Abstract
Allergic bronchopulmonary aspergillosis (ABPA) is typically associated with asthma. Presence of asthma is one of the minimal essential diagnostic criteria for ABPA. Rarely, ABPA has been described in association with other diseases without asthma. It has so far not been known to complicate pulmonary tuberculosis. We report one such case in a young lady where all other diagnostic criteria were fulfilled. The patient responded to corticosteroids and then had acute exacerbations of ABPA twice, each time requiring an increased dosage of corticosteroids as well as itraconazole and responded favorably.
KEY WORDS: Allergic bronchopulmonary aspergillosis, asthma, tuberculosis
INTRODUCTION
Allergic bronchopulmonary aspergillosis (ABPA) is a dual Type I and III hypersensitivity response to aspergillus antigens and is typically associated with patients with asthma and occasionally with cystic fibrosis. The presence of asthma is one of the minimal essential diagnostic criteria for ABPA.[1] The prevalence of ABPA in asthma clinics is reported to be around 13%.[1]
Rarely, ABPA has been described without asthma.[2,3] Patients with current or previous tuberculosis may develop aspergillus-related lung disease including aspergilloma and chronic pulmonary necrotizing aspergillosis CPNA.[4] However, ABPA without asthma has so far not been known to complicate previous pulmonary tuberculosis though typical ABPA may occur concurrently with active tuberculosis[5] or follow it.[6] We report one such case in a young lady.
CASE REPORT
A 30-year-old lady, non-smoker and housewife, presented with complaints of progressive exertional breathlessness without wheezing, and productive cough that was occasionally blood-streaked, with three to four febrile episodes every year. She also gave a history of recurrent sneezing and rhinorrhoea. Two years ago, she was diagnosed to have sputum direct-smear acid-fast bacilli (AFB)-positive pulmonary tuberculosis, received anti-tubercular treatment for six months and was declared cured. However, breathlessness and cough persisted.
Examination revealed dullness on percussion and coarse inspiratory crepts bilaterally in the infraclavicular areas with bronchial breath sounds on the left side. She had a hemoglobin of 8.8 g/dl and a total leucocyte count of 10500/mm3 with 75% neutrophils and 5% eosinophils. The plain chest radiograph revealed extensive bilateral fibrosis, more on the left side with a right upper zone cavity. A few cystic shadows were seen in both lungs [Figure 1]. Sputum cultures for pyogenic organisms and direct-smear examination for AFB (three consecutive morning samples) were negative. Lung function tests showed a restrictive ventilatory defect: Forced vital capacity (FVC), 1.25 L (37% predicted); Forced expiratory volume in 1 s (FEV1) 0.96 L (32% predicted); FEV1/FVC ratio, 77%; Total lung capacity, 1.72 L (37% predicted).
Figure 1.

Plain chest radiograph (PA view) showing extensive bilateral fibrosis, more on the left side with a right upper zone cavity. A few cystic shadows were seen in both lungs
A high-resolution computed tomogram (HRCT) revealed bilateral upper lobe fibrocavitary lesions, more on the left side, with central bronchiectasis as well as middle-lobe bronchiectasis [Figures 2 and 3]. There was no mediastinal lymphadenopathy. A diagnosis of post-tubercular fibrocavitary sequelae was made.
Figure 2.
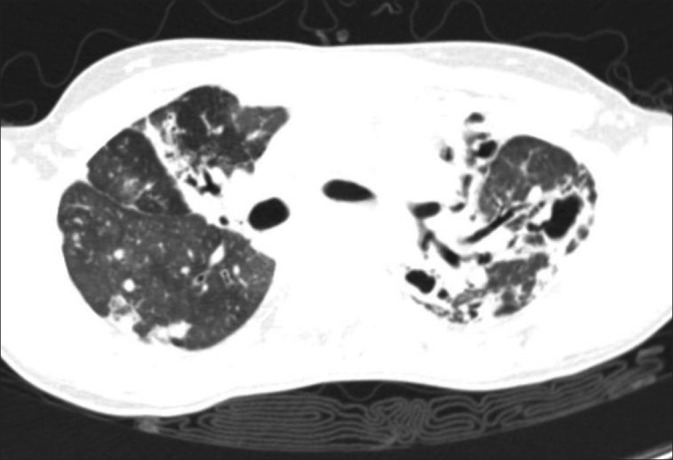
High-resolution computed tomogram of the chest (lung window) showing bilateral upper lobe fibrocavitary lesions, more on the left side, with central bronchiectasis
Figure 3.
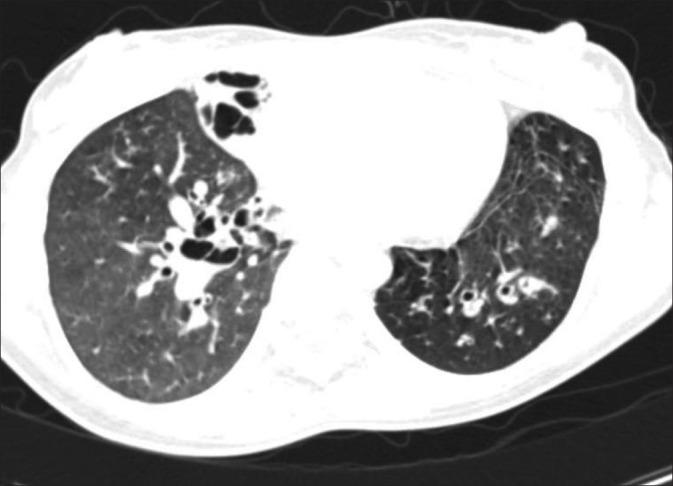
High-resolution computed tomogram of the chest (lung window) showing middle-lobe and bilateral central bronchiectasis
The presence of central bronchiectasis, a radiological sign characteristically associated with ABPA, prompted further investigations which were as follows: Skin prick tests for Type 1 hypersensitivity reaction against Aspergillus fumigatus and Aspergillus niger positive; serum total immunoglobulin E IgE elevated (8512 IU/ml), serum precipitins and specific immunoglobulin G (IgG) against Aspergillus fumigatus, positive, elevated titers of specific IgE against Aspergillus fumigatus (48.7 kUA/L); sputum for fungus on direct microscopy showed branching septate hyphae; culture negative for fungal growth. Thus, all the diagnostic criteria for ABPA were met except for the presence of asthma.[1,7]
The patient was advised oral prednisolone, 30 mg daily that was tapered over five to six months as the patient improved. Post treatment, the serum IgE levels had decreased to 2416 IU/ml and serum precipitins against Aspergillus fumigatus became negative. During the next one year, the patient had a relapse of symptoms twice with elevation of serum IgE levels and serum precipitins against Aspergillus fumigatus turning positive. Two consecutive sputum cultures this time also revealed growth of Aspergillus fumigatus. On both occasions, the patient responded to reinstitution of corticosteroids with reduced serum IgE levels and serum precipitins became negative. Oral itraconazole was also prescribed, 200 mg twice daily for 12 weeks. Currently, the patient is under follow-up in a stage of remission.
DISCUSSION
The diagnosis of ABPA is based on hematological, radiological and immunological criteria along with presence of asthma, and occasionally, cystic fibrosis.[1,7] However, ABPA occurring without asthma is very uncommon and such instances have been documented as case reports.[2–4]
While an aspergilloma is well known to complicate cavities resulting from a previous tuberculous disease,[5] aspergillus sensitization in patients with prior tuberculosis remains largely unexplored. A literature search yielded only one case reporting ABPA in a patient with post-tubercular sequelae[6] in whom wheezing and airways obstruction were present suggesting asthma. Our patient, however, had differences as there was no history suggestive of asthma and lung function tests showed a restrictive pattern. All the required diagnostic criteria for ABPA were satisfied except asthma. The clinical and immunological response to corticosteroids with remissions and relapses during the follow-up confirmed the diagnosis.
The relationship of tuberculosis to manifestations of atopy is complex. It has been suggested that the CD4+/Th 1 type of immune response in tuberculosis may protect against the development of asthma that is associated with a Th 2 type of response.[8] Mycobacteria culture supernatants have been shown to effectively prevent the development of asthma associated with altered Th1/Th2 cytokines in sensitized mice.[9] Therefore, it is possible that protection against atopic conditions may wane and allergic conditions may manifest after tuberculosis is treated. This, however, has not been investigated. Nevertheless, clinical experience shows that occurrence of wheezing and airways’ obstruction after treatment of tuberculosis is common and is attributed to endobronchial inflammation, scarring and mechanical distortion of the tracheobronchial tree. Interestingly, one study reported that the majority of patients with post-tubercular wheezing actually had confirmed bronchial asthma emerging within three years of stopping anti-tuberculosis treatment and required prolonged corticosteroid administration.[10] The remarkable feature of our patient was the absence of asthma while all other diagnostic criteria for ABPA were satisfied. ABPA complicating previously treated tuberculosis and occurring without asthma has never been reported earlier.
As aspergillus colonization in the airways and healed cavities is common in lungs with previously treated tuberculosis; sensitization may develop if the subject is atopic. Although our patient did not have asthma, she had atopy as shown by a history of allergic rhinitis and raised total IgE. Therefore, sensitization to aspergillus may have occurred followed by development of ABPA. The case highlights the curious link between tuberculosis and atopy and also suggests that presence of atopy without manifest asthma is sufficient for ABPA to develop. Patients with post-tubercular cough and dyspnoea should be investigated for ABPA if they are atopic.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Agarwal R. Allergic bronchopulmonary aspergillosis. Chest. 2009;135:805–26. doi: 10.1378/chest.08-2586. [DOI] [PubMed] [Google Scholar]
- 2.Agarwal R, Aggarwal AN, Gupta D, Bal A, Das A. Case report: A rare cause of miliary nodules – allergic bronchopulmonary aspergillosis. Br J Radiol. 2009;82:e151–4. doi: 10.1259/bjr/20940804. [DOI] [PubMed] [Google Scholar]
- 3.Shah A, Maurya V, Panjabi C, Khanna P. Allergic bronchopulmonary aspergillosis without clinical asthma caused by Aspergillus niger. Allergy. 2004;59:236–7. doi: 10.1046/j.1398-9995.2003.00372.x. [DOI] [PubMed] [Google Scholar]
- 4.Kim HY, Song KS, Goo JM, Lee JS, Lee KS, Lim TH. Thoracic sequelae and complications of tuberculosis. Radiographics. 2001;21:839–60. doi: 10.1148/radiographics.21.4.g01jl06839. [DOI] [PubMed] [Google Scholar]
- 5.Min KH, Park SJ, Kim SR, Lee MH, Chung CR, Han HJ, et al. Coexistence of allergic bronchopulmonary aspergillosis and active pulmonary tuberculosis. Am J Respir Crit Care Med. 2011;183:137–9. doi: 10.1164/ajrccm.183.1.137. [DOI] [PubMed] [Google Scholar]
- 6.Agarwal R, Singh N, Aggarwal AN. An unusual association between Mycobacterium tuberculosis and Aspergillus fumigatus. Monaldi Arch Chest Dis. 2008;69:32–4. doi: 10.4081/monaldi.2008.409. [DOI] [PubMed] [Google Scholar]
- 7.Malde B, Greenberger PA. Allergic bronchopulmonary aspergillosis. Allergy Asthma Proc. 2004;25:S38–9. [PubMed] [Google Scholar]
- 8.Jones PD, Gibson PG, Henry RL. The prevalence of asthma appears to be inversely related to the incidence of typhoid and tuberculosis: Hypothesis to explain the variation in asthma prevalence around the world. Med Hypotheses. 2000;55:40–2. doi: 10.1054/mehy.1999.0997. [DOI] [PubMed] [Google Scholar]
- 9.Han ER, Choi IS, Eom SH, Kim HJ. Preventive effects of mycobacteria and their culture supernatants against asthma development in BALB/c mice. Allergy Asthma Immunol Res. 2010;2:34–40. doi: 10.4168/aair.2010.2.1.34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Rajasekaran S, Savithri S, Jeyaganesh D. Post-tuberculosis bronchial asthma. Indian J Tub. 2001;48:139–42. [Google Scholar]


