In this issue of Diabetes Care, McCoy et al. (1) report 3.4-fold higher mortality in patients with diabetes who self-reported severe hypoglycemia (that which required the assistance of another person) 5 years earlier. They suggest that patient-related outcomes such as hypoglycemia would augment risk stratification and management of patients with diabetes.
Iatrogenic hypoglycemia is the limiting factor in the glycemic management of diabetes (2). It causes recurrent morbidity in most people with type 1 diabetes and many with advanced type 2 diabetes and is sometimes fatal. It impairs defenses against subsequent hypoglycemia and, thus, causes a vicious cycle of recurrent hypoglycemia. The barrier of hypoglycemia generally precludes maintenance of euglycemia over a lifetime of diabetes and, therefore, full realization of the benefits of glycemic control.
Although it can be caused by an episode of marked absolute therapeutic hyperinsulinemia, iatrogenic hypoglycemia is typically the result of the interplay of mild-to-moderate absolute or even relative therapeutic hyperinsulinemia and compromised physiological and behavioral defenses against falling plasma glucose concentrations (2). The compromised physiological defenses include attenuated adrenomedullary epinephrine responses that, in the setting of absent insulin and glucagon responses, cause the clinical syndrome of defective glucose counterregulation with its 25-fold or greater increased risk of severe hypoglycemia during aggressive glycemic therapy. The compromised behavioral defense is the failure to ingest carbohydrates, which results from attenuated sympathoadrenal (largely sympathetic neural) responses that cause the clinical syndrome of hypoglycemia unawareness with its sixfold or greater increased risk of severe hypoglycemia during aggressive glycemic therapy. Defective glucose counterregulation and hypoglycemia unawareness are the components of hypoglycemia-associated autonomic failure (HAAF) in diabetes. HAAF is a form of functional sympathoadrenal failure, which is most often caused by recent antecedent iatrogenic hypoglycemia and is generally largely reversible by scrupulous avoidance of hypoglycemia.
There is no doubt that hypoglycemia can be fatal (3). The Toronto insulin extract sometimes killed diabetic dogs and marked hypoglycemia kills experimental animals. In addition, there are many documented examples of associations between iatrogenic hypoglycemia and death (3). For example, increased hypoglycemia associated with excessive mortality during intensive glycemic therapy has been reported from randomized controlled trials in patients with type 2 diabetes (4) and in hyperglycemic critically ill individuals (5). It appears that something about an intensive therapy regimen designed to lower plasma glucose concentrations increased the possibility of death in those trials. Excess mortality during intensive glycemic therapy could have been the result of chance, a nonglycemic effect of some aspect of the intensive treatment regimen (e.g., a side effect of one or more of the drugs used, weight gain, or something else), or iatrogenic hypoglycemia (6,7). Denial notwithstanding (8), since plasma glucose concentrations at the times of each of the deaths are not known, one cannot know if hypoglycemia was or was not a culprit in some of the deaths. Additional associations between hypoglycemia and death in diabetes (3) include 1) reports of increased mortality associated with low, as well as high, hemoglobin A1c levels in type 2 diabetes; 2) those of hypoglycemia, cardiac arrhythmias, and death in diabetes; and 3) the finding of a temporal relationship between vanishingly low subcutaneous glucose concentrations and death in a patient with type 1 diabetes found dead in bed.
Finally, in addition to case reports of hypoglycemic deaths in diabetes, there are an increasing number of series reporting hypoglycemic mortality rates (3). For example, recent reports indicate that 4% (9), 6% (10), 7% (11), and 10% (12) of deaths of patients with type 1 diabetes were caused by hypoglycemia. It is sobering to think that as many as 1 in 25—or even 1 in 10—patients with type 1 diabetes will die of iatrogenic hypoglycemia. Obviously, life-threatening episodes of hypoglycemia need not be frequent to be devastating.
Associations between hypoglycemia and mortality (1,4,5,13,14) do not, of course, establish a causal connection. Indeed, Zoungas et al. (15) noted that severe hypoglycemia was associated not only with all-cause and cardiovascular mortality but also with noncardiovascular mortality in type 2 diabetes. That prompted them to suggest that hypoglycemia might be a marker of serious underlying disease rather than a cause of death. Notably, the current data of McCoy et al. (1) do not support that interpretation. They found that the Charlson comorbidity index, an extensively studied index for predicting mortality that has been judged valid and reliable (16), was no different at baseline or at 5 years between the patients with diabetes who reported severe hypoglycemia and those who reported no or mild hypoglycemia. Thus, there was no evidence that the former group had more serious underlying disease, although their self-report of severe hypoglycemia predicted higher mortality 5 years later even after adjustment for age, sex, diabetes type and duration, hemoglobin A1c, and Charlson comorbidity index.
While profound, prolonged hypoglycemia can cause brain death, most episodes of fatal hypoglycemia are the result of other mechanisms, presumably cardiac arrhythmias (3,17). As noted earlier, HAAF in diabetes is commonly caused by recent antecedent iatrogenic hypoglycemia, which reduces sympathoadrenal and symptomatic responses to subsequent hypoglycemia (3,18). It is now known that recent antecedent hypoglycemia also reduces subsequent baroreceptor sensitivity (19). The latter increases the risk of a fatal ventricular arrhythmia. Thus, the mechanism of hypoglycemic death may involve an episode of recent antecedent iatrogenic hypoglycemia that 1) reduces baroreflex sensitivity, thereby setting the stage for a ventricular arrhythmia and 2) increases the likelihood of another episode of hypoglycemia with a sympathoadrenal discharge that triggers a ventricular arrhythmia (3). Recent experimental data support the role of a sympathoadrenal discharge in that combined α- and β-adrenergic blockade reduced the deaths of rats during marked hypoglycemia (20).
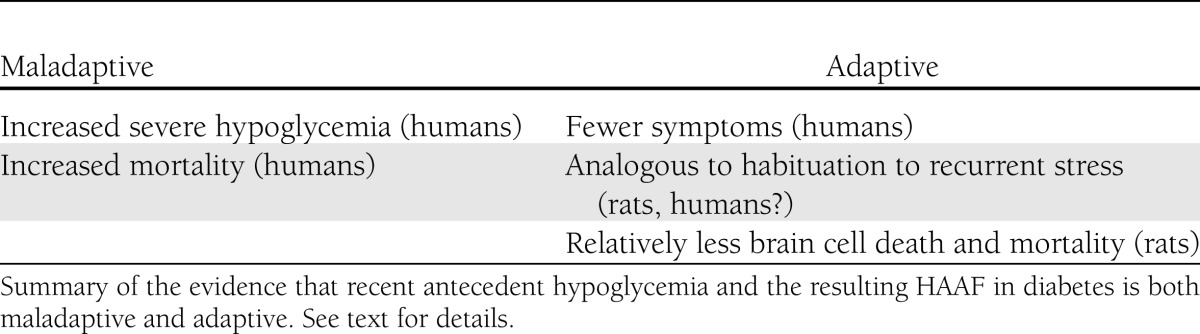
Is iatrogenic hypoglycemia and the resulting HAAF maladaptive or adaptive? HAAF is maladaptive in that both defective glucose counterregulation and hypoglycemia unawareness substantially increase the risk of severe clinical hypoglycemia with its morbidity and potential mortality (2,3). On the other hand, HAAF could be viewed as adaptive. First, it allows individuals to be less troubled by symptoms during hypoglycemia. Second, it may be analogous to the phenomenon of habituation of the hypothalamic-pituitary-adrenocortical response to recurrent restraint stress in rats (21), which could also apply to habituation of the sympathoadrenal response to recurrent hypoglycemic stress in humans (22). Third, Puente et al. (23) found that rats subjected to recurrent moderate hypoglycemia had less brain cell death following marked hypoglycemia than those not subjected to recurrent hypoglycemia. Fourth, Reno et al. (24) found that rats subjected to recurrent moderate hypoglycemia had less mortality during marked hypoglycemia. Thus, it appears that iatrogenic hypoglycemia and the resulting HAAF is both maladaptive and adaptive (Table 1). It may make people with diabetes more prone to hypoglycemia but less vulnerable to its devastating effects.
Table 1.
Antecedent hypoglycemia and HAAF
The attenuated sympathoadrenal responses that characterize HAAF would be expected to result in fewer symptoms at a given low plasma glucose concentration and thus, fewer episodes of recognized symptomatic hypoglycemia. That might explain an inverse relationship between the frequency of self-monitored low plasma glucose values and mortality (25). Furthermore, given a relationship between the sympathoadrenal discharge and development of a ventricular arrhythmia during hypoglycemia (3), attenuated sympathoadrenal responses would be expected to reduce the likelihood of a fatal arrhythmia. Nonetheless, a particularly low plasma glucose concentration might trigger a robust, potentially fatal, sympathoadrenal discharge. Again, life-threatening episodes of hypoglycemia need not be frequent to be devastating.
Acknowledgments
The author’s original research cited was supported by National Institutes of Health grants R37-DK2085, MO1-RR00036 (now UL1-RR249892), P60-DK20579, and T32-DK07120, and a fellowship award from the American Diabetes Association.
P.E.C. has served as a consultant to Bristol-Myers Squibb/AstraZeneca and Novo Nordisk in the past year. He does not receive research funds from, hold stock in, or speak for any pharmaceutical or device firm. No other potential conflicts of interest relevant to this article were reported.
Janet Dedeke, the author’s assistant, prepared the manuscript.
References
- 1.McCoy RG, Van Houten HK, Ziegenfuss JY, Shah ND, Wermers RA, Smith SA. Increased mortality of patients with diabetes reporting severe hypoglycemia. Diabetes Care 2012;35:1897–1900 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Cryer PE. Hypoglycemia in Diabetes. Pathophysiology, Prevalence and Prevention. Alexandria, VA, American Diabetes Association, 2009 [Google Scholar]
- 3.Cryer PE. Death during intensive glycemic therapy of diabetes: mechanisms and implications. Am J Med 2011;124:993–996 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gerstein HC, Miller ME, Byington RP, et al. Action to Control Cardiovascular Risk in Diabetes Study Group Effects of intensive glucose lowering in type 2 diabetes. N Engl J Med 2008;358:2545–2559 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Finfer S, Chittock DR, Su SY, et al. NICE-SUGAR Study Investigators Intensive versus conventional glucose control in critically ill patients. N Engl J Med 2009;360:1283–1297 [DOI] [PubMed] [Google Scholar]
- 6.Lachin JM. Point: Intensive glycemic control and mortality in ACCORD—a chance finding? Diabetes Care 2010;33:2719–2721 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Riddle MC, Ambrosius WT, Brillon DJ, et al. Action to Control Cardiovascular Risk in Diabetes Investigators Epidemiologic relationships between A1C and all-cause mortality during a median 3.4-year follow-up of glycemic treatment in the ACCORD trial. Diabetes Care 2010;33:983–990 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gerstein HC, Miller ME, Genuth S, et al. ACCORD Study Group Long-term effects of intensive glucose lowering on cardiovascular outcomes. N Engl J Med 2011;364:818–828 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Patterson CC, Dahlquist G, Harjutsalo V, et al. Early mortality in EURODIAB population-based cohorts of type 1 diabetes diagnosed in childhood since 1989. Diabetologia 2007;50:2439–2442 [DOI] [PubMed] [Google Scholar]
- 10.Jacobson AM, Musen G, Ryan CM, et al. Diabetes Control and Complications Trial/Epidemiology of Diabetes Interventions and Complications Study Research Group Long-term effect of diabetes and its treatment on cognitive function. N Engl J Med 2007;356:1842–1852 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Feltbower RG, Bodansky HJ, Patterson CC, et al. Acute complications and drug misuse are important causes of death for children and young adults with type 1 diabetes: results from the Yorkshire Register of Diabetes in Children and Young Adults. Diabetes Care 2008;31:922–926 [DOI] [PubMed] [Google Scholar]
- 12.Skrivarhaug T, Bangstad H-J, Stene LC, Sandvik L, Hanssen KF, Joner G. Long-term mortality in a nationwide cohort of childhood-onset type 1 diabetic patients in Norway. Diabetologia 2006;49:298–305 [DOI] [PubMed] [Google Scholar]
- 13.Patel A, MacMahon S, Chalmers J, et al. ADVANCE Collaborative Group Intensive blood glucose control and vascular outcomes in patients with type 2 diabetes. N Engl J Med 2008;358:2560–2572 [DOI] [PubMed] [Google Scholar]
- 14.Duckworth W, Abraira C, Moritz T, et al. VADT Investigators Glucose control and vascular complications in veterans with type 2 diabetes. N Engl J Med 2009;360:129–139 [DOI] [PubMed] [Google Scholar]
- 15.Zoungas S, Patel A, Chalmers J, et al. ADVANCE Collaborative Group Severe hypoglycemia and risks of vascular events and death. N Engl J Med 2010;363:1410–1418 [DOI] [PubMed] [Google Scholar]
- 16.de Groot V, Beckerman H, Lankhorst GJ, Bouter LM. How to measure comorbidity. a critical review of available methods. J Clin Epidemiol 2003;56:221–229 [DOI] [PubMed] [Google Scholar]
- 17.Frier BM, Schernthaner G, Heller SR. Hypoglycemia and cardiovascular risks. Diabetes Care 2011;34Suppl. 2S132–S137 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Heller SR, Cryer PE. Reduced neuroendocrine and symptomatic responses to subsequent hypoglycemia after 1 episode of hypoglycemia in nondiabetic humans. Diabetes 1991;40:223–226 [DOI] [PubMed] [Google Scholar]
- 19.Adler GK, Bonyhay I, Failing H, Waring E, Dotson S, Freeman R. Antecedent hypoglycemia impairs autonomic cardiovascular function: implications for rigorous glycemic control. Diabetes 2009;58:360–366 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Reno C, Daphna-Iken D, Fisher S. Adrenergic blockade prevents life threatening cardiac arrhythmias and sudden death due to severe hypoglycemia [abstract] Diabetes 2012;61(Suppl. 1):A46 [Google Scholar]
- 21.Jaferi A, Nowak N, Bhatnagar S. Negative feedback functions in chronically stressed rats: role of the posterior paraventricular thalamus. Physiol Behav 2003;78:365–373 [DOI] [PubMed] [Google Scholar]
- 22.Arbeláez AM, Powers WJ, Videen TO, Price JL, Cryer PE. Attenuation of counterregulatory responses to recurrent hypoglycemia by active thalamic inhibition: a mechanism for hypoglycemia-associated autonomic failure. Diabetes 2008;57:470–475 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Puente EC, Silverstein J, Bree AJ, et al. Recurrent moderate hypoglycemia ameliorates brain damage and cognitive dysfunction induced by severe hypoglycemia. Diabetes 2010;59:1055–1062 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Reno CM, Tanoli T, Puente EC, et al. Deaths due to severe hypoglycemia are exacerbated by diabetes and ameliorated by hypoglycemic pre-conditioning [abstract] Diabetes 2011;60Suppl. 1A81 [Google Scholar]
- 25.Seaquist ER, Miller ME, Bonds DE, et al. ACCORD Investigators The impact of frequent and unrecognized hypoglycemia on mortality in the ACCORD study. Diabetes Care 2012;35:409–414 [DOI] [PMC free article] [PubMed] [Google Scholar]