Abstract
We reviewed the incidence, predisposing factors, presentation and management of complications related to the use of synthetic mesh in the management of stress urinary incontinence and pelvic organ prolapse repair. Immediate complications, such as bleeding, hematoma, injury to adjacent organs during placement of mesh and complication of voiding dysfunction are not discussed in this review, since they are primarily related to technique. A PubMed search of related articles published in English was done from April 2008 to March 2011. Key words used were urinary incontinence, mesh, complications, midurethral sling, anterior prolapse, anterior vaginal repair, pelvic organ prolapse, transvaginal mesh, vault prolapse, midurethral slings, female stress urinary incontinence, mesh erosion, vaginal mesh complications, and posterior vaginal wall prolapse. Since there were very few articles dealing with the management of mesh-related complications in the period covered in the search we extended the search from January 2005 onwards. Articles were selected to fit the scope of the topic. In addition, landmark publications and Manufacturer and User Facility Device Experience (MAUDE) data (FDA website) were included on the present topic. A total of 170 articles were identified. The use of synthetic mesh in sub-urethral sling procedures is now considered the standard for the surgical management of stress urinary incontinence. Synthetic mesh is being increasingly used in the management of pelvic organ prolapse. While the incidence of extrusion and erosion with mid-urethral sling is low, the extrusion rate in prolapse repair is somewhat higher and the use in posterior compartment remains controversial. When used through the abdominal approach the extrusion and erosion rates are lower. The management of mesh complication is an individualized approach. The choice of the technique should be based on the type of mesh complication, location of the extrusion and/or erosion, its magnitude, severity and potential recurrence of pelvic floor defect.
Keywords: Anterior vaginal repair, mesh complications, mid-urethral sling, pelvic organ prolapse, stress urinary incontinence
INTRODUCTION
Increasing use of biomaterials, most often non- absorbable meshes, resulted in a dramatic shift in surgical techniques, use of commercial kits and publications in the recent era. The minimal invasiveness and availability of kits resulted in a substantial increase in the number of these procedures by both urologists and gynecologists, often with minimal training. This exponential use of synthetic material gave rise to a wide variety of complications. These complications can be broadly classified as technique (procedure or surgeon)-based and product-based [Figure 1].
Figure 1.
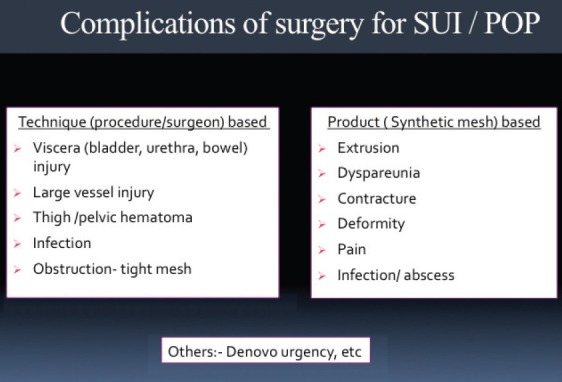
Classification of complications of surgery for female stress urinary incontinence and pelvic organ prolapse surgery employing prosthetic material
In this review article, we identified various predisposing factors, clinical presentation and management strategy of these mesh-related complications. Recurrent or persistent urinary incontinence or development of postoperative voiding dysfunction is not included in this review. Intra- operative complications, such as bleeding, hematoma, injury to adjacent organs during placement of mesh etc., are also not discussed since all these complications are mostly related to technique rather than directly to the use of mesh. These mesh-related complications could have a significant impact on the patient's quality of life and add to the cost of healthcare. Clinicians’ understanding of mesh-related complications and their proper management would result in improved outcome.
Clinical need for use of mesh in stress urinary incontinence and pelvic organ prolapse
Procedures for pelvic reconstruction utilizing native tissue are associated with a high recurrence rate.[1–4] This treatment failure can be attributable to the technique or defect in native tissues. Scarring and sclerosis produced by the standard pelvic reconstructive surgical procedures can restore only 50% of the preoperative tissue strength.[5] Reduced amount of collagen in connective tissue matrices in stress urinary incontinence (SUI) women compared to unaffected women has been demonstrated. Data suggest that the process responsible for reduced collagen content in the tissues of women with SUI is not limited to the pubocervical fascia, but represents a systemic process detectable in tissues not involved in support of pelvic organs. Collagenase activity in the conditioned media from skin and pubocervical fascia biopsy explant cultures is higher in biopsies taken from women with SUI; that circulating collagenolytic activity is higher in women with SUI and that urinary levels of collagen degradation products are higher in women with SUI, all provide supportive evidence for increased collagenolysis in the etiology of SUI.[6,7] Hence, in a recently published randomized control trial, recurrences of anterior vaginal prolapse were higher in the colporrhaphy group vs. reinforcement by mesh.[1–4]
To overcome these disadvantages of local tissue, autologous material like autologous fascia lata or rectus sheath were employed. But these required secondary harvesting procedure with increased operating time and its attendant morbidity, and furthermore have a size limitation for their use in prolapse surgery. Hence, non-autologous, biodegradable material came into use. However, the main problem with these materials was the unpredictability of grafts, variable preparation (retained DNA), cost of biomaterials and bacterial adherence to some, e.g. bovine pericardium.[8]
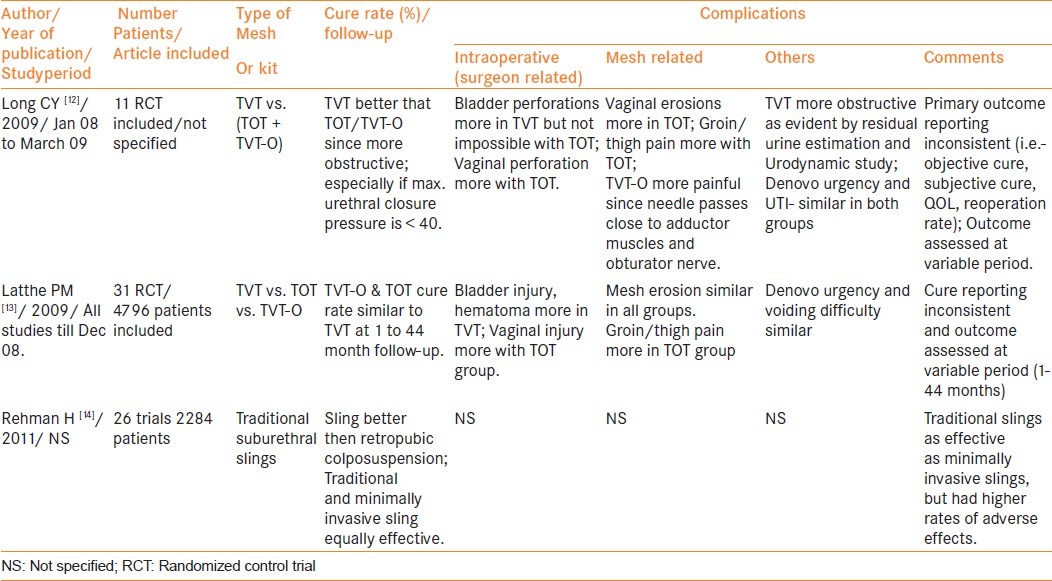
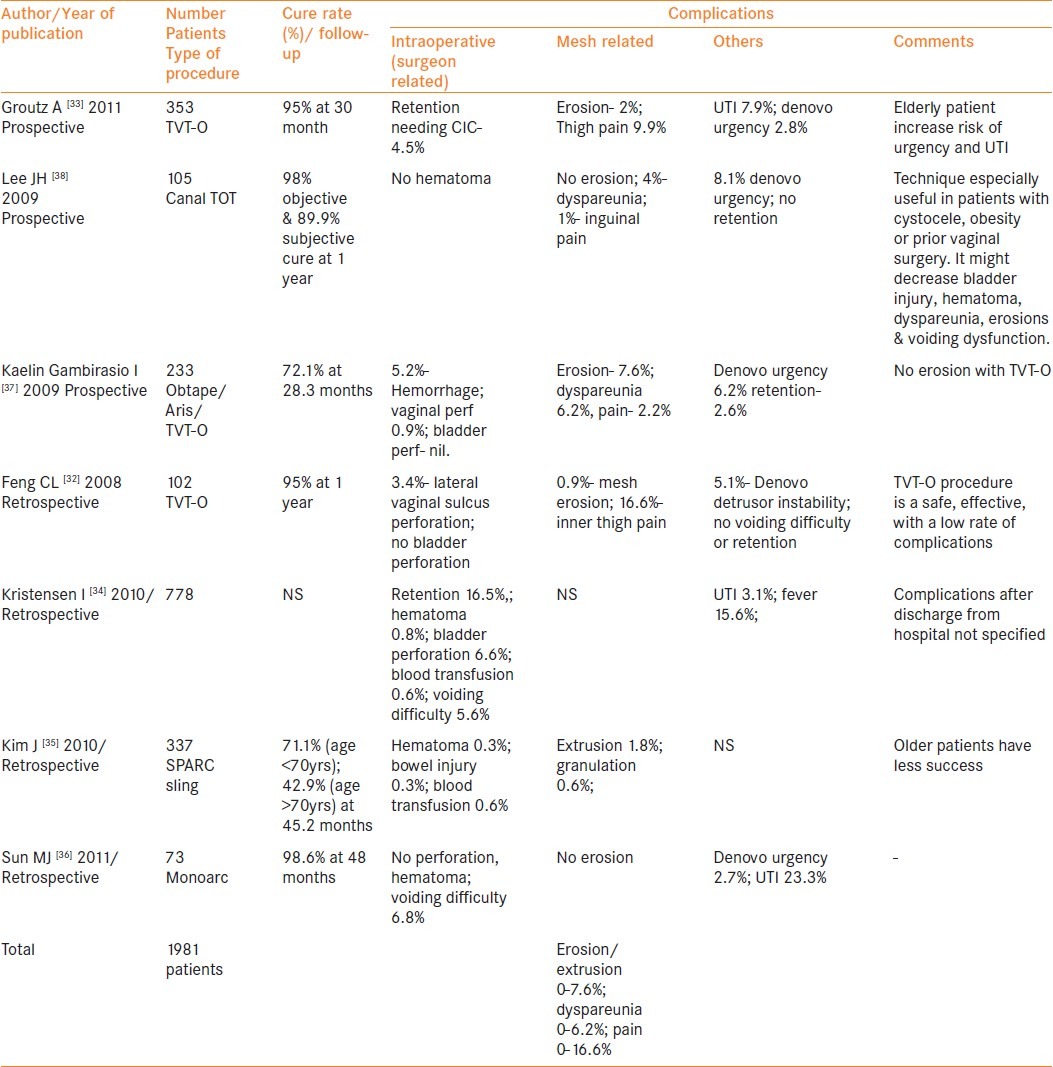
Over the last decade, synthetic materials have gradually become the primary material of choice for managing SUI in females. Their popularity is related to the avoidance of a secondary harvesting site, decreased surgical time and similar efficacy in comparison with autologous slings. The safety and durability of tension-free vaginal tape (TVT) has been confirmed by various meta-analyses and long-term (up to 11.5 years) data [Tables 1 and 2].[9–14] The use of synthetic mesh in prolapse repair is widespread, however, it remains controversial.
Table 1.
Review of studies evaluating long term outcome of TVT for SUI published in last 3 years
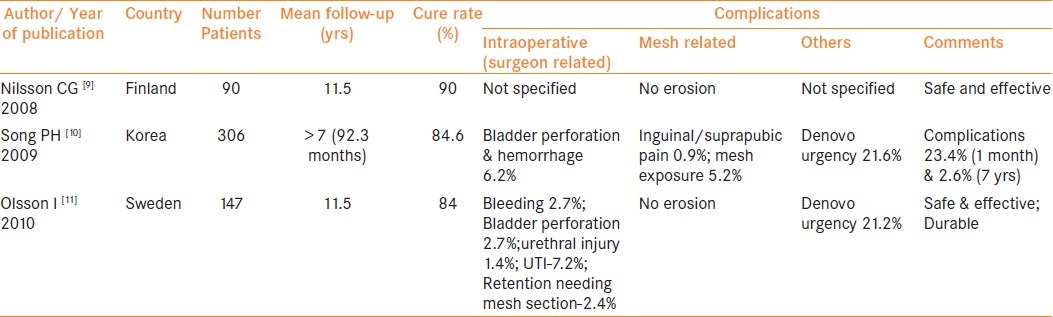
Table 2.
Review of Metaanalysis evaluating safety and efficacy of various midurethral slings for SUI published in last 3 years
MATERIALS AND METHODS
A PubMed search was made with key words “urinary incontinence”, “mesh”, “complications”, “mid-urethral sling”, “anterior prolapse”, “anterior vaginal repair”, “pelvic organ prolapse”, “transvaginal mesh”, “vault prolapse”, “female stress urinary incontinence”, “mesh erosion”, “vaginal mesh complications”, “posterior vaginal wall prolapse” for all available English literature from April 2008 to March 2011. All the articles reporting on the use of graft in female pelvic reconstructive surgery (SUI and/ or pelvic organ prolapse (POP) were selected to assess incidence and type of various complications associated with these surgeries. Since there were very few article dealing with the management of mesh-related complications in the period covered in the search we extended the search from January 2005 onwards. Articles were selected to fit scope of the topic, i.e. dealing with mesh complications and their management. In addition, landmark publications on the etiopathogenesis and management of mesh complications before 2008 and Manufacturer and User Facility Device Experience (MAUDE) data were included on the present topic.[15] A total 170 articles were identified.
Types of synthetic mesh
In 1997, Amid categorized synthetic materials used in abdominal hernia based on their properties including pore size and fiber type.[16] Unique mesh characteristics that are necessary in pelvic organ reconstruction include ease of use, the capability to incorporate host tissue with reduced risk for erosion, infection and extrusion, and non-carcinogenic. Grafts differ in their sources (synthetic or biological), composition (mono-filament or multi-filament), pore size, flexibility and architecture (knitted or woven). Type I monofilament, macroporous polypropylene mesh is the currently preferred synthetic material for use as graft since the large pore size (> 75 μm) facilitates infiltration of the mesh by macrophages, fibroblast and blood vessels. Thus host tissue in-growth is promoted resulting in good support and minimizing the risk of infection. A “light-weight” Type 1 mesh is created by decreasing the polypropylene density thereby causing less foreign-body response and improving tissue compliance. This might cause less contraction or shrinkage of the mesh and allow for better tissue incorporation. Type II monofilament microporous mesh allows bacterial infiltration; however, angiogenesis and fibroplasias are prevented because macrophage infiltration of the mesh and fibroblast incorporation is deterred due to small pore size (< 10 μm). These result in higher risk of infection that is difficult to treat. Type III multifilament mesh have interstices that are <10 μm and bacteria (<1 μm) can replicate within these interstices. However, access to macrophages and ability to fight bacterial colonization within the interstices is impaired. There is also increased risk of bacterial adherence due to increased surface area of mesh. Type IV meshes are sub-microporous coated biomaterials with pores of <1 μm. They are sparingly used in pelvic reconstructive surgery.
MESH COMPLICATIONS
Mesh erosion
Recently, the International Urogynecological Association (IUGA) and International Continence Society (ICS) jointly published the terminology and classification of the complications related directly to the insertion of prostheses (meshes, implants, tapes) and grafts in female pelvic floor surgery.[17] The important definitions given by them include-
Exposure
A condition of displaying, revealing, exhibiting, or making accessible (e.g., vaginal mesh visualized through separated vaginal epithelium).
Extrusion
Passage gradually out of a body structure or tissue (e.g., a loop of tape protruding into the vaginal cavity).
Perforation
Abnormal opening into a hollow organ or viscus.
They recommend, “the generic term of erosion (medically defined as the “state of being worn away, as by friction or pressure”), does not necessarily suit the clinical scenarios encountered and hence its use should be best avoided”. However, most publications reviewed have used the term erosion synonymously with extrusion. Hence while reviewing the literature and in tables, we have used the term “erosion” to include exposure, extrusion and perforation.
Incidence
Incidence of mesh erosion (including exposure, extrusion and perforation) initially described in the literature varies widely from 0–33%.[18] In a recent meta-analysis, Abed et al., studied 110 articles that included 11,785 patients and noted that the mean incidence of graft erosion was 10.3%.[19] In the last three years, the reported rate of mesh erosion after surgery for female SUI was 0–7.3% [Tables 3–7].[20–49] This was low in comparison with the 0–21% incidence reported in various randomized control trials and prospective studies published on POP surgeries by vaginal approach [Tables 8 and 9].[1–4,50–62] By virtue of its inherent limitation, the retrospective studies published on POP surgeries by vaginal approach noted relatively lower incidence (0–11.9%) of mesh erosion [Table 10].[63–75]
Table 3.
Review of RCT on various treatments for SUI published in last 3 years (except mini-slings and adjustable slings)
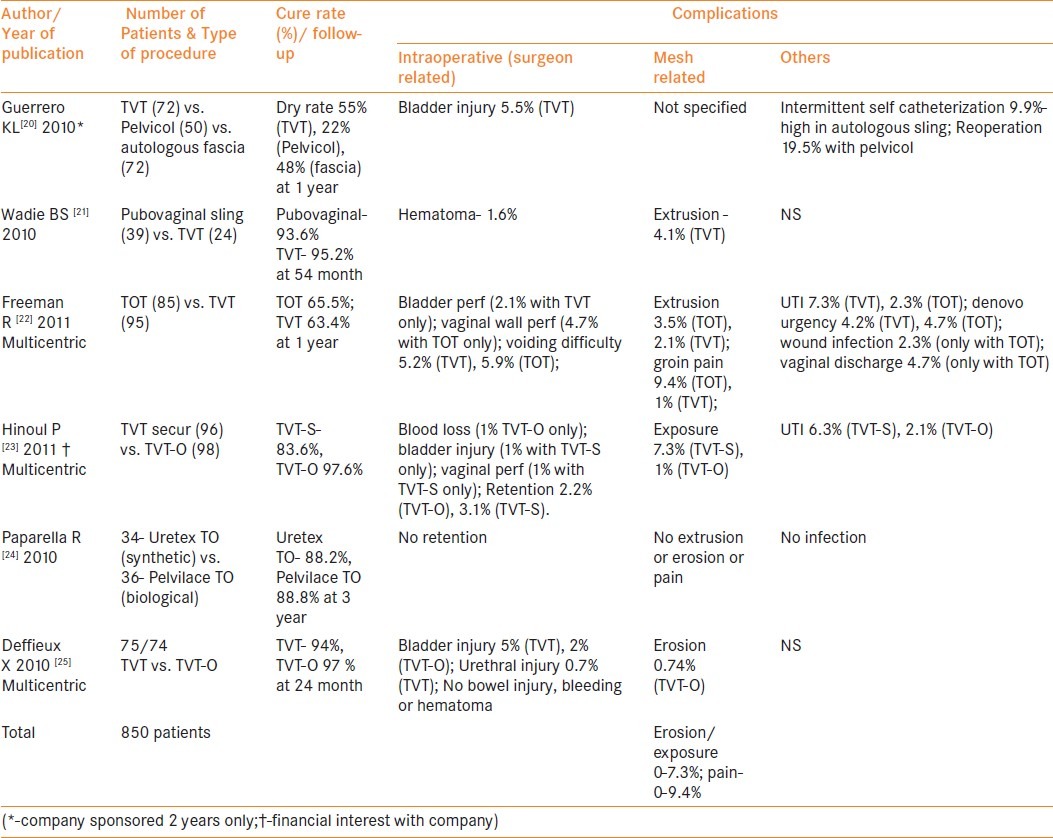
Table 7.
Review of literature on mini-slings for SUI published in last 3 years
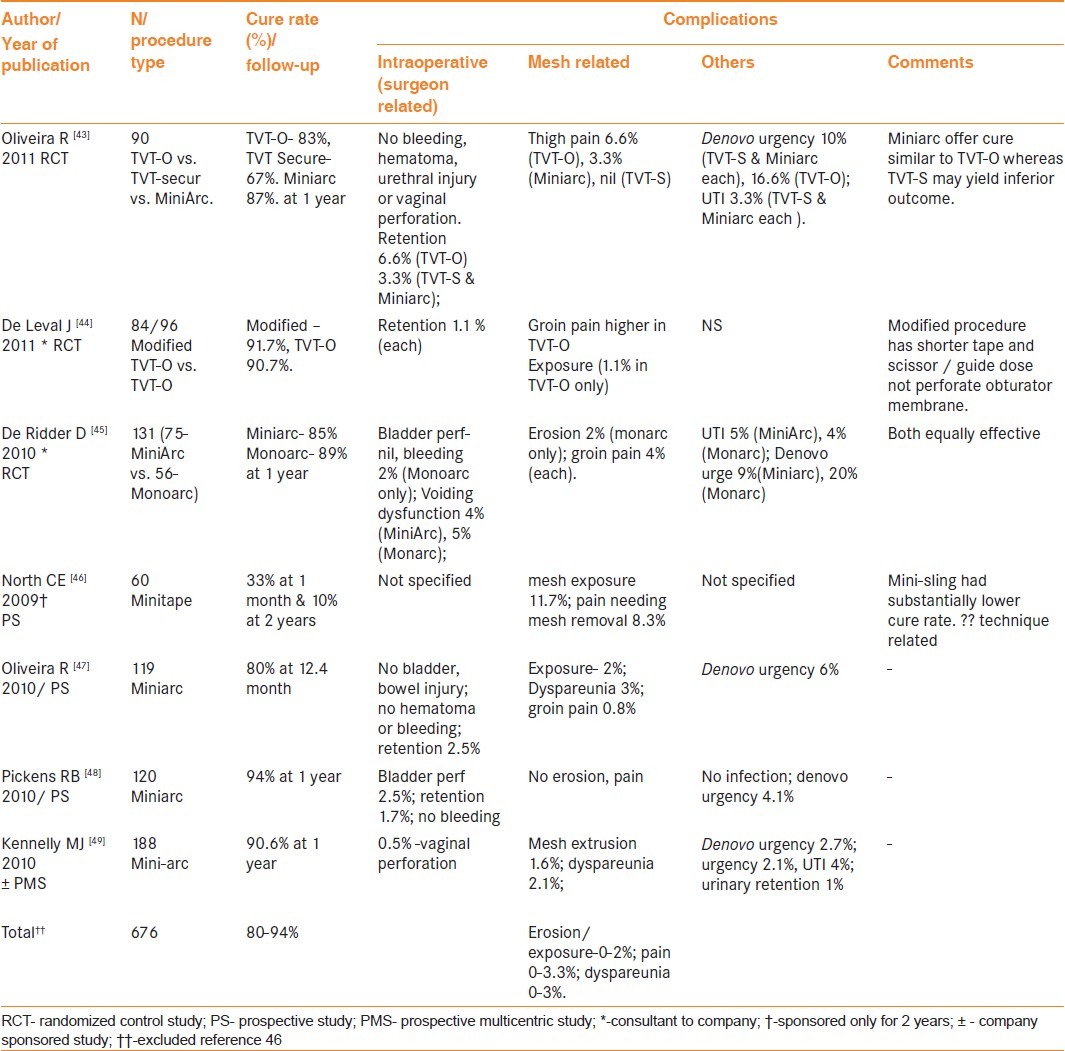
Table 8.
Review of RCT & prospective multicentre studies using synthetic mesh for transvaginal pelvic reconstructive surgery published in last 3 years
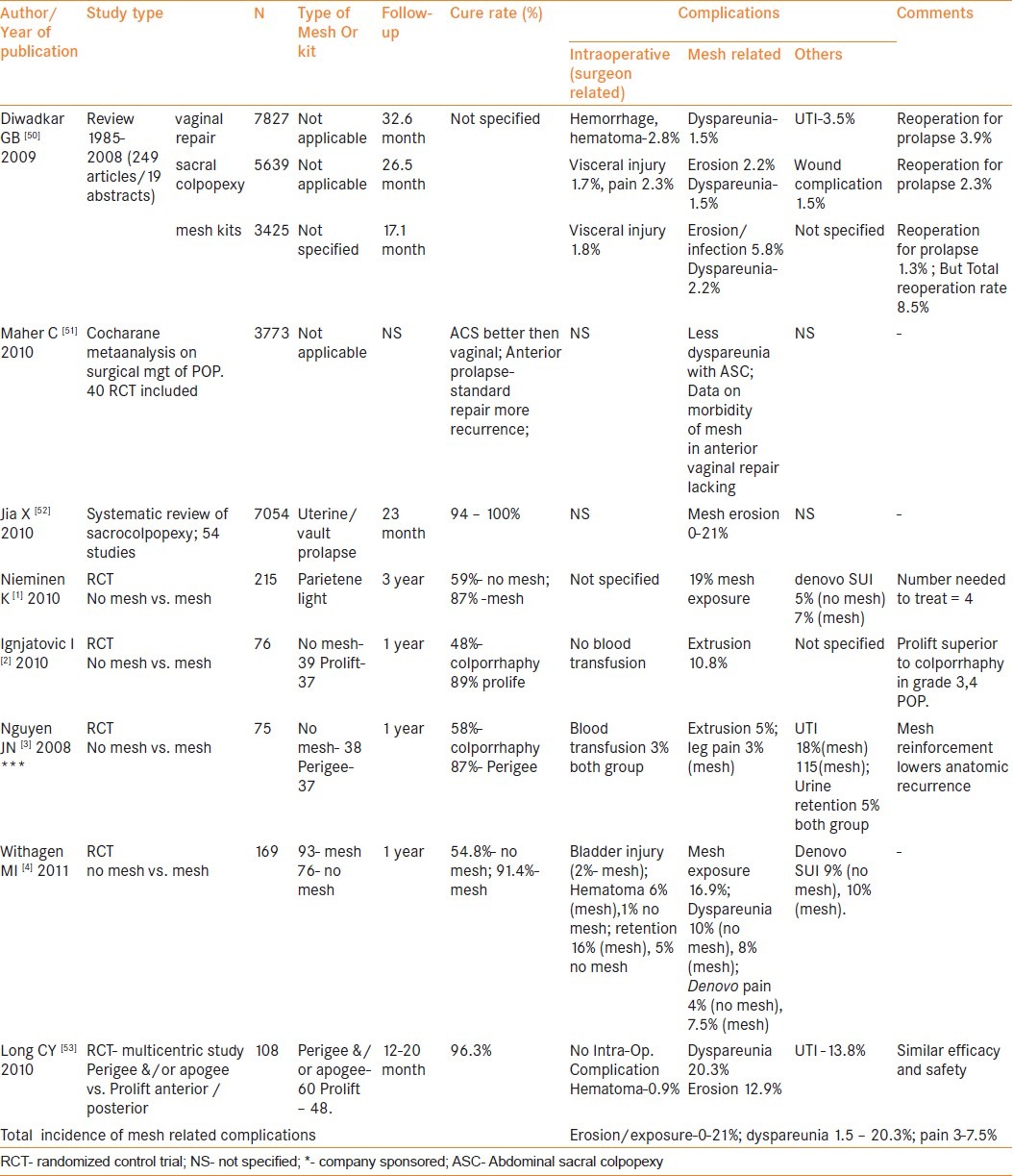
Table 9.
Review of prospective studies using synthetic mesh for transvaginal pelvic reconstructive surgery published in last 3 years
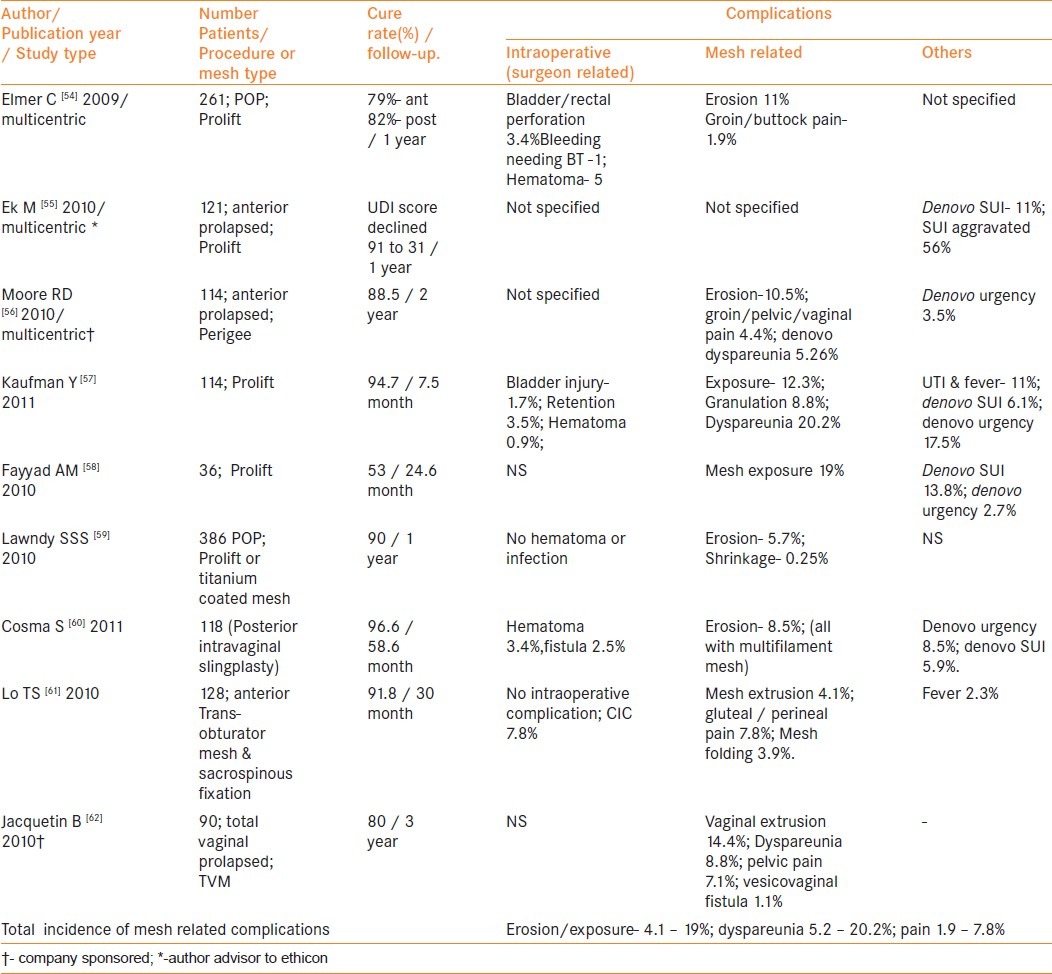
Table 10.
Review of retrospective single centre studies using synthetic mesh for transvaginal pelvic reconstructive surgery published in last 3 years.
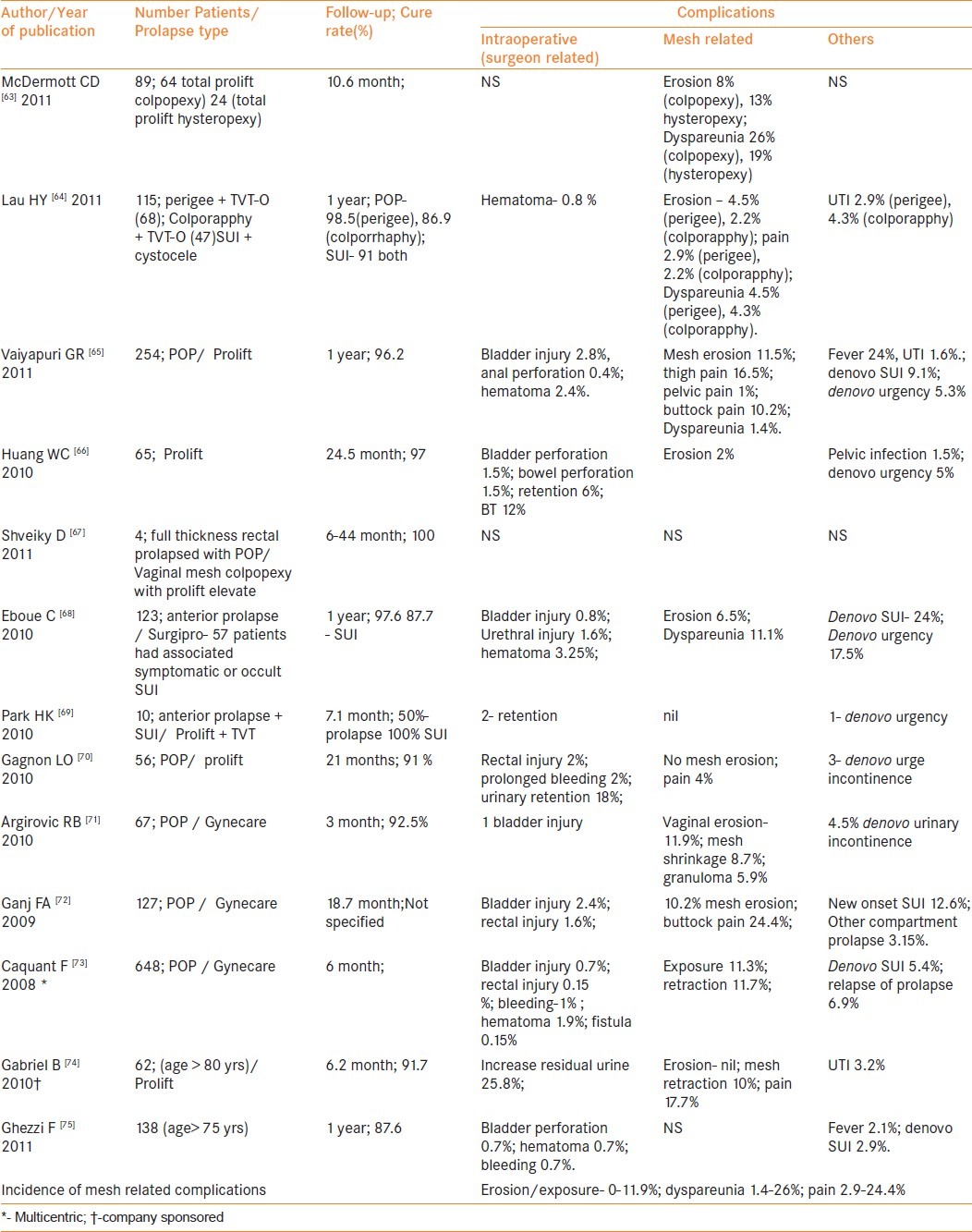
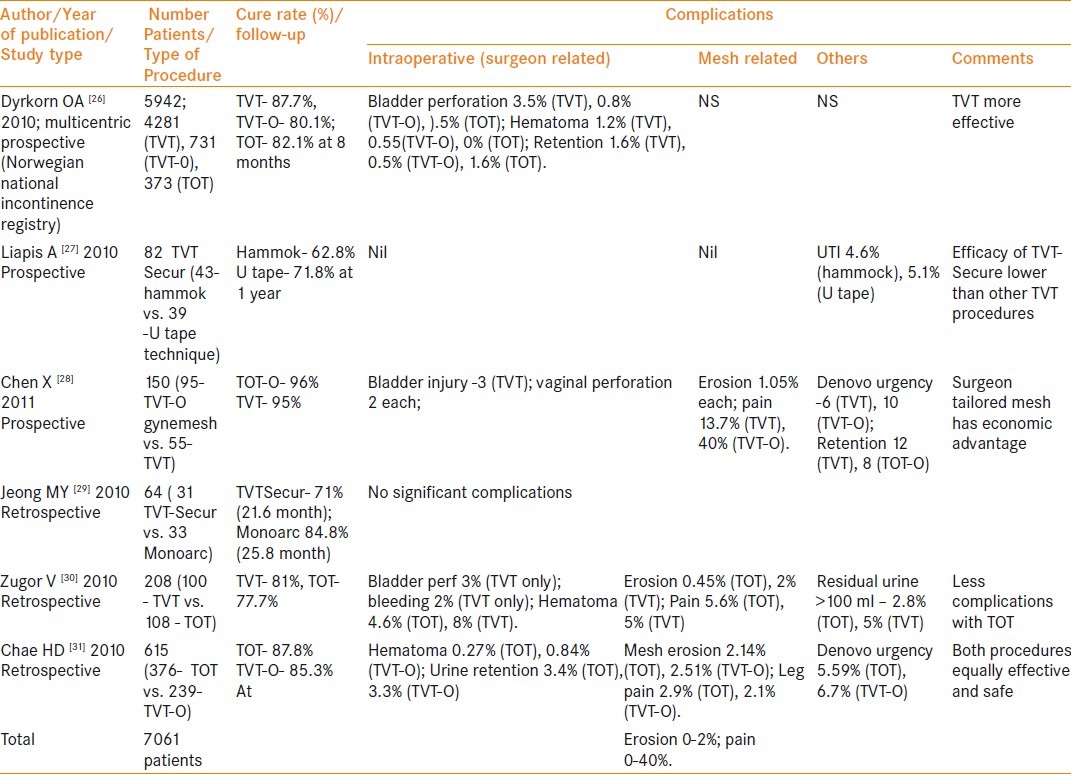
Table 4.
Review of comparative studies (prospective and retrospective) evaluating safety and efficacy of various midurethral slings for SUI published in last 3 years
Risk factors
There are no studies powered to look at the risk factors for mesh erosion following pelvic reconstructive surgery with synthetic mesh. These risk factors can be broadly divided into patient-related, mesh-related and technique or procedure-related.
Patient-related:- Patient-related risk factors include extreme of age and estrogen deficiency, severe genital atrophy, prior surgical scarring, diabetes, steroid use, and smoking. Kaufman et al., identified younger age and sexual activity as a risk factor for mesh erosions.[57] However Kim et al., noted similar extrusion rates in patients younger or older than 70 years.[35] In two retrospective series dealing with the outcome of POP repair on patients with age > 80 years, no mesh erosions were identified.[74,75] Cindiff GW et al. noted smoking to be associated with increased risk of mesh erosions.[76]
Mesh related:- Type and size of mesh may have an implication on the rate of erosions. Cindiff et al., noted that expanded PTFE meshes (Type II) were associated with a higher rate of mesh erosion then non-PTFE meshes (19% vs. 5%).[76] Silicone-coated polyethylene or polyester (Type IV) can also serve as a focus for chronic infection increasing the possibility of erosions and infections up to 23.8%.[77,78] Yamada et al., noted high vaginal erosion with the use of polypropylene non-knitted, non-woven mesh (Obtape).[79] It was hypothesized that composite mesh might minimize mesh-related complications. However, this was not noted in clinical practice [Table 11].[80–84] Other modifications of commercially available kits like trocarless mesh system and non-anchored mesh system were also associated with mesh exposure of 5% and 8% respectively [Table 11].[85,86] This proves that no mesh material is immune to erosions. Kavvadias et al., compared tissue reaction between eroded macroporous polypropylene mesh from five eroded sub-urethral sling patients with non-eroded material from a similar group of patients needing mesh removal for indications other then erosion.[87] Authors found that eroded Type 1 mesh showed a significantly more intense aggregation of macrophages at the perifilamentous area, which may indicate a stronger inflammatory reaction of the vaginal wall in eroded slings. Authors postulated that the detected foreign body reaction might be the actual trigger for the erosion. However, it is also possible that it may be a result of bacterial colonization.
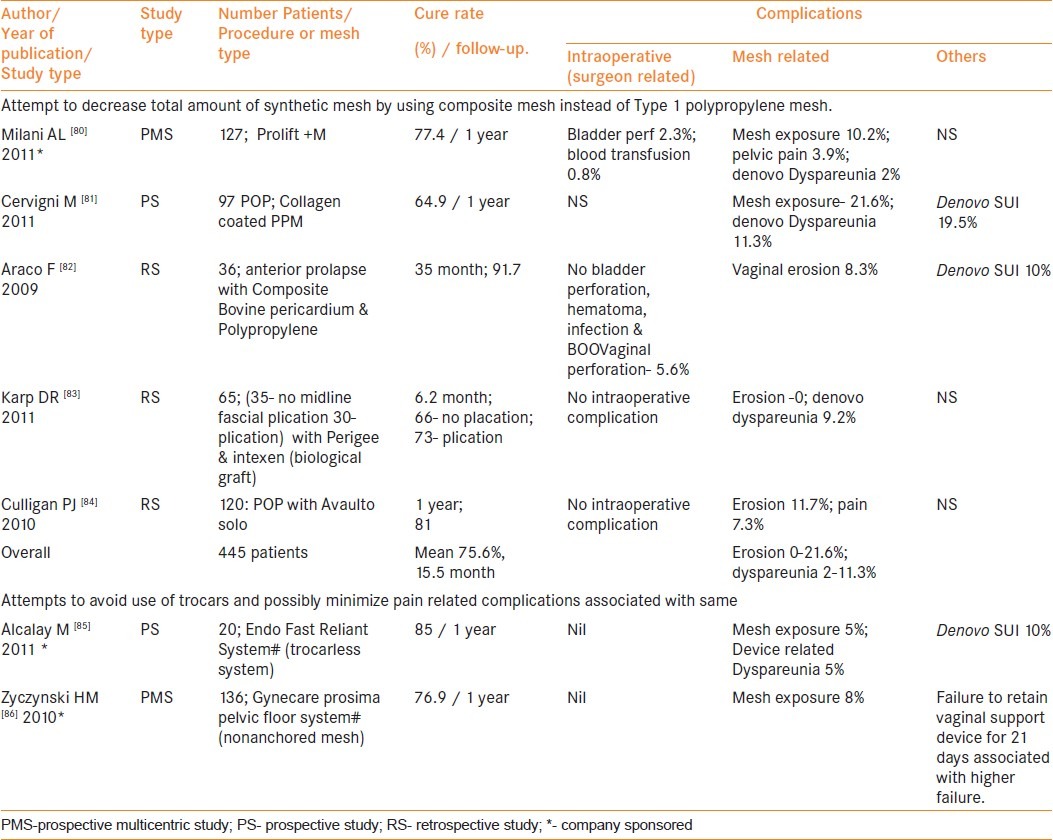
Table 11.
Review of studies using composite mesh & other kit modification for vaginal pelvic reconstructive surgery published in last 3 years
Although most of the studies confirm the safety and cost-effectiveness of surgeon-tailored mesh for vaginal reconstructive surgery, Finamore et al., found lower erosion rate with commercial kits as compared with surgeon-tailored mesh (1.4% vs. 23.6%).[88–90] In contrast to this isolated series a recent meta-analysis done by Murray et al., confirmed the safety and cost-efficacy of surgeon-tailored mesh.[91]
Recently available mini-slings for the management of SUI are associated with a lower rate of mesh erosion (0–2%) [Table 7].[43–49] An exception is an article by North et al., who reported that minitape was associated with a mesh exposure rate of 11.7% and cure rate of 10% at two-year follow-up.[46]
Procedure or surgeon-related:- Concomitant surgery, especially hysterectomy was found to increase the risk of mesh erosion.[72,76] Contrary to these reports, Stepanian et al., found that there was no increase in the risk of mesh extrusion or other mesh-related complications with concomitant hysterectomy.[92] Similarly, combining surgery for SUI and POP were not associated with any increase in mesh-related complications [Table 12].[93–99]
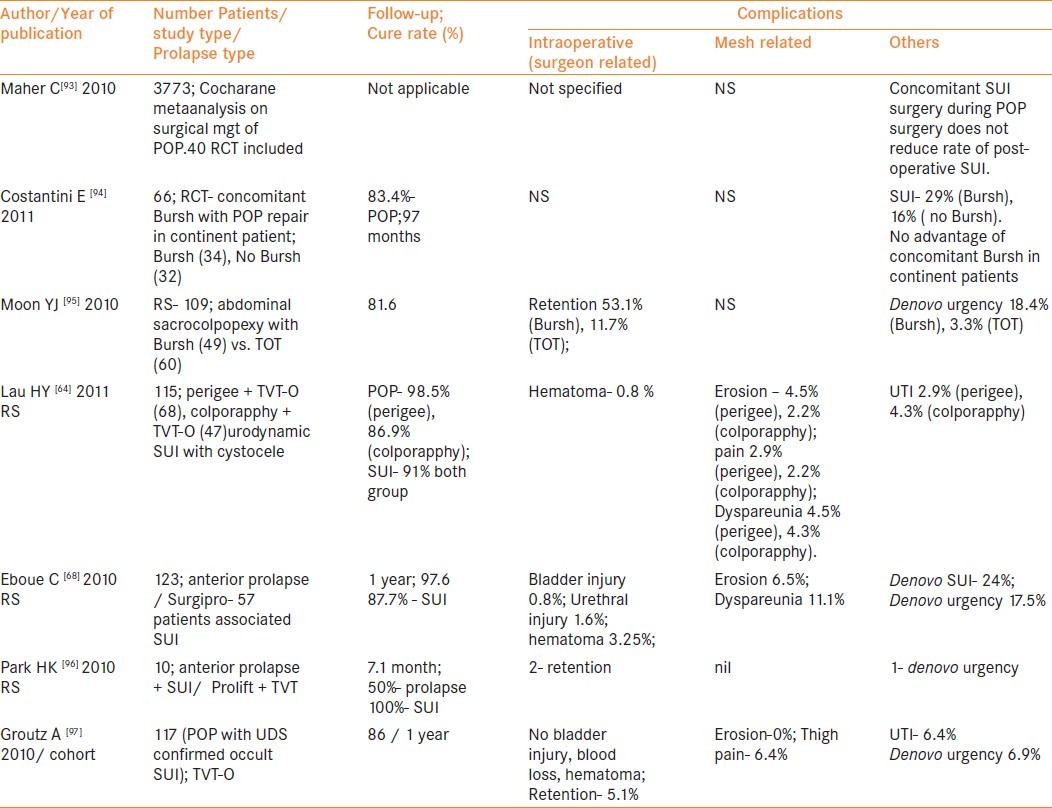
Table 12.
Review of literature on concomitant sling with POP repair published in last 3 years
Ganj et al., believe that the most important factor to reduce mesh complications is to minimize the length of the incisions and closure of the incisions without tension[72]. Anchoring the mesh may also be associated with a lower mesh erosion rate by preventing ‘puckering’ movement and extrusion through the vaginal incision. Margulies et al., identified mesh folding in nine out of 13 patients suffering from vaginal mesh extrusion. Authors believed that mesh folding might be an important contributing factor in mesh exposure because a folded mesh does not lie flat against the vaginal wall.[98] Placement of sling in a plane too close to the urethra or the presence of inadequate vaginal tissue coverage, poor vaginal tissue vascularity, or bacterial infection secondary to a draining hematoma or seeding of the mesh may lead to early sling erosions/extrusions.[99]
In a meta-analysis of 11 randomized control trials (RCT), Long et al., noted a higher incidence of vaginal erosions after mid-urethral sling placement by transobturator route. However, this was not confirmed by Latthe et al., in their meta-analysis of 31 RCT [Table 2].[12,13] Lee et al., modified the technique and recommended “canal transobturator-tape (TOT)” in which two oblique lateral incisions were made in the anterior vaginal wall and a suburethral canal was created between the incisions.[38] Mesh was transferred beneath the canal. Authors felt that canal TOT more precisely dissects the layer between the periurethral fascia and the urethra thereby reducing the rate of erosions. Adjustable slings were introduced to minimize the incidence of postoperative voiding dysfunction after surgery for SUI. Surprisingly, there was no incidence of mesh erosion in 365 patients reportedly treated with these slings in the last three years [Table 6].[39–42]
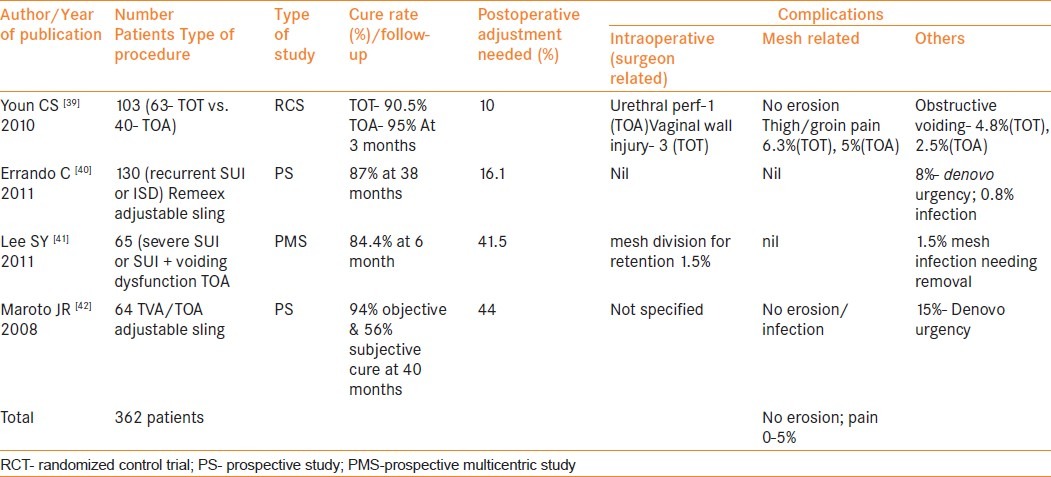
Table 6.
Review of literature on adjustable slings for SUI published in last 3 years
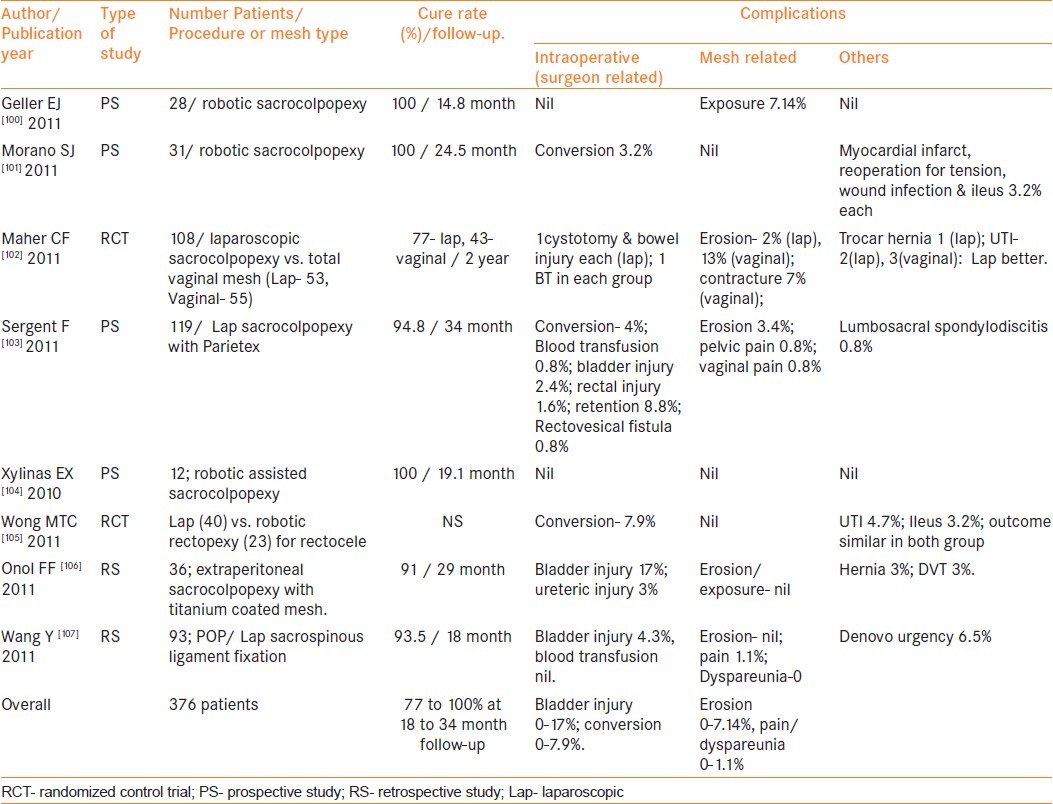
On comparing various approaches for POP repair, laparoscopic or robotic approach was associated with a lower incidence of mesh-related complications when compared with vaginal approach [Table 13].[100–107] A crucial factor, which has made the most significant impact on the extrusion rate, is the depth of the vaginal dissection, i.e.- raising full-thickness vaginal flaps is believed to minimize erosions.
Table 13.
Review of studies on laparoscopic &/or robotic approach for pelvic reconstructive surgery published in last 3 years
Clinical presentation
The presenting symptoms vary depending on the organ involved. For example, vaginal mesh extrusion may result in vaginal bleeding, abnormal discharge, dyspareunia or vaginal pain [Figure 2]. Symptoms of mesh erosion into the bladder/urethra include painful voiding, urinary frequency, urgency, hematuria, recurrent urinary tract infection, urinary calculi and urinary fistula.
Figure 2.
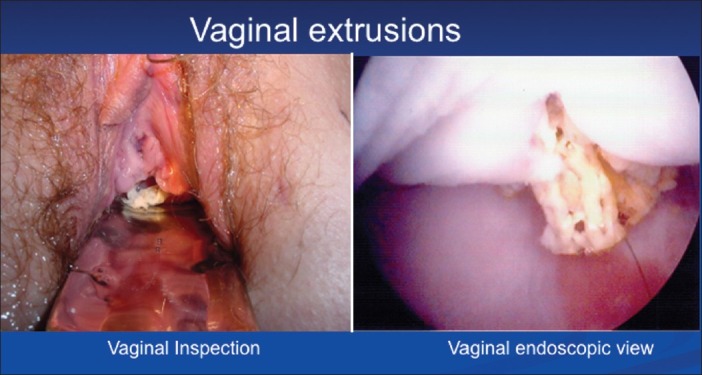
Mesh extrusion
Treatment
There is limited data on the optimal cost-effective management of mesh exposure. No single approach is suitable for all cases, and the choice of the technique used should be based on the location of the extrusion, its magnitude and severity and associated recurrence of SUI and/or urinary retention [Tables 14–16].[108–148]
Table 14.
Literature regarding various conservative and open surgical modalities for management of mesh related complications from Jan 2005 to March 2011 (except endoscopic and laparoscopic approach) (Total number of patients = 250)
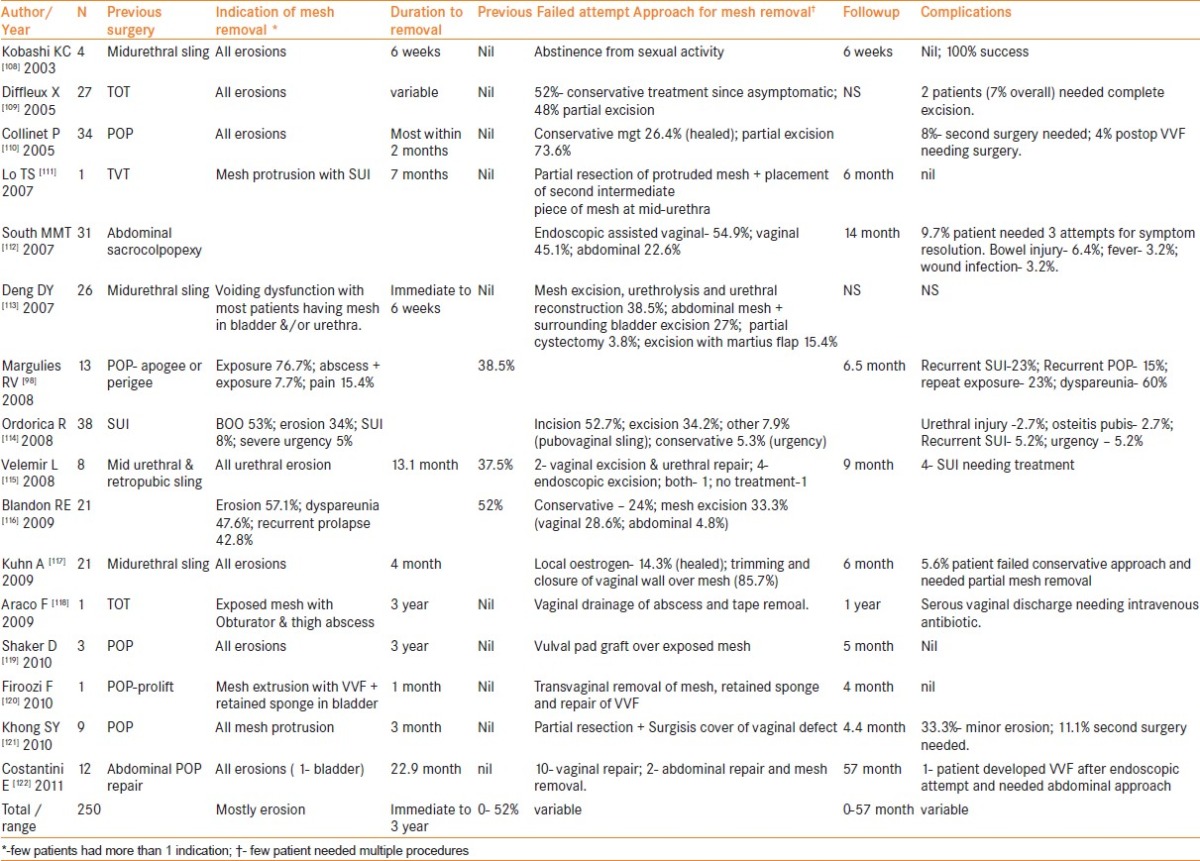
Table 16.
Literature on laparoscopic mesh removal reported from Jan 2005 to March 2011. (N = 102)
Management of mesh exposure /vaginal extrusion
In all the cases of mesh exposure, it would be pragmatic to rule out simultaneous erosion into the urethra or bladder by cystoscopy.
Conservative management
It should be initially attempted, especially in small vaginal mesh exposure. Patient is advised to abstain from intercourse.[108] Local application of estrogen cream might allow a layer of vaginal mucosa to grow and cover the sling.[114] Based on patient selection, this may be helpful in 0–100% cases [Table 14].
Vaginal approach
It is the most preferred approach and usually performed under general or spinal anesthesia in order to have adequate exploration of mesh [Table 14].
Partial removal of mesh
The extruded part of the mesh is removed and the remaining mesh is carefully examined for signs of infection. The vagina is closed with mobilized flap to cover the defect using absorbable sutures [Figure 3].
Figure 3.
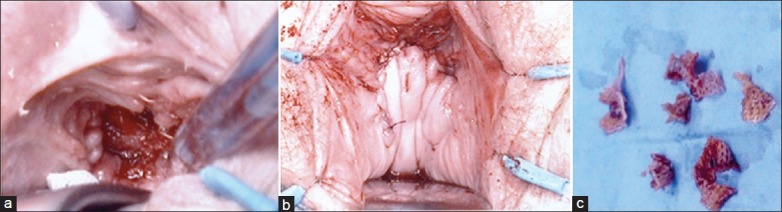
(a) Partial excision of mesh extrusion by vaginal approach; (b) final appearance of vagina after mesh excision; (c) excised mesh pieces
Complete removal of mesh
A midline full-thickness incision is performed on the anterior vagina, extending up to 2-3 cm from the urethral meatus. The bladder is dissected away from the vaginal wall, and the arcus tendineous of the levator ani are reached. The body of the mesh is trapped and the surrounding tissues are carefully dissected away. The mesh is then removed from under the bladder, and the arms from the para-vesical fossas. The vagina is closed with running locked absorbable suture. This can be done in the acute or immediate postoperative situation of hematoma and/or infection resulting in mesh exposure. This is extremely difficult later on when done for graft-related pain or contracture. Biological mesh can be used to manage the defect following complete explantation of synthetic mesh immediately or in a staged fashion.
Conservative mesh-preserving approach
This includes vulval pad graft coverage over the exposed mesh as recently described by Shaker et al.[119]
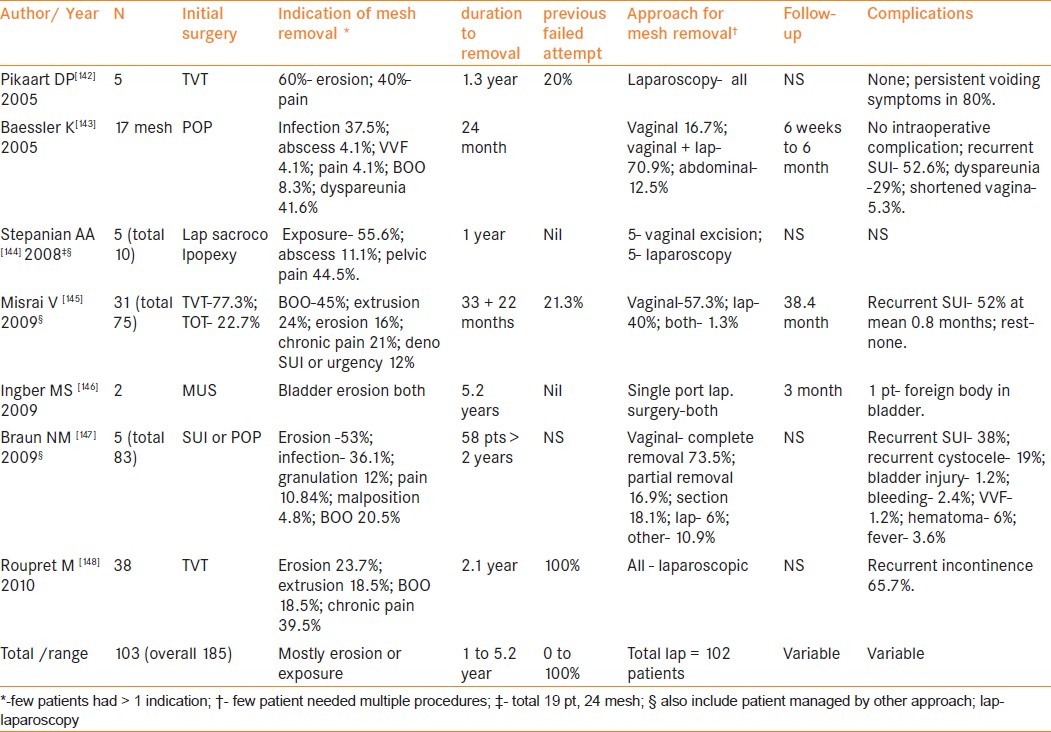
Laparoscopic approach
Extraperitoneal approach is usually adapted to reach the Retzius space. The dissection is carried out until the Cooper's ligaments and the urethra are reached anteriorly and the arcus tendineous fascia pelvis posteriorly, followed by dissection of mesh from the pelvic walls. In case of urinary obstruction, the remaining mesh is removed through vaginal approach. It is usually employed for cases in which previous vaginal approach has failed.[148] Transvesical laparoscopic port can also aid in transurethral endoscopic removal of mesh that has eroded in the bladder [Table 15].[136–141] Recently, even single-port laparoscopic surgery has been described for the removal of mesh eroded in the bladder.[146] The details of various series reported on laparoscopic or robotic mesh removal are summarized in Table 16.[142–148]
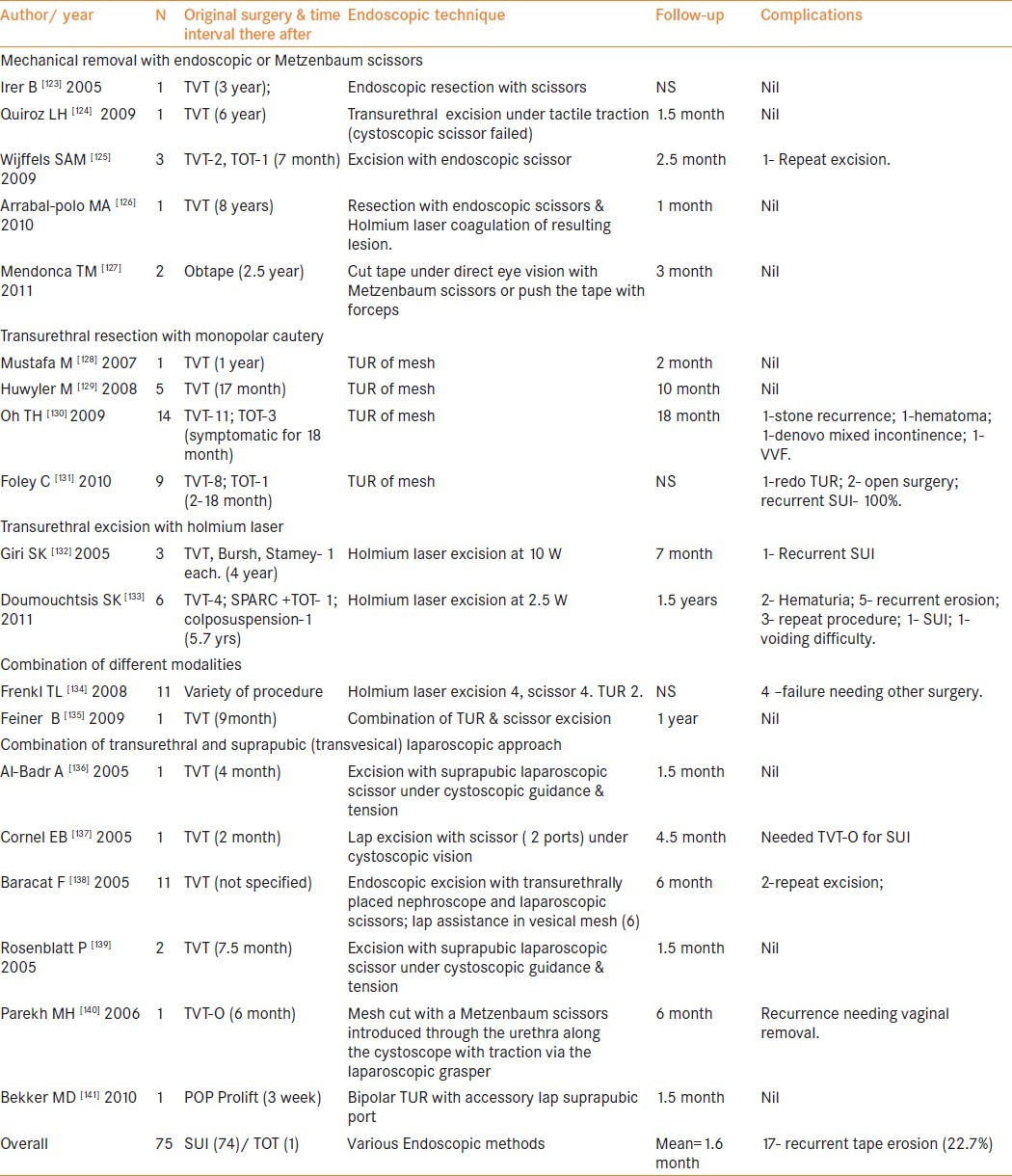
Table 15.
Review of reports on endoscopic management of mesh erosion into bladder or urethra from Jan 2005 to March 2011 in English literature
Management of intravesical/intraurethral mesh erosion
The recommended management is removal of the mesh from the bladder or urethra.
Open surgery (Vaginal or abdominal approach)
Open cystotomy through suprapubic or retropubic approach can be used for intravesical erosion. Some patients may need partial cystectomy if significant amount of mesh had eroded in the bladder wall.[113] Urethral erosion may need open excision and urethral reconstruction via vaginal approach [Figure 4]. Anjulo et al., described three patients of sub-urethral erosion and secondary severe urethral stricture who needed total extirpation of the mesh and complete reconstruction of the urethro-vaginal septum. The technique included combined urethroplasty with bladder flap and vaginal reinforcement with pediculated vaginal flap transferred in a mini-sling fashion.[149] Interposition of the Martius graft has been advocated in such a scenario to reduce the risk of urethrovaginal fistula.[150]
Figure 4.
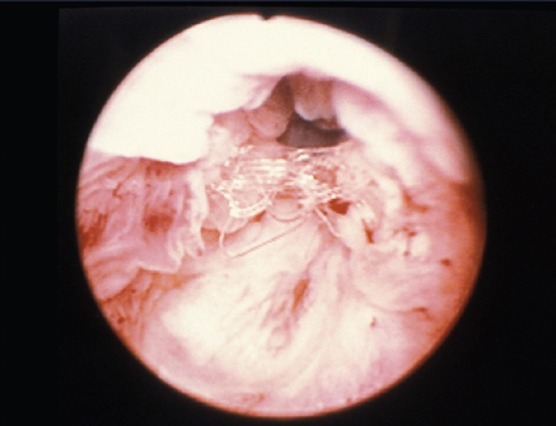
Urethral mesh erosion
Laparoscopic approach
Pure laparoscopy or laparoscopic-assisted endoscopic removal of mesh in the bladder has been described [Tables 15 and 16]. There are no major intraoperative complications, but it is associated with postoperative recurrent incontinence in up to 65.7%.[148]
Endoscopic approach
Mechanical removal with scissors- Cystoscopic excision of mesh eroded in bladder or urethra is described using endoscopic scissors [Table 15]. Transurethral nephroscopy with use of laparoscopic scissors has also been described.[138] It also may be of advantage to have a suprapubic transvesical laparoscopic port to give traction on mesh thereby assisting in excision with endoscopic scissors.[136–141] Use of transurethral nasal speculum or Metzenbaum scissors by the side of an endoscope may also be useful in some scenarios.[127]
Transurethral resection (TUR) of mesh – It completely resects intravesical mesh as well as the infiltrated muscle around the mesh with a resectoscope loop similar to transurethral surgery of bladder tumors. Although the polypropylene mesh itself is not an insulator, muscle infiltrated mesh can be resected with high-voltage electric current. Oh et al., employed this technique in 14 patients and noted that mesh could be completely removed in 13 patients with only one patient developing recurrent stone at a mean follow-up of 18 months.[130] Some patients may need multiple TUR for complete mesh excision [Table 15].[131] The possible complications of this approach include extraperitoneal bladder rupture and vesicovaginal fistula formation.[130] This technique is not recommended for urethral erosion, due to higher possibility of incomplete removal and urethral perforation. To avoid complications associated with monopolar cautery, Bekker et al., recently described bipolar TUR for excision of intravesical mesh.[141]
Transurethral endoscopic excision using Holmium laser (TEEH)- It has been described as an alternative to electric current at a setting ranging from 2.5 to 10 W. Of the nine patients described since 2005, six developed recurrence over a short follow-up of slightly above one year.[132,133]
It is not uncommon to have strands remaining when endoscopic small shears or laser is used to remove the mesh, these can continue to pose a problem, thus we find the open or intravesical laparoscopic approach the most efficient for the bladder and endoscopic best for urethral erosion.
Erosion in bowel
Although rare, enterovaginal fistula or colovaginal fistula with or without local abscess have been reported in the literature. The possible mechanisms are intraoperative injury, mechanical injury by mesh alone or in conjuction with local sepsis.[151,152]
MESH INFECTION
This may be associated with or without vaginal mesh exposure. Various pathogens have been implicated, including Gram-positive and Gram-negative aerobic and anaerobic bacteria. They are usually linked to the type of mesh material and are now a rarity since the generalized use of knitted polypropylene monofilament implants.[153]
Incidence
Incidence ranges from 0–8%.[18]
Risk factors
Factors related to the development of mesh infection include types of mesh material, procedure, preventive measures taken, age and underlying comorbidity of the subject. Type II, III and IV meshes due to their inherent property are predisposed to develop mesh infection. Clave et al., on analyzing 100 explants, noted that multifilament polypropylene, non-knitted, non-woven polypropylene and composite implants were more frequently associated with infection than monofilament polypropylene implants (70% vs. 39%).[154] Limited dissection with gentle tissue handling, meticulous attention to hemostasis, would help to minimize hematoma formation and bacterial colonization. Peri-operative antibiotic, thorough antisepsis of the perineum, vulva and vagina and covering the anus at surgery are important infection prevention strategies. There is no conclusive evidence that embedding the mesh in antiseptic solution may play a crucial role.[155] It is also important to avoid performing a diagnostic paracentesis of mesh-related seromas, when there are no symptoms and/ or signs of inflammation. Such a procedure could transform an aseptic reaction into an infectious process.
Effect of infection of mesh material
Contrary to the prevailing understanding of polypropylene as an inert material when used in vaginal surgeries, Clave et al., in their study of 100 explants noted that all polypropylene implants showed evidence of degradation on scanning electron microscopy after three months.[154] Mesh damage included superficial degradation, which appeared as peeling of the fiber surface, transverse cracks in the implant threads, significant cracks with disintegrated surfaces and partially detached material, and superficial and deep flaking. Fractures were variable in number and depth. Authors described several hypotheses concerning the degradation of the polypropylene including direct oxidation, fatty acid diffusion and oxidation due to free radical attack. It was noted that polypropylene implants degraded more in the presence of an acute infection or chronic inflammation. However, none of the poly(ethylene terephthalate) was found to be altered or degraded. Hence authors expressed a need for clinical trials to comparatively investigate the performance of new type of monofilament meshes, such as poly(ethylene terephthalate).
Clinical presentation
Non-specific pelvic pain, persistent vaginal discharge or bleeding, dyspareunia, and urinary or fecal incontinence are the most common manifestations of vaginal mesh-related infection. Clinical examination may reveal induration of the vaginal incision, vaginal granulation tissue, draining sinus tracts and prosthesis erosion or rejection. A mesh-related infection may sometimes present as a pelvic abscess, urogenital or other fistulas, discharging sinus or osteomyelitis. Mesh-related infection in the form of thigh abscess has also been reported to manifest even five years after initial surgery.[156]
Treatment
Mesh infection requires removal of the whole mesh either transvaginally or abdominally. This is accompanied with drainage of abscess cavities and administration of intravenous or oral antibiotics. Additionally, microbiological studies of removed meshes are recommended to guide appropriate antimicrobial management postoperatively.[18] Use of copious local irrigation with antimicrobials is recommended in such a scenario.
MESH RETRACTION
Retraction of tissues surrounding the mesh is usual with a reduction in the size of the mesh. The average shrinkage is 25–30% in experimental surgery on the rat's abdominal wall; it may reach 40% of the initial surface of the implant in the patients after surgery. Therefore, many surgeons use large implants to cover defects, and anticipate scarring, shrinkage and puckering. Lo et al., found 19.6% reduction in the length of mesh on ultrasonography at one month postoperatively.[157] However, contrary to these findings, Dietz et al., found no evidence of mesh contraction in their patients.[158] The authors performed four-dimensional ultrasound at 3-53 months in 40 women, at least twice in each to measure mesh dimensions at two time points after implantation. However, objective recurrence of cystocele was seen in 16 patients in this study.
Clinical presentation
Normal urinary, sexual and defecatory functions require a vagina that is compliant and whose walls can easily and painlessly change conformation. With excessive stiffness of the vaginal walls, secondary to the mesh that has undergone shrinkage, it is possible that dyspareunia, defecatory, and urinary dysfunction could result.[98] Mesh shrinkage can expose a patient to recurrence of previous prolapse or SUI since the defect is no longer better covered. Patients may have pain of varying frequency and various natures including “tenderness” at palpation of the mesh, painful intercourse or pain when doing physical exercise. It is important to assess the impact of this pain on the quality of life using validated questionnaire scales. The exact responsibility of the retraction may be difficult to assert, but it seems likely if palpation of the retracted implant arises a pain similar to the patient's description. Retraction may also be appreciated on palpation. In a series of 17 women described by Feiner B and Maher C recently, clinical presentation included severe vaginal pain aggravated by movements and focal tenderness over contracted portions of mesh on vaginal examination in all patients.[159] Additionally, dyspareunia was seen in all sexually active patients. Associated clinical findings were mesh erosion (9 of 17), vaginal tightness (7 of 17) and shortening (5 of 17).
Treatment
Initially, medical management must be tried including painkillers, local hormonal therapy and local anti-inflammatory drug injections. If symptoms persist surgery might be required. The goal of surgical management is to relieve the tension by dividing the central graft from the arms and excising all areas of mesh contraction after mobilizing it from underlying tissues.[159] In a case series of 17 patients who presented with mesh contraction after repair of pelvic prolapse using synthetic mesh, Feiner et al., reported that postoperatively 88% women experienced substantial reduction in vaginal pain and 64% experienced substantial reduction in dyspareunia. In the author's experience, repeat excision of entire accessible mesh was required in 17.7% patients because of persisting symptoms. Since these patients are challenging to manage surgically, they should be referred to an expert centre where a limited or a large excision, rarely a total removal may be done effectively.[153]
DYSPAREUNIA
Dyspareunia may be caused by mesh erosion, mesh infection, mesh shrinkage or extensive fibrosis. A recent meta-analysis reported an overall incidence of 9.1% in 70 studies analyzed.[91] On reviewing the literature on the management of SUI over a period of the last three years we noted that the incidence of dyspareunia was noted in up to 6.2% patients [Table 5]. However, the incidence was reported significantly higher after POP surgery, approaching up to 24.4% [Table 10].
Table 5.
Review of case series using various midurethral slings for SUI published in last 3 years
Interestingly, there was no difference in the rates of dyspareunia while using absorbable and non-absorbable mesh at one year.[160] Similarly, in a recently published study the use of mesh was not associated with an increase in dyspareunia as compared with anterior colporapphy alone.[1,4] A concurrent procedure combined with mid- urethral sling can increase the possibility of postoperative dyspareunia. Cholhan et al., noted that postoperative de novo dyspareunia after TOT was associated with a phenomenon they call “Para-urethral banding”, which are palpable bands in the urethral folds.[161] These bands were only observed in patients undergoing TOT procedure and contributed to a substantial rate of dyspareunia (24%). Similarly, new-onset dyspareunia after transobturator tape TVT-O procedure was attributable to posterior migration of the tape, which could be palpated close to the anterior vaginal fornix.[162] In the authors’ experience cutting the tape in the midline successfully treated all four patients. However, it may become an indication for mesh removal.[143]
In an interesting study by Mohr et al., male dyspareunia (hispareunia) was evaluated in male partners of 32 patients who underwent surgery for mesh extrusion.[163] They noted that visual analogue scale VAS score as a measurement of hispareunia significantly improved from median score of 8 to 1 after intervention of their female partners for mesh extrusion.
PAIN
Chronic pelvic pain often presents as a serious and challenging problem after use of synthetic mesh for pelvic floor reconstruction.[164] Groin and thigh pain is a potential problem of mid-urethral sling placement, especially transobturator slings. It has been reported in up to 40% patients after transobturator sling placement.[28] A recent meta-analysis revealed that it was more common in inside-to-outside transobturator approach.[13] Its incidence can be decreased by newly introduced mini-slings, which reported a lower incidence of pain ranging from 0–3.3% only [Table 7]. In POP surgery, the incidence of pain reported in various publications over the last three years is 1.9–24.4% [Table 8–10]. If initial conservative management with anti-inflammatory medications fails to relieve pain, a few patients may need removal of mesh with its attendant risk of recurrence of pelvic floor defect.
United States Food and Drug Administration, manufacturer and user facility device experience (MAUDE) on use of vaginal mesh in female pelvic floor reconstruction
MAUDE data represents reports of adverse events involving medical devices. The data consists of all voluntary reports since June 1993, user facility reports since 1991, distributor reports since 1993, and manufacturer reports since August 1996 and is updated on a monthly basis.[15] There are more than 2310 complications reported with the search criteria of “vaginal mesh” till March 2011. The incidence of complications reported under various search criteria till March 2011 is given in Table 17. A steep increase in the incidence of reported complications with search criteria “vaginal mesh” and “mesh erosion” is noted in the MAUDE database [Figure 5].
Table 17.
The incidence of complications reported under various search criteria till March 2011 in MAUDE database-
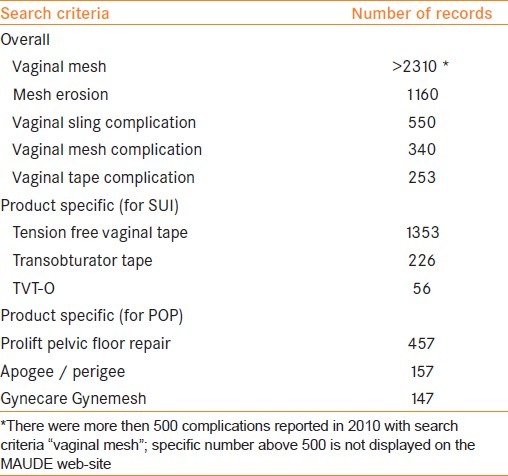
Figure 5.
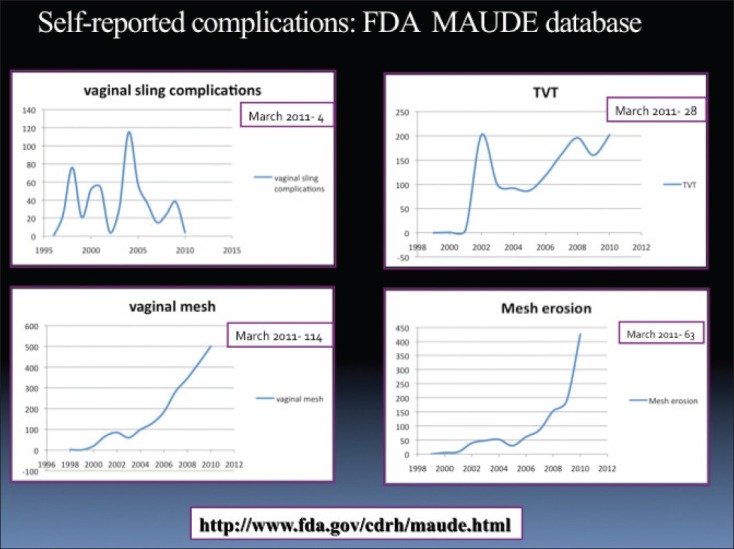
Incidence of complications reported under various search criteria till March 2011 in the MAUDE database. The incidence till the year 2010 is plotted in the graph; while the number of cases reported in the present year till March 2011 is reflected with in number on right upper quadrant of each graph
In October 2008, the US Food and Drug Administration's (FDA's) Centre for Devices and Radiological Health, issued a warning on higher-than-expected complications reported for use of mesh in transvaginal surgeries.[165] The FDA warning states: “Over the past three years, the FDA has received over 1,000 reports from nine surgical mesh manufacturers of complications that were associated with surgical mesh devices used to repair POP and SUI…The most frequent complications included erosions through vaginal epithelium, infection, pain, urinary problems, and recurrence of prolapse and/or incontinence. There were also reports of bowel, bladder, and blood vessel perforation during insertion. In some cases, vaginal scarring and mesh erosion led to a significant decrease in patient quality of life due to discomfort and pain, including dyspareunia.
On July 13, 2011, the FDA stated in a news release, “There are clear risks associated with the transvaginal placement of mesh to treat POP.” It further stated “The FDA issued a safety communication in 2008 due to increasing concerns about adverse events associated with the transvaginal placement of mesh. Since then, the number of adverse events has continued to climb. From 2008 to 2010, the FDA received 1503 adverse event reports associated with mesh used for POP repair, five times as many as the agency received from 2005 to 2007.” This safety communication was “limited to the transvaginal placement of mesh to repair POP. It does not address the safety and effectiveness of mesh used to treat SUI or mesh implanted abdominally.[166]”
CONCLUSIONS
Sub-urethral sling procedures using synthetic meshes are now considered the gold standard for the surgical management of stress urinary incontinence with estimated cure/dry rates ranging from 81–84%.[167] It is also now increasingly used in the management of pelvic floor prolapse. It is imperative that we understand the complications associated with these surgeries. Awareness of these complications should help us in proper patient counseling as well as stimulate further investigations of the underlying mechanisms. Decreasing complications should be considered an important outcome in future clinical studies. The incidence of extrusion and erosion with mid-urethral sling is low, the extrusion with prolapse is higher and use in the posterior compartment remains controversial. When used through the abdomen the extrusion and erosion rates are lower. There is an FDA warning about the use of mesh in pelvic organ prolapse.[166] However, with appropriate counseling these may still be indicated after the surgeon and the patient take into account the benefits and complications thereof. In spite of certain perceived problems with the use of mesh in incontinence procedures, it seems to be safe and beneficial to the patient.
What is needed in future?
Surgical management of SUI continues to evolve. The rapid expansion of the market does not await results of the RCTs, a newer and more competitive product could be on the market. This might be the reason why only a few companies and centers are interested in setting up RCTs. Still it is important not to fall prey to industry-driven treatment options, but to follow evidence-based medicine in managing our patients. Ou et al., stressed the impact of attrition rate of follow-up with time that directly affects the strength of Level 1 and 2 studies regarding surgical treatment of female SUI.[168] The incidence of patients lost to follow-up was 8.1% at 12 months, 28% at 24 months, 36% at 36 months and 32.4% at 60 months or greater. Hence it is important to cautiously analyze results of various published studies in the literature. It is also of paramount importance that national societies should establish a registry for complications. There should be a protocol of recording all complications in this registry so as to know the true incidence of morbidities associated with different surgical procedures. Need of proper surgical training and experience in placing vaginal meshes need not be under emphasized.[169,170] In order to record the denominator, the industry should consider a form with each kit to record and follow its use.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Nieminen K, Hiltunen R, Takala T, Heiskanen E, Merikari M, Niemi K, et al. Outcomes after anterior vaginal wall repair with mesh: A randomized, controlled trial with a 3 year follow-up. Am J Obstet Gynecol. 2010;203(235):e1–8. doi: 10.1016/j.ajog.2010.03.030. [DOI] [PubMed] [Google Scholar]
- 2.Ignjatovic I, Stojkovic I, Basic D, Medojevic N, Potic M. Optimal primary minimally invasive treatment for patients with stress urinary incontinence and symptomatic pelvic organ prolapse: Tension free slings with colporrhaphy, or Prolift with the tension free midurethral sling? Eur J Obstet Gynecol Reprod Biol. 2010;50:97–101. doi: 10.1016/j.ejogrb.2010.01.009. [DOI] [PubMed] [Google Scholar]
- 3.Nguyen JN, Burchette RJ. Outcome after anterior vaginal prolapse repair: A randomized controlled trial. Obstet Gynecol. 2008;111:891–8. doi: 10.1097/AOG.0b013e31816a2489. [DOI] [PubMed] [Google Scholar]
- 4.Withagen MI, Milani AL, den Boon J, Vervest HA, Vierhout ME. Trocar-guided mesh compared with conventional vaginal repair in recurrent prolapse: A randomized controlled trial. Obstet Gynecol. 2011;117(2 Pt 1):242–50. doi: 10.1097/AOG.0b013e318203e6a5. [DOI] [PubMed] [Google Scholar]
- 5.Boreham MK, Wai CY, Miller RT, Schaffer JI, Word RA. Morphometric analysis of smooth muscle in the anterior vaginal wall of women with pelvic organ prolapse. Am J Obstet Gynecol. 2002;187:56–63. doi: 10.1067/mob.2002.124843. [DOI] [PubMed] [Google Scholar]
- 6.Chen Y, DeSautel M, Anderson A, Badlani G, Kushner L. Collagen synthesis is not altered in women with stress urinary incontinence. Neurourol Urodyn. 2004;23:367–73. doi: 10.1002/nau.20006. [DOI] [PubMed] [Google Scholar]
- 7.Kushner L, Mathrubutham M, Burney T, Greenwald R, Badlani G. Excretion of collagen derived peptides is increased in women with stress urinary incontinence. Neurourol Urodyn. 2004;23:198–203. doi: 10.1002/nau.10174. [DOI] [PubMed] [Google Scholar]
- 8.Karlovsky ME, Kushner L, Badlani GH. Synthetic biomaterials for pelvic floor reconstruction. Curr Urol Rep. 2005;6:376–84. doi: 10.1007/s11934-005-0057-7. [DOI] [PubMed] [Google Scholar]
- 9.Nilsson CG, Palva K, Rezapour M, Falconer C. Eleven years prospective follow-up of the tension-free vaginal tape procedure for treatment of stress urinary incontinence. Int Urogynecol J Pelvic Floor Dysfunct. 2008;19:1043–7. doi: 10.1007/s00192-008-0666-z. [DOI] [PubMed] [Google Scholar]
- 10.Song PH, Kim YD, Kim HT, Lim HS, Hyun CH, Seo JH, et al. The 7-year outcome of the tension-free vaginal tape procedure for treating female stress urinary incontinence. BJU Int. 2009;104:1113–7. doi: 10.1111/j.1464-410X.2009.08504.x. [DOI] [PubMed] [Google Scholar]
- 11.Olsson I, Abrahamsson AK, Kroon UB. Long-term efficacy of the tension- free vaginal tape procedure for the treatment of urinary incontinence: A retrospective follow-up 11.5 years post-operatively. Int Urogynecol J Pelvic Floor Dysfunct. 2010;21:679–83. doi: 10.1007/s00192-009-1083-7. [DOI] [PubMed] [Google Scholar]
- 12.Long CY, Hsu CS, Wu MP, Liu CM, Wang TN, Tsai EM. Comparison of tension-free vaginal tape and transobturator tape procedure for the treatment of stress urinary incontinence. Curr Opin Obstet Gynecol. 2009;21:342–7. doi: 10.1097/GCO.0b013e32832e07bf. [DOI] [PubMed] [Google Scholar]
- 13.Latthe PM, Singh P, Foon R, Toozs-Hobson P. Two routes of transobturator tape procedures in stress urinary incontinence: A meta-analysis with direct and indirect comparison of randomized trials. BJU Int. 2010;106:68–76. doi: 10.1111/j.1464-410X.2009.09051.x. [DOI] [PubMed] [Google Scholar]
- 14.Rehman H, Bezerra CC, Bruschini H, Cody JD. Traditional suburethral sling operations for urinary incontinence in women. Cochrane Database Syst Rev. 2011;1:CD001754. doi: 10.1002/14651858.CD001754.pub3. [DOI] [PubMed] [Google Scholar]
- 15. [Last accessed on 2011 Aug 01]. Available from: http://www.fda.gov/Medical Devices/DeviceRegulationandGuidance/PostmarketRequirements/ReportingAdverseEvents/ucm127891.htm .
- 16.Amid PK, Shulman AG, Lichtenstein IL, Hakakha M. Biomaterials for abdominal wall hernia surgery and principles of their applications. Langenbecks Arch Chir. 1994;379:168–71. doi: 10.1007/BF00680113. [DOI] [PubMed] [Google Scholar]
- 17.Haylen BT, Freeman RM, Swift SE, Cosson M, Davila GW, Deprest J, et al. An International Urogynecological Association (IUGA)/International Continence Society (ICS) joint terminology and classification of the complications related directly to the insertion of prostheses (meshes, implants, tapes) and grafts in female pelvic floor surgery. Neurourol Urodyn. 2011;30:2–12. doi: 10.1002/nau.21036. [DOI] [PubMed] [Google Scholar]
- 18.Falagas ME, Velakoulis S, Iavazzo C, Athanasiou S. Mesh-related infections after pelvic organ prolapse repair surgery. Eur J Obstet Gynecol Reprod Biol. 2007;134:147–56. doi: 10.1016/j.ejogrb.2007.02.024. [DOI] [PubMed] [Google Scholar]
- 19.Abed H, Rahn DD, Lowenstein L, Balk EM, Clemons JL, Rogers RG For the Systematic Review Group of the Society of Gynecologic Surgeons. Incidence and management of graft erosion, wound granulation, and dyspareunia following vaginal prolapse repair with graft materials: A systematic review. Int Urogynecol J. 2011;22:789–98. doi: 10.1007/s00192-011-1384-5. [DOI] [PubMed] [Google Scholar]
- 20.Guerrero KL, Emery SJ, Wareham K, Ismail S, Watkins A, Lucas MG. A randomized controlled trial comparing TVT, Pelvicol and autologous fascial slings for the treatment of stress urinary incontinence in women. BJOG. 2010;117:1493–502. doi: 10.1111/j.1471-0528.2010.02696.x. [DOI] [PubMed] [Google Scholar]
- 21.Wadie BS, Mansour A, El-Hefnawy AS, Nabeeh A, Khair AA. Minimum 2-year follow-up of mid-urethral slings, effect on quality of life, incontinence impact and sexual function. Int Urogynecol J. 2010;21:1485–90. doi: 10.1007/s00192-010-1216-z. [DOI] [PubMed] [Google Scholar]
- 22.Freeman R, Holmes D, Hillard T, Smith P, James M, Sultan A, et al. What patients think: Patient-reported outcomes of retropubic versus trans-obturator mid-urethral slings for urodynamic stress incontinence—a multi-centre randomised controlled trial. Int Urogynecol J. 2011;22:279–86. doi: 10.1007/s00192-010-1343-6. [DOI] [PubMed] [Google Scholar]
- 23.Hinoul P, Bonnet P, Krofta L, Waltregny D, de Leval J. An anatomic comparison of the original versus a modified inside-out transobturator procedure. Int Urogynecol J. 2011;22:997–1004. doi: 10.1007/s00192-011-1415-2. [DOI] [PubMed] [Google Scholar]
- 24.Paparella R, Marturano M, Pelino L, Scarpa A, Scambia G, La Torre G, et al. Prospective randomized trial comparing synthetic vs biological out-in transobturator tape: A mean 3-year follow-up study. Int Urogynecol J. 2010;21:1327–36. doi: 10.1007/s00192-010-1197-y. [DOI] [PubMed] [Google Scholar]
- 25.Deffieux X, Daher N, Mansoor A, Debodinance P, Muhlstein J, Fernandez H. Transobturator TVT-O versus retropubic TVT: Results of a multicenter randomized controlled trial at 24 months follow-up. Int Urogynecol J. 2010;21:1337–45. doi: 10.1007/s00192-010-1196-z. [DOI] [PubMed] [Google Scholar]
- 26.Dyrkorn OA, Kulseng-Hanssen S, Sandvik L. TVT compared with TVT-O and TOT: Results from the Norwegian National Incontinence Registry. Int Urogynecol J. 2010;21:1321–6. doi: 10.1007/s00192-010-1195-0. [DOI] [PubMed] [Google Scholar]
- 27.Liapis A, Bakas P, Creatsas G. Comparison of the TVT SECUR System “hammock” and “U” tape positions for management of stress urinary incontinence. Int J Gynaecol Obstet. 2010;111:233–6. doi: 10.1016/j.ijgo.2010.07.013. [DOI] [PubMed] [Google Scholar]
- 28.Chen X, Tong X, Jiang M, Li H, Qiu J, Shao L, et al. A modified inexpensive transobturator vaginal tape inside-out procedure versus tension-free vaginal tape for the treatment of SUI: A prospective comparative study. Arch Gynecol Obstet. 2011 Mar 22; doi: 10.1007/s00404-011-1871-4. [Epub ahead of print] PubMed PMID: 21424711. [DOI] [PubMed] [Google Scholar]
- 29.Jeong MY, Kim SJ, Kim HS, Koh JS, Kim JC. Comparison of Efficacy and Satisfaction between the TVT-SECUR® and MONARC® Procedures for the Treatment of Female Stress Urinary Incontinence. Korean J Urol. 2010;51:767–71. doi: 10.4111/kju.2010.51.11.767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Zugor V, Labanaris AP, Rezaei-Jafari MR, Hammerer P, Dembowski J, Witt J, et al. TVT vs. TOT: A comparison in terms of continence results, complications and quality of life after a median follow-up of 48 months. Int Urol Nephrol. 2010;42:915–20. doi: 10.1007/s11255-010-9708-9. [DOI] [PubMed] [Google Scholar]
- 31.Chae HD, Kim SR, Jeon GH, Kim DY, Kim SH, Kim JH, et al. A comparative study of outside-in and inside-out transobturator tape procedures for stress urinary incontinence. Gynecol Obstet Invest. 2010;70:200–5. doi: 10.1159/000318866. [DOI] [PubMed] [Google Scholar]
- 32.Feng CL, Chin HY, Wang KH. Transobturator vaginal tape inside out procedure for stress urinary incontinence: Results of 102 patients. Int Urogynecol J Pelvic Floor Dysfunct. 2008;19:1423–7. doi: 10.1007/s00192-008-0658-z. [DOI] [PubMed] [Google Scholar]
- 33.Groutz A, Cohen A, Gold R, Pauzner D, Lessing JB, Gordon D. The safety and efficacy of the “inside-out” trans-obturator TVT in elderly versus younger stress-incontinent women: A prospective study of 353 consecutive patients. Neurourol Urodyn. 2011;30:380–3. doi: 10.1002/nau.20976. [DOI] [PubMed] [Google Scholar]
- 34.Kristensen I, Eldoma M, Williamson T, Wood S, Mainprize T, Ross S. Complications of the tension-free vaginal tape procedure for stress urinary incontinence. Int Urogynecol J. 2010;21:1353–7. doi: 10.1007/s00192-010-1210-5. [DOI] [PubMed] [Google Scholar]
- 35.Kim J, Lucioni A, Govier F, Kobashi K. Worse long-term surgical outcomes in elderly patients undergoing SPARC(TM) retropubic midurethral sling placement. BJU Int. 2011;108:708–12. doi: 10.1111/j.1464-410X.2010.09880.x. [DOI] [PubMed] [Google Scholar]
- 36.Sun MJ, Tsai HD. Is transobturator suburethral sling effective for treating female urodynamic stress incontinence with low maximal urethral closure pressure? Taiwan J Obstet Gynecol. 2011;50:20–4. doi: 10.1016/j.tjog.2011.01.027. [DOI] [PubMed] [Google Scholar]
- 37.Kaelin-Gambirasio I, Jacob S, Boulvain M, Dubuisson JB, Dällenbach P. Complications associated with transobturator sling procedures: Analysis of 233 consecutive cases with a 27 months follow-up. BMC Womens Health. 2009;25:28. doi: 10.1186/1472-6874-9-28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Lee JH, Yoon HJ, Lee SJ, Kim KH, Choi JS, Lee KW. Modified transobturator tape (canal transobturator tape) surgery for female stress urinary incontinence. J Urol. 2009;181:2616–21. doi: 10.1016/j.juro.2009.02.033. [DOI] [PubMed] [Google Scholar]
- 39.Youn CS, Shin JH, Na YG. Comparison of TOA and TOT for Treating Female Stress Urinary Incontinence: Short-Term Outcomes. Korean J Urol. 2010;51:544–9. doi: 10.4111/kju.2010.51.8.544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Errando C, Rodriguez-Escovar F, Gutierrez C, Baez C, Araño P, Villavicencio H. A re-adjustable sling for female recurrent stress incontinence and sphincteric deficiency: Outcomes and complications in 125 patients using the Remeex sling system. Neurourol Urodyn. 2010;29:1429–32. doi: 10.1002/nau.20879. [DOI] [PubMed] [Google Scholar]
- 41.Lee SY, Lee YS, Lee HN, Choo MS, Lee JG, Kim HG, et al. Transobturator adjustable tape for severe stress urinary incontinence and stress urinary incontinence with voiding dysfunction. Int Urogynecol J. 2011;22:341–6. doi: 10.1007/s00192-010-1289-8. [DOI] [PubMed] [Google Scholar]
- 42.Maroto JR, Gorraiz MO, Bueno JJ, Pérez LG, Bru JJ, Chaparro LP. Transobturator adjustable tape (TOA) permits to correct postoperatively the tension applied in stress incontinence surgery. Int Urogynecol J. 2009;20:797–805. doi: 10.1007/s00192-009-0872-3. [DOI] [PubMed] [Google Scholar]
- 43.Oliveira R, Botelho F, Silva P, Resende A, Silva C, Dinis P, et al. Exploratory Study Assessing Efficacy and Complications of TVT-O, TVT-Secur, and Mini-Arc: Results at 12-Month Follow-Up. Eur Urol. 2011;59:940–4. doi: 10.1016/j.eururo.2011.01.018. [DOI] [PubMed] [Google Scholar]
- 44.de Leval J, Thomas A, Waltregny D. The original versus a modified inside-out transobturator procedure: 1-year results of a prospective randomized trial. Int Urogynecol J. 2011;22:145–56. doi: 10.1007/s00192-010-1264-4. [DOI] [PubMed] [Google Scholar]
- 45.De Ridder D, Berkers J, Deprest J, Verguts J, Ost D, Hamid D, et al. Single incision mini-sling versus a transobutaror sling: A comparative study on MiniArc and Monarc slings. Int Urogynecol J. 2010;21:773–8. doi: 10.1007/s00192-010-1127-z. [DOI] [PubMed] [Google Scholar]
- 46.North CE, Hilton P, Ali-Ross NS, Smith AR. A 2-year observational study to determine the efficacy of a novel single incision sling procedure (Minitape) for female stress urinary incontinence. BJOG. 2010;117:356–60. doi: 10.1111/j.1471-0528.2009.02449.x. [DOI] [PubMed] [Google Scholar]
- 47.Oliveira R, Botelho F, Silva P, Resende A, Silva C, Dinis P, et al. Single- incision sling system as primary treatment of female stress urinary incontinence: Prospective 12 months data from a single institution. BJU Int. 2011;108:1616–21. doi: 10.1111/j.1464-410X.2011.10158.x. [DOI] [PubMed] [Google Scholar]
- 48.Pickens RB, Klein FA, Mobley JD, 3rd, White WM. Single incision mid- urethral sling for treatment of female stress urinary incontinence. Urology. 2011;77:321–4. doi: 10.1016/j.urology.2010.07.538. [DOI] [PubMed] [Google Scholar]
- 49.Kennelly MJ, Moore R, Nguyen JN, Lukban JC, Siegel S. Prospective evaluation of a single incision sling for stress urinary incontinence. J Urol. 2010;184:604–9. doi: 10.1016/j.juro.2010.04.003. [DOI] [PubMed] [Google Scholar]
- 50.Diwadkar GB, Barber MD, Feiner B, Maher C, Jelovsek JE. Complication and reoperation rates after apical vaginal prolapse surgical repair: A systematic review. Obstet Gynecol. 2009;113(2 Pt 1):367–73. doi: 10.1097/AOG.0b013e318195888d. [DOI] [PubMed] [Google Scholar]
- 51.Maher C, Feiner B, Baessler K, Adams EJ, Hagen S, Glazener CM. Surgical management of pelvic organ prolapse in women. Cochrane Database Syst Rev. 2010;4:CD004014. doi: 10.1002/14651858.CD004014.pub3. [DOI] [PubMed] [Google Scholar]
- 52.Jia X, Glazener C, Mowatt G, Jenkinson D, Fraser C, Bain C, et al. Systematic review of the efficacy and safety of using mesh in surgery for uterine or vaginal vault prolapse. Int Urogynecol J. 2010;21:1413–31. doi: 10.1007/s00192-010-1156-7. [DOI] [PubMed] [Google Scholar]
- 53.Long CY, Hsu CS, Jang MY, Liu CM, Chiang PH, Tsai EM. Comparison of clinical outcome and urodynamic findings using “Perigee and/or Apogee” versus “Prolift anterior and/or posterior” system devices for the treatment of pelvic organ prolapse. Int Urogynecol J. 2011;22:233–9. doi: 10.1007/s00192-010-1262-6. [DOI] [PubMed] [Google Scholar]
- 54.Elmér C, Altman D, Engh ME, Axelsen S, Väyrynen T, Falconer C Nordic Transvaginal Mesh Group. Trocar-guided transvaginal mesh repair of pelvic organ prolapse. Obstet Gynecol. 2009;113:117–26. doi: 10.1097/AOG.0b013e3181922164. [DOI] [PubMed] [Google Scholar]
- 55.Ek M, Altman D, Falconer C, Kulseng-Hanssen S, Tegerstedt G. Effects of anterior trocar guided transvaginal mesh surgery on lower urinary tract symptoms. Neurourol Urodyn. 2010;29:1419–23. doi: 10.1002/nau.20880. [DOI] [PubMed] [Google Scholar]
- 56.Moore RD, Beyer RD, Jacoby K, Freedman SJ, McCammon KA, Gambla MT. Prospective multicenter trial assessing type I, polypropylene mesh placed via transobturator route for the treatment of anterior vaginal prolapse with 2-year follow-up. Int Urogynecol J. 2010;21:545–52. doi: 10.1007/s00192-009-1071-y. [DOI] [PubMed] [Google Scholar]
- 57.Kaufman Y, Singh SS, Alturki H, Lam A. Age and sexual activity are risk factors for mesh exposure following transvaginal mesh repair. Int Urogynecol J. 2011;22:307–13. doi: 10.1007/s00192-010-1270-6. [DOI] [PubMed] [Google Scholar]
- 58.Fayyad AM, North C, Reid FM, Smith AR. Prospective study of anterior transobturator mesh kit (Prolift™) for the management of recurrent anterior vaginal wall prolapse. Int Urogynecol J. 2011;22:157–63. doi: 10.1007/s00192-010-1260-8. [DOI] [PubMed] [Google Scholar]
- 59.Lawndy SS, Kluivers KB, Milani AL, Withagen MI, Hendriks JC, Vierhout ME. Which factors determine subjective improvement following pelvic organ prolapse 1 year after surgery? Int Urogynecol J. 2011;22:543–9. doi: 10.1007/s00192-010-1321-z. [DOI] [PubMed] [Google Scholar]
- 60.Cosma S, Preti M, Mitidieri M, Petruzzelli P, Possavino F, Menato G. Posterior intravaginal slingplasty: Efficacy and complications in a continuous series of 118 cases. Int Urogynecol J. 2011;22:611–9. doi: 10.1007/s00192-010-1350-7. [DOI] [PubMed] [Google Scholar]
- 61.Lo TS, Ashok K. Combined anterior trans-obturator mesh and sacrospinous ligament fixation in women with severe prolapse--a case series of 30 months follow-up. Int Urogynecol J. 2011;22:299–306. doi: 10.1007/s00192-010-1266-2. [DOI] [PubMed] [Google Scholar]
- 62.Jacquetin B, Cosson M, Debodinance P, Hinoul P. Vaginal mesh for prolapse: A randomized controlled trial. Obstet Gynecol. 2010;116:1457–8. doi: 10.1097/AOG.0b013e3181ff9781. [DOI] [PubMed] [Google Scholar]
- 63.McDermott CD, Terry CL, Woodman PJ, Hale DS. Surgical outcomes following total Prolift: Colpopexy versus hysteropexy. Aust N Z J Obstet Gynaecol. 2011;51:61–6. doi: 10.1111/j.1479-828X.2010.01258.x. [DOI] [PubMed] [Google Scholar]
- 64.Lau HY, Twu NF, Chen YJ, Horng HC, Juang CM, Chao KC. Comparing effectiveness of combined transobturator tension-free vaginal mesh (Perigee) and transobturator tension-free vaginal tape (TVT-O) versus anterior colporrhaphy and TVT-O for associated cystocele and urodynamic stress incontinence. Eur J Obstet Gynecol Reprod Biol. 2011;156:228–32. doi: 10.1016/j.ejogrb.2011.01.030. [DOI] [PubMed] [Google Scholar]
- 65.Vaiyapuri GR, Han HC, Lee LC, Tseng LA, Wong HF. Use of the Gynecare Prolift® system in surgery for pelvic organ prolapse: 1-year outcome. Int Urogynecol J. 2011;22:869–77. doi: 10.1007/s00192-011-1400-9. [DOI] [PubMed] [Google Scholar]
- 66.Huang WC, Lin TY, Lau HH, Chen SS, Hsieh CH, Su TH. Outcome of transvaginal pelvic reconstructive surgery with Prolift after a median of 2 years’ follow-up. Int Urogynecol J. 2011;22:197–203. doi: 10.1007/s00192-010-1259-1. [DOI] [PubMed] [Google Scholar]
- 67.Shveiky D, Sokol AI, Gutman RE, Kudish BI, Iglesia CB. Vaginal mesh colpopexy for the treatment of concomitant full thickness rectal and pelvic organ prolapse: A case series. Eur J Obstet Gynecol Reprod Biol. 2011;157:113–5. doi: 10.1016/j.ejogrb.2011.02.017. [DOI] [PubMed] [Google Scholar]
- 68.Eboue C, Marcus-Braun N, von Theobald P. Cystocele repair by transobturator four arms mesh: Monocentric experience of first 123 patients. Int Urogynecol J. 2010;21:85–93. doi: 10.1007/s00192-009-0993-8. [DOI] [PubMed] [Google Scholar]
- 69.Park HK, Paick SH, Lee BK, Kang MB, Jun KK, Kim HG. Initial experience with concomitant prolift™ system and tension-free vaginal tape procedures in patients with stress urinary incontinence and cystocele. Int Neurourol J. 2010;14:43–7. doi: 10.5213/inj.2010.14.1.43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Gagnon LO, Tu LM. Mid-term results of pelvic organ prolapse repair using a transvaginal mesh: The experience in Sherbooke, Quebec. Can Urol Assoc J. 2010;4:188–91. doi: 10.5489/cuaj.09084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Argirovic RB, Gudovic AM, Babovic IR, Berisavac MV. Transvaginal repair of genital prolapse with polypropylene mesh using a tension-free technique. Eur J Obstet Gynecol Reprod Biol. 2010;153:104–7. doi: 10.1016/j.ejogrb.2010.07.011. [DOI] [PubMed] [Google Scholar]
- 72.Ganj FA, Ibeanu OA, Bedestani A, Nolan TE, Chesson RR. Complications of transvaginal monofilament polypropylene mesh in pelvic organ prolapse repair. Int Urogynecol J. 2009;20:919–25. doi: 10.1007/s00192-009-0879-9. [DOI] [PubMed] [Google Scholar]
- 73.Caquant F, Collinet P, Debodinance P, Berrocal J, Garbin O, Rosenthal C, et al. Safety of Trans Vaginal Mesh procedure: Retrospective study of 684 patients. J Obstet Gynaecol Res. 2008;34:449–56. doi: 10.1111/j.1447-0756.2008.00820.x. [DOI] [PubMed] [Google Scholar]
- 74.Gabriel B, Rubod C, Córdova LG, Lucot JP, Cosson M. Prolapse surgery in women of 80 years and older using the Prolift™ technique. Int Urogynecol J. 2010;21:1463–70. doi: 10.1007/s00192-010-1217-y. [DOI] [PubMed] [Google Scholar]
- 75.Ghezzi F, Uccella S, Cromi A, Bogani G, Candeloro I, Serati M, et al. Surgical treatment for pelvic floor disorders in women 75 years or older: A single-center experience. Menopause. 2011;18:314–8. doi: 10.1097/gme.0b013e3181f2e629. [DOI] [PubMed] [Google Scholar]
- 76.Cundiff GW, Varner E, Visco AG, Zyczynski HM, Nager CW, Norton PA, et al. Pelvic Floor Disorders Network. Risk factors for mesh/suture erosion following sacral colpopexy. Am J Obstet Gynecol. 2008;199:688. doi: 10.1016/j.ajog.2008.07.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Lee JK, Agnew G, Dwyer PL. Mesh-related chronic infections in silicone-coated polyester suburethral slings. Int Urogynecol J. 2011;22:29–35. doi: 10.1007/s00192-010-1244-8. [DOI] [PubMed] [Google Scholar]
- 78.Govier FE, Kobashi KC, Kuznetsov DD, Comiter C, Jones P, Dakil SE, et al. Complications of transvaginal silicone-coated polyester synthetic mesh sling. Urology. 2005;66:741–5. doi: 10.1016/j.urology.2005.04.027. [DOI] [PubMed] [Google Scholar]
- 79.Yamada BS, Govier FE, Stefanovic KB, Kobashi KC. High rate of vaginal erosions associated with the mentor ObTape. J Urol. 2006;176:651–4. doi: 10.1016/j.juro.2006.03.064. [DOI] [PubMed] [Google Scholar]
- 80.Milani AL, Hinoul P, Gauld JM, Sikirica V, van Drie D, Cosson M. Prolift+M Investigators. Trocar-guided mesh repair of vaginal prolapse using partially absorbable mesh: 1 year outcomes. Am J Obstet Gynecol. 2011;204:74. doi: 10.1016/j.ajog.2010.08.036. [DOI] [PubMed] [Google Scholar]
- 81.Cervigni M, Natale F, La Penna C, Saltari M, Padoa A, Agostini M. Collagen-coated polypropylene mesh in vaginal prolapse surgery: An observational study. Eur J Obstet Gynecol Reprod Biol. 2011;156:223–7. doi: 10.1016/j.ejogrb.2011.01.027. [DOI] [PubMed] [Google Scholar]
- 82.Araco F, Gravante G, Overton J, Araco P, Dati S. Transvaginal cystocele correction: Midterm results with a transobturator tension-free technique using a combined bovine pericardium/polypropylene mesh. J Obstet Gynaecol Res. 2009;35:953–60. doi: 10.1111/j.1447-0756.2009.01036.x. [DOI] [PubMed] [Google Scholar]
- 83.Karp DR, Peterson TV, Mahdy A, Ghoniem G, Aguilar VC, Davila GW. Biologic grafts for cystocele repair: Does concomitant midline fascial plication improve surgical outcomes? Int Urogynecol J. 2011;22:985–90. doi: 10.1007/s00192-011-1408-1. [DOI] [PubMed] [Google Scholar]
- 84.Culligan PJ, Littman PM, Salamon CG, Priestley JL, Shariati A. Evaluation of a transvaginal mesh delivery system for the correction of pelvic organ prolapse: Subjective and objective findings at least 1 year after surgery. Am J Obstet Gynecol. 2010;203:506. doi: 10.1016/j.ajog.2010.07.020. [DOI] [PubMed] [Google Scholar]
- 85.Alcalay M, Cosson M, Livneh M, Lucot JP, Von Theobald P. Trocarless system for mesh attachment in pelvic organ prolapse repair-1-year evaluation. Int Urogynecol J. 2011;22:551–6. doi: 10.1007/s00192-010-1349-0. [DOI] [PubMed] [Google Scholar]
- 86.Zyczynski HM, Carey MP, Smith AR, Gauld JM, Robinson D, Sikirica V, et al. Prosima Study Investigators. One-year clinical outcomes after prolapse surgery with nonanchored mesh and vaginal support device. Am J Obstet Gynecol. 2010;203:587. doi: 10.1016/j.ajog.2010.08.001. [DOI] [PubMed] [Google Scholar]
- 87.Kavvadias T, Kaemmer D, Klinge U, Kuschel S, Schuessler B. Foreign body reaction in vaginally eroded and noneroded polypropylene suburethral slings in the female: A case series. Int Urogynecol J. 2009;20:1473–6. doi: 10.1007/s00192-009-0974-y. [DOI] [PubMed] [Google Scholar]
- 88.Amrute KV, Eisenberg ER, Rastinehad AR, Kushner L, Badlani GH. Analysis of outcomes of single polypropylene mesh in total pelvic floor reconstruction. Neurourol Urodyn. 2007;26:53–8. doi: 10.1002/nau.20362. [DOI] [PubMed] [Google Scholar]
- 89.Patel BN, Smith JJ, Badlani GH. Minimizing the cost of surgical correction of stress urinary incontinence and prolapse. Urology. 2009;74:762–4. doi: 10.1016/j.urology.2009.06.004. [DOI] [PubMed] [Google Scholar]
- 90.Finamore PS, Echols KT, Hunter K, Goldstein HB, Holzberg AS, Vakili B. Risk factors for mesh erosion 3 months following vaginal reconstructive surgery using commercial kits vs. mufashioned mesh-augmented vaginal repairs. Int Urogynecol J. 2010;21:285–91. doi: 10.1007/s00192-009-1005-8. [DOI] [PubMed] [Google Scholar]
- 91.Murray S, Haverkorn RM, Lotan Y, Lemack GE. Mesh kits for anterior vaginal prolapse are not cost effective. Int Urogynecol J. 2011;22:447–52. doi: 10.1007/s00192-010-1291-1. [DOI] [PubMed] [Google Scholar]
- 92.Stepanian AA, Miklos JR, Moore RD, Mattox TF. Risk of mesh extrusion and other mesh-related complications after laparoscopic sacral colpopexy with or without concurrent laparoscopic-assisted vaginal hysterectomy: Experience of 402 patients. J Minim Invasive Gynecol. 2008;15:188–96. doi: 10.1016/j.jmig.2007.11.006. [DOI] [PubMed] [Google Scholar]
- 93.Maher C, Feiner B, Baessler K, Adams EJ, Hagen S, Glazener CM. Surgical management of pelvic organ prolapse in women. Cochrane Database Syst Rev. 2010;4:CD004014. doi: 10.1002/14651858.CD004014.pub3. [DOI] [PubMed] [Google Scholar]
- 94.Costantini E, Lazzeri M, Bini V, Del Zingaro M, Zucchi A, Porena M. Pelvic organ prolapse repair with and without prophylactic concomitant burch colposuspension in continent women: A randomized, controlled trial with 8-year followup. J Urol. 2011;185:2236–40. doi: 10.1016/j.juro.2011.01.078. [DOI] [PubMed] [Google Scholar]
- 95.Moon YJ, Jeon MJ, Kim SK, Bai SW. Comparison of Burch colposuspension and transobturator tape when combined with abdominal sacrocolpopexy. Int J Gynaecol Obstet. 2011;112:122–5. doi: 10.1016/j.ijgo.2010.08.017. [DOI] [PubMed] [Google Scholar]
- 96.Park HK, Paick SH, Lee BK, Kang MB, Jun KK, Kim HG. Initial experience with concomitant prolift™ system and tension-free vaginal tape procedures in patients with stress urinary incontinence and cystocele. Int Neurourol J. 2010;14:43–7. doi: 10.5213/inj.2010.14.1.43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Groutz A, Levin I, Gold R, Pauzner D, Lessing JB, Gordon D. “Inside-out” transobturator tension-free vaginal tape for management of occult stress urinary incontinence in women undergoing pelvic organ prolapse repair. Urology. 2010;76:1358–61. doi: 10.1016/j.urology.2010.04.070. [DOI] [PubMed] [Google Scholar]
- 98.Margulies RU, Lewicky-Gaupp C, Fenner DE, McGuire EJ, Clemens QJ, De Lanceyet JO. Complications requiring reoperation following vaginal mesh kit procedures for prolapse. Am J Obstet Gynecol. 2008;199:678.e1–678.e4. doi: 10.1016/j.ajog.2008.07.049. [DOI] [PubMed] [Google Scholar]
- 99.Deval B, Haab F. Management of the complications of the synthetic slings. Curr Opin Urol. 2006;16:240–3. doi: 10.1097/01.mou.0000232043.95427.d6. [DOI] [PubMed] [Google Scholar]
- 100.Geller EJ, Parnell BA, Dunivan GC. Pelvic floor function before and after robotic sacrocolpopexy: One-year outcomes. J Minim Invasive Gynecol. 2011;18:322–7. doi: 10.1016/j.jmig.2011.01.008. [DOI] [PubMed] [Google Scholar]
- 101.Moreno Sierra J, Ortiz Oshiro E, Fernandez Pérez C, Galante Romo I, Corral Rosillo J, Prieto Nogal S, et al. Long-Term Outcomes after Robotic Sacrocolpopexy in Pelvic Organ Prolapse: Prospective Analysis. Urol Int. 2011;86:414–8. doi: 10.1159/000323862. [DOI] [PubMed] [Google Scholar]
- 102.Maher CF, Feiner B, Decuyper EM, Nichlos CJ, Hickey KV, O’Rourke P. Laparoscopic sacral colpopexy versus total vaginal mesh for vaginal vault prolapse: A randomized trial. Am J Obstet Gynecol. 2011;204:360.e1–7. doi: 10.1016/j.ajog.2010.11.016. [DOI] [PubMed] [Google Scholar]
- 103.Sergent F, Resch B, Loisel C, Bisson V, Schaal JP, Marpeau L. Mid-term outcome of laparoscopic sacrocolpopexy with anterior and posterior polyester mesh for treatment of genito-urinary prolapse. Eur J Obstet Gynecol Reprod Biol. 2011;156:217–22. doi: 10.1016/j.ejogrb.2011.01.022. [DOI] [PubMed] [Google Scholar]
- 104.Xylinas E, Ouzaid I, Durand X, Ploussard G, Salomon L, Gillion N, et al. Robot-assisted laparoscopic sacral colpopexy: Initial experience in a high-volume laparoscopic reference center. J Endourol. 2010;24:1985–9. doi: 10.1089/end.2010.0160. [DOI] [PubMed] [Google Scholar]
- 105.Wong MT, Meurette G, Rigaud J, Regenet N, Lehur PA. Robotic versus laparoscopic rectopexy for complex rectocele: A prospective comparison of short-term outcomes. Dis Colon Rectum. 2011;54:342–6. doi: 10.1007/DCR.0b013e3181f4737e. [DOI] [PubMed] [Google Scholar]
- 106.Onol FF, Kaya E, Köse O, Onol SY. A novel technique for the management of advanced uterine/vault prolapse: Extraperitoneal sacrocolpopexy. Int Urogynecol J. 2011;22:855–61. doi: 10.1007/s00192-011-1378-3. [DOI] [PubMed] [Google Scholar]
- 107.Wang Y, Wang D, Li Y, Liang Z, Xu H. Laparoscopic sacrospinous ligament fixation for uterovaginal prolapse: Experience with 93 cases. Int Urogynecol J. 2011;22:83–9. doi: 10.1007/s00192-010-1232-z. [DOI] [PubMed] [Google Scholar]
- 108.Kobashi KC, Govier FE. Management of vaginal erosion of polypropylene mesh slings. J Urol. 2003;169:2242–3. doi: 10.1097/01.ju.0000060119.43064.f6. [DOI] [PubMed] [Google Scholar]
- 109.Deffieux X, de Tayrac R, Huel C, Bottero J, Gervaise A, Bonnet K, et al. Vaginal mesh erosion after transvaginal repair of cystocele using Gynemesh or Gynemesh-Soft in 138 women: A comparative study. Int Urogynecol J. 2007;18:73–9. doi: 10.1007/s0192-005-0041-2. [DOI] [PubMed] [Google Scholar]
- 110.Collinet P, Belot F, Debodinance P, Ha Duc E, Lucot JP, Cosson M. Transvaginal mesh technique for pelvic organ prolapse repair: Mesh exposure management and risk factors. Int Urogynecol J. 2006;17:315–20. doi: 10.1007/s00192-005-0003-8. [DOI] [PubMed] [Google Scholar]
- 111.Lo TS, Lee SJ. Simple sling resection and a second, intermediate polypropylene mesh for treatment of vaginal tape protrusion concurrent with recurrent urinary stress incontinence after TVT procedure. J Obstet Gynaecol Res. 2007;33:739–42. doi: 10.1111/j.1447-0756.2007.00643.x. [DOI] [PubMed] [Google Scholar]
- 112.South MM, Foster RT, Webster GD, Weidner AC, Amundsen CL. Surgical excision of eroded mesh after prior abdominal sacrocolpopexy. 2007;197:615. Am J Obstet Gynecol. 2007;197:615.e1–5. doi: 10.1016/j.ajog.2007.08.012. [DOI] [PubMed] [Google Scholar]
- 113.Deng DY, Rutman M, Raz S, Rodriguez LV. Presentation and management of major complications of midurethral slings: Are complications under-reported? Neurourol Urodyn. 2007;26:46–52. doi: 10.1002/nau.20357. [DOI] [PubMed] [Google Scholar]
- 114.Ordorica R, Rodriguez AR, Coste-Delvecchio F, Hoffman M, Lockhart J. Disabling complications with slings for managing female stress urinary incontinence. BJU Int. 2008;102:333–6. doi: 10.1111/j.1464-410X.2008.07608.x. [DOI] [PubMed] [Google Scholar]
- 115.Velemir L, Amblard J, Jacquetin B, Fatton B. Urethral erosion after suburethral synthetic slings: Risk factors, diagnosis, and functional outcome after surgical management. Int Urogynecol J. 2008;19:999–1006. doi: 10.1007/s00192-007-0558-7. [DOI] [PubMed] [Google Scholar]
- 116.Blandon RE, Gebhart JB, Trabuco EC, Klingele CJ. Complications from vaginally placed mesh in pelvic reconstructive surgery. Int Urogynecol J. 2009 Feb 10; doi: 10.1007/s00192-009-0818-9. [Epub ahead of print] PubMed PMID: 19209374. [DOI] [PubMed] [Google Scholar]
- 117.Kuhn A, Eggeman C, Burkhard F, Mueller MD. Correction of erosion after suburethral sling insertion for stress incontinence: Results and related sexualfunction. Eur Urol. 2009;56:371–6. doi: 10.1016/j.eururo.2008.07.001. [DOI] [PubMed] [Google Scholar]
- 118.Araco F, Gravante G, DE Vita D, Konda D, Rombola P, Araco P, et al. Obturator abscess with spread to the thigh after three years from a transobturator procedure. Aust N Z J Obstet Gynaecol. 2009;49:335–6. doi: 10.1111/j.1479-828X.2009.00986.x. [DOI] [PubMed] [Google Scholar]
- 119.Shaker D. Surgical management of vaginal mesh erosion: An alternative to excision. Int Urogynecol J. 2010;21:499–501. doi: 10.1007/s00192-009-1009-4. [DOI] [PubMed] [Google Scholar]
- 120.Firoozi F, Ingber MS, Goldman HB. Pure transvaginal removal of eroded mesh and retained foreign body in the bladder. Int Urogynecol J. 2010;21:757–60. doi: 10.1007/s00192-009-1066-8. [DOI] [PubMed] [Google Scholar]
- 121.Khong SY, Lam A. Use of Surgisis mesh in the management of polypropylene mesh erosion into the vagina. Int Urogynecol J. 2011;22:41–6. doi: 10.1007/s00192-010-1234-x. [DOI] [PubMed] [Google Scholar]
- 122.Costantini E, Zucchi A, Lazzeri M, Del Zingaro M, Vianello A, Porena M. Managing Mesh Erosion after Abdominal Pelvic Organ Prolapse Repair: Ten Years’ Experience in a Single Center. Urol Int. 2011;86:419–23. doi: 10.1159/000324243. [DOI] [PubMed] [Google Scholar]
- 123.Irer B, Aslan G, Cimen S, Bozkurt O, Celebi I. Development of vesical calculi following tension-free vaginal tape procedure. Int Urogynecol J. 2005;16:245–6. doi: 10.1007/s00192-004-1241-x. [DOI] [PubMed] [Google Scholar]
- 124.Quiroz LH, Cundiff GW. Transurethral resection of tension-free vaginal tape under tactile traction. Int Urogynecol J. 2009;20:873–5. doi: 10.1007/s00192-008-0758-9. [DOI] [PubMed] [Google Scholar]
- 125.Wijffels SA, Elzevier HW, Lycklama A, Nijeholt AA. Transurethral mesh resection after urethral erosion of tension-free vaginal tape: Report of three cases and review of literature. Int Urogynecol J. 2009;20:261–3. doi: 10.1007/s00192-008-0705-9. [DOI] [PubMed] [Google Scholar]
- 126.Arrabal-Polo MA, Arrabal-Martin M, Tinaut-Ranera J, Mijan-Ortiz JL, Zuluaga-Gomez A. Bladder lithiasis on tension-free polypropylene tape after TVT technique. Urol Res. 2010;38:519–21. doi: 10.1007/s00240-010-0266-5. [DOI] [PubMed] [Google Scholar]
- 127.Mendonça TM, Martinho D, Dos Reis JP. Late urethral erosion of transobturator suburethral mesh (Obtape®): A minimally invasive management under local anaesthesia. Int Urogynecol J. 2011;22:37–9. doi: 10.1007/s00192-010-1230-1. [DOI] [PubMed] [Google Scholar]
- 128.Mustafa M, Wadie BS. Bladder erosion of tension-free vaginal tape presented as vesical stone; management and review of literature. Int Urol Nephrol. 2007;39:453–5. doi: 10.1007/s11255-006-9080-y. [DOI] [PubMed] [Google Scholar]
- 129.Huwyler M, Springer J, Kessler TM, Burkhard MC. A safe and simple solution for intravesical tension-free vaginal tape erosion: Removal by standard transurethral resection. BJUI. 2008;102:582–5. doi: 10.1111/j.1464-410X.2008.07734.x. [DOI] [PubMed] [Google Scholar]
- 130.Oh TH, Ryu DS. Transurethral resection of intravesical mesh after midurethral sling procedures. J Endourol. 2009;23:1333–7. doi: 10.1089/end.2009.0098. [DOI] [PubMed] [Google Scholar]
- 131.Foley C, Patki P, Boustead G. Unrecognized bladder perforation with mid-urethral slings. BJU Int. 2010;106:1514–8. doi: 10.1111/j.1464-410X.2010.09378.x. [DOI] [PubMed] [Google Scholar]
- 132.Giri SK, Drumm J, Flood HD. Endoscopic holmium laser excision of intravesical tension-free vaginal tape and polypropylene suture after anti-incontinence procedures. J Urol. 2005;174:1306–7. doi: 10.1097/01.ju.0000173926.04596.55. [DOI] [PubMed] [Google Scholar]
- 133.Doumouchtsis SK, Lee FY, Bramwell D, Fynes MM. Evaluation of holmium laser for managing mesh/suture complications of continence surgery. BJU Int. 2011;108:1472–8. doi: 10.1111/j.1464-410X.2010.10012.x. [DOI] [PubMed] [Google Scholar]
- 134.Frenkl TL, Rackley RR, Vasavada SP, Goldman HB. Management of Iatrogenic Foreign Bodies of the Bladder and Urethra Following Pelvic Floor Surgery. Neurourol Urodyn. 2008;27:491–5. doi: 10.1002/nau.20558. [DOI] [PubMed] [Google Scholar]
- 135.Feiner B, Auslender R, Mecz Y, Lissak A, Stein A, Abramov Y. Removal of an eroded transobturator tape from the bladder using laser cystolithotripsy and cystoscopic resection. Urology. 2009;73:681.e15–6. doi: 10.1016/j.urology.2008.01.002. [DOI] [PubMed] [Google Scholar]
- 136.Al-Badr A, Fouda K. Suprapubic-assisted cystoscopic excision of intravesical tension-free vaginal tape. J Minim Invasive Gynecol. 2005;12:370–1. doi: 10.1016/j.jmig.2005.05.001. [DOI] [PubMed] [Google Scholar]
- 137.Cornel EB, Vervest HA. Removal of a missed polypropylene tape by a combined transurethral and transabdominal endoscopic approach. Int Urogynecol J. 2005;16:247–9. doi: 10.1007/s00192-004-1242-9. [DOI] [PubMed] [Google Scholar]
- 138.Baracat F, Mitre AI, Kanashiro H, Montellato NI. Endoscopic treatment of vesical and urethral perforations after tension-free vaginal tape (TVT) procedure for female stress urinary incontinence. Clinics (Sao Paulo) 2005;60:397–400. doi: 10.1590/s1807-59322005000500008. [DOI] [PubMed] [Google Scholar]
- 139.Rosenblatt P, Pulliam S, Edwards R, Boyles SH. Suprapubically assisted operative cystoscopy in the management of intravesical TVT synthetic mesh segments. Int Urogynecol J. 2005;16:509–11. doi: 10.1007/s00192-004-1282-1. [DOI] [PubMed] [Google Scholar]
- 140.Parekh MH, Minassian VA, Poplawsky D. Bilateral bladder erosion of a transobturator tape mesh. Obstet Gynecol. 2006;180(3 Pt 2):713–5. doi: 10.1097/01.AOG.0000227968.64752.1a. [DOI] [PubMed] [Google Scholar]
- 141.Bekker MD, Bevers RF, Elzevier HW. Transurethral and suprapubic mesh resection after Prolift bladder perforation: A case report. Int Urogynecol J. 2010;21:1301–3. doi: 10.1007/s00192-010-1122-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Pikaart DP, Miklos JR, Moore RD. Laparoscopic removal of pubovaginal polypropylene tension-free tape slings. JSLS. 2006;10:220–5. [PMC free article] [PubMed] [Google Scholar]
- 143.Baessler K, Hewson AD, Tunn R, Schuessler B, Maher CF. Severe mesh complications following intravaginal slingplasty. Obstet Gynecol. 2005;106:713–6. doi: 10.1097/01.AOG.0000177970.52037.0a. [DOI] [PubMed] [Google Scholar]
- 144.Stepanian AA, Miklos JR, Moore RD, Mattox TF. Risk of mesh extrusion and othermesh-related complications after laparo- scopic sacral colpopexy with or without concurrent laparoscopic- assisted vaginal hysterectomy: Experience of 402 patients. J Minim Invasive Gynecol. 2008;15:188–96. doi: 10.1016/j.jmig.2007.11.006. [DOI] [PubMed] [Google Scholar]
- 145.Misrai V, Rouprêt M, Xylinas E, Cour F, Vaessen C, Haertig A, et al. Surgical Resection for Suburethral Sling Complications After Treatment for Stress Urinary Incontinence. J Urol. 2009;181:2198–203. doi: 10.1016/j.juro.2009.01.036. [DOI] [PubMed] [Google Scholar]
- 146.Ingber MS, Stein RJ, Rackley RR, Firoozi F, Irwin BH, Kaouk JH, et al. Single-port Transvesical Excision of Foreign Body in the Bladder. Urology. 2009;74:1347–50. doi: 10.1016/j.urology.2009.07.1218. [DOI] [PubMed] [Google Scholar]
- 147.Marcus-Braun N, von Theobald P. Mesh removal following transvaginal mesh placement: A case series of 104 operations. Int Urogynecol J. 2010;21:423–30. doi: 10.1007/s00192-009-1050-3. [DOI] [PubMed] [Google Scholar]
- 148.Roupre M, Misra V, Vaessen C, Cour F, Haertig A, Chartier-Kastler E. Laparoscopic surgical complete sling resection for tension-free vaginal tape–related complications refractory to first-line conservative management: A single-centre experience. Eur Urol. 2010;58:270–4. doi: 10.1016/j.eururo.2010.04.025. [DOI] [PubMed] [Google Scholar]
- 149.Angulo JC, Mateo E, Lista F, Andrés G. Reconstructive treatment of female urethral estenosis secondary to erosion by suburethral tape. Actas Urol Esp. 2011;35:240–5. doi: 10.1016/j.acuro.2011.01.001. [DOI] [PubMed] [Google Scholar]
- 150.Al-Wadi K, Al-Badr A. Martius graft for the management of tension-free vaginal tape vaginal erosion. Obstet Gynecol. 2009;114(2 Pt 2):489–91. doi: 10.1097/AOG.0b013e31819eca9b. [DOI] [PubMed] [Google Scholar]
- 151.Nicolson A, Adeyemo D. Colovaginal fistula: A rare long-term complication of polypropylene mesh sacrocolpopexy. J Obstet Gynaecol. 2009;29:444–5. doi: 10.1080/01443610902954360. [DOI] [PubMed] [Google Scholar]
- 152.Hopkins MP, Rooney C. Entero mesh vaginal fistula secondary to abdominal sacral colpopexy. Obstet Gynecol. 2004;103:1035–6. doi: 10.1097/01.AOG.0000127940.45774.b4. [DOI] [PubMed] [Google Scholar]
- 153.Jacquetin B, Cosson M. Complications of vaginal mesh: Our experience. Int Urogynecol J. 2009;20:893–6. doi: 10.1007/s00192-009-0926-6. [DOI] [PubMed] [Google Scholar]
- 154.Clavé A, Yahi H, Hammou J, Montanari S, Gounon P, Clave H. Polypropylene as a reinforcement in pelvic surgery is not inert: Comparative analysis of 100 explants. Int Urogynecol J. 2010;21:261–70. doi: 10.1007/s00192-009-1021-8. [DOI] [PubMed] [Google Scholar]
- 155.Bako A, Dhar R. Review of synthetic mesh-related complications in pelvic floor reconstructive surgery. Int Urogynecol J. 2009;20:103–11. doi: 10.1007/s00192-008-0717-5. [DOI] [PubMed] [Google Scholar]
- 156.Lee SY, Kim JY, Park SK, Kwon YW, Nguyen HB, Chang IH, et al. Bilateral Recurrent Thigh Abscesses for Five Years after a Transobturator Tape Implantation for Stress Urinary Incontinence. Korean J Urol. 2010;51:657–9. doi: 10.4111/kju.2010.51.9.657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Lo TS. One-year outcome of concurrent anterior and posterior transvaginal mesh surgery for treatment of advanced urogenital prolapse: Case series. J Minim Invasive Gynecol. 2010;17:473–9. doi: 10.1016/j.jmig.2010.03.003. [DOI] [PubMed] [Google Scholar]
- 158.Dietz HP, Vancaillie P, Svehla M, Walsh W, Steensma AB, Vancaillie TG. Mechanical properties of urogynecologic implant materials. Int Urogynecol J. 2003;14:239–43. doi: 10.1007/s00192-003-1041-8. [DOI] [PubMed] [Google Scholar]
- 159.Feiner B, Maher C. Vaginal mesh contraction: Definition, clinical presentation, and management. Obstet Gynecol. 2010;115(2 Pt 1):325–30. doi: 10.1097/AOG.0b013e3181cbca4d. [DOI] [PubMed] [Google Scholar]
- 160.Foon R, Smith P. The effectiveness and complications of graft materials used in vaginal prolapse surgery. Curr Opin Obstet Gynecol. 2009;21:424–7. doi: 10.1097/GCO.0b013e32832fd255. [DOI] [PubMed] [Google Scholar]
- 161.Cholhan HJ, Hutchings TB, Rooney KE. Dyspareunia associated with paraurethral banding in the transobturator sling. Am J Obstet Gynecol. 2010;202:481–5. doi: 10.1016/j.ajog.2010.01.061. [DOI] [PubMed] [Google Scholar]
- 162.Neuman M. TVT-obturator: Short-term data on an operative procedure for the cure of female stress urinary incontinence performed on 300 patients. Eur Urol. 2007;51:1083. doi: 10.1016/j.eururo.2006.10.003. [DOI] [PubMed] [Google Scholar]
- 163.Mohr S, Kuhn P, Mueller MD, Kuhn A. Painful Love-“Hispareunia” after Sling Erosion of the Female Partner. J Sex Med. 2011;8:1740–6. doi: 10.1111/j.1743-6109.2011.02261.x. [DOI] [PubMed] [Google Scholar]
- 164.Lin LL, Haessler AL, Ho MH, Betson LH, Alinsod RM, Bhatia NN. Dyspareunia and chronic pelvic pain after polypropylene mesh augmentation for transvaginal repair of anterior vaginal wall prolapse. Int Urogynecol J. 2007;18:675–8. doi: 10.1007/s00192-006-0187-6. [DOI] [PubMed] [Google Scholar]
- 165.US Food and Drug Administration Web site. [Last accessed on 2011 Aug 01]. Available from: http:// www.fda.gov/cdrh/safety/102008-surgicalmesh. html . Updated October 21, 2008 .
- 166.US Food and Drug Administration Web site. [Last accessed on 2011 Aug 01]. Available from: http://www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/ucm262752.htm .
- 167.Dmochowski RR, Blaivas JM, Gormley EM, Juma S, Karram MM, Lightner DJ, et al. Update of AUA Guideline on the Surgical Management of Female Stress Urinary Incontinence. J Urol. 2010;183:1906–14. doi: 10.1016/j.juro.2010.02.2369. [DOI] [PubMed] [Google Scholar]
- 168.Ou R, Xie XJ, Zimmern PE. Level I/II Evidence-Based Studies of Surgical Treatment of Female Stress Urinary Incontinence: Patients Lost to Followup. J Urol. 2011;185:1338–43. doi: 10.1016/j.juro.2010.11.071. [DOI] [PubMed] [Google Scholar]
- 169.Jacquetin B, Cosson M. Complications of vaginal mesh: Our experience. Int Urogynecol J. 2009;20:893–6. doi: 10.1007/s00192-009-0926-6. [DOI] [PubMed] [Google Scholar]
- 170.Daneshgari F, Kong W, Swartz M. Complications of mid urethral slings: Important outcomes for future clinical trials. J Urol. 2008;180:1890–7. doi: 10.1016/j.juro.2008.07.029. [DOI] [PubMed] [Google Scholar]


