Abstract
Background:
The purpose of this study is to retrospectively review our experience with stent-assisted embolization of patients with an acutely ruptured cerebral aneurysm.
Methods:
Medical records and imaging were reviewed for 36 patients who underwent stent-assisted embolization of a ruptured cerebral aneurysm.
Results:
Seventeen patients (47%) received a preprocedural loading dose of clopidogrel and five patients (14%) received an intraprocedural dose of clopidogrel. The remaining 14 patients (36%) were treated with antiplatelet therapy following the procedure. Six (17%) stent related intraprocedural thromboembolic complications were encountered; four of these resolved (one partial, three complete) following treatment with abciximab and/or heparin during the procedure. Five of the six thromboembolic events occurred in patients who were not pretreated with clopidogrel (P = 0.043). Two patients in this series (6%) had a permanent thrombotic complication resulting in mild hemiparesis in one patient, and hemianopsia in the second. No procedure related hemorrhagic complications occurred in any patient. One patient had a spontaneous parenchymal hemorrhage contralateral to the treated aneurysm discovered 10 days after treatment. Twenty-eight patients (78%) had a Glasgow Outcome Score of 4 or better at discharge. Seven of 21 patients (33%) with angiographic follow-up required further treatment of the coiled aneurysm.
Conclusion:
Stent-assisted coil embolization is an option for treatment of ruptured wide neck ruptured aneurysms and for salvage treatment during unassisted embolization of ruptured aneurysms but complications and retreatment rates are higher than for routine clipping or coiling of cerebral aneurysms. Pretreatment with clopidogrel appears effective in reducing thrombotic complications without significant increasing risk of hemorrhagic complications.
Keywords: Cerebral aneurysm, coil, embolization, stent, stroke subarachnoid hemorrhage
INTRODUCTION
Endovascular embolization of intracranial aneurysms has emerged as a viable and sometimes preferable method of treatment of intracranial aneurysms as demonstrated in the International Subarachnoid Aneurysm Trial (ISAT).[10] However, endovascular treatment of wide-necked aneurysms continues to pose a challenge to interventionalists.[14] While the development of intracranial stents has enhanced treatment of wide-necked aneurysms, there is reluctance to use this technology during the acute posthemorrhage period. This reluctance stems mainly from the risk of thromboembolic complications associated with using stents in patients who are not pretreated with antiplatelet therapy, and the fear that use of antiplatelet agents in the postrupture period may increase the risk of re-hemorrhage or periprocedural complications related to placement of ventriculostomies.[20] Balloon remodeling has provided an alternative to intracranial stents especially since it can be used without antiplatelet therapy.[4,11] However, there is a concern that balloon remodeling is not always the ideal choice of treatment for all wide necked aneurysms.[3,5,17]
The purpose of this study is to report on our series of ruptured intracranial aneurysms that were treated with stent-assisted coil embolization. Special emphasis will be given to the timing of treatment, use of antiplatelet therapy, periprocedural complications including iatrogenic rupture and thromboembolism, and neurological outcome.
MATERIALS AND METHODS
The neurointerventional database was screened for patients presenting with subarachnoid hemorrhage (SAH) who were treated with stent-assisted coil embolization during the same hospitalization at two high volume centers between 2003 and 2010. Inclusion criteria for these patients were as follows: the presence of acute SAH on CT (hyperdensity in the basal cisterns), and stent-assisted embolization or re-embolization within 7 days of the initial hemorrhage. Exclusion criteria included: evidence of brain death on admission, previously treated aneurysm, evidence of dissecting aneurysm or pseudoaneurysm, and contraindication to antiplatelet therapy. Data were collected from electronic charts, physical charts, and angiography. All protocols were reviewed and approved by the Institutional Review Board of both centers independently. Nineteen of the patients in this study were also included in a larger more generalized series of patients undergoing stent-assisted embolization of cerebral aneurysms.[8]
Preprocedural and demographic data collection consisted of the following: age, sex, Hunt Hess grade, Fisher grade, focal neurological deficits on admission, and presence of ventriculostomy prior to treatment. All time related data were recorded in reference to the day of SAH including timing of admission to the hospital, timing of ventriculostomy placement, timing of antiplatelet treatment, and timing of aneurysm treatment(s). Aneurysm characteristics were recorded from the angiogram or the three-dimensional reconstructions including: location, size of dome, and size of neck. A dome-to-neck ratio was calculated. The dome diameter chosen for this measurement was the largest two-dimensional diameter, which could be used for sizing of the initial framing coil. The type of Neuroform stent (Boston Scientific, Freemont CA) used was also recorded. The efficacy of embolization was classified as follows per previous publication:[16] (1) complete embolization, (2) residual neck, and (3) opacification of sac. Any intraprocedural complications related to embolization of the aneurysm were recorded including thrombus formation in parent vessel, stent migration, iatrogenic rupture, and parent vessel dissection or vasospasm. In addition, if the stent was placed after initial unassisted embolization, it was defined as a salvage procedure and the reason for placement of the stent (e.g., instability of coil pack) was noted.
Medical records were carefully screened for any evidence of postoperative complications including those related to thrombotic events, antiplatelet therapy, vasospasm, and complications related to invasive procedures such as placement of ventriculostomy or ventriculoperitoneal shunts. Glasgow Outcome Score (GOS) at the time of discharge was extracted from the medical record as well as disposition. Follow-up angiography was reviewed when available to evaluate for recurrent residual aneurysm when available. Long-term angiographic outcome was classified as follows: (1) no residual aneurysm; (2) residual neck measuring <3 mm; (3) residual neck measuring >3 mm; and (4) recurrent residual filling of dome.
The one-way Fisher Exact Test was used to evaluate the association between use antiplatelet therapy with the incidence of intraprocedural thrombotic events.
RESULTS
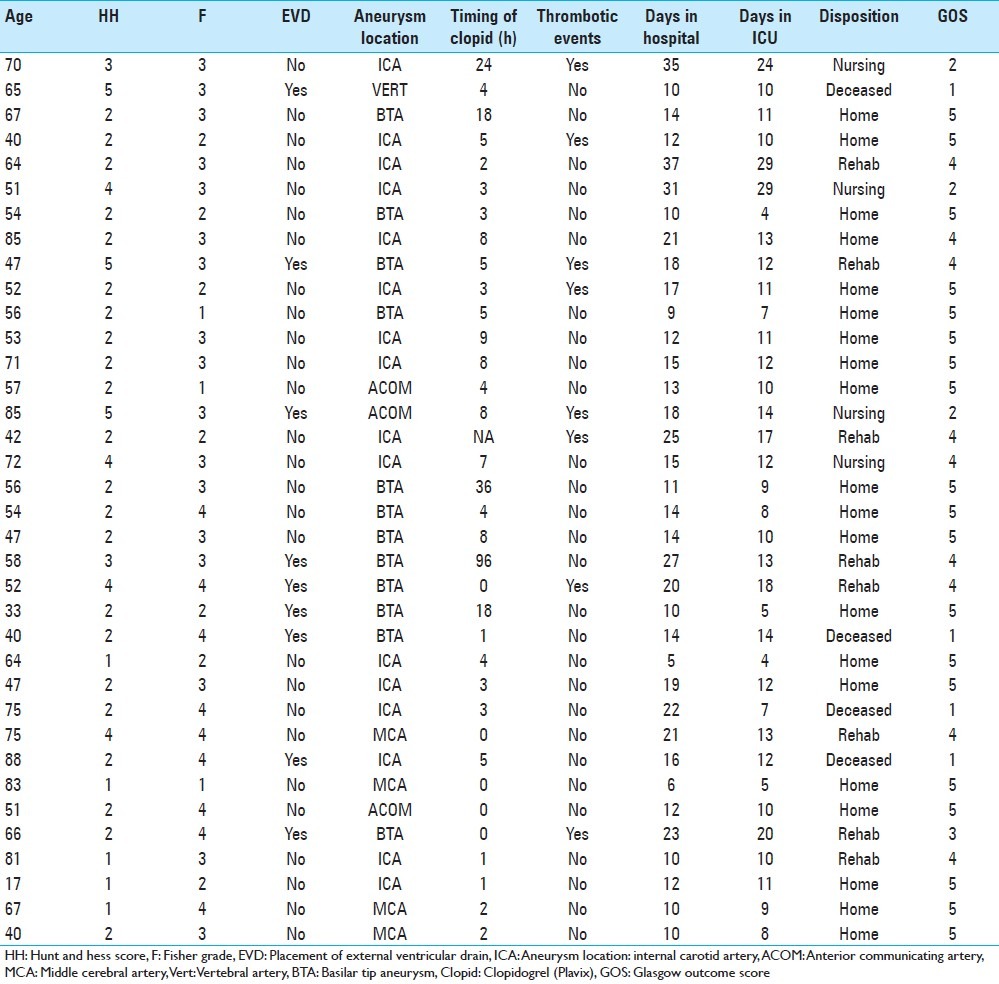
Thirty-six patients were identified who met the inclusion criteria above [Table 1]. The average age of these patients was 59, and the range was 33-88. The average time of presentation after the SAH was 2 days (range, 0–7). The median Hunt Hess score was 2 (range, 1–5), and the median Fisher grade was 3 (range, 1–4) [Table 1]. Twenty-three patients were treated for aneurysms in the anterior circulation. The majority of these aneurysms were sidewall postclinoid ICA aneurysms (N = 16) and three patients were treated for aneurysms located in the anterior communicating complex. Four patients were treated for ruptured middle cerebral artery aneurysms. Only one patient was treated for an aneurysm of the vertebral artery. The remaining 12 patients had basilar apex aneurysms. Nearly all of the aneurysms treated had a dome-to-neck ratio less than 1.5 (N = 32, mean ratio 1.1, and range 0.8–1.47). The remaining four patients had a neck size greater than 4 mm. Nine patients underwent placement of ventriculostomy prior to embolization and antiplatelet therapy.
Table 1.
Patient characteristics and outcomes
Average timing of stent placement for embolization was 3.2 days after the initial hemorrhage (range, 1–7). There were two treatment failures in which a stent was placed, but the aneurysm was not coiled. One of these patients had complete thrombosis of the ICA (see later section). The other patient had an aneurysm which could not be accessed with a microcatheter after stent placement. Ten patients were treated in a staged fashion with initial placement of stent followed by coil embolization (N = 1) or initial subtotal embolization of dome followed by definitive stent embolization (N = 9, see Case #1). (All staged embolizations were completed during the acute phase of hospitalization.) The former patient had a distal thrombotic event after stent placement. Although the flow was partially re-established in this vessel using mechanical disruption of the thrombus, treatment of the aneurysm was postponed to minimize the risk of re-occlusion. This latter group includes a patient who initially failed balloon-assisted embolization. Thirteen patients underwent stent placement as a salvage procedure for complications associated with unassisted coiling of the ruptured aneurysm (see Case #2). (All salvage embolizations were completed in the same setting as unassisted embolization). The reason for salvage stenting included protrusion of the coil mass out of the neck of the aneurysm (N = 7), inability to obtain purchase within the aneurysm due to the small size or tortuosity of the parent vessel (N = 4), stagnant flow in a distal branch following embolization of an anterior communicating artery aneurysm (N = 1), and a combination of coil pack protrusion through the neck of the aneurysm and thrombus formation at the origin of distal vessels (N = 1) [Figure 1].
Figure 1.
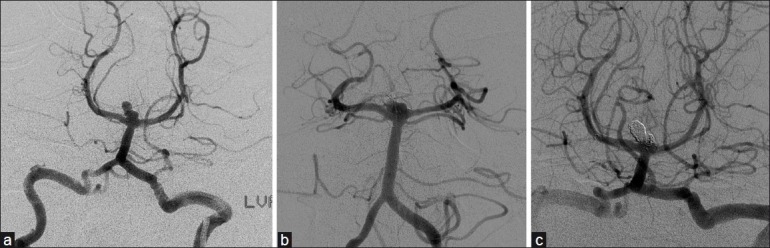
Illustrative case of a basilar tip aneurysm treated via staged embolization. (a) Digital subtraction angiography (DSA) showing a basilar tip aneurysm with a lobule extending from the dome. (b) DSA showing coil embolization of lobule as stage 1. (c) DSA showing stent-assisted embolization of the remainder of the aneurysm once the patient has been pretreated with clopidogrel
Seventeen patients were pretreated with aspirin and clopidogrel prior to their procedure. There was no consensus about the timing of antiplatelet therapy; therefore, this varied depending on the case and the preference of the responsible practitioner. Ten of these patients were treated with a loading dose of clopidogrel (300 mg), an average of 8.5 h prior to deployment of the stent (range, 1–36 h). One patient began antiplatelet therapy (daily clopidogrel 75 mg and aspirin 81 mg) after initial embolization of the dome of the aneurysm and 4 days prior to definitive stent-assisted embolization. Five patients received an intraoperative loading dose of clopidogrel during the procedure. Fourteen patients were treated with antiplatelet therapy an average of 4.9 h after stent embolization of their aneurysm (range, 1–9). All but one patient received intravenous heparin during stent placement. The average dose of heparin was 5250 (range, 2000–8000).
The majority of patients had total or near total embolization of the aneurysm on postprocedural arteriography. Seven patients (30%) had a class 1 result (no residual filling of the aneurysm). Another seven patients (30%) had residual filling of neck (class 2 result). Seven patients (30%) also had residual filling of the dome of the aneurysm (class 3 result) although six of these had significant stagnation of contrast within the dome. Two (9%) aneurysms were left untreated in this series. One of these aneurysm cases involved thrombosis of the ICA as described below. The other aneurysm (carotid-ophthalmic) could not be accessed with a microcatheter through the interstices of the stent due to the tortuosity of the carotid siphon and the small height of the aneurysm (3 mm).
Six patients (17%) experienced thrombotic events associated with stent embolization of the ruptured aneurysm. Two patients had nonocclusive thrombus formation at the neck of the aneurysm. One of these was treated with intra-arterial abciximab (2 mg) and intravenous abciximab (0.25 mg/kg) resulting in partial resolution on follow-up arteriography. The other was treated with intravenous abciximab (0.25 mg/kg) with complete resolution on follow-up arteriography. One patient was found to have a nonocclusive embolus distal to the aneurysm with some evidence of migration. This was treated with an intravenous bolus of heparin (2000 units) resulting in complete resolution. Two patients had evidence of complete carotid occlusion. One of these patients was treated with abciximab (2 mg intra-arterial, 0.25 mg/kg intravenous bolus followed by infusion) resulting in partial recanalization and distal flow. The other patient was not treated with abciximab because the aneurysm was not secured and there was excellent collateral blood supply across the anterior communicating artery. One patient had complete occlusion of the posterior cerebral artery (PCA) after placement of a stent across the neck of the aneurysm. Although flow was re-established by passing the microcatheter through the stent, the distal PCA remained occluded. Abciximab was not administered because the aneurysm was not secured.
The prevalence of thrombotic events increased based on the timing of administration of antiplatelet (P = 0.043). Six percent of patients pretreated with clopidogrel experienced a thrombotic event and 20% of patients treated with clopidogrel during the procedure experienced a thrombotic event. The prevalence of thrombotic events in patients who received clopidogrel after the procedure was 29%.
There was no evidence of intraprocedural rupture during treatment of any patient. Two patients had thromboembolic complications not associated with stenting. One of these is a patient who underwent placement of a Y-stent as a salvage procedure for thrombus at the neck of the aneurysm after coiling. The thrombus resolved after deployment of the two stents without any use of abciximab. In addition, there was no evidence of distal embolus. The other patient had evidence of thrombus formation at the neck of an anterior communicating artery aneurysm, which was coiled after stent-assisted embolization of an ICA aneurysm. This patient also received IV abciximab bolus (0.25 mg/kg) with interval resolution of the thrombus on follow-up arteriography [Figure 2].
Figure 2.

Illustrative case of a basilar tip aneurysm requiring salvage stent placement following unassisted embolization complicated by coil migrations and thrombus formation. (a) DSA of basilar tip aneurysm prior to embolization. (b) DSA of initial unassisted embolization complicated by coil migration of thrombus formation along the origin of the left posterior cerebral artery. (c) DSA following salvage Y-stent placement and complete embolization of aneurysm
Of the six patients described above who had intraprocedural stent-related thrombotic complication, three patients had evidence of ischemia after the procedure. Two of these patients had complete occlusion of the ICA and one had complete occlusion of the PCA. The patient who was treated with abciximab with partial recanalization had mild-to-moderate contralateral hemiparesis postoperatively. The patient's hemiparesis improved during the hospital course until the patient suffered a contralateral intraparenchymal hemorrhage 10 days after the procedure. Angiography at this time did not reveal any evidence of thromboembolism. The second patient had good evidence of collateral circulation from the contralateral ICA. Postoperatively, the patient had evidence of a watershed infarct on CT but was neurologically intact. Another two patients, who had no evidence of intraprocedural thromboembolism, had small areas of diffusion restriction on postoperative MRI, which were of no neurological consequence. Only one patient had evidence of severe SAH-related vasospasm resulting in a hemispheric stroke.
The median GOS for patients at the time of discharge was 5, and 28 patients (78%) had a GOS of 4 or better. Average number of days in the hospital was 16 days (range, 9–37) and average number of days in ICU was 12 days (range, 4–29). Seven patients had a GOS of 2 or less. Two of these patients presented with a Hunt Hess grade 5 SAH and failed to make a neurological improvement during their hospital course. A third patient who initially presented with a Hunt Hess grade 4 SAH suffered a severe hemispheric stroke related to vasospasm. All patients who suffered intraprocedural thromboembolic complications had a GOS of 4 or better at discharge with the exception of the patient described above who suffered an intraparenchymal hemorrhage contralateral to the side of the treated aneurysm. A total of 12 ventriculostomy procedures (including placement of ventriculoperitoneal shunts) were completed in nine patients while they were treated with aspirin and clopidogrel. All patients received preprocedural platelet infusion and no patients suffered any hemorrhagic or thromboembolic complications. Routine CT scans were not completed after removal of drains; therefore, subclinical hemorrhages may not have been identified.
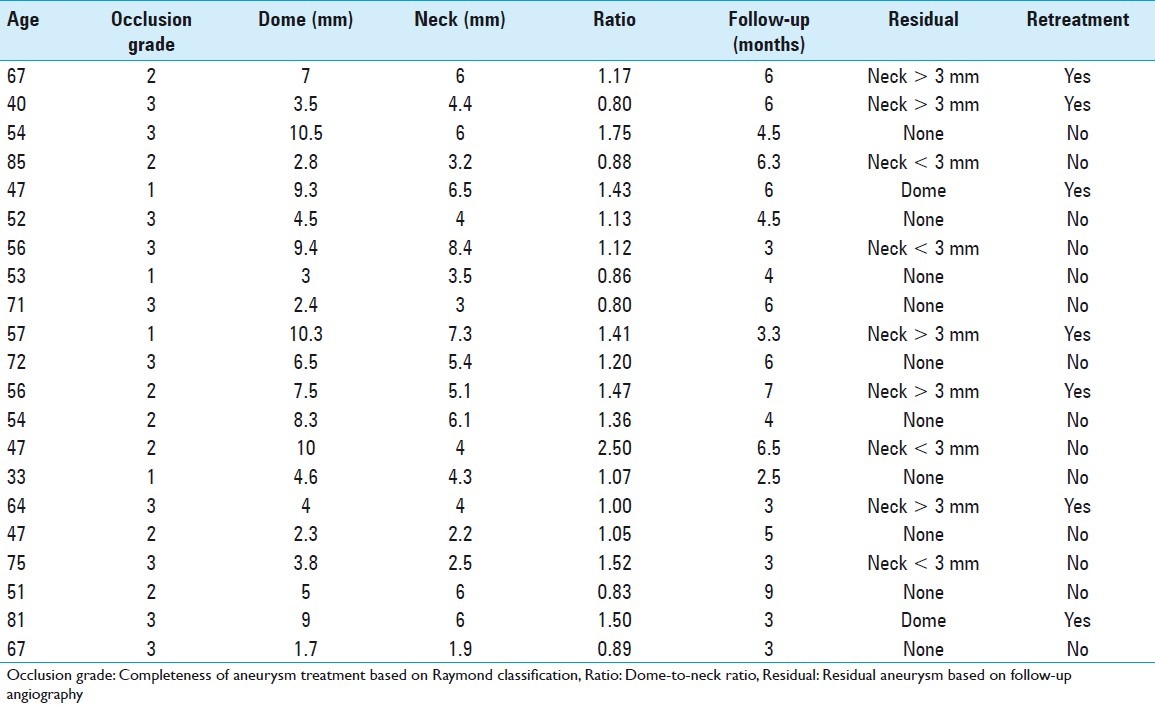
Follow-up angiographic data were available for 21 patients [Table 2]. Mean time to follow-up was 4.8 months (range, 2.5–9). Ten patients (48%) had no evidence of residual aneurysm and four patients (19%) had a residual neck measuring less than 3 mm and required no further embolization. Five (24%) patients had residual filling of the neck of the aneurysm measuring greater than 3 mm. All of these patients underwent successful re-embolization. Two patients (10%) had recanalization of the dome of the aneurysm and also underwent re-embolization.
Table 2.
Treatment efficacy and recurrence
DISCUSSION
Although stent-assisted embolization is a viable option for treatment of ruptured aneurysms, it is typically used only when other alternatives for the treatment of the aneurysm have been excluded or when patient or aneurysm factors change the usual treatment algorithm. Furthermore, stents can be used in salvage procedures in which nonassisted embolization or balloon-assisted embolization have either failed to adequately secure the aneurysm or have resulted in instability of the coil pack with or without thrombus formation in the parent vessel. Using stent-assisted embolization for treatment of ruptured aneurysms has lacked much enthusiasm due to the concern for hemorrhagic complications associated with the use of antiplatelet agents during the acute period and thromboembolic complications associated with the stent placement in the absence of antiplatelet agents. This study reviews our experience of the complications associated with stent-assisted embolization of ruptured intracranial aneurysms.
Thromboembolic events
In our case series, six patients (17%) did experience thrombotic complications during treatment associated with stent embolization of the ruptured aneurysm. Only one of these was in a patient who had preprocedure clopidogrel dosing, suggesting that preoperative treatment with clopidogrel may decrease intraoperative thromboembolic events in this patient population. Other factors may also have contributed to these events. Patient #1 had a large (14 mm) aneurysm and was treated with a first generation Neuroform stent. Although there are no studies measuring the radial force of the various Neuroform stents, the hybrid closed/open cell technology in the Neuroform 3 stent likely increases the radial force of the stent making it more resistant to collapse. Another patient with parent vessel occlusion had significant vasospasm in the carotid artery proximal to the stent. The stagnant antegrade flow likely contributed to in-stent thrombosis. One of our patients with a basilar tip aneurysm had a single stent used from the basilar artery into the PCA. Following embolization of the aneurysm, thrombus was noted at the origin of the unprotected PCA. We have since adopted more routine use of the Y-stent method, which allows protection of both PCAs during embolization of a basilar tip aneurysm. Lastly, two patients with thromboembolic events were initially treated with a subtherapeutic dose of heparin. Although we typically withhold heparin prophylaxis until the aneurysm is at least partially secured with one to two coils, we pretreated most of the patients in this series with heparin due to the risks of thromboembolism associated with use of a stent. However, our initial heparin dose was subtherapeutic (<5000 units) in seven patients.
Benitez et al. also initially withheld heparin when treating ruptured aneurysms and did not report any intraoperative thrombotic events in their series.[2] However, they did report neurological deficits in three of their patients during the postoperative course. Using a similar protocol, Tahtinen et al. reported thromboembolic complications in only 7 of 61 patients.[18] It is unclear from their article if the incident of these thromboembolic complications was higher in the patients who were not pretreated with acetylsalicylic acid (30% of their cohort). Katsaridis et al. reported a series of 44 patients (33 with SAH) who were treated with stent-assisted embolization; only one of the patients in this series had evidence of thromboembolism.[7] Not only were these patients aggressively anticoagulated with heparin at the start of the treatment, but anticoagulation was continued after the procedure for 3 days while the patient was being treated with aspirin and clopidogrel. Although low molecular weight heparin can be used to bridge the period between stent-assisted coiling and therapeutic levels of clopidogrel, the risk of hemorrhagic complications may be increased when both aspects of the clotting cascade are inhibited. Katsaridis et al. do not report on hemorrhagic complications; however, they do highlight the fact that heparin is more readily reversible than antiplatelet therapy.
In our series, four of the six thromboembolic events either improved or resolved with treatment during the procedure. One of the cases included a small filling defect distal to the stent, which resolved when the patient received a second dose of heparin. Two cases completely resolved with administration of abciximab. Lastly, one case of complete parent vessel embolization was treated with abciximab resulting in partial recanalization of the vessel. Recanalization was incomplete in part due to compression of the stent by the coil pack. None of these patients had evidence of aneurysm recanalization or rupture. Similar experiences with abciximab have been reported in other studies with complete resolution in 14–68% of patients and partial recanalization in 39–60% of patients.[1,6,12,15] Two of our patients had complete occlusion of the parent vessel following deployment of the stent but prior to treatment of the aneurysm. We decided not to attempt the recanalization of this vessel for two reasons: (1) administration of abciximab into an unsecured aneurysm would increase the risk of rupture; and (2) one of the patients with ICA occlusion had excellent collateral circulation from the contralateral side. Fortunately, that patient did not have any neurological deficits after the procedure and had only mild evidence of hypodensity in a watershed distribution on CT.
Hemorrhagic complications
The significant hemorrhagic complications of concern are the risk of aneurysm rupture prior to endovascular treatment or hemorrhagic complications from procedures such as external ventricular drain placement. However, a recent review of the patients in the ISAT trial did not show a significant difference in the outcome between those treated with intraoperative antiplatelet therapy or those not treated.[21] Unfortunately, these data cannot be broadly extrapolated because only two centers treated patients with clopidogrel while the other centers treated with salicylates. Benitez et al. described a series of patients treated with stent-assisted embolization including 16 patients with ruptured aneurysms.[2] Due to concern over intraprocedural aneurysm rupture, patients received a loading dose of clopidogrel during the procedure via nasogastric tubes, and they do not report any cases of intraprocedural aneurysm rupture. The only series to report preprocedures of antiplatelet therapy includes 61 patients with SAH in whom 70% were treated with an infusion of acetylsalicylic acid prior to embolization.[18] They report periprocedural aneurysm perforation in four cases but do not mention if these occurred in patients who received antiplatelet therapy.
None of the patients in our series had any evidence of re-rupture despite pretreatment with clopidogrel (N = 17) and intraprocedural treatment with abciximab (N = 3). Our data indicate that the risk of aneurysm re-rupture is relatively small when a clopidogrel load is administered within hours of embolization. Many studies have reported on the use of abciximab in the treatment of thromboembolic complications in patients with ruptured aneurysms, and only two of these case series report evidence intraprocedural rupture.[1,6,12,15] Aviv et al. reported one case of intraprocedural rupture in a series of 13 patients.[1] This complication occurred when the interventionalist attempted to repack the aneurysm with more coils after treatment with abciximab. It is difficult to assert if this complication occurred because the aneurysm was only partially treated or because the aneurysm was manipulated after treatment with abciximab. Park et al. reported three cases in which patients had evidence of increased SAH on postoperative CT following treatment of thromboembolic complications with intra-arterial abciximab.[12] All three patients had complete embolization of the aneurysm prior to treatment with abciximab, and none had evidence of extravasation during the procedure. Based on these data, one can surmise that there was recanalization of the aneurysm at some points following treatment with abciximab resulting in re-rupture. The route of administration may have increased the risk of recanalization in these patients. However, because the risk on aneurysm recanalization does exist, one must carefully weigh the risks and benefits of using abciximab when encountering a thromboembolic event particularly in patients with ruptured aneurysms. It is for this reason that we did not use abciximab to treat the thrombotic complication in patient 16 and 32 who had thrombosis of the parent vessel prior to deployment of coils into the aneurysm.
Antiplatelet agents may also increase hemorrhagic complications during the postoperative period. Tumialan et al. reported six hemorrhagic complications in patients with SAH who were treated with clopidogrel during their hospital course.[20] However, only three of these were related to placement or exchange of a ventricular catheter and only one of these patients received a preprocedural platelet infusion. In contrast, none of the patients in our series experienced hemorrhagic complications related to placement or exchange or a ventricular catheter. The lack of such hemorrhagic complications is likely related to periprocedural infusion of platelets and similar findings are reported in other case series.[18] One of the patients in this series did have an intracerebral hemorrhage during the postoperative course. Although this patient was on clopidogrel and also received an intraoperative dose of abciximab, the fact that this hemorrhage occurred 10 days after treatment and was located contralateral to the aneurysm decreases the likelihood that it was related to aneurismal rupture. Given that abciximab has been associated with hemorrhagic conversion in patients who have recently experienced an ischemic event, we cannot rule out hemorrhagic conversion of an infarct.[6,13] Although the etiology of this hemorrhage is unclear, the severity of the hemorrhage was likely aggravated by antiplatelet therapy. It is also important to note that stent thrombosis or thrombotic complications did not occur in any of the patients who received platelet infusions prior to EVD placement in this series.
Salvage intracranial stenting
Our series include 12 patients in which a stent was used as a salvage procedure. All of the patients initially underwent unassisted embolization of the aneurysm. These salvage stents were used because there was evidence of parent vessel occlusion from the coil mass or thrombus. Luo et al. also reported nine cases in which a Neuroform stent was successfully used as a bailout.[9] Their reason for use of a stent was similar to ours involving eight patients who had evidence of parent vessel compromise and one patient with flow compromise distal to the aneurysm. All cases were salvaged with the use of the stent but only two patients had transient neurological deficits, which fully recovered. In addition, no patients had stent-related thrombotic complications despite being loaded with clopidogrel after the embolization. Yoo et al. also reports 16 patients in which stent delivery was attempted as a salvage procedure during nonassisted embolization of aneurysms.[22] Although the bailout procedure failed in four patients either due to inability to deliver the stent or due to unsuccessful remodeling of the coil pack, 12 patients (75%) had desirable results. None of these patients had thrombotic complications related to successful delivery of the stent although all except three patients who presented with SAH were pretreated with aspirin and clopidogrel.
Outcome and follow-up
Despite the thromboembolic and hemorrhagic complications, the majority of the patients in this study had good outcomes. Only seven patients (19%) in this case series had a GOS of two or less at the time of discharge. Three of these patients presented with a Hunt Hess score of four or five and failed to make a significant recovery during their hospital course. One patient had neurological compromise related to the hemorrhagic complication described above. The embolization was also technically successful in securing the dome of the aneurysm in the 34 of 36 patients. In addition, the majority of the patients had little to no residual aneurysm on follow-up angiography despite subtotal embolization of the aneurysms. This finding may be due to redirection of flow induced by the stent itself.[19] However, more data are necessary to determine if the flow redirection by a stent significantly reduces the rate of recurrence during subtotal aneurysm embolization. The follow-up for this study is rather short and not sufficient to evaluate the long-term rate of recurrence; however, the data are sufficient to evaluate the efficacy of this protocol in protecting against short-term rehemorrhage.
CONCLUSION
Given that this is a small retrospective review, the procedural protocols and criteria for stenting were not standardized, and the follow-up for patients is incomplete and variable, the conclusions that can be drawn from this study are limited. Surgical options for treatment of wide-necked ruptured aneurysms should be considered especially in relation to the risk of thrombotic complications found within this study. Stent-assisted coil embolization appears to be a safe and viable option for treatment of select wide-neck ruptured aneurysms and for salvage treatment during unassisted embolization of ruptured aneurysms. Lack of pretreatment with clopidogrel appears to increase the risk of thromboembolic complications; however, many of the thromboembolic complications encountered in this series had other technical aspects, which may have contributed to the risk of thromboembolism. A loading dose of clopidogrel prior to embolization does not appear to increase the risk of re-rupture. No evidence of procedure related hemorrhagic complications were found in this series of patients who were on antiplatelet therapy and received periprocedural platelet transfusions. Only one patient had evidence of a spontaneous hemorrhage 10 days after embolization of the aneurysm. While the etiology of this complication is not likely related to antiplatelet therapy or intraoperative infusion of abciximab, the lack of the platelet function likely increased the severity of the parenchymal hemorrhage. The majority of patients in this series had a good clinical outcome; however, 5 of 18 patients required further treatment of their aneurysm after angiographic follow-up.
Footnotes
Available FREE in open access from: http://www.surgicalneurologyint.com/text.asp?2012/3/1/84/99174
Contributor Information
Kiarash Golshani, Email: kgolshani@llu.edu.
Andrew Ferrel, Email: andrew.ferrell@duke.edu.
Mark Lessne, Email: mlessne@alum.bu.edu.
Pratish Shah, Email: pratishshaw@yahoo.com.
Abhineet Chowdhary, Email: abhineet.chowdhary@cshs.org.
Armen Choulakian, Email: armen.choulakian@cshs.org.
Michael J. Alexander, Email: michael.alexander@cshs.org.
Tony P. Smith, Email: smith146@mc.duke.edu.
David S. Enterline, Email: david.enterline@duke.edu.
Ali R. Zomorodi, Email: ali.zomorodi@duke.edu.
Gavin W. Britz, Email: gavin.britz@duke.edu.
REFERENCES
- 1.Aviv RI, O’Neill R, Patel MC, Colquhoun IR. Abciximab in patients with ruptured intracranial aneurysms. AJNR Am J Neuroradiol. 2005;26:1744–50. [PMC free article] [PubMed] [Google Scholar]
- 2.Benitez RP, Silva MT, Klem J, Veznedaroglu E, Rosenwasser RH. Endovascular occlusion of wide-necked aneurysms with a new intracranial microstent (Neuroform) and detachable coils. Neurosurgery. 2004;54:1359–67. doi: 10.1227/01.neu.0000124484.87635.cd. [DOI] [PubMed] [Google Scholar]
- 3.Brooks NP, Turk AS, Niemann DB, Aagaard-Kienitz B, Pulfer K, Cook T. Frequency of thromboembolic events associated with endovascular aneurysm treatment: Retrospective case series. J Neurosurg. 2008;108:1095–100. doi: 10.3171/JNS/2008/108/6/1095. [DOI] [PubMed] [Google Scholar]
- 4.Cottier JP, Pasco A, Gallas S, Gabrillargues J, Cognard C, Drouineau J, et al. Utility of balloon-assisted Guglielmi detachable coiling in the treatment of 49 cerebral aneurysms: A retrospective, multicenter study. AJNR Am J Neuroradiol. 2001;22:345–51. [PMC free article] [PubMed] [Google Scholar]
- 5.Cronqvist M, Wirestam R, Ramgren B, Brandt L, Nilsson O, Saveland H, et al. Diffusion and perfusion MRI in patients with ruptured and unruptured intracranial aneurysms treated by endovascular coiling: Complications, procedural results, MR findings and clinical outcome. Neuroradiology. 2005;47:855–73. doi: 10.1007/s00234-005-1408-2. [DOI] [PubMed] [Google Scholar]
- 6.Gralla J, Rennie AT, Corkill RA, Lalloo ST, Molyneux A, Byrne JV, et al. Abciximab for thrombolysis during intracranial aneurysm coiling. Neuroradiology. 2008;50:1041–7. doi: 10.1007/s00234-008-0457-8. [DOI] [PubMed] [Google Scholar]
- 7.Katsaridis V, Papagiannaki C, Violaris C. Embolization of acutely ruptured and unruptured wide-necked cerebral aneurysms using the neuroform 2 stent without pretreatment with antiplatelets: A single center experience. AJNR Am J Neuroradiol. 2006;27:1123–8. [PMC free article] [PubMed] [Google Scholar]
- 8.Lessne M, Shah P, Alexander M, Barnhart H, Powers C, Golshani K, et al. Thromboembolic complications after Neuroform™ stent assisted treatment of cerebral aneurysms: The Duke Cerebrovascular Center experience in 235 patients with 274 stents. Neurosurgery. 2011;69:369–75. doi: 10.1227/NEU.0b013e31821bc49c. [DOI] [PubMed] [Google Scholar]
- 9.Luo CB, Chang FC, Teng MM, Guo WY, Chang CY. Stent management of coil herniation in embolization of internal carotid aneurysms. AJNR Am J Neuroradiol. 2008;29:1951–5. doi: 10.3174/ajnr.A1268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Molyneux A, Kerr R, Stratton I, Sandercock P, Clarke M, Shrimpton J, et al. International Subarachnoid Aneurysm Trial (ISAT) of neurosurgical clipping versus endovascular coiling in 2143 patients with ruptured intracranial aneurysms: A randomised trial. Lancet. 2002;360:1267–74. doi: 10.1016/s0140-6736(02)11314-6. [DOI] [PubMed] [Google Scholar]
- 11.Moret J, Cognard C, Weill A, Castaings L, Rey A. Reconstruction technic in the treatment of wide-neck intracranial aneurysms. Long-term angiographic and clinical results. Apropos of 56 cases. J Neuroradiol. 1997;24:30–44. [PubMed] [Google Scholar]
- 12.Park JH, Kim JE, Sheen SH, Jung CK, Kwon BJ, Kwon OK, et al. Intraarterial abciximab for treatment of thromboembolism during coil embolization of intracranial aneurysms: Outcome and fatal hemorrhagic complications. J Neurosurg. 2008;108:450–7. doi: 10.3171/JNS/2008/108/3/0450. [DOI] [PubMed] [Google Scholar]
- 13.Qureshi AI, Saad M, Zaidat OO, Suarez JI, Alexander MJ, Fareed M, et al. Intracerebral hemorrhages associated with neurointerventional procedures using a combination of antithrombotic agents including abciximab. Stroke. 2002;33:1916–9. doi: 10.1161/01.str.0000019423.08947.43. [DOI] [PubMed] [Google Scholar]
- 14.Raymond J, Guilbert F, Weill A, Georganos SA, Juravsky L, Lambert A, et al. Long-term angiographic recurrences after selective endovascular treatment of aneurysms with detachable coils. Stroke. 2003;34:1398–403. doi: 10.1161/01.STR.0000073841.88563.E9. [DOI] [PubMed] [Google Scholar]
- 15.Ries T, Siemonsen S, Grzyska U, Zeumer H, Fiehler J. Abciximab is a safe rescue therapy in thromboembolic events complicating cerebral aneurysm coil embolization: Single center experience in 42 cases and review of the literature. Stroke. 2009;40:1750–7. doi: 10.1161/STROKEAHA.108.539197. [DOI] [PubMed] [Google Scholar]
- 16.Roy D, Milot G, Raymond J. Endovascular treatment of unruptured aneurysms. Stroke. 2001;32:1998–2004. doi: 10.1161/hs0901.095600. [DOI] [PubMed] [Google Scholar]
- 17.Shapiro M, Babb J, Becske T, Nelson PK. Safety and efficacy of adjunctive balloon remodeling during endovascular treatment of intracranial aneurysms: A literature review. AJNR Am J Neuroradiol. 2008;29:1777–81. doi: 10.3174/ajnr.A1216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Tahtinen OI, Vanninen RL, Manninen HI, Rautio R, Haapanen A, Niskakangas T, et al. Wide-necked intracranial aneurysms: Treatment with stent-assisted coil embolization during acute (<72 hours) subarachnoid hemorrhage--experience in 61 consecutive patients. Radiology. 2009;253:199–208. doi: 10.1148/radiol.2531081923. [DOI] [PubMed] [Google Scholar]
- 19.Tateshima S, Tanishita K, Hakata Y, Tanoue SY, Vinuela F. Alteration of intraaneurysmal hemodynamics by placement of a self-expandable stent. Laboratory investigation. J Neurosurg. 2009;111:22–7. doi: 10.3171/2009.2.JNS081324. [DOI] [PubMed] [Google Scholar]
- 20.Tumialan LM, Zhang YJ, Cawley CM, Dion JE, Tong FC, Barrow DL. Intracranial hemorrhage associated with stent-assisted coil embolization of cerebral aneurysms: A cautionary report. J Neurosurg. 2008;108:1122–9. doi: 10.3171/JNS/2008/108/6/1122. [DOI] [PubMed] [Google Scholar]
- 21.van den Bergh WM, Kerr RS, Algra A, Rinkel GJ, Molyneux AJ. Effect of antiplatelet therapy for endovascular coiling in aneurysmal subarachnoid hemorrhage. Stroke. 2009;40:1969–72. doi: 10.1161/STROKEAHA.108.528802. [DOI] [PubMed] [Google Scholar]
- 22.Yoo E, Kim DJ, Kim DI, Lee JW, Suh SH. Bailout stent deployment during coil embolization of intracranial aneurysms. AJNR Am J Neuroradiol. 2009;30:1028–34. doi: 10.3174/ajnr.A1482. [DOI] [PMC free article] [PubMed] [Google Scholar]


