Abstract
The most prominent stigma of supratentorial skull base surgery is the defect caused by wasting of the temporalis muscle by denervation, devascularization, or rotation of the muscle. Any of the above may lead to a unilateral temporal deformity informally referred to patients as “the divot in my head.” Abdominal free fat grafting has been used by surgeons for years to close posterior fossa defects with excellent results. We present our experience using abdominal free fat grafts to improve cosmetic results and to prevent cerebrospinal fluid leaks in supratentorial skull base surgery. The basic technique and its benefits are described.
Keywords: supratentorial skull base surgery, cerebrospinal fluid leak, free fat grafting, dural closure, craniotomy
The most prominent stigma of supratentorial skull base surgery is the deformity caused by wasting of the temporalis muscle that results in a cosmetic defect. Temporal muscle volume loss may be caused by several factors, including: (1) denervation after iatrogenic transection of a division of the mandibular nerve; (2) compromise of the vascular supply; (3) loss of the anatomical insertion site of the temporalis muscle; (4) trauma; (5) tumoral invasion of the muscle; or (6) rotation of the temporalis muscle for use as a vascularized in situ graft.
Abdominal free fat grafting has been described by surgeons as an effective mean to close posterior fossa defects after both retrosigmoid and translabyrinthine craniotomies.1,2,3,4,5 The plastic surgery literature is also ripe with examples of closure techniques that incorporate free fat grafts to enhance the cosmetic result of a variety of their elective and reconstructive procedures.6,7,8 In the discussion that follows, we describe the use of abdominal free fat grafts for correction of cosmetic defects and for prevention of cerebrospinal fluid (CSF) leaks in supratentorial skull base craniotomy.
Methods
Between January 2007 and December 2010, 17 patients required volumetric augmentation and/or closure of CSF leak at the conclusion of supratentorial skull base surgery. In this retrospective series, the indications for abdominal free fat grafting included the following: (1) to fill the defect caused by rotating the temporalis muscle for use as an in situ graft in six patients; (2) for reconstruction after extensive removal of orbital and sphenoid bone in four patients; (3) for volume loss from previous operations in three patients; (4) for primary closure of resected dura in two patients; and (5) for primary volume loss from penetrating trauma in two patients. Mean postoperative follow-up for our patient population was ~9 months, with a range of 6 to 18 months.
Institutional Review Board approval was obtained prior to undertaking this study.
Results
Surgical Technique: Graft Harvesting
The abdomen is prepped and draped in the standard surgical fashion. A curvilinear, periumbilical incision is used. The amount of abdominal free fat harvested for grafting is proportional to the size of the cranial defect plus 30 to 40%, with the radius of the lobule generally ranging from 4 to 8 cm in our patient population. It has been our practice to cut our fat graft into smaller pieces that may be manipulated to plug the bony, dural, or muscular defect created during surgery. We routinely leave a subcutaneous, abdominal Jackson-Pratt drain to prevent the development of a seroma in light of the newly-created dead space. Fig. 1 displays our standard technique for fat graft harvesting.
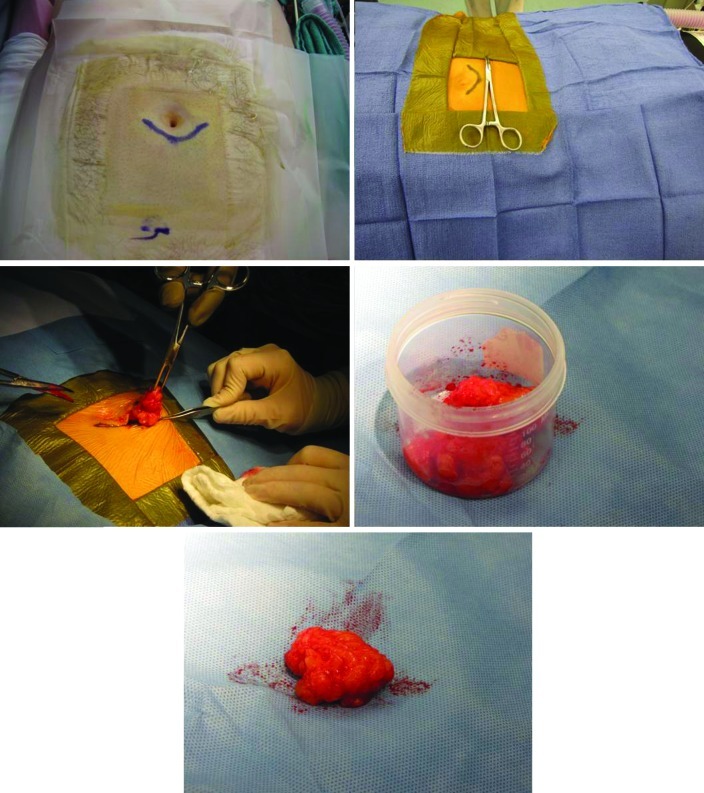
Figure 1.
Shown is a periumbilical incision, separately prepped from the cranial incision (top left/right panel). Fat is harvested according to the amount needed for the reconstruction and then placed in a sterile container for use during closure (middle/bottom panels).
Surgical Technique: Graft Placement
The goal in employing abdominal free fat grafts is to optimize cosmesis while maintaining the functional capacity of the graft as a barrier to prevent CSF leak when primary, water-tight closure of the dura is impossible. When securing the fat graft to a cranial wound, it is critical to make certain that the graft is well-seated and immobilized, and great care is taken to approximate the fascial layer for the express purpose of securing the fat in place. The immobility of the fat graft is not only of particular importance when addressing a CSF leak, but is also not trivial in reconstructing the original contour of the scalp. Fig. 2 shows the dual effectiveness of abdominal free fat in optimizing cosmesis while at the same time preventing CSF leak.
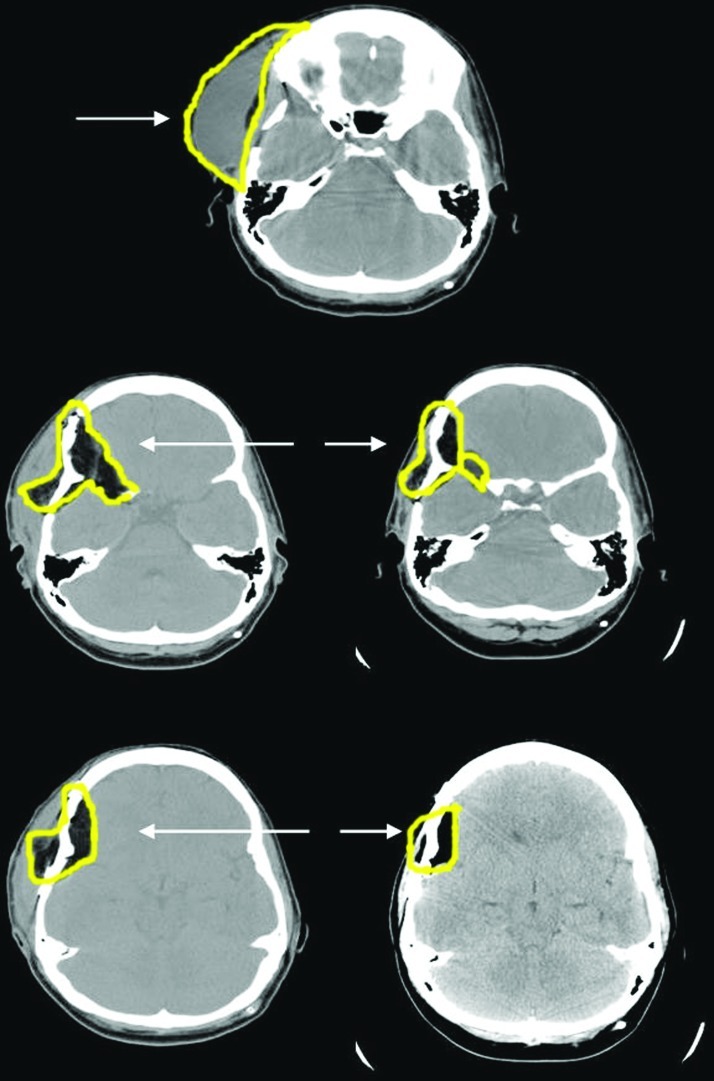
Figure 2.
Top panel shows a computed tomography scan obtained immediately prior to abdominal fat graft repair of cerebrospinal fluid leak. Middle panel images reflect the immediate postoperative period. Bottom panel images are taken 9 months after the surgery and demonstrate the natural reduction in graft size.
We find that middle cranial fossa craniotomies present some of the more challenging defects as they are often “conical” due to drilling of the sphenoid bone. We address these wedge-shaped defects by cutting the fat graft into strips that are first placed deeply into the defect with subsequent strips then draped outward. In addition to replacing the bone flap, we tightly reattach the temporalis muscle in an effort to ensure water-tight closure of the dural repair. We report no postoperative CSF leaks.
The amount of abdominal fat that we harvest and re-implant beneath the cranial incision allows for ~30 to 40% volume-loss postoperatively when implanted in the following locations: (1) over the periorbita, but under the muscle; (2) over the muscle, but under the temporalis fascia or pericranial graft; and (3) between the bone flap and the muscle. We found that the final contour of the head settled between 3 and 6 months after surgery, with one patient requiring liposuction for cosmesis. Figure 3 shows the pre- and postoperative results in a patient with an orbital and soft tissue malignancy reconstructed with the free fat technique. Finally, Fig. 4 shows the effectiveness of abdominal free fat grafting in addressing wounds affected by postoperative radiation therapy.
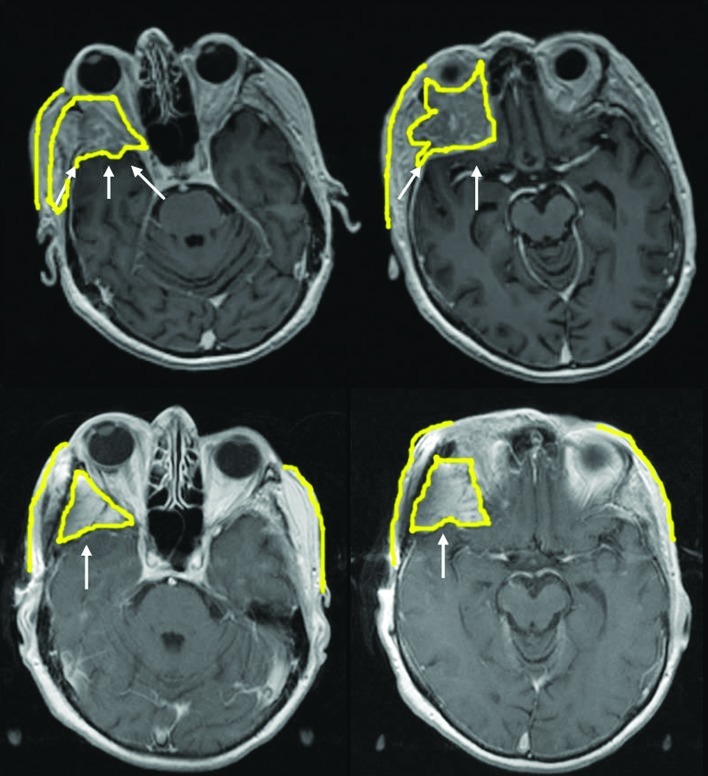
Figure 3.
Top panels show an invasive orbital and soft tissue malignancy. Bottom panels show resected tumor and replacement of bone and soft tissue with free fat graft.
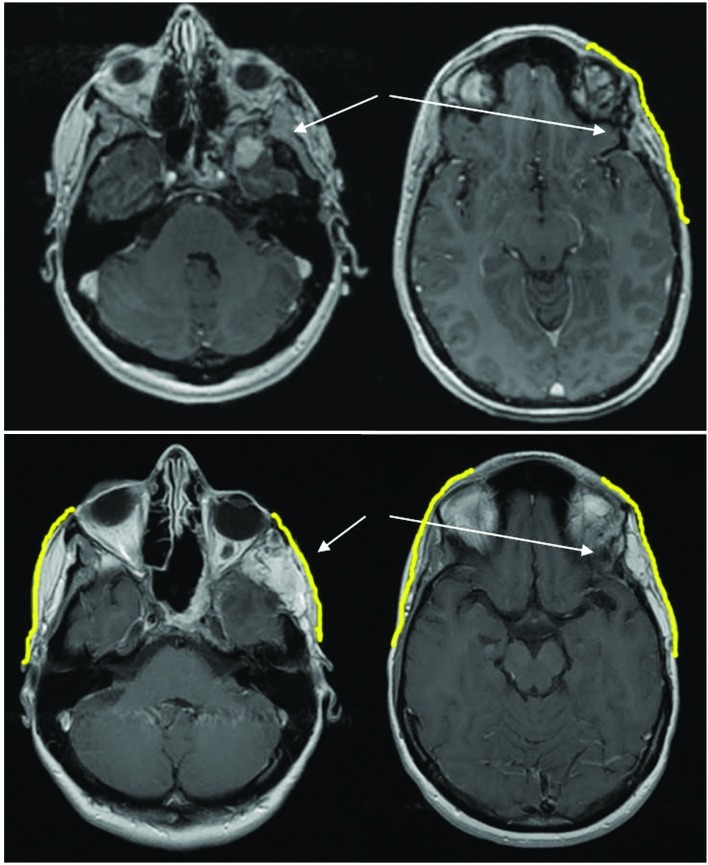
Figure 4.
Patient had prior surgery and radiation for malignant skull base tumor. Top panels shows preoperative temporal soft tissue thinning and recurrent mass on magnetic resonance imaging (MRI). Bottom panels show postoperative placement of free fat graft in the region of the drilled sphenoid bone and temporalis muscle with reconstruction of the natural facial contour on follow-up MRI 6 months after surgery.
Discussion
Abdominal free fat grafting has been widely adopted across multiple surgical disciplines to optimize cosmetic outcomes and to reduce the incidence of CSF leak. Despite many specific indications, abdominal free fat grafting is generally employed to restore volume lost during craniotomy, to create an aesthetically appealing temporal contour, or to plug CSF leaks associated with irreparable dural defects.3,4,5 Many of the benefits of the free fat graft technique, including its long-term durability, appear to be associated with the revascularization of the transplanted fat graft over time.
We find abdominal free fat to be a plentiful source of autologous, malleable tissue amenable to molding into irregularly shaped defects–compliance not afforded to the surgeon by synthetic implants. The risk of graft rejection after autologous tissue transplantation is exceedingly low, as is the risk of postoperative infection. According to one 10-year clinical series, customized titanium mesh had a postoperative infection rate of 2.6%, and other series published in the ophthalmology and facial reconstruction literature describe slightly lower infection rates when using porous polyethylene implants.9,10,11 Infection after abdominal fat grafting, however, is an extremely rare occurrence.12,13 We report no postoperative infections in our series.
It is important to consider also that fat grafts do not create artifact or obscure visualization of the skull base when a patient's underlying pathology necessitates serial postoperative surveillance imaging. This benefit of fat grafting can be invaluable in cases of skull base tumors.
In addition, abdominal free fat grafting is fiscally prudent. Of late, medical technology companies have introduced an array of synthetic products that may serve as surgical implants, either for improved cosmesis or for dural repair or prevention of CSF leak, and has prompted the publication of numerous studies reviewing the various materials.14,15,16,17,18 At our institution, patients who undergo implantation of a pterional polyethylene bone graft incur an additional $600 in operative cost; whereas 10 g of bone cement adds nearly $2500, and customizable titanium mesh implants cost upwards of $3500. Abdominal free fat grafting, by contrast, offers a simple, low-cost, and effective mean to augment operative closure which may be utilized across all socioeconomic strata.
Conclusion
Abdominal free fat provides surgeons with a plentiful source of malleable, autologous material by which to enhance the cosmesis of supratentorial skull base closures while also serving as a cost-effective, reliable plug by which to prevent CSF leaks. The incidence of infection or graft rejection is low, and fat grafting maintains the integrity of postoperative surveillance imaging without focal obscuration of the surrounding tissues by streak artifact. Based on our experience, we anticipate broadening our indications for the use of abdominal free fat grafting in bolstering the closure of supratentorial skull base craniotomies.
References
- 1.Yuen H W, Chen J M. Reconstructive options for skull defects following translabyrinthine surgery for vestibular schwannomas. Curr Opin Otolaryngol Head Neck Surg. 2008;16(4):318–324. doi: 10.1097/MOO.0b013e32830139b8. [DOI] [PubMed] [Google Scholar]
- 2.Smith P G, Leonetti J P, Grubb R L. Management of cerebrospinal fluid otorhinorrhea complicating the retrosigmoid approach to the cerebellopontine angle. Am J Otol. 1990;11(3):178–180. [PubMed] [Google Scholar]
- 3.House J L, Hitselberger W E, House W F. Wound closure and cerebrospinal fluid leak after translabyrinthine surgery. Am J Otol. 1982;4(2):126–128. [PubMed] [Google Scholar]
- 4.Wiet R J, Mamikoglu B, Hoistad D, Battista R. A technique to prevent cerebrospinal fluid leakage after translabyrinthine approach. Laryngoscope. 2000;110(7):1234–1236. doi: 10.1097/00005537-200007000-00032. [DOI] [PubMed] [Google Scholar]
- 5.Black P. Cerebrospinal fluid leaks following spinal or posterior fossa surgery: use of fat grafts for prevention and repair. Neurosurg Focus. 2000;9(1):e4. doi: 10.3171/foc.2000.9.1.4. [DOI] [PubMed] [Google Scholar]
- 6.Baumann D, Skoracki R, Hanasono M. Improving Aesthetic Outcomes in Head and Neck Reconstruction With Structural Fat Grafting. Plast Reconstr Surg. 2010;126:721. [Google Scholar]
- 7.Mizuno H, Hyakusoku H. Fat grafting to the breast and adipose-derived stem cells: recent scientific consensus and controversy. Aesthet Surg J. 2010;30(3):381–387. doi: 10.1177/1090820X10373063. [DOI] [PubMed] [Google Scholar]
- 8.Fulton J E, Parastouk N. Fat grafting. Dermatol Clin. 2001;19(3):523–530, ix. doi: 10.1016/s0733-8635(05)70292-8. [DOI] [PubMed] [Google Scholar]
- 9.Matsuno A, Tanaka H, Iwamuro H. et al. Analyses of the factors influencing bone graft infection after delayed cranioplasty. Acta Neurochir (Wien) 2006;148(5):535–540, discussion 540. doi: 10.1007/s00701-006-0740-6. [DOI] [PubMed] [Google Scholar]
- 10.Romano J J, Iliff N T, Manson P N. Use of Medpor porous polyethylene implants in 140 patients with facial fractures. J Craniofac Surg. 1993;4(3):142–147. doi: 10.1097/00001665-199307000-00007. [DOI] [PubMed] [Google Scholar]
- 11.Liu J K, Gottfried O N, Cole C D, Dougherty W R, Couldwell W T. Porous polyethylene implant for cranioplasty and skull base reconstruction. Neurosurg Focus. 2004;16(3):ECP1. doi: 10.3171/foc.2004.16.3.14. [DOI] [PubMed] [Google Scholar]
- 12.Goddard J C, Oliver E R, Lambert P R. Prevention of cerebrospinal fluid leak after translabyrinthine resection of vestibular schwannoma. Otol Neurotol. 2010;31(3):473–477. doi: 10.1097/MAO.0b013e3181cdd8fc. [DOI] [PubMed] [Google Scholar]
- 13.Merkus P, Taibah A, Sequino G, Sanna M. Less than 1% cerebrospinal fluid leakage in 1,803 translabyrinthine vestibular schwannoma surgery cases. Otol Neurotol. 2010;31(2):276–283. doi: 10.1097/MAO.0b013e3181cc06ad. [DOI] [PubMed] [Google Scholar]
- 14.Kveton J F, Friedman C D, Costantino P D. Indications for hydroxyapatite cement reconstruction in lateral skull base surgery. Am J Otol. 1995;16(4):465–469. [PubMed] [Google Scholar]
- 15.Luginbuhl A J, Campbell P G, Evans J, Rosen M. Endoscopic repair of high-flow cranial base defects using a bilayer button. Laryngoscope. 2010;120(5):876–880. doi: 10.1002/lary.20861. [DOI] [PubMed] [Google Scholar]
- 16.Litvack Z N, West G A, Delashaw J B, Burchiel K J, Anderson V C. Dural augmentation: part I-evaluation of collagen matrix allografts for dural defect after craniotomy. Neurosurgery. 2009;65(5):890–897, discussion 897. doi: 10.1227/01.NEU.0000356970.22315.BC. [DOI] [PubMed] [Google Scholar]
- 17.Cosgrove G R, Delashaw J B, Grotenhuis J A. et al. Safety and efficacy of a novel polyethylene glycol hydrogel sealant for watertight dural repair. J Neurosurg. 2007;106(1):52–58. doi: 10.3171/jns.2007.106.1.52. [DOI] [PubMed] [Google Scholar]
- 18.Dusick J R, Mattozo C A, Esposito F, Kelly D F. BioGlue for prevention of postoperative cerebrospinal fluid leaks in transsphenoidal surgery: A case series. Surg Neurol. 2006;66(4):371–376, discussion 376. doi: 10.1016/j.surneu.2006.06.043. [DOI] [PubMed] [Google Scholar]