Abstract
Aim:
The aim of this work was to determine the frequency and nature of oral manifestations in a hypertensive patient.
Materials and Methods:
The study sample consisted of 465 known hypertensive patients, between the age group of 20-80 years of which 250 patients were males and 215 were females. 105 were between the age group of 1-40 years, 136 in 41-50 years, 110 in 51-60 years, and 114 in 60 and above year of age. Data were statistically analyzed Student's t-test.
Results:
79.14% of the patients presented with Russell's periodontal index score ranging from 2- 4.9 which suggested an established periodontal lesion. The risk factors for old men and women to develop hypertension were 90%, among those who survived to ages 65 to 89 years.
Conclusion:
The frequency of potential oral manifestations in patients with hypertension was significantly high, thus showing an association of gingival and periodontal pathology in hypertensive patients
Keywords: Hypertension, lichenoid reactions, periodontitis
INTRODUCTION
The World Health Organization attributes hypertension, or high blood pressure, as the leading cause of cardiovascular mortality. An elevated arterial pressure is probably the most important public health problem in developed countries.[1] It is common, asymptomatic readily detectable and easily treatable, and if untreated, often leads to complications. Although our understanding of the pathophysiology of elevated arterial pressure has increased, in 90 to 95% of cases the etiology is still largely unknown. As a consequence, in most cases hypertension is treated non-specifically, resulting in the large number of minor side effects and relatively high non-compliance rate. The ratio of hypertension frequency in women versus men increases from 0.6 to 0.7 at age 30 to 1.1 to 1.2 at age 65.[1]
Dentists have a rare opportunity to detect cases of hypertension. It is a professional responsibility of a dental clinician to inform the patient of their hypertensive state and to offer medical advice, including epropriate referrals. There are no recognized oral manifestations of hypertension but antihypertensive drugs can often cause side-effects, such as xerostomia, gingival overgrowth, salivary gland swelling or pain, lichenoid drug reactions, erythema multiforme, taste sense alteration, and parasthesia.[2]
Dental disease has often oral manifestation of acute, chronic, and systemic disease. Studies have indicated that, afflictions such as heart disease, diabetes, stroke, hypertension, multiple sclerosis, and HIV/AIDS often can be discovered during a routine visit to the dentist.[3]
Periodontitis is one of the most chronic infectious diseases. The mouth is an ideal breeding area for bacteria and those affected by periodontal disease are at increased risk, for potentially fatal bacteria entering the bloodstream via infected oral tissue. Those suffering from periodontitis are highly susceptible to major health issues such as premature births and low birth-weight babies, cancer, anorexia, vascular and heart disease including that caused by the introduction of germs that attack the heart's mitral valve.[3,4]
Periodontal disease in an expectant mother has been identified as one of the signs that an infant will be born prematurely or at a low birth weight. People with periodontal disease may be at greater risk of heart attack or stroke. Recent studies have shown that the inflammatory effects of periodontal disease help to promote blood clot formation in arteries.
This clinical study was aimed an investigation the effect or oral manifestations in hypertensive patients.
MATERIALS AND METHODS
0The study sample consisted of 465 known hypertensive patients, between the age group of 20-80 years of which 250 patients were males and 215 were females. About 105 were between the age group of 1-40 years, 136 in 41-50 years, 110 in 51-60 years, and 114 in 60 or above of age, all patients were from different socio-economic status. Patients were examined clinically using a mouth mirror, probe, Williams's periodontal probe to check the periodontal pockets, Russell's periodontal index was used to estimate the gingival and periodontal health and further histopathological examination for mucosal changes was also carried out [Figure 1]. All the patients included in the study were known hypertensive patients and who were under the medication of the antihypertensive drugs.
Figure 1.

Gingival enlargements in hypertensive patients
Oral changes mainly observed were gingivitis, periodontitis, Lichenoid reactions, and hypo salivation and facial nerve paralysis. Gingivitis and periodontitis were confirmed from patients Russell's periodontal index, and hypo salivation was noted by asking questions to the patients regarding symptoms [Figures 2 and 3].[3]
Figure 2.

Lichenoid reactions seen in a hypertensive patient
Figure 3.
Facial paralysis seen in malignant hypertensive patient
RESULTS
From the data recorded it was evident that majority of the hypertensive patients examined during the course of study belonged to the age group of 41-50 years.
Around 79.14% of the patients under study presented with Russell's periodontal index score ranging from 2- 4.9. 85.38% of patients presented with gingival bleeding on probing and were characterized by redness of the marginal gingiva. 16.99% of patients presented with hypo salivation. 4.5% of the total patients presented with lichenoid reactions and they were characterized by linear striations occurring on the buccal mucosa. 1.2% of patients presented with facial nerve paralysis and 16.9% patients presented with gingival enlargement characterized by firm nodular gingival overgrowth seen on both buccal and facial and lingual or palatal aspects of the marginal gingival [Figure 4].
Figure 4.
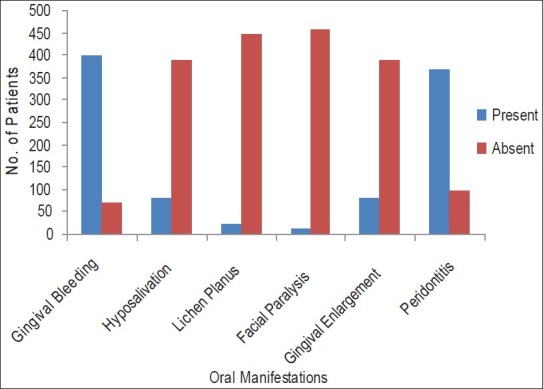
Oral manifestations observed in the clinical observed patients
The risk factors for old men and women to develop hypertension were 90%, among those who survived to ages 65 to 89 years. Systolic BP elevations were found in 87% of hypertensive men and 93% of hypertensive women, as they were examined for their hypertension during this study. This was compatible with our study.
DISCUSSION
Hypertension (HTN) or high blood pressure, sometimes arterial hypertension, is a chronic medical condition in which the blood pressure in the arteries is elevated. This requires the heart to work harder than normal to circulate blood through the blood vessels.
Gingival bleeding was one of the common clinical features seen in hypertensive patients. Patients showed the Russell's periodontal index score of 0.3-0.9. In a study by Mailboridin et al[4] wherein the Russell's index was show to be 2.0-4.9 with 79.14% of the patients presented with the symptoms of periodontitis, was similar to the results of the this present study. Mailboridin et al studied the Micro lympho hemocirculatory bed and leucocytogram of gingival tissue by the light microscopy in patients with chronic periodontitis having normal and high arterial blood pressure. In most cases of arterial hypertension the gingival mucous was characterized by widening of lymphatic vessels and interstitial spaces. In cases of arterial hypertension combination with inflammatory reaction the tendency for widening of lymphatic vessels and interstitial spaces persisted compared with cases of normal blood pressure. It testifies to high probability of lymphogenic generalization of inflammation. Besides, in cases of inflammatory gingival pathology in arterial hypertension the absolute neutrophil number was significantly higher showing for more acute inflammatory process and greater volume of tissue involvement. Thus, concluding that the increased periodontitis in hypertensive patients could probably attributed as one of the manifestation of hypertension.[4] Similar findings were mentioned by Holmlund et al.[5]
Hypo salivation was also found as one of the clinical manifestations in hypertensive patients. This hypo salivation was related to the sustained increase in both systolic as well as diastolic blood pressure and also in patients who were under antihypertensive medication especially with diuretics. There will be decrease in the unstipulated saliva. The results of this study, 16.99% (79) patients who were under medication with diuretics presented hypo salivation. These results were similar to the studies of Tenovuo et al[6] and Glick et al.[7]
Lichen planus like lesions or lichenoid reactions are white lesions characterized by linear striations occurring on the buccal mucosa.[8] They are seen bilaterally and usually in the posterior regions. These are sometimes seen in hypertensive patients as a manifestation secondary to the use of the drug or medication. The most common drugs causing this side effect are the ACE inhibitor drugs especially the captopril. They are characterized by acanthosis, basal cell degeneration, hyperparakeratosis, numerous chronic inflammatory cell infiltrate throughout the connective tissue especially the plasma cells and histiocytes. The results of this study showed 21 patients with lichenoid reactions. The results were similar to the studies of Mandys et al,[9] but this study results did not correlate with the studies of Christensen et al[8] as their investigation did not support the hypothesis of relationship between lichen planus and hypertension.
Facial nerve paralysis in hypertension is because of edema or hemorrhage in the facial canal, but the exact etiology is unknown. Usually facial nerve paralysis is seen in patients with malignant hypertension. It is characterized by the sustained increase in systolic blood pressure ≥ 200 mm HG and/or sustained increase in diastolic blood pressure ≥ 120 mm HG. But it is more significant in patients with increased diastolic blood pressure rather than increase in systolic blood pressure. Facial nerve paralysis was assessed clinically by paralysis of facial musculature, drooling of saliva from the corner of the mouth, loss of wrinkles on the forehead with expressionless appearance, inability to blow, inability to close the eyes and continuous rolling of tears. The results of this present study were similar to the study results of Margabanthu et al, Ellis et al.[10]
Gingival enlargement is also one of the most common clinical finding in patients with ypertension taking anti-hypertensive medication especially calcium channel blockers. Gingival enlargements appear clinically as firm nodules of gingival overgrowth seen on either buccal or facial aspects and lingual or palatal aspects of the marginal gingiva. Sometimes they may even the entire crown causing difficulty in eating. The drugs, which cause the gingival enlargement are amlodipine, nifedipine.
The results of this study showed that 79 patients with gingival enlargement who were under either amlodipine or nifedipine therapy. These results were not significant to the studies of Lawrence et al,[11] and Lafzi et al and Barclay et al.[12,13]
CONCLUSIONS
The study concluded that there is association between hypertension and gingival/periodontal pathology. But the finding failed to assess whether the periodontitis is due to the hypertension per se or not. The mucosal changes were mainly due to the anti-hypertensive drugs. There was some group of people showing increased incidence of dental caries, this may be correlated with the hypo salivation in patients who were under anti-hypertensive therapy. Facial nerve paralysis was associated with the malignant hypertension.
This study concludes the need to do further studies on the relation between hypertension and periodontitis, the relation between hypertension and facial nerve paralysis.
ANNEXURE 1
An affirmative response to at least one of the five following questions about symptoms was shown to correlate with a decrease in saliva:
Does your mouth usually feel dry?
Does your mouth feel dry when eating a meal?
Do you have difficulty swallowing dry foods?
Do you sip liquids to aid in swallowing dry foods?
Is the amount of saliva in your mouth too little most of the time, or don’t you notice it?
ANNEXURE 2
Definations
Xerostomia, also known as dry mouth, is marked by a significant reduction in the secretion of saliva
Erythema multiforme is a skin condition of unknown cause, possibly mediated by deposition of immune complex (mostly IgM) in the superficial microvasculature of the skin and oral mucous membrane that usually follows an infection or drug exposure. It is a common disorder, with peak incidence in the second and third decades of life.
AIDS A severe immunological disorder caused by the retrovirus HIV, resulting in a defect in cell-mediated immune response that is manifested by increased susceptibility to opportunistic infections and to certain rare cancers, especially Kaposi's sarcoma. It is transmitted primarily by exposure to contaminated body fluids, especially blood and semen.
Multiple sclerosis A chronic autoimmune disease of the central nervous system in which gradual destruction of myelin occursin patches throughout the brain or spinal cord or both, interfering with the nerve pathways and causing muscular weakness, loss of coordination, and speech and visual disturbances.
Hypo salivation Abnormally reduced salivation
Facial nerve paralysis is a common problem that involves the paralysis of any structures innervated by the facial nerve. The pathway of the facial nerve is long and relatively convoluted, and so there are a number of causes that may result in facial nerve paralysis.[1] The most common is Bell's palsy, an idiopathic disease that may only be diagnosed by exclusion.
Lichen planus A dermatologic disease of unknown etiology that also occurs in the mouth, on the tongue, or on the lips as smooth lacy networks of white lines or, less commonly, as white patches that may become ulcerative.
Acanthosis Any thickening of the prickle-cell layer of the epidermis; associated with many skin diseases.
ANNEXURE 3
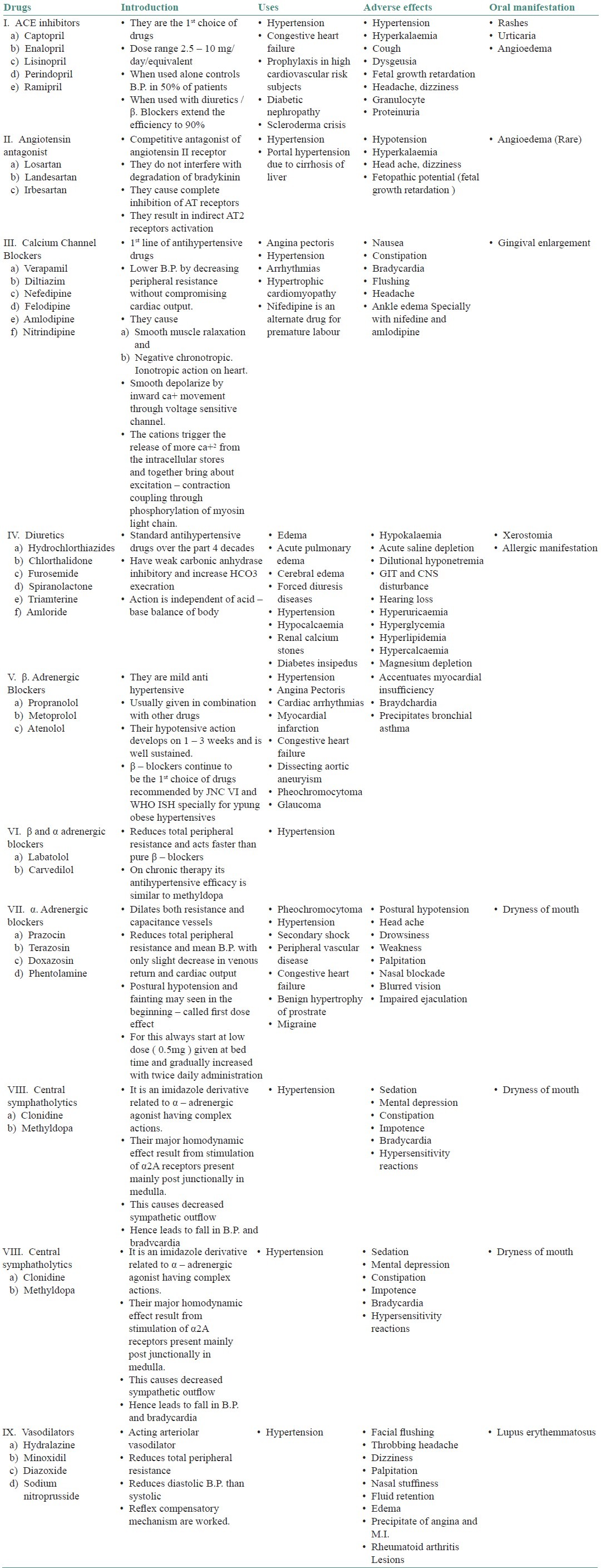
Medications used in the treatment of hypertension and its side effects
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
REFERENCES
- 1.Slots J. Subgingival microflora and periodontal disease. J Clin Periodontol. 1979;6:351–82. doi: 10.1111/j.1600-051x.1979.tb01935.x. [DOI] [PubMed] [Google Scholar]
- 2.Guggenheimer J, Moore PA. Xerostomia: etiology, recognition and treatment. J Am Dent Assoc. 2003;134:61–9. doi: 10.14219/jada.archive.2003.0018. quiz 118-9. [DOI] [PubMed] [Google Scholar]
- 3.Ellis J, Syemour RA, Steela JG, Robertson P, Butler TJ, Thomason JM. Prevalence of gingival overgrowth induced by calcium channel blockers a community based study. J Periodontol. 1999;70:63–7. doi: 10.1902/jop.1999.70.1.63. [DOI] [PubMed] [Google Scholar]
- 4.Maiborodin IV, Kolmakova IA, Pritchina IA, Chupina VV. Changes in gum in cases of arterial hypertension combination with periodontitis. Stomatologiia (Mosk) 2005;84:15–9. [PubMed] [Google Scholar]
- 5.Holmlund A, Holm G, Lind L. Severity of periodontal disease and number of remaining teeth are related to the prevalence of myocardial infarction and hypertension in a study based on 4,254 subjects. J Periodontal. 2006;77:1173–8. doi: 10.1902/jop.2006.050233. [DOI] [PubMed] [Google Scholar]
- 6.Tenovuo J. Salivary parameters of relevance for assessing caries activity in individuals and populations. Community Dent Oral Epidemiol. 1997;25:82–6. doi: 10.1111/j.1600-0528.1997.tb00903.x. [DOI] [PubMed] [Google Scholar]
- 7.Glick M. New guidelines for prevention, detection, evaluation and treatment of high blood pressure. J Am Dent Assoc. 1998;129:1588–94. doi: 10.14219/jada.archive.1998.0105. [DOI] [PubMed] [Google Scholar]
- 8.Christensen E, Holmstrup P, Wiberg-Jorgensen F, Neumann-Jensen B, Pindborg JJ. Arterial blood pressure in patients with oral lichen planus. J Oral Pathol. 1977;6:139–42. doi: 10.1111/j.1600-0714.1977.tb01874.x. [DOI] [PubMed] [Google Scholar]
- 9.Harting MS, Hsu S. Lichen planus pemphigoides: a case report and review of the literature. Dermatol Online J. 2006;12:10. [PubMed] [Google Scholar]
- 10.Margabanthu G, Brooks J, Barron D, Miller P. Facial palsy as a presenting feature of coarctation of aorta. Interact Cardiovasc Thorac Surg. 2003;2:91–3. doi: 10.1016/S1569-9293(02)00110-X. [DOI] [PubMed] [Google Scholar]
- 11.Lawrence DB, Weart CW, Laro JJ, Neville BW. Calcium channel blocker-induced gingival hyperplasia: case report and review of this iatrogenic disease. J Fam Pract. 1994;39:483–8. [PubMed] [Google Scholar]
- 12.Lafzi A, Farahani RM, Shoja MA. Amlodipine-induced gingival hyperplasia. Med Oral Patol Oral Cir Bucal. 2006;11:E480–2. [PubMed] [Google Scholar]
- 13.Barclay S, Thomason JM, Idle JR, Seymour RA. The incidence and severity of nifedipine-induced gingival overgrowth. J Clin Periodontol. 1992;19:311–4. doi: 10.1111/j.1600-051x.1992.tb00650.x. [DOI] [PubMed] [Google Scholar]


