Abstract
We report a case of combined pulmonary fibrosis and emphysema (CPFE) with severe pulmonary hypertension in a 46-year-old man, nonsmoker, tyre industry worker. CPFE is commonly reported to be associated with tobacco smoking. This case highlights the possible role of environmental dust exposure (talc) in the pathogenesis of the disease and confirms the clinical characteristics of CPFE described in previous studies.
KEY WORDS: Emphysema, smoking, talc
INTRODUCTION
The term combined pulmonary fibrosis and emphysema (CPFE) as a distinct underrecognized entity was described by Cottin et al.[1] The findings of co-existing cryptogenic fibrosing alveolitis and emphysema were first described in 1990 by Wiggins et al.[2] Subsequently, the same disease characteristics were described as an atypical phenotype of idiopathic interstitial pneumonias.[3] Cases of CPFE are usually tobacco smokers. Hence, CPFE has been proposed as a new clinical entity in smokers or a different clinical phenotype in smokers developing interstitial pulmonary fibrosis (IPF). These cases have severe dyspnea, nearly stable lung functions,exercise desaturation, reduced diffusion capacity, severe pulmonary hypertension (PH) and associated shortened survival.[4] High-resolution computed tomography (HRCT) findings in CPFE are characteristic, with predominantly upper lobe centrilobular emphysema and lower lobe fibrosis. The prevalence of CPFE may be close to 30% among cases of IPF, and these cases have a significantly lower survival as compared to those with only IPF.[5]
Workers with a history of long-term employment in tyre manufacturing plants are susceptible to various pulmonary and pleural diseases. Talc powder used in the tyre building department to prevent the rubber surfaces from sticking together is responsible for various lung diseases. Talc-related inflammatory reaction may progress to interstitial fibrosis and emphysema. We report a case of CPFE in a nonsmoker tyre industry worker in order to emphasize the possible role of environmental dust exposure in the pathogenesis of the disease.
CASE REPORT
A 46-year-old man, nonsmoker, presented with dry cough and progressive breathlessness for 10 years. He had been working in the building department of tyre industry for 26 years. On examination, he was tachypnoeic, with a respiratory rate of 36/min, clubbed and had pedal edema with elevated jugular venous pressure and bilateral fine crackles. His hematological investigations were within normal limits, except polycythemia. Arterial blood gas analysis (ABG) showed pH 7.33/PaO2 56.8/PaCO2 21.5/HCO3 11.1, with an alveolar arterial gradient of 67.13. X-ray chest [Figure 1] showed reticulonodular pattern. HRCT [Figure 2] showed extensive fibrosis and ground glass pattern with mid-zone predominance with areas of honeycombing and paraseptal emphysema. Spirometry showed a restrictive abnormality with forced vital capacity (FVC) 2.95L (62%predicted), forced expiratory volume in one second (FEV1) –2.20 L (56% predicted) and FEV1/FVC–75%. Diffusion capacity for carbon monoxide (DLCO) was 6% of the predicted value. Two-dimensional echocardiography (2D-ECHO) showed PH with tricuspid regurgitation (TR) jet-estimated pulmonary artery systolic pressure (PASP) of 62 mmHg with dilatation of right atrium and right ventricle. Diagnosis of rubber industry-related interstitial lung disease (ILD) with cor pulmonale was made. He was started on prednisolone 20 mg on alternate days, cyclophosphamide 2 mg/kg and long-term oxygen therapy (LTOT), and was advised to change his job. Reassessment 3 months later showed improvement in symptoms and spirometric findings of FVC–3.64 (76%), FEV1–2.50 (64%), FEV1/FVC– 69%, i.e. increase in FVC and FEV1 by 690 ml and 300 ml, respectively. Diffusion carrying capacity for carbon monoxide improved to 28% of the predicted. However, he did not follow-up subsequently and was noncompliant with therapy.
Figure 1.
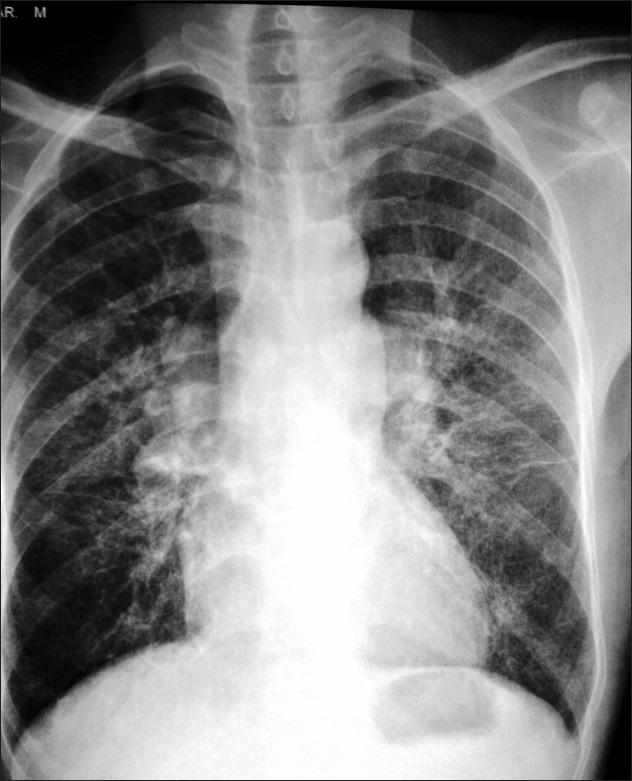
Initial chest X-ray showing reticulonodular pattern with midzone predominance
Figure 2.
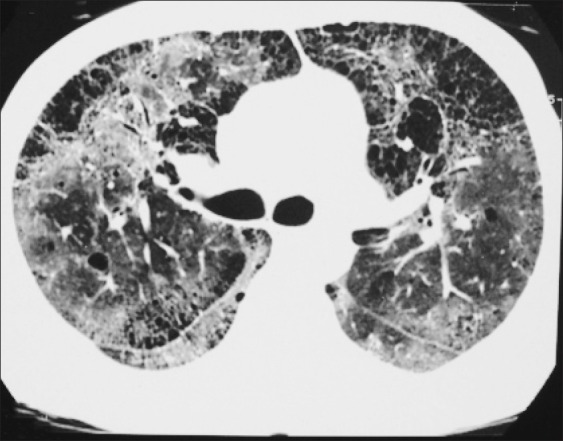
Initial high-resolution computer tomography showing extensive fibrosis and ground glass pattern with midzone predominance, few areas of honeycombing and areas of paraseptal emphysema
Four years later, he presented with increased symptoms of dyspnea and right heart failure. ABG showed PH 7.43/PaO2 54.9/PaCO224.2/HCO3 15.6/SO2 88.7. Chest X-ray [Figure 3] showed reticulonodular pattern with hyperinflation and HRCT [Figure 4a–b] showed extensive areas of centrilobular and paraseptal emphysema with overinflation. Areas of fibrosis were not very well appreciated as compared with earlier findings. 2D-ECHO showed PH with TR jet-estimated PASP of 90 mmHg and dilatation of right atrium and right ventricle. The patient refused for right heart catheterization. Spirometry showed FVC–3.12 (67%), FEV1–.99 (53%) and FEV1/FVC–64%, suggesting obstructive abnormality. DLCO was 19% of the predicted value. Total lung capacity (TLC) was 6.43 L (92% predicted) and residual volume (RV) was 2.84 (137% predicted), while the RV/TLC ratio was 148%. A diagnosis of combined pulmonary fibrosis and emphysema with severe PH due to occupational exposure to talc was made. The patient was discharged after stabilization, with advice to continue long-term oxygen therapy and change of job.
Figure 3.

Chest X-ray 4 years later showing reticulonodular pattern with hyperinflation
Figure 4.
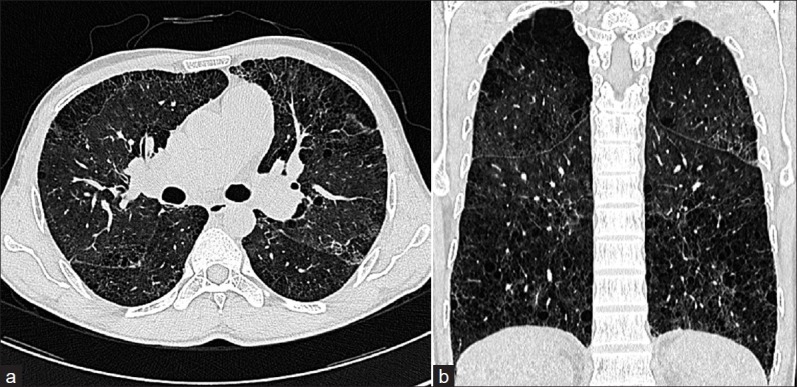
(a and b) High-resolution computer tomography 4 years later showing centrilobular and paraseptal emphysema with associated areas of fibrosis which are not very well appreciated due to the predominance of emphysema
DISCUSSION
Tyre building is the process of assembling all the components on to a tyre-building drum. The compounds needed for tyre making are prepared by mechanically mixing in a banbury mixture to mechanically break down the rubber to obtain a uniformly homogenous mass. This is subsequently formed into slabs of rubber that are extruded or calendered for use in tyre building. Before being transferred to the building machine, components are stored in large rolls. While the tyre is being extruded, powdered talc is blown through it by means of compressed air or woven fabric liners coated with talc or soap stone are placed between the layers of the rolled material to prevent the components from sticking together. These rolls are placed onto the feeding portion of the assembly equipment. This leads to extensive lifting and handling of heavy rolls and exposure to talc in a limited space.[6] The workers in these occupational settings are exposed to potentially harmful effects of talc dust and can present with pulmonary and pleural pathologies.[6–11] Talc causes granuloma formation, and the inflammatory reaction may progress to interstitial fibrosis and emphysema.
Our patient was working in the tyre industry for 26 years where he was exposed to talc. He presented with significant dyspnea with stable lung volumes over 6 years with increase in the RV/TLC ratio and reduction in DLCO. HRCT over time showed marked increase in areas of centrilobular and paraseptal emphysema, with overinflation and reduction in fibrotic areas. These findings were consistent with HRCT findings in patients with CPFE decribed by Cottin et al.[1] These changes are probably because of the same pathogenic mechanisms involved in development of fibrosis and emphysema. Whether emphysematous and fibrotic lesions progress independently or the development of one of them (emphysema) modifies the progression of the other has been questioned.[5] CPFE has been reported with tobacco smoking and classical presentation with severe dyspnea, preserved lung functions, significant reductions in gas exchange postexercise desaturation, characteristic imaging features and high prevalence of pulmonary hypertension. This was initially reported to be coincidental, but has now been proposed as a distinct syndrome.[1] The literature emphasizes the importance of diagnosing CPFE because it carries an increased risk of developing pulmonary hypertension with increased mortality.[5] Its association with connective tissue diseases like rheumatoid arthritis and systemic sclerosis and exposure to agrochemical compounds has also been described.[12,13] There is no data on effective therapy for this entity.
Smoking plays a central role in the over expression of tumor necrosis factor-alfa (TNF-α), due to which it may be an important factor in producing emphysema and pulmonary fibrosis. Overexpression of TNF-α and platelet-derived growth factor (PDGF-b) produces airspace dilatation, and fibrosis has been confirmed by animal data.[14,15] In a study by Wei et al.,[16] pulmonary fibrosis in CPFE showed intrinsic characteristics, with smoking not being the major or direct pulmonary fibrosis-driven factor. He suggested the role of blood serum pro-collagen III N-terminal peptide (PIIINP) as a marker of early detection and efficacy assessment parameter of treatment and the possible utility of anti-lymphocytes and immune regulation strategy for disease intervention. Phenotype characteristics to evaluate biological markers in sputum and peripheral blood T-lymphocytes are ongoing. Emphysema involved in pulmonary fibrosis has a significantly higher Th1 and Th2 expression. Hence, studies regarding the role of Th1 and Th2 expression in CPFE are under review. The pathophysiology of CPFE is yet unknown, but it is speculated that both emphysema and fibrosis may be related to a common environmental trigger or a genetic susceptibility factor. Our case highlights the possible role of environmental dust exposure (talc) in the pathogenesis of the disease.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Cottin V, Nunes H, Brillet PY, Delaval P, Devouassoux G, Tillie-Leblond I, et al. Combined pulmonary fibrosis and emphysema: A distinct under- recognized entity. Eur Respir J. 2005;26:586–93. doi: 10.1183/09031936.05.00021005. [DOI] [PubMed] [Google Scholar]
- 2.Wiggins J, Strickland B, Turner-Warwick M. Combined cryptogenic fibrosing alveolitis and emphysema: The value of high resolution computed tomography in assessment. Respir Med. 1990;84:365–9. doi: 10.1016/s0954-6111(08)80070-4. [DOI] [PubMed] [Google Scholar]
- 3.Cottin V. Interstitial lung disease: New challenges and evolving phenotypes. (91-3).Eur Respir Rev. 2010;19:116. doi: 10.1183/09059180.00003910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Cottin V, Pavec JL, Prévot G, Mal H, Humbert M, Simonneau G, et al. Pulmonary hypertension in patients with combined pulmonary fibrosis and emphysema syndrome. Eur Respir J. 2010;35:105–11. doi: 10.1183/09031936.00038709. [DOI] [PubMed] [Google Scholar]
- 5.Mejia M, Carrillo G, Serrano J, Estrada A, Suarez T, Alonso D, et al. Idiopathic pulmonary fibrosis and emphysema: Decreased survival associated with severe pulmonary arterial hypertension. Chest. 2009;136:10–5. doi: 10.1378/chest.08-2306. [DOI] [PubMed] [Google Scholar]
- 6.McLaughlin A, Rogers E, Dunham KC. Talc Pneumoconiosis. Br J Ind Med. 1949;6:184. doi: 10.1136/oem.6.3.184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Fischbein A. Cancer mortality in a northern italian cohort of rubber workers: Correspondence. Br J Ind Med. 1990;47:71–2. doi: 10.1136/oem.47.1.71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Neghab M, Rahimi E, Emad A, Rajaeei Fard AR. An epidemiological study of talc-related respiratory morbidity among employees of a rubber industry in Shiraz-Iran. Int Arch Occup Environ Health. 2007;80:539–46. doi: 10.1007/s00420-006-0161-0. [DOI] [PubMed] [Google Scholar]
- 9.Hunt AC. Massive Pulmonary fibrosis from the inhalation of talc. Thorax. 1956;11:287. doi: 10.1136/thx.11.4.287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gamble JF, Fellner W, Dimeo MJ. An epidemiologic study of a group of talc workers. Am Rev Respir Dis. 1979;119:741–53. doi: 10.1164/arrd.1979.119.5.741. [DOI] [PubMed] [Google Scholar]
- 11.McMichael A, Gerber W, Gamble J, Lednar W. Chronic respiratory symptom and job type within the rubber industry. J Occup Med. 1976;18:611–7. [PubMed] [Google Scholar]
- 12.Cottin V, Nunes H, Mouthon L, Gamondes D, Lazor R, Hachulla E, et al. Combined pulmonary fibrosis and emphysema syndrome in connective tissue disease. Arthritis Rheum. 2011;63:295–304. doi: 10.1002/art.30077. [DOI] [PubMed] [Google Scholar]
- 13.Daniil Z, Koutsokera A, Gourgoulianis K. Combined pulmonary ribrosis and emphysema in patients exposed to agrochemical compounds: Correspondence. Eur Respir J. 2006;27:434–39. doi: 10.1183/09031936.06.00124505. [DOI] [PubMed] [Google Scholar]
- 14.Lundblad LK, Thompson-Figueroa J, Leclair T, Sullivan MJ, Poynter ME, Irvin CG, et al. Tumor necrosis factor-alpha over expression in lung disease: A single cause behind a complex phenotype. Am J Respir Crit Care Med. 2005;171:1363–70. doi: 10.1164/rccm.200410-1349OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hoyle GW, Li J, Finkelstein JB, Eisenberg T, Liu JY, Lasky JA, et al. Emphysematous lesions, inflammation, and fibrosis in the lungs of transgenic mice over expressing platelet-derived growth factor. Am J Pathol. 1999;154:1763–75. doi: 10.1016/S0002-9440(10)65432-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Wei XH, Wu XY, Wang JH, Thakur A, Ma AQ. Correlation of lymphocytes and PIIINP with the combined pulmonary fibrosis and emphysema. Xi Bao Yu Fen Zi Mian Yi Xue Za Zhi. 2010;26:675–8. [PubMed] [Google Scholar]


