Abstract
OBJECTIVE
Management of diabetic foot infection (DFI) has been hampered by limited means of accurately classifying disease severity. New hybrid nuclear/computed tomography (CT) imaging techniques elucidate a combination of wound infection parameters not previously evaluated as outcome prognosticators. Our aim is to determine if a novel standardized hybrid image–based scoring system, Composite Severity Index (CSI), has prognostic value in DFI.
RESEARCH DESIGN AND METHODS
Masked retrospective 99mTc-white blood cell (WBC) single photon emission CT (SPECT)/CT image interpretation and independent chart review of 77 patients (101 feet) suspected of DFI-associated osteomyelitis at a large municipal hospital between January 2007 and July 2009. CSI scores were correlated with probability of favorable outcome (no subsequent amputation/readmission after therapeutic intervention) during median 342-day follow-up.
RESULTS
CSI ranged from 0–13. Receiver operating characteristic accuracy for predicting favorable outcome was 0.79 (optimal cutoff CSI, ≤2; odds ratio of therapeutic failure for CSI >2, 15.1 [95% CI 4.4–51.5]). CSI of 0 had a 92% chance of favorable outcome, which fell progressively to 25% as indices rose to ≥7. Image-based osteomyelitis versus no osteomyelitis assessment was less accurate than CSI at predicting outcome (P = 0.016). In patients with intermediate severity (CSI 3–6), treatment failure decreased from 68 to 36% when antibiotic duration was extended to ≥42 days (P = 0.026).
CONCLUSIONS
99mTc-WBC SPECT/CT hybrid image–derived wound infection parameters incorporated into a standardized scoring system, CSI, has prognostic value in DFI.
Assessing the severity of diabetic foot infection (DFI) often requires imaging studies that may be difficult to interpret due to the variable interaction of superimposed infectious and non infectious processes (1–3). Plain X-ray findings lag behind the actual progression of infection into bone. Three-phase bone scanning with 99mTc-methyl diphosphonate (MDP) is quite sensitive for osteomyelitis, but has poor specificity due to common degenerative/reparative changes unrelated to an active infection (4,5). Radiolabeled white blood cell (WBC) imaging is more specific for infection; however, it lacks anatomic spatial resolution, limiting ability to separate soft tissue from bone involvement (6–8). Dual isotope imaging using 111In-WBC and 99mTc-MDP or 99mTc-Sulfa colloid attempts to circumvent these limitations (9–11); however, it is still limited in demonstration of the extent of disease and therefore provides little improvement in accuracy (4,8,11). Magnetic resonance imaging (MRI), the current imaging procedure of choice, has higher spatial resolution and sensitivity, but as above, suffers specificity especially when Charcot or other noninfectious changes are present (8,12–16).
New hybrid imaging technologies combine single photon emission computed tomography (SPECT) localization of radiolabeled WBC and high-resolution diagnostic-quality X-ray CT (99mTc-WBC SPECT/CT). This technologic advance offers significant improvements in both assessment of local WBC scintigraphic intensity and detailed depiction of cortical bone destruction (17,18). Yet, to date, there has been limited evaluation of this technology’s newly available combination of wound infection parameters as diagnostic markers for extent of disease (17,19–21). Moreover, there remains a paucity of data establishing the potential role of radiolabeled WBC SPECT/CT in direct treatment guidance for patients in clinical settings (19–23).
It is our hypothesis that the severity of DFI is best gauged by compositing key anatomic and physiologic parameters available from 99mTc-WBC SPECT/CT images (specifically WBC intensity, number, and anatomic location of lesions, as well as radiographic evidence of adjacent disrupted bone architecture) into a computed Composite Severity Index (CSI) (23,24). We also propose that such a multifactorial interpretation scheme can offer an integrated diagnostic and prognostic assessment, benchmarking a continuous spectrum of disease severity that allows for more accurate, real-time, and customized patient management. Thus, we have assessed the utility of hybrid imaging and this novel interpretation scheme via its ability to accurately predict the probability of favorable clinical outcomes.
RESEARCH DESIGN AND METHODS
Selection and description of the participants
This study was performed in retrospective fashion. Diabetic patients with clinically suspected DFI (including but not limited to erythematous changes, drainage, ulceration, and systemic symptoms such as fevers) who underwent 99mTc-WBC SPECT/CT imaging at our hospital between January 2007 and July 2009 (n = 94) were screened by chart review for inclusion in the study. Those patients with both documented follow-up of at least 3 months (follow-up median 325.4 days, SD ± 148.8) after completion of initial therapy (n = 79) and technically satisfactory image acquisition were included in the study (n = 77). Seventy-seven diabetic patients with either unilateral or bilateral infected feet (total of 101 feet) met these criteria. Institutional review board approval was obtained. and informed consent was waived for this study.
Imaging methods and display technique
SPECT/CT images were acquired on Symbia T2 (Siemens Medical Systems) dual-head mounted with low-energy, high-resolution collimators, 2 h after injection of 20–25 mCi of autologous 99mTc-WBC. SPECT parameters were as follows: 180°, 32 views at 45 s/view × 2 heads for 64 views total, 128 × 128 matrix, zoom factor 1.23, 20% energy window centered on 141 keV 99mTc peak. Reconstruction was performed using CT-based attenuation-correction and iterative reconstruction (Siemens Flash 3D; Siemens Medical Systems) using 4 subsets at 10 iterations. CT images were acquired with 130 kVp, 50 mAs (effective) helical scans and reconstructed as 1-mm slices on 0.7 centers. A B80s sharp reconstruction kernel was used. Pitch was in the range of 0.9–1.25. Images were displayed on an E-Soft workstation (Siemens Medical Sytems) multiformat fused SPECT/CT display including rotating 3D Maximum Intensity Projection of the SPECT data. Coronal, sagittal, and axial WBC slice data were overlaid on the CT slice in color individually windowed so that maximum intensity was obtained in at least one pixel in a given infection focus. Background subtraction was adjusted to remove adjacent soft tissue activity without removing the smooth gradation of activity from the epicenter of the focus to its peripheral margin. CT data were evaluated with bone and soft tissue windows (B40s reconstruction kernel). Bilateral foot infections were evaluated as separate events.
Image interpretation
Retrospective SPECT/CT image interpretation was performed 14 weeks after conclusion of the accrual period by randomly assigning images to either of two attending physicians, each with >15 years of experience in clinical nuclear medicine and radiology. Interpreters were blinded to all clinical and laboratory information other than the deidentified study images. Interpreters were instructed to score images of each infected foot according to the a priori criteria of the CSI, described below and defined in Table 1. To ensure consistent application of the diagnostic criteria, a third investigator was present for all interpretations and recorded the results into a coded database.
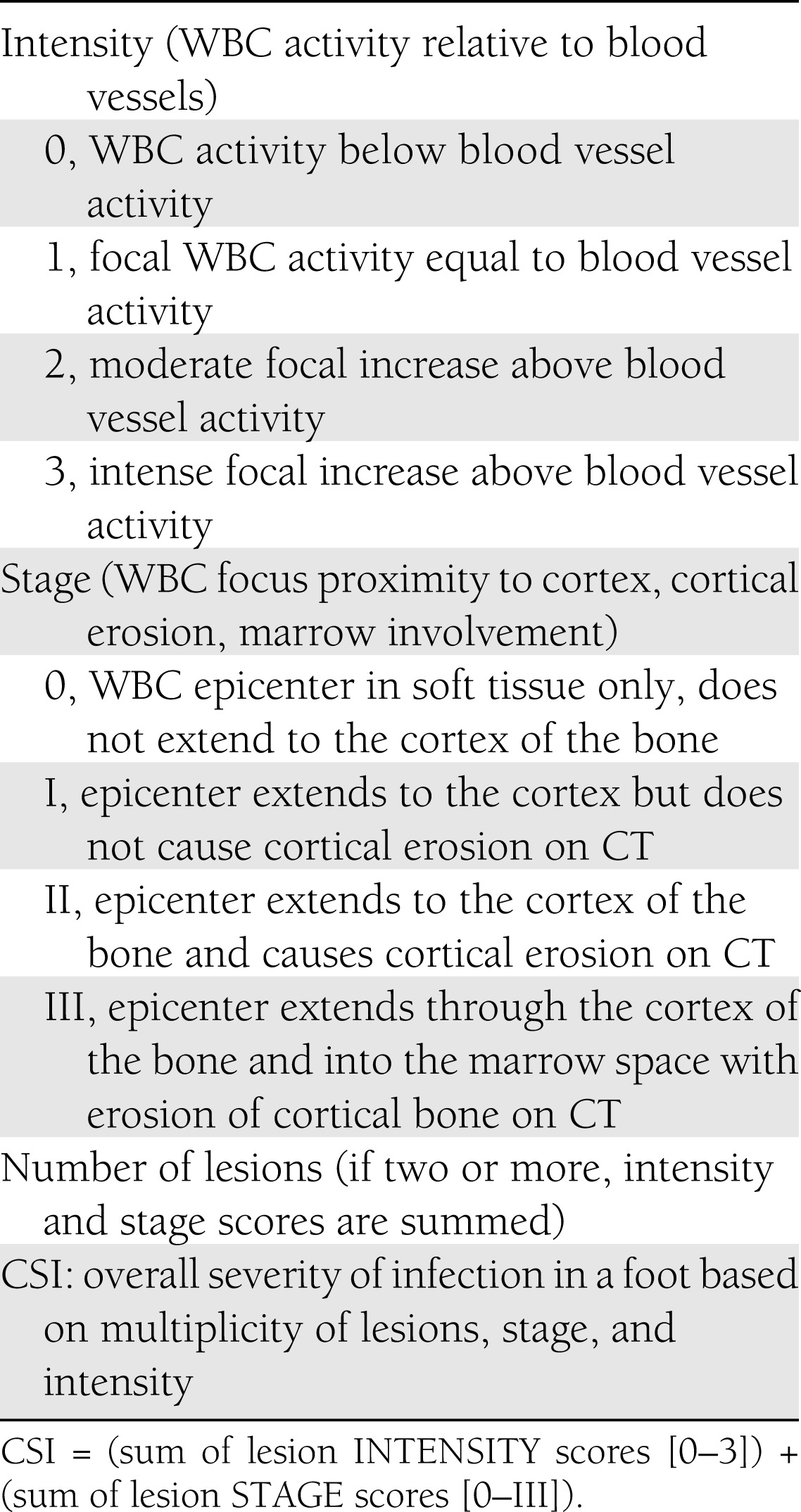
Table 1.
CSI staging system for diabetic foot infection
A second interpretation of all the studies was performed at a remote time (440 days median) using the osteomyelitis versus no osteomyelitis criteria. As above, images were randomly assigned to either of the original two attending physicians for interpretation. Receiver operating characteristic (ROC) curves of aggregate interpreter accuracy during the initial and remote interpretation sessions were compared.
CSI interpretation method.
We have previously explored some aspects of the clinical implications of 99mTc-WBC SPECT/CT of DFI regarding: 1) relative amount of WBC accumulation, 2) WBC activity proximity to bone, 3) multiple separate adjacent WBC foci, and 4) correlation of bone cortical disruption and WBC activity (21,23,24).
On the basis of the above experience, we constructed the CSI on the concept that among patients whose limbs have not progressed to complete nonviability (i.e., dry gangrene), the presence of more intense WBC activity, more extensive bone involvement, and more numerous inflammatory foci all reflect more severe disease. Thus, CSI interpretation involves a relatively simple grading of each individual focus of infection for the following features:
Intensity: scintigraphic activity of each WBC focus visually quantified via comparison with WBC activity noted in the region of the posterior tibial and/or peroneal vessels on the Maximum Intensity Projection image (score 0–3) (Table 1 and Supplementary Fig. 1).
Stage: progression of WBC infiltration, ranging from isolated soft tissue involvement to involvement (including destruction) of bone cortex and marrow (score 0–III) (Table 1 and Supplementary Fig. 2).
To account for the impact of multiple lesions, the CSI is computed as the sum total of all intensity scores and stage scores for all lesions in a given foot. Thus, the final CSI score for a foot with one lesion may range from 0–6, two lesions may range from 0–12, and so on (Table 1 and Supplementary Fig. 3).
Conventional binary (osteomyelitis vs. no osteomyelitis) interpretation method.
To determine if the combined anatomic and physiologic features incorporated into the CSI interpretation scheme (described above) improved accuracy for predicting outcome, a separate retrospective blinded analysis using the standard binary diagnostic algorithm was performed for comparison purposes. The conventional interpretation of DFI imaging has been based on the concept that DFI involving bone (i.e., osteomyelitis) portends a worse prognosis than DFI limited to soft tissue, and duration and route of antimicrobial therapy have historically been based on this principle. In this analysis, WBC activity that abutted the bone cortex or extended into the marrow space was reported as osteomyelitis, whereas WBC activity localized only in soft tissue was reported as no osteomyelitis.
Antibiotic therapy duration and therapy outcome interpretation
Independent chart review was performed by an investigator not responsible for clinical image interpretation. Favorable outcome was defined as resolution of DFI symptoms, either at the completion of initial therapy or after additional outpatient therapy, without recurrence during the follow-up period. Unfavorable outcome was failure to resolve symptoms after initial therapy or recurrence of symptoms that required hospitalization for additional therapy and/or amputation.
Despite a scarcity of evidence-based data available to guide the clinician, DFI with evidence of osteomyelitis has historically been managed with prolonged antibiotic courses (≥6 weeks) versus shorter therapeutic courses (14 days) for DFI limited to soft tissue structures or superficial wounds (1,2). On that basis, our subjects were additionally divided into two groups (those who received <42 days vs. ≥42 days of antimicrobial therapy) to further analyze the impact of antimicrobial duration on clinical outcomes for a given CSI.
Statistical analysis
Descriptive statistics were used to summarize patient demographics, characteristics, and image-based results. Logistic regression analysis was used to determine the role of CSI as a predictor of successful clinical outcome. Based on this model, the ROC curve analysis was used to determine the optimal cutoff value of CSI in predicting the outcome. Accuracy of CSI in predicting outcome was evaluated with area under the ROC curve (AUC) and also through its positive predictive value (PPV); that is, probability of predicting treatment success given different discrete levels of CSI (0, ≤1, ≤2, and so on). Comparisons of the accuracy of CSI versus the conventional image interpretation methods were made using ROC analysis, which adjusted for the duration of antibiotic therapy as covariate, using DeLong, DeLong, and Clarke-Pearson’s method (25). The 95% CIs on AUC were also computed. The Fisher exact test was used to compare percentages between groups. Statistical analyses were performed using SAS Version 9.2 (SAS Institute, Cary, NC) and SigmaPlot Version 11.2 (Systat Software).
RESULTS
Patient demographics and image interpretation reproducibility
Image sets were technically adequate in a total of 77 patients imaged during the study period (January 2007–July 2009). No adverse events from the index tests were reported. Most infections were characterized by a single focus in the forefoot and occurred with equal frequency in the right or left foot (Supplementary Table 1 and Fig. 1). Mean antibiotic duration was 40 days, but ranged from 0–9 months. Approximately 50% of patients had osteomyelitis according to the conventional image diagnostic criteria described above. Antibiotic regimens varied (including various combinations of amoxicillin/clavulanate, clindamycin, doxycycline, minocycline, vancomycin, ertapenem, ceftriaxone, ciprofloxacin, levofloxacin, and linezolid). The assessment of test interpretation reproducibility using osteomyelitis versus no osteomyelitis criteria showed ROC-derived accuracy of 0.69 for the initial readings and 0.66 (P = 1.000) for the remote interpretations. Complete patient details and image interpretation results are summarized in Supplementary Tables 1 and 2, respectively.
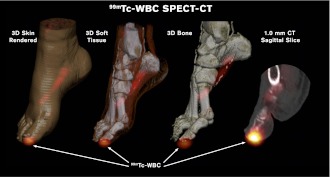
Figure 1.
99mTc‐WBC SPECT/CT hybrid image of diabetic foot with osteomyelitis of first digit terminal tuft. Extent, depth, severity, and bone involvement of infection were not clinically apparent. Hybrid image CSI score was 6. (A high-quality digital representation of this figure is available in the online issue.)
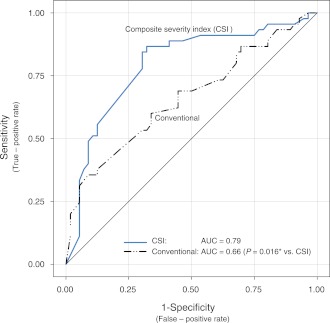
The probability of CSI predicting a favorable outcome (i.e., PPV as a function of CSI) was determined. Patients with CSI of 0 showed a 92% PPV, which declined incrementally to 25% in patients with CSIs of ≥7. In short, as the CSI increased, the probability of favorable outcome decreased and that of treatment failure increased (Supplementary Fig. 4). The ROC-derived optimal cut point in predicting therapeutic outcome was a CSI ≤2 (not shown). The CSI accuracy (AUC) was 0.79 (Fig. 2). The odds ratio of therapeutic failure for patients with CSI >2 versus those with CSI ≤ 2 was 15.1 (95% CI 4.4–51.5).
Figure 2.
ROC analysis comparing accuracy of CSI versus conventional binary diagnostic method for predicting outcome. CSI shows significantly improved accuracy in predicting therapy outcome for diabetic foot infections. (A high-quality color representation of this figure is available in the online issue.)
CSI staging system is more accurate than conventional imaging interpretation method
The accuracy of the CSI at therapeutic outcome prediction was compared with that of the conventional binary interpretation methods using ROC analysis, which was modeled to account for the duration of antibiotic therapy (Fig. 2). Both duration of antibiotic therapy (P = 0.004) and CSI were significant predictors of therapeutic failure (P < 0.001). CSI was statistically more accurate than the conventional binary interpretation method at predicting therapeutic outcome in our study population (P = 0.016).
CSI identifies patients who may benefit from extended antibiotic therapy
Twelve study participants with limited (<10 days) preamputation antibiotic therapy were excluded from this subanalysis, as they were not determined to benefit from conservative medical management. Using logistic regression, the predicted probability of therapeutic failure was lower (<30%) when CSI was low (0–2) and higher (>70%) when CSI was high (7–13). For low CSI of 0–2, sensitivity was ≥90%; for high CSI of 7–13, specificity was ≥90%.
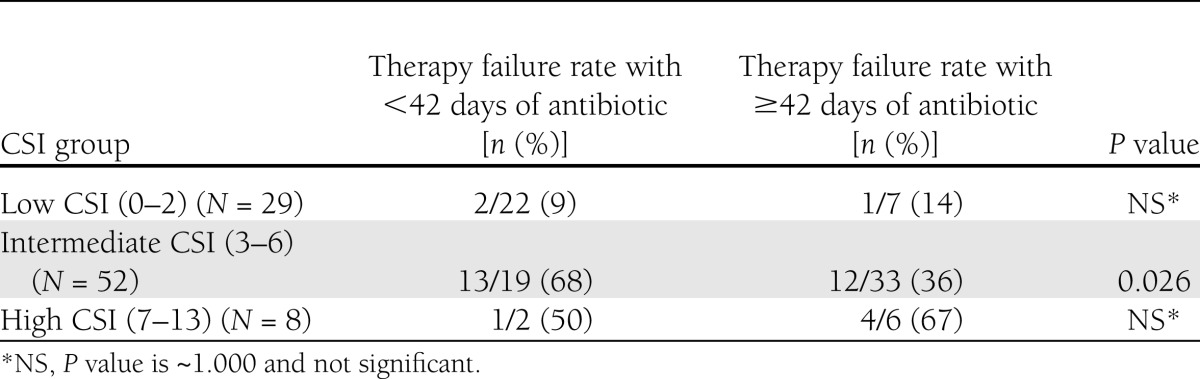
CSI of 3–6 was defined as intermediate range, because for these subjects, both sensitivity and specificity for predicting therapeutic outcome were <90%. Therefore, CSI scores were reorganized into three subgroups: low (CSI 0–2), intermediate (CSI 3–6), and high (CSI 7–13). Table 2 shows the therapeutic failure rate among those receiving antibiotic therapy for <42 days versus ≥42 days for each group. The failure rate did not change based on duration of the antibiotic therapy in either the low or high CSI groups (P = 1.000). However, in the intermediate CSI group (CSI 3–6), the failure rate decreased from 68 to 36% when the duration of therapy increased from <42 days to ≥42 days (P = 0.026).
Table 2.
Influence of antibiotic treatment duration on therapy failure in different CSI groups
Of note, our proposed CSI algorithm did not require radiographic evidence of osteomyelitis to achieve a high CSI, nor was evidence of osteomyelitis as predictive of therapeutic failure as a high CSI in our study population.
CONCLUSIONS
We have shown that dual modality SPECT/CT scanners can be used to demonstrate a spectrum of DFI characteristics not previously achievable with conventional imaging methods. Moreover, these characteristics can be integrated into a prognostic algorithm (CSI) that in our study sample outperformed the osteomyelitis-based standard that has historically defined clinical decision-making (Fig. 2).
Specifically, patients who achieved low CSI values (0–2) were very likely to have favorable outcomes, whereas those with high CSI values (7–13) fared poorly; there was no benefit to prolonged antibiotic therapy in either group. Conversely, over half the study patients fell into an intermediate CSI group (3–6), and regardless of whether bone involvement was evident scintigraphically, they were almost twice as likely to benefit if antibiotic therapy was continued for ≥6 weeks (Table 2). This finding may be of particular value for clinical decision-making, because the wide range of clinically moderate infections remains difficult to separate from infections of greater or lesser severity via available diagnostic methods (1).
The CSI approach to interpreting DFI hybrid imaging is analogous to clinical wound-scoring systems in that semiquantitative grading of observed features are combined to risk stratify patients for outcome and thus aid management decisions.
The majority of DFI wound scoring systems focus on local pathology of individual ulcers (26). More recently, investigators have incorporated signs and symptoms of infection in addition to local wound measurements for successful prediction of outcome (27).
Our image-based CSI reflects a new perspective on evaluation of wound and infection features that are not readily visible to the clinician observer (e.g., depth of WBC localization, cortical bone erosion, and multiple separate foci located beneath the skin). More importantly, 99mTc-WBC SPECT/CT allows semiquantitive grading of WBC intensity, a characteristic not discernible by clinical examination. WBC scintigraphic intensity is not a representation of the infectious process per se but rather the physiologic response to it (28). Nonetheless, conventional WBC studies successfully use intensity above a threshold (and in contact with bone) to reflect osteomyelitis (6,29,30). Conversely, posttherapy decline in WBC intensity has been shown to correlate with DFI resolution (6,17,30). SPECT/CT allows more accurate assessment of focal increased WBC intensity (19,20), and this has been shown to predict poor outcome even if confined to soft tissue without bone contact (24).
99mTc-WBC SPECT/CT has several inherent advantages over dual isotope 111In-WBC/99mTc-MDP bone scanning, which positions it as a more competitive option for comparison with MRI, the current diagnostic imaging standard. Conventional nuclear medicine imaging techniques have been criticized for suboptimal delineation of infection due to spatial resolution constraints, particularly when involving the forefoot (31), and thus have historically been excluded from published guidelines as a first-line diagnostic method (1,4). However, the 1-mm SPECT/CT slice thickness we employed enabled fine visualization of cortical bone margins, even among the smallest digits, and surpassed available MRI cortical resolution (15,32,33).
A 99mTc-WBC SPECT/CT study incurs 24% less cost at our institution and delivers 28% less effective radiation dose equivalents than the dual-isotope technique. Moreover, our study protocol requires only 1 day versus the 2-day protocol common to dual-isotope methods (29). Our shortened protocol may offer additional cost advantages via a reduction in required inpatient days.
Our investigation has limitations, the most salient of which is its retrospective design. 99mTc-WBC SPECT/CT-generated CSI needs prospective validation at other institutions, with larger number of patients, especially including those with the most severe infections and highest CSI scores. Although 99mTc-WBC SPECT/CT appears to improve upon some of the spatial resolution limitations of nuclear imaging studies (19,20) and the specificity issues of MRI (34,35), a rigorous head-to-head comparison of hybrid imaging with the latter seems warranted.
Imaging tests for DFI have primarily been aimed at predicting the presence of osteomyelitis, and, in the case of MRI, defining deep soft tissue infections to guide management decisions (36). They have not attempted to quantify other important prognostic determinant factors such as perfusion, peripheral neuropathy, infection grade, and extent, which may be indirectly reflected in the image (37,38). Although hybrid imaging, as evaluated in this study, may extend the assessment of DFI beyond conventional parameters, it poses the future possibility of including additional derivative image characteristics of diabetic foot pathology such as neuro-osteoarthropathy, arterial calcification, and endothelial WBC uptake. Our study establishes a system for facilitating and standardizing interpretation of future evaluations of DFI with 99mTc-WBC SPECT/CT as well as with other new hybrid imaging modalities, such as positron emission tomography/CT and positron emission tomography/MRI (39).
99mTc-WBC SPECT/CT hybrid image–derived wound infection parameters incorporated into a standardized scoring system, CSI, have prognostic value in DFI.
Acknowledgments
Funding was provided by the Alpha Omega Alpha Carolyn L. Kuckein Student Research Fellowship.
No potential conflicts of interest relevant to this article were reported.
W.A.E. and J.B. researched data and wrote the manuscript. R.B. contributed to the data analysis. H.K.G., C.T., P.M., J.A., S.K., and O.K.O. researched data, edited the manuscript, and contributed to the discussion. W.A.E. and J.B. are the guarantors of this work and, as such, had full access to all the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
The authors thank Dr. Ildiko Lingvay, Dr. James Luby, and Dr. Neil Rofsky, all from University of Texas Southwestern Medical Center, for editorial assistance.
Footnotes
This article contains Supplementary Data online at http://care.diabetesjournals.org/lookup/suppl/doi:10.2337/dc11-2425/-/DC1.
References
- 1.Lipsky BA, Berendt AR, Deery HG, et al. Infectious Diseases Society of America Diagnosis and treatment of diabetic foot infections. Plast Reconstr Surg 2006;117(Suppl.):212S–238S [DOI] [PubMed] [Google Scholar]
- 2.Frykberg RG, Zgonis T, Armstrong DG, et al. American College of Foot and Ankle Surgeons Diabetic foot disorders. A clinical practice guideline (2006 revision). J Foot Ankle Surg 2006;45(Suppl.):S1–S66 [DOI] [PubMed] [Google Scholar]
- 3.Lipman BT, Collier BD, Carrera GF, et al. Detection of osteomyelitis in the neuropathic foot: nuclear medicine, MRI and conventional radiography. Clin Nucl Med 1998;23:77–82 [DOI] [PubMed] [Google Scholar]
- 4.Schweitzer ME, Daffner RH, Weissman BN, et al. ACR Appropriateness Criteria on suspected osteomyelitis in patients with diabetes mellitus. J Am Coll Radiol 2008;5:881–886 [DOI] [PubMed] [Google Scholar]
- 5.Jay PR, Michelson JD, Mizel MS, Magid D, Le T. Efficacy of three-phase bone scans in evaluating diabetic foot ulcers. Foot Ankle Int 1999;20:347–355 [DOI] [PubMed] [Google Scholar]
- 6.Devillers A, Moisan A, Hennion F, Garin E, Poirier JY, Bourguet P. Contribution of technetium-99m hexamethylpropylene amine oxime labelled leucocyte scintigraphy to the diagnosis of diabetic foot infection. Eur J Nucl Med 1998;25:132–138 [DOI] [PubMed] [Google Scholar]
- 7.Blume PA, Dey HM, Daley LJ, Arrighi JA, Soufer R, Gorecki GA. Diagnosis of pedal osteomyelitis with Tc-99m HMPAO labeled leukocytes. J Foot Ankle Surg 1997;36:120–126; discussion 160 [DOI] [PubMed] [Google Scholar]
- 8.Capriotti G, Chianelli M, Signore A. Nuclear medicine imaging of diabetic foot infection: results of meta-analysis. Nucl Med Commun 2006;27:757–764 [DOI] [PubMed] [Google Scholar]
- 9.Palestro CJ, Torres MA. Radionuclide imaging in orthopedic infections. Semin Nucl Med 1997;27:334–345 [DOI] [PubMed] [Google Scholar]
- 10.Schauwecker DS. The scintigraphic diagnosis of osteomyelitis. AJR Am J Roentgenol 1992;158:9–18 [DOI] [PubMed] [Google Scholar]
- 11.Termaat MF, Raijmakers PG, Scholten HJ, Bakker FC, Patka P, Haarman HJ. The accuracy of diagnostic imaging for the assessment of chronic osteomyelitis: a systematic review and meta-analysis. J Bone Joint Surg Am 2005;87:2464–2471 [DOI] [PubMed] [Google Scholar]
- 12.Erdman WA, Tamburro F, Jayson HT, Weatherall PT, Ferry KB, Peshock RM. Osteomyelitis: characteristics and pitfalls of diagnosis with MR imaging. Radiology 1991;180:533–539 [DOI] [PubMed] [Google Scholar]
- 13.Seabold JE, Flickinger FW, Kao SC, et al. Indium-111-leukocyte/technetium-99m-MDP bone and magnetic resonance imaging: difficulty of diagnosing osteomyelitis in patients with neuropathic osteoarthropathy. J Nucl Med 1990;31:549–556 [PubMed] [Google Scholar]
- 14.Craig JG, Amin MB, Wu K, et al. Osteomyelitis of the diabetic foot: MR imaging-pathologic correlation. Radiology 1997;203:849–855 [DOI] [PubMed] [Google Scholar]
- 15.Morrison WB, Schweitzer ME, Batte WG, Radack DP, Russel KM. Osteomyelitis of the foot: relative importance of primary and secondary MR imaging signs. Radiology 1998;207:625–632 [DOI] [PubMed] [Google Scholar]
- 16.Ahmadi ME, Morrison WB, Carrino JA, Schweitzer ME, Raikin SM, Ledermann HP. Neuropathic arthropathy of the foot with and without superimposed osteomyelitis: MR imaging characteristics. Radiology 2006;238:622–631 [DOI] [PubMed] [Google Scholar]
- 17.Heiba SI, Kolker D, Mocherla B, et al. The optimized evaluation of diabetic foot infection by dual isotope SPECT/CT imaging protocol. J Foot Ankle Surg 2010;49:529–536 [DOI] [PubMed] [Google Scholar]
- 18.Buck AK, Nekolla S, Ziegler S, et al. Spect/Ct. J Nucl Med 2008;49:1305–1319 [DOI] [PubMed] [Google Scholar]
- 19.Filippi L, Schillaci O. Usefulness of hybrid SPECT/CT in 99mTc-HMPAO-labeled leukocyte scintigraphy for bone and joint infections. J Nucl Med 2006;47:1908–1913 [PubMed] [Google Scholar]
- 20.Filippi L, Uccioli L, Giurato L, Schillaci O. Diabetic foot infection: usefulness of SPECT/CT for 99mTc-HMPAO-labeled leukocyte imaging. J Nucl Med 2009;50:1042–1046 [DOI] [PubMed] [Google Scholar]
- 21.Erdman W, Maewal P, Thompson C, Anderson J, Oz O. Staging diabetic foot infection using Tc- WBC and high resolution SPECT- CT imaging. J Nucl Med 2009;50(Suppl. 2):1342 [Google Scholar]
- 22.Horger M, Eschmann SM, Pfannenberg C, et al. The value of SPET/CT in chronic osteomyelitis. Eur J Nucl Med Mol Imaging 2003;30:1665–1673 [DOI] [PubMed] [Google Scholar]
- 23.Song J, Erdman W, Oz O, et al. Predicting response to therapy of diabetic foot infection utilizing high resolution 99mTc-WBC SPECT-CT fusion imaging. J Nucl Med 2010;51(Suppl. 2):371 [Google Scholar]
- 24.Song J, Erdman W, Bhore R, Ghayee H, Anderson J, Oz O. Diagnosing severity of diabetic foot ulcer is more complicated than just soft tissue infection vs osteomyelitis. Presented at the Radiological Society of North America 97th Scientific Assembly and Annual Meeting, Chicago, Illinois, 27 November–2 December 2011. [Google Scholar]
- 25.DeLong ER, DeLong DM, Clarke-Pearson DL. Comparing the areas under two or more correlated receiver operating characteristic curves: a nonparametric approach. Biometrics 1988;44:837–845 [PubMed] [Google Scholar]
- 26.Karthikesalingam A, Holt PJ, Moxey P, Jones KG, Thompson MM, Hinchliffe RJ. A systematic review of scoring systems for diabetic foot ulcers. Diab Med 2010;27:544–549 [DOI] [PubMed] [Google Scholar]
- 27.Lipsky BA, Polis AB, Lantz KC, Norquist JM, Abramson MA. The value of a wound score for diabetic foot infections in predicting treatment outcome: a prospective analysis from the SIDESTEP trial. Wound Repair Regen 2009;17:671–677 [DOI] [PubMed] [Google Scholar]
- 28.Goldsmith SJ, Vallabhajosula S. Clinically proven radiopharmaceuticals for infection imaging: mechanisms and applications. Semin Nucl Med 2009;39:2–10 [DOI] [PubMed] [Google Scholar]
- 29.Palestro CJ, Love C, Tronco GG, Tomas MB, Rini JN. Combined labeled leukocyte and technetium 99m sulfur colloid bone marrow imaging for diagnosing musculoskeletal infection. Radiographics 2006;26:859–870 [DOI] [PubMed] [Google Scholar]
- 30.Newman LG, Waller J, Palestro CJ, et al. Unsuspected osteomyelitis in diabetic foot ulcers. Diagnosis and monitoring by leukocyte scanning with indium in 111 oxyquinoline. JAMA 1991;266:1246–1251 [DOI] [PubMed] [Google Scholar]
- 31.Palestro CJ, Love C. Nuclear medicine and diabetic foot infections. Semin Nucl Med 2009;39:52–65 [DOI] [PubMed] [Google Scholar]
- 32.Ertugrul MB, Baktiroglu S, Salman S, Unal S, Aksoy M, Berberoglu K, Calangu S. The diagnosis of osteomyelitis of the foot in diabetes: microbiological examination vs. magnetic resonance imaging and labelled leucocyte scanning. Diab Med 2006;23:649–653 [DOI] [PubMed] [Google Scholar]
- 33.Morrison WB, Schweitzer ME, Wapner KL, Hecht PJ, Gannon FH, Behm WR. Osteomyelitis in feet of diabetics: clinical accuracy, surgical utility, and cost-effectiveness of MR imaging. Radiology 1995;196:557–564 [DOI] [PubMed] [Google Scholar]
- 34.Maewal P, Song J, Erdman W, et al. Effectiveness of technetium labeled leukocytes SPECT CT imaging in patients with nonspecific or clinically incongruent MRI scans. J Nucl Med 2010;51(Suppl. 2):1631 [Google Scholar]
- 35.Agarwal ABJ, Omar HA, Anderson JA, Oz OK, Erdman WA. Utility of 99m-Tc WBC SPECT/CT in predicting outcome of diabetic lower extremity infections with clinically incongruent or inconclusive MRI. Presented at the Radiological Society of North America 97th Scientific Assembly and Annual Meeting, Chicago, Illinois, 27 November–2 December 2011. [Google Scholar]
- 36.Lipsky BA, Peters EJ, Senneville E, et al. Expert opinion on the management of infections in the diabetic foot. Diabetes Metab Res Rev 2012;28(Suppl. 1):163–178 [DOI] [PubMed] [Google Scholar]
- 37.Lavery LA, Armstrong DG, Murdoch DP, Peters EJ, Lipsky BA. Validation of the Infectious Diseases Society of America’s diabetic foot infection classification system. Clin Infect Dis 2007;44:562–565 [DOI] [PubMed] [Google Scholar]
- 38.Schaper NC. Diabetic foot ulcer classification system for research purposes: a progress report on criteria for including patients in research studies. Diabetes Metab Res Rev 2004;20(Suppl. 1):S90–S95 [DOI] [PubMed] [Google Scholar]
- 39.Keidar Z, Militianu D, Melamed E, Bar-Shalom R, Israel O. The diabetic foot: initial experience with 18F-FDG PET/CT. J Nucl Med 2005;46:444–449 [PubMed] [Google Scholar]