Abstract
Lipoma is a common soft-tissue tumor. There are only very few reported cases of intraosseous lipoma of the jaws in the literature. Intraosseous angiolipomas are even rarer. The exact nature of these lesions is debatable, but it is widely accepted that they represent true benign tumors. These are slow-growing tumor consisting of a mass of mature fat cells. When the vascular component within these tumors is a prominent feature, they are considered to be angiolipomas. The cause of these lesions is uncertain. Clinically, intraosseous lipoma may be asymptomatic, may cause swelling, or may show neurologic signs such as hypesthesia or paresthesia, as was manifested in this case. Radiographically, the lesion usually appears as a well-circumscribed radiolucency. The diagnosis of intraosseous lipoma of the mandible may be a challenge, due to its rarity and clinical similarity with many other radiolucent jaw lesions; therefore, the histopathological examination is always required. Here, we report a case of intraosseous angiolipoma of mandible in a 21-year-old female patient.
Keywords: Angiolipoma, intraosseous, lipoma, mandible
INTRODUCTION
Angiolipoma, a histological variant of lipoma, is one of the rare tumors with its characteristic histology consisting of mature adipose tissue and interspersed proliferated vascular component. It accounts for 5–17% of lipomas.[1]
Lipoma is a benign soft-tissue tumor of mature adipose tissue with no cellular atypia present. It can occur anywhere in the human body where adipose tissue is present. They can be encapsulated or diffuse.[2] These are most common soft-tissue tumor, and about 20% of cases occur in the head and neck region. However, only 1–4% of cases involve the oral cavity. Oral lipomas represent 0.5–5% of all benign oral cavity neoplasms.[3]
Oral lipomas can occur in various anatomic sites including the major salivary glands, buccal mucosa, lip, tongue, palate, vestibule, and floor of mouth. The most recent classification of benign lipomatous tumors includes the following categories: classic lipoma, lipoma variants, such as angiolipoma, chondroid lipoma, myolipoma, and spindle cell/pleomorphic lipoma, all with specific clinical and histologic features, hamartomatous lesions, diffuse lipomatous proliferations, and hibernoma.[4]
The occurrence of multiple lipomas is associated with Cowden's syndrome or multiple hamartoma syndrome. This condition is either familial or sporadic and is associated with the predominantly postpubertal development of a variety of cutaneous, stromal, and visceral neoplasms, resulting from mutations of the phosphatase and tensin homolog (PTEN) gene.[3]
Although adipocytes are distributed throughout the bone marrow of the human skeleton, lipomas have been considered infrequent primary intraosseous tumors. A search for cases of jaw lipoma revealed that only a limited number of maxillary lipomas have been documented. Occurrence of true intraosseous mandibular lipoma (IML) is extremely rare.[2]
Probably, the first intraosseous lipoma was described by Brault, in 1868, involving the diaphysis of the femur. Several have since been reported. Since then, intraosseous lipomas have been reported in the fibula, the tibia, the ulna, and frontal bone, the calcaneus, the humerus, and the rib.[5–7] IML was first fully reported half a century ago by Maurice Oringer.[2]
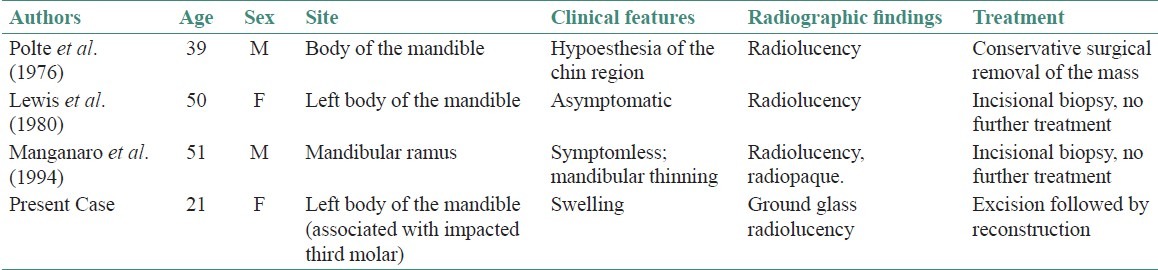
The intraosseous lipoma is a benign, slow-growing tumor consisting of a mass of mature fat cells. When the vascular component within these tumors is a prominent feature, they are considered to be angiolipomas. The cause of these lesions is uncertain.[6] Since the first report of intramandibular angiolipoma by Polte et al, the available literature shows that there have been only 3 reports of intramandibular angiolipoma [Table 1]. We hereby report another case of intramandibular angiolipoma.
Table 1.
Clinical, radiographic, and histopathologic features of the previous reported intraosseous angiolipomas of the mandible
CASE REPORT
A 21-year-old woman in apparently good general health was referred to us with the chief complaint of swelling on the lower left side of the face since 5 years [Figure 1a]. It was not associated with pain, paresthesia, or discharge.
Figure 1.
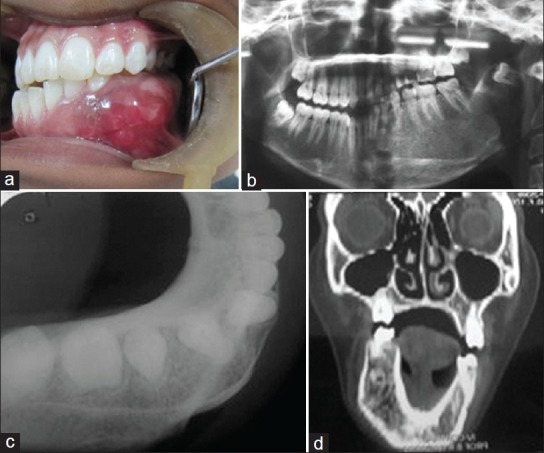
(a) Preoperative intraoral view of the lesion; (b) Panoramic radiograph showing a radiolucent lesion extending from left ramus to right parasymphyseal area with impacted a third molar; (c) Occlusal radiograph showing the expansion of the buccal and lingual cortical plate; (d) Computed tomographic image showing expansile lesion
Intraoral examination revealed a fixed swelling present with respect to the symphysis and left body of the mandible. Radiographic examination showed presence of ground glass radiolucency with distinct borders and extended from the right mandibular lateral incisor to the left ramus. An impacted molar tooth was present in relation to the left ramus. There was no evidence of root resorption [Figures 1b–1d]. Laboratory investigations revealed that the serum calcium, serum phosphorus, and alkaline phosphatase levels were within normal limits. The clinical impression was that this lesion was either a vascular malformation or an odontogenic cyst or tumor.
In attempt to take incisional biopsy, the lesion was explored surgically from an intraoral approach. Excessive bleeding was encountered. Vascular malformation was suspected and patient was asked to get an angiogram done. Patient did not give consent for an angiogram to be done. Surgeons on the basis of provisional diagnosis decided to resect the mandible. Patient's consent was obtained. Reconstruction was done following resection of the tumor mass.
Part of the resected specimen was submitted to the Department of Oral Pathology. The accompanying provisional diagnoses were “vascular malformation,” “hemangioma,” and “central giant cell granuloma.” After recording the gross macroscopic feature, a part of bone was removed and kept for decalcification. The bone bit was typically floating in the acid solution.
On histological examination, the lesion consisted of well-delineated lobules of mature fat separated by anatomizing septa composed of loose fibrous connective tissue. Interspersed throughout these lobules of fat were numerous endothelium-lined spaces of varying sizes [Figures 2a and 2b]. These endothelium-lined spaces were congested with erythrocytes, and thrombus formation was evident at their periphery. Except for numerous mast cells present throughout the fibrous connective tissue septa, there was an absence of inflammatory cells in the lesion. There was no evidence of a hematopoietic marrow component.
Figure 2.
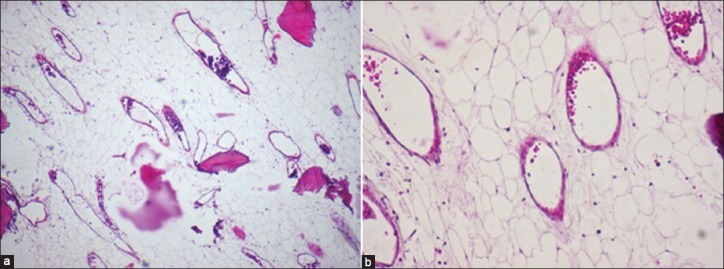
(a, b) Numerous vascular spaces interspersed throughout stroma of mature fat cells, with few bony spicules. (Hematoxylin and eosin stain, original magnification ×40, ×100).
A microscopic diagnosis of angiolipoma was made.
DISCUSSION
Mandibular lesions have a wide range of pathologic features but a similar imaging appearance, hence familiarity with embryologic characteristics, and secondary findings is crucial. Taking into account the patient's age, location within the mandible, radiological appearance, and effect of the lesion on adjacent structures, a number of pathological processes may be considered for diagnosis. But as the patient does not give any history of pain or rapid or sudden change in the size of the lesion, we can rule out a malignant disease process. Benign lesions namely central giant cell granuloma, fibro-osseous lesion, odontogenic cyst and tumors, arteriovenous malformation, hemangioma, aneurysmal bone cyst, and hemorrhagic bone cyst could be considered in the list of differential diagnosis but can be easily ruled out following histopathological examination.[8]
Lipomas, lipomatosis, lipoblastoma, lipoblastomatosis, angiolipomas, myolipomas, chondroid lipomas, spindle cell lipomas, and pleomorphic lipomas are the benign adipose tissue tumors that can mimick the condition.[1]
The solitary lipoma is a common soft-tissue tumor that reflects a proliferation of histologically and chemically (in composition of fatty acids) normal adipose tissue. Solitary lipoma is not developmental in origin and thus is not properly considered a hamartoma, but rather a true neoplasm; lipoblastomatosis, on the other hand, appears to be a true hamartoma of the buccal fat pad.[9]
If the vascular component of the connective tissue septa in these tumors is prominent (15–40%), the tumor is more properly considered to be an angiolipoma; the endothelial cells may be plump and surrounded by immature fat cells, but the tumor is benign. It is believed that this variant is preceded by a simple lipoma which undergoes capillary and fibrous proliferation from the periphery.[9] These angiolipomas are benign lipomatous lesions, which were first defined by Bowen in 1912 and differentiated from lipomas histopathologically by Howard in 1960.[1]
Occurrence in the head and neck is rare, but a lipoma with a rich vascular component deserves a critical appraisal, since recurrence is likely. There is varying ratio of fat to angiomatous elements in different areas of the tumor.[9]
Although adipocytes are distributed throughout the bone marrow of the human skeleton, lipomas have been considered infrequent primary intraosseous tumors.[5,10]
Hart in an extensive review of the subject, has classified fatty tumors affecting bone as follows: (1) soft-tissue lipomas or liposarcomas which secondarily involve bone, (2) periosteal lipomas, (3) intraosseous lipomas, and (4) liposarcomas of bone.[10]
Lipomas have been reported in the long bones, such as the humerus, radius, femur, tibia, fibula, as well as the calcaneus and cervical spine, whereas the ribs, pelvis, and skull are the common sites in the flat bone. A search for cases of jaw lipoma revealed that only a limited number documented case. Occurrence of true IML is extremely rare.[2]
In the dental literature, Oringer in 1948 described a lipoma in the body of the mandible associated with the mesial and distal roots of a mandibular second molar. In 1969, Johnson reported an intraosseous lipoma in the ramus of the mandible, which was stated to have some increased vascularity. A third lesion of the mandible, diagnosed as a fibrolipoma, was reported by Newman.[5–7]
The etiology and pathogenesis of mandibular central angiolipoma remain unclear. The clinical history and anatomic site suggest the trauma (caused due to extraction) as a possible cause of the lesions. Trauma as an etiologic agent in intraosseous lipomas has been previously suggested; however, Hart was able to document trauma in only 4 of the 28 cases. He noted that it is difficult to establish a causal relationship over long periods of time and concluded that trauma as a causal agent is unlikely.[10]
In a series of 3,829 examinations of the vertebrae, Junghanns found intraosseous lipomatous areas present in 0.6% of all the cases. He never encountered these in patients under 50 years of age and suggested that these findings represented fatty degeneration of the bone marrow.[7] However in our case, the patient is relatively young so fatty degeneration of bone marrow is ruled out.
Johnson in the year 1969 reported a case of an intraosseous lipoma of the mandible involving impacted teeth. After his initial report, Miller in 1982 also reported an intraosseous lipoma associated with impacted left mandibular third molar.[5] Our case also documents the existence of an intraosseous lipoma in relation to impacted tooth. However, sufficient numbers of cases are yet not available to find an association between impacted tooth and an intraosseous lipoma.
Recently, mast cells have been thought to mediate angiogenesis in various pathophysiological conditions .Also, in angiolipomas, it has been speculated that mast cells might play some roles in their increased vascularity, based on the data that angiolipomas had 10 times the number of mast cells than classic lipomas. However, there has been no direct demonstration of molecular mechanisms for angiogenesis participation by mast cells in angiolipoma.[11] In the present case also mast cells were associated with the lesion but no direct correlation was demonstrated.
The symptoms of IML depend mainly on location and size of the tumor. In cases where nerves are not involved and there is no infection, IML remains asymptomatic for many years and may cause only painless swelling. With extensive enlargement of an IML and pressure on the nerve trunks, a sensory change in the form of paresthesia or hypersthesia can result. Therefore, swelling, pain, and paresthesia remain the most significant symptoms and signs of IML.[5,6] In the reported case, there were no symptoms, and the only sign was a painless swelling that was radiographically seen as radiolucency.
Since intraosseous lipoma of the jaws is an extremely rare diagnosis, it is obviously important to exclude the possibility of hematopoietic bone marrow with prominent areas of fibro-fatty change. In fact, some authors have suggested that it may not be possible to differentiate intraosseous lipoma from an osteoporotic bone marrow defect.[12] We feel that both the clinical and microscopic evidence in the current case support the diagnosis of intraosseous angiolipoma.
Till date, the most accepted theory regarding the origin of intraosseous angiolipoma of the mandible include trauma, possibly related to a previous extraction. Other theories include fatty metamorphosis of a central hemangioma and or it can be a possible variant of the osteoporotic bone marrow defect.[9]
Hemangiomas generally are present at birth and become apparent within the first two decades of life. All the currently reported cases fall beyond the accepted age range for hemangioma.
The osteoporotic bone marrow defect favors the posterior mandible, and occurs most commonly in females. It contains mature adipocytes but lacks a prominent vascular component.
The intraosseous angiolipoma may thus represent either hyperplasia of fat, with an associated increase in the vascular channels, or a true neoplasm. There are, unfortunately, insufficient cases to permit a more conclusive determination.[13]
CONCLUSION
Lipomas are common mesenchymal neoplasms in the oral cavity. Angiolipoma is a variant of lipoma exhibiting proliferating capillaries admixed with mature adipocytes. However, the diagnosis may be difficult for lesions occurring in bone. The origin and cause of intraosseous angiolipomas are not certain. It has been said that they may arise from the adipose tissue of bone marrow. The diagnosis of intraosseous lipoma is given to an intramedullary lesion that shows benign behavior and is shown histologically to be composed of mature fat cells admixed with vascular tissue. It is important for practicing oral pathologists to recognize rare or unusual variants to ensure accurate diagnosis and appropriate treatment for the patient.
ACKNOWLEDGMENT
We extend our heartfelt thanks to Dr. Girrish G. Giraddi for providing the detailed clinical history, clinical photographs and the treatment plan of the patient.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
REFERENCES
- 1.Kacar S, Kuran S, Temucin T, Odemis B, Karadeniz N, Sasmaz N. Rectal angiolipoma: A case report and review of literature. World J Gastroenterol. 2007;13:1460–5. doi: 10.3748/wjg.v13.i9.1460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Buric N, Krasic D, Visnjic M, Katic V. Intraosseous mandibular lipoma: A casereport and review of the literature. J Oral Maxillofac Surg. 2001;59:1367–71. doi: 10.1053/joms.2001.27538. [DOI] [PubMed] [Google Scholar]
- 3.Bandéca MC, de Pádua JM, Nadalin MR, Ozório JE, Silva-Sousa YT, da Cruz Perez DE. Oral soft tissue lipomas: A case series. J Can Dent Assoc. 2007;73:431–4. [PubMed] [Google Scholar]
- 4.Furlong MA, Fanburg-Smith JC, Childers EL. Lipoma of the oral and maxillofacial region: Site and Subclassification of 125 cases. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2004;98:441–50. doi: 10.1016/j.tripleo.2004.02.071. [DOI] [PubMed] [Google Scholar]
- 5.Miller WB, Ausich JE, Mcdaniel RK, Longo JJ. Mandibular intraosseous lipoma. J Oral Maxillofac Surg. 1982;40:594–6. doi: 10.1016/0278-2391(82)90291-9. [DOI] [PubMed] [Google Scholar]
- 6.Polte HW, Kolodny SC, Hooker SP. Intraosseous angiolipoma of the mandible. Oral Surg Oral Med Oral Pathol. 1976;41:637–41. doi: 10.1016/0030-4220(76)90316-9. [DOI] [PubMed] [Google Scholar]
- 7.Barker GR, Sloan P. intraosseous lipomas: Clinical features of a mandibular case with possible aetiology. Br J Oral Maxillofac Surg. 1986;24:459–63. doi: 10.1016/0266-4356(86)90063-x. [DOI] [PubMed] [Google Scholar]
- 8.Dunfee BL, Sakai O, Pistey R, Gohel R. radiologic and pathologic characteristics of benign and malignant lesions of the mandible. Radiographics. 2006;26:1751–68. doi: 10.1148/rg.266055189. [DOI] [PubMed] [Google Scholar]
- 9.Greer RO, Richardson JF. The nature of lipomas and their significance in the oral cavity: A review and report of cases. Oral Surg Oral Med Oral Pathol. 1973;36:551–7. doi: 10.1016/0030-4220(73)90313-7. [DOI] [PubMed] [Google Scholar]
- 10.Lewis DM, Brannon RB, Isaksson B, Larsson A. Intraosseous angiolipoma of the mandible. Oral Surg Oral Med Oral Pathol. 1980;50:156–9. doi: 10.1016/0030-4220(80)90204-2. [DOI] [PubMed] [Google Scholar]
- 11.Ida-Yonemochi H, Swelam W, Saito C, Saku T. Angiolipoma of the buccal mucosa: A possible role of mast cell-derived VEGF in its enhanced vascularity. J Oral Pathol Med. 2005;34:59–61. doi: 10.1111/j.1600-0714.2004.00230.x. [DOI] [PubMed] [Google Scholar]
- 12.Darling MR, Daley TD. Radiolucent lesion of the anterior mandible. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2005;99:529–31. doi: 10.1016/j.tripleo.2004.12.022. [DOI] [PubMed] [Google Scholar]
- 13.Manganaro AM, Hammond HL, Williams TP. lntraosseous Angiolipoma of the Mandible: A Case Report and Review of the Literature. J Oral Maxillofac Surg. 1994;52:767–9. doi: 10.1016/0278-2391(94)90498-7. [DOI] [PubMed] [Google Scholar]


