004;130(11):1276–1281. doi: 10.1001/archotol.130.11.1276. [DOI] [PubMed] [Google Scholar]
- 10.Snyderman C H, Kassam A B. Endoscopic techniques for pathology of the anterior cranial fossa and ventral skull base. J Am Coll Surg. 2006;202(3):563. doi: 10.1016/j.jamcollsurg.2005.11.019. [DOI] [PubMed] [Google Scholar]
- 11.Gil Z, Patel S G, Bilsky M, Shah J P, Kraus D H. Complications after craniofacial resection for malignant tumors: are complication trends changing? Otolaryngol Head Neck Surg. 2009;140(2):218–223. doi: 10.1016/j.otohns.2008.10.042. [DOI] [PubMed] [Google Scholar]
- 12.Abergel A, Fliss D M, Margalit N, Gil Z. A prospective evaluation of short-term health-related quality of life in patients undergoing anterior skull base surgery. Skull Base. 2010;20(1):27–33. doi: 10.1055/s-0029-1242982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Gil Z, Fliss D M. Pericranial wrapping of the frontal bone after anterior skull base tumor resection. Plast Reconstr Surg. 2005;116(2):395–398, discussion 399. doi: 10.1097/01.prs.0000172761.65844.d0. [DOI] [PubMed] [Google Scholar]
- 14.Pant H, Bhatki A M, Snyderman C H. et al. Quality of life following endonasal skull base surgery. Skull Base. 2010;20(1):35–40. doi: 10.1055/s-0029-1242983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Palme C E, Irish J C, Gullane P J, Katz M R, Devins G M, Bachar G. Quality of life analysis in patients with anterior skull base neoplasms. Head Neck. 2009;31(10):1326–1334. doi: 10.1002/hed.21102. [DOI] [PubMed] [Google Scholar]
- 16.Symon Z, Daignault S, Symon R, Dunn R L, Sanda M G, Sandler H M. Measuring patients' expectations regarding health-related quality-of-life outcomes associated with prostate cancer surgery or radiotherapy. Urology. 2006;68(6):1224–1229. doi: 10.1016/j.urology.2006.08.1092. [DOI] [PubMed] [Google Scholar]
- 17.Brouwer C N, Schilder A G, Stel H F van. et al. Reliability and validity of functional health status and health-related quality of life questionnaires in children with recurrent acute otitis media. Qual Life Res. 2007;16(8):1357–1373. doi: 10.1007/s11136-007-9242-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Patel S G. Internet-Based Multi-institutional Clinical Research: A New Method to Conduct and Manage Quality of Life Studies. Skull Base. 2010;20(1):23–26. doi: 10.1055/s-0029-1242981. [DOI] [PMC free article] [PubMed] [Google Scholar]