Abstract
BACKGROUND:
Adequate sleep has been considered important for the adolescent's health and well being. On the other hand, self-imposed sleep curtailment is now recognized as a potentially important and novel risk factor for obesity. The present study aimed to assess the prevalence of short sleep duration and its association with obesity among Saudi adolescents.
METHODS:
This is a school-based cross-sectional study with self-reported sleep questionnaires. It was conducted during the years 2009/2010 in three cities in Saudi Arabia; Al-Khobar, Jeddah, and Riyadh. Participants were 2868 secondary-school males (1379) and females (1389) aged 15 to 19 years, randomly selected using a multistage stratified sampling technique. Measurements included weight, height, waist circumference, BMI, and sleeping duration. Logistic regression analysis while adjusted for age, gender, and location was used to examine the associations between sleep duration and obesity measures.
RESULTS:
The mean (SD) of sleep duration was 7.2 (1.6) hours/day with no significant differences between males and females. About 31% of the participants obtain less than 7 hours of sleep per day, while approximately 50% of the sample gets less than 8 hours of daily sleep. Two-way ANCOVA results while controlling for the effect of age revealed a significant gender by school-type interaction (P<0.001). In addition, adequate sleep duration increased the odds of having normal weight (adjusted odds ratios = 1.28, 95% CI = 1.08-1.50, P = 0.003).
CONCLUSION:
The present study observed a high prevalence of short sleep duration among Saudi adolescents 15- to 19-year olds and that short sleep duration was significantly associated with increased risk of overweight and obesity. Future interventions should investigate whether adopting a healthy lifestyle by adolescents with short sleep duration would improve their sleeping habits or not.
Keywords: Adolescents, obesity, Saudi Arabia, sleep duration, waist circumference
Adequate sleep has been considered important for the adolescent's biological and psychological health.[1,2] Adolescents obtaining adequate sleep were shown to have higher frequency of health-promoting behaviors.[1] On the other hand, sleep restriction can have adverse effects on endocrine function, cognitive performance, and metabolic as well as inflammatory responses.[3] Despite the increasing evidence that adequate sleep is important for overall health, sleep reduction is prevalent among adolescents. Cross-sectional[4,5] as well as longitudinal[6] researches conducted in Western countries indicate that sleep duration among children and adolescents has been declining over the recent decades.
In addition to conventional risk factors such as physical inactivity and unhealthy dietary habits, self-imposed sleep curtailment is now recognized as a potentially important and novel risk factor for obesity. Indeed, several recent studies including systematic reviews have indicated that short sleep duration has evolved as a significant determinant of overweight and obesity.[7–14] Moreover, there is even evidence for the long-term impact of childhood sleeping problems on later development of obesity.[15]
In Saudi Arabia, obesity among children and adolescent has reached epidemic proportion in recent years.[16,17] Childhood obesity is well recognized to associate with comorbidities.[18,19] Current evidence indicates that obesity is a multi-factorial condition influenced by many variables including genetic, demographic, and lifestyle factors.[18,20] Despite the widely spread problem of obesity among Saudi children and adolescents, there is a dearth of published research on the epidemiology of sleep pattern and its association with obesity among Saudi young people.[21–23] This fact was reflected in a recent review on sleep medicine in Saudi Arabia emphasizing the need for more sleep research in the country, especially to address the prevalence of different sleep disorders among various segments of the population.[24] Among Saudi adolescents in particular, there is only one published study from Riyadh that investigated sleep duration and obesity and found an inverse association between obesity and short sleep duration.[23] Therefore, the present study aimed to build upon previous literature and assess the prevalence of short sleep duration among adolescents 15- to 19-year olds who were drawn from three major cities in Saudi Arabia. It was also the intent of this study to examine the associations of sleep duration with measures of overweight and obesity.
Methods
Study design
The present study is part of the Arab Teens Lifestyle Study (ATLS). The ATLS is a school-based cross-sectional multi-center collaborative project that was conducted during the years 2009/2010.[25] Detailed description of ATLS design, methodology, standardization, data collection, and implementations were published elsewhere.[26] The study protocol was approved by the Research Center at King Saud University as well as by the General Directorate of School Education in each of the respective city. In addition, schools’ consent as well as students’ approval for conducting the survey were all secured.
Study sample
The sample came from adolescent males and females enrolled in the secondary schools at three major cities in Saudi Arabia; Riyadh, Jeddah, and Al-Khobar. The minimum needed sample size in each city was determined so that the sample proportion would be within ± 0.05 of the population proportion with a 95% confidence level. Depending on the participating center, there were 10% to 15% of additional students who were included to account for missing data.
A multistage stratified random sampling technique was used to select the sample. At the first stage, a systematic random sampling procedure was used to select the schools. The schools were stratified into boys’ and girls’ secondary schools, with further stratification into public and private schools. The selection of the private/public schools was proportional to population size. Four schools (two from each of the boys’ and girls’ schools) were selected from each of the four geographical areas (east, north, south, and west). At the second stage, classes were selected at each grade (level) using simple random sampling design. In this way, one class was randomly selected in each grade of the three grades (grades 10, 11, and 12) in each secondary school. Thus, we have a total selection of at least 24 classes in each city (12 from each of the boys’ and girls’ schools). All students in the selected classes, who were free from any physical deformity, were invited to participate in the study. The total sample size included in the analysis of the present study consisted of 2868 adolescents, comprising 1379 males and 1389 females.
Anthropometric measurements
Anthropometric variables included body weight, height, and waist circumference (WC). Measurements were performed in the morning by trained researcher according to written standardized procedures. Body weight was measured to the nearest 100 g and with minimal clothing and without shoes using calibrated portable scale. Height was measured to the nearest 1 cm while subject is in full standing position without shoes using calibrated portable measuring rod. Body mass index (BMI) was calculated as a ratio of weight in kg by height squared in meter. The International Obesity Task Force (IOTF) age- and sex-specific BMI cut-off reference standards were used to identify overweight and obesity in adolescents between the age of 14 and 17 years.[27] For participants who were 18 years and above, we used WHO adults’ cut-off points of 25-29.9 kg/ m2 for overweight and 30 kg/m2 and higher for obesity. WC was measured horizontally to the nearest 0.1 cm using a non-stretchable measuring tape at the level of umbilical and at the end of gentle expiration. When measuring WC, the tape was snug but did not compress the skin. For cultural reason, WC was measured in girls with light shirt on, and this was later adjusted (corrected) using a correction factor of -1 cm, based on the results of a small pilot study that we have previously conducted. Waist height ratio (WHtR) was calculated as the ratio of WC in cm and height in cm. A WHtR cut-off point of 0.50 was used to define abdominal obesity in males and females.[28,29]
ATLS research instrument
The ATLS research instrument used for the data collection from the adolescents consists of 47-item questionnaires. It includes detailed questions related to physical activity, sedentary behaviors, and dietary habits. In addition, the participants were asked about the number of typical sleeping hours per day (night and day) using self-reported questionnaire. No differentiating between weekdays and weekends in sleeping hours was ascertained. In the current paper, only sleep data as it relates to obesity are analyzed and presented. We defined insufficient sleep (short sleep) as sleeping less than 7 hours per night, according to the definition of the National Sleep Foundation for adolescent population.[30] To ensure accurate and consistent measurements throughout this multi-center project, a standardized measurement protocol was employed in all participating data collection centers.
Data and statistical analysis
Data at each center were checked and entered into a computer using standardized entry codes written on an SPSS data file. The entered data were then sent to one central processing place (Riyadh). At the central processing center, all data were checked again for outliers and wrong entries. Data were then analyzed using SPSS, version 15 (SPSS, Inc, Chicago, IL). Descriptive statistics are presented as means, standard deviations, and proportions. The 10th, 50th, and 90th percentiles of sleep duration were also calculated. The relationship of sleep duration with BMI, WC, and WHtR were examined using both Pearson correlation and partial correlation while controlling for age. Differences in anthropometric measurements between those who have inadequate (<7 hours per day) and adequate (≥7 hours per day) sleep duration in males and females were tested using two-way ANCOVA, while controlling for the effect of age. We also separately used two-way ANOVA to test the interactions of sleep duration with each of age and school type (public versus private). In addition, Chi-Square test was used to examine the differences in the proportions of BMI cut-offs (obese and non-obese) and WHtR categories (above and below 50% of WHtR) relative to sleep duration categories. Finally, we used logistic regression analysis to examine the independent associations between obesity levels and school types with the dependent measures of sleep duration while adjusting our analysis for age, gender, and location (as covariates). The adjusted odds ratios and the corresponding 95% confidence intervals (CIs) were calculated for each independent variable.
Results
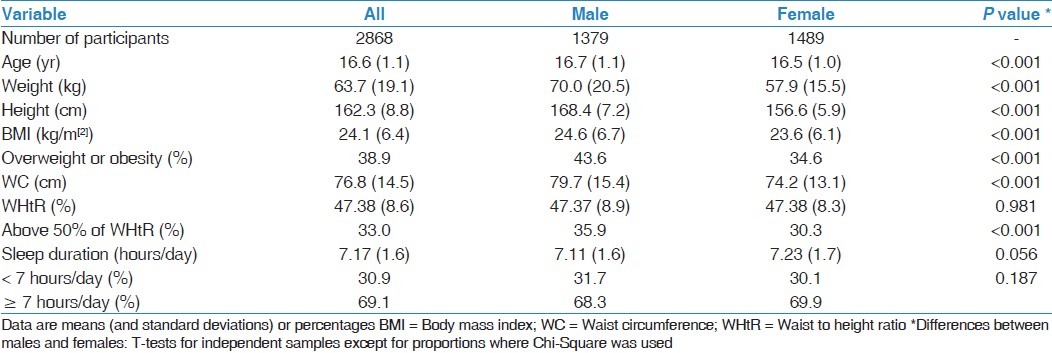
The descriptive characteristics of the participants are shown in Table 1. The percentage of females in the sample slightly exceeds that of male participants (51.9% vs 48.1%). Males are significantly heavier, taller, and have higher values for BMI and WC. The prevalence of overweight or obesity is also higher in males than in females. In addition, the mean sleep duration is 7.17 hours per day with no significant differences between males and females. About 31% of the participants obtain less than 7 hours of sleep per day with no significant differences relative to sex, while approximately 50% of the sample gets less than 8 hours of daily sleep. The 10th, 50th, and 90th percentiles of sleep duration were 5, 7, and 9 hours per day, respectively.
Table 1.
Descriptive characteristics of the participants
Mean sleep duration (hours/day) for the males and females relative to age is shown in Figure 1. Two-way ANOVA results indicate a significant main effect for age (P = 0.002) but not for gender (P = 0.897) or for age and gender interaction (P = 0.386). Figure 2 illustrates the mean sleep duration in hours per day for males and females relative to school type. Two-way ANCOVA results, while controlling for the effect of age, reveals a significant gender by school-type interaction effect (P<0.001). Mean sleep duration among males was longer than that of females in private schools, whereas in public schools, females have longer mean sleep duration than males. Mean sleep duration for the participants according to BMI cut-off values are shown in Figure 3. It appears that as participants move from normal weight category to overweight/obesity categories, the sleep duration is consistently reduced. However, one-way ANOVA test shows that only participants in the obese group are significantly (P = 0.002) different from those in normal weight group. Correlation coefficients of sleep duration with BMI, WC, and WHtR were -0.069 (P<0.001), -0.060 (P = 0.001), and -0.051 (P = 0.006), respectively. The corresponding values after controlling for the effect of age were still significant at P value of less than 0.01.
Figure 1.

Sleep duration (hours/day) relative to age. Two-way ANOVA results: P values for age = 0.002, gender = 0.897, and age by gender interaction = 0.386
Figure 2.
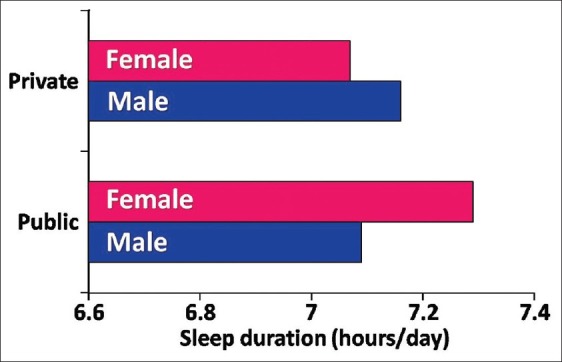
Sleep duration (hours/day) among male and female adolescents relative to school type (public vs private). Two-way ANCOVA results controlling for the effect of age: P values for age <0.001 and gender by school type interaction = 0.047
Figure 3.
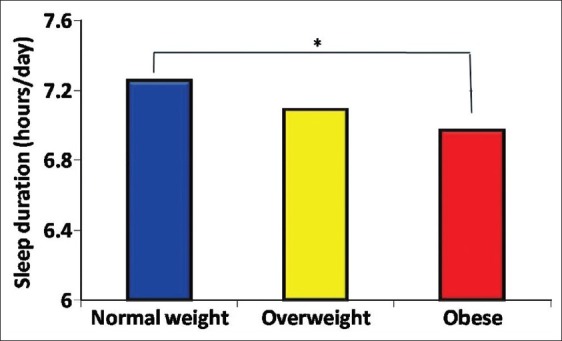
Sleep duration (hours/day) relative to BMI cut-off categories (*significant difference between normal weight and obese adolescents at Pvalues = 0.002)
Table 2 presents the anthropometric measurements relative to sleeping duration levels (<7 hours/day vs ≥7 hours/day). Two-way ANCOVA tests, while controlling for the effect of age, reveals that there were significant (P<0.05) gender by sleep duration interactions at height, BMI, and sleeping duration. The main effect of sleep duration was significant (P<0.05) at age, body weight, and BMI. Indicators of overall obesity (based on BMI cut-offs) and abdominal obesity (based on WHtR cut-offs) relative to sleep duration cut-off values (<7 hours/day vs ≥7 hours/day) are shown in Figures 4 and 5, respectively. Chi-Square results showed significant results, indicating that overall obesity and abdominal obesity are inversely related to sleep duration.
Table 2.
Anthropometric measurements among Saudi adolescents stratified by gender and sleep duration category
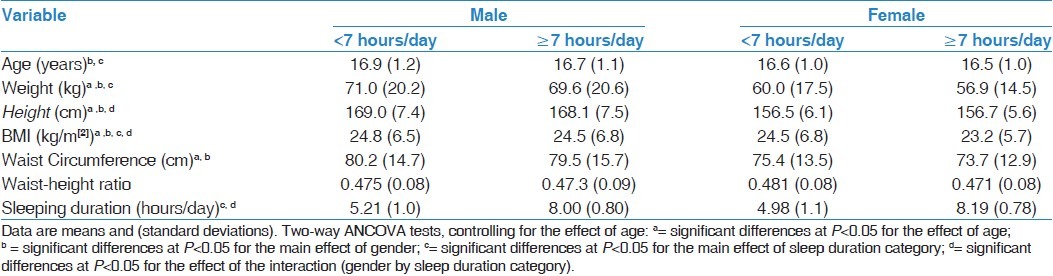
Figure 4.
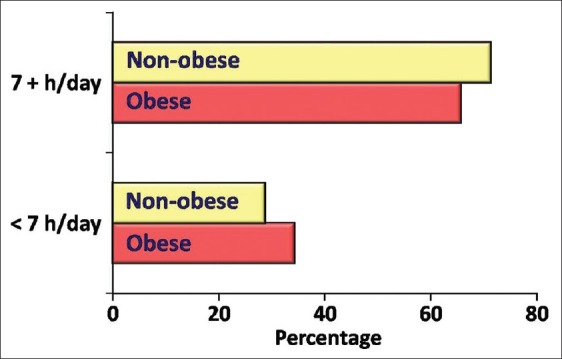
The proportions of obese and non-obese adolescents relative to sleep duration cut-offs (<7 hours per day vs ≥7 hours per day). Test of Chi-Square was significant at P<0.001
Figure 5.
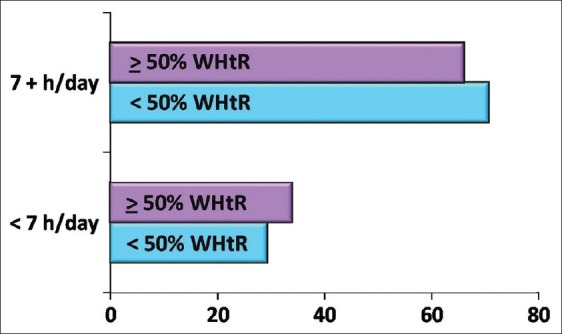
The proportions of adolescents above and below 50% of waist to height ratio (WHtR) relative to sleep duration cut-offs (<7 hours per day vs ≥7 hours per day). Test of Chi-Square was significant at P= 0.007
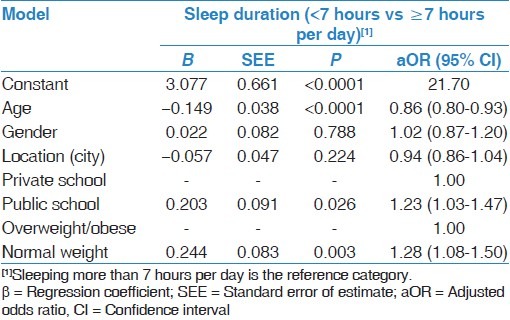
Table 3 shows the results of logistic regression analysis, adjusted for age, gender, and location (city) for the independent variables overweight and obesity as well as school type. Regression coefficients for age, school type, and overweight or obesity were all significant. The results indicate that the odds of having adequate sleep is increased by a factor of 1.23 (95% CI: 1.03-1.47, P = 0.026) if the participant is in public school compared with that in private school. Also, the odds of having normal weight (as opposed to overweight or obese) is increased by a factor of 1.28 (95% CI: 1.08-1.50, P = 0.003) if the participant gets adequate sleep (≥7 hours per day).
Table 3.
Logistic regression analyses, adjusted for age, gender, and location for overweight and obesity and school type in Saudi adolescents relative to sleep duration category (less than 7 hours vs 7 hours or more per day)
Discussion
A healthy lifestyle includes among other things a good sleeping pattern. Human beings spend almost one third of their lifetimes sleeping and adequate sleep is essential to human health and well being.[1,2] The main findings of this study indicate that depending on the cut-off values used, about 31% to 50% of Saudi adolescents do not obtain enough daily sleep, and that sleep duration decreases with increasing age from 15 to 19 years of age. In addition, adolescents in private school or/and overweight or obese are more likely to have inadequate daily sleep. In addition, short sleep duration was associated with higher risk of overweight and obesity.
The average sleep duration (7.2 hours/day) found among Saudi adolescents in the current study appears lower than that reported by Australian adolescents (ranging from 9.10 to 8.40 hours/day for 15.5- to 17.5-year olds),[4] Spanish adolescents (8.35 hours/day),[31] adolescents from 10 European cities (8 hours/day),[9] German adolescents 16 years and older (7.8 hours/day),[32] Swiss adolescents (8.3 and 7.9 hours/day for 15- and 16-year-old adolescents, respectively),[6] or Indian adolescents (7.8 hours/day).[33] However, sleep duration obtained in the present study was not much far from that reported for adolescents of similar age from South Africa (7.55 hours/weekday)[34] or some Asian countries such as China (7.5 hours/weekday)[35] and Taiwan (7.35 hours/weekday).[36] Our findings on adolescents corroborate findings from a previous study conducted on Saudi children 6-to 13-year olds that reported shorter sleep duration compared with that found for children from Western countries.[22]
The findings of the present study showed that about one third of the Saudi adolescents did not obtain 7 hours of daily sleep, while about 50% of the participants had less than 8 hours of daily sleep. In comparison with our findings, Mcknight-Eily et al. have reported insufficient sleep (<8 hours/day) on average school day by 68.9% of United States high school students.[37] In Japan, the proportions of adolescent boys and girls who reported less than 6 hours of daily sleep were 28.7% and 32.6%, respectively.[38] Among Taiwanese adolescents, 54% have reported that they slept less than the suggested 6 to 8 hours per day.[1]
The reduced sleep duration observed among Saudi adolescents in the current study may be attributed to several factors. Adolescence is a critical period in which a growing sense of autonomy and increased socialization may dominate adolescent life. Our modern society lifestyles with round-the-clock satellite television programming and high-speed internet availability, along with the increased demands for more study and school home works, may distract adolescents from retiring early to bed. Adding to that the fact that Saudi school system starts the school day in the early morning (around 7:00 am). All of that would place the adolescents at greater risk for sleep curtailment. Previous research has indicated that early starting of school negatively affect total sleep time among school children.[39]
In the present study, sleep duration declined with advancing age from 15 to 19 years. Such findings agree with results of previous studies from different countries.[4,6,11,14,33] Findings from the National Sleep Foundation in the United States showed that mean sleep duration among adolescents has steadily decreased from 8.4 hours at ages 11-12 years to only 6.9 hours at ages 17- 18 years.[40] Among Saudi elementary school children, total sleep duration was also reported to decline from age 6 to 13 years.[22] The decline in sleep duration with advancing age may in part reflect the role of pubertal development. Previous research has shown an inverse association between sleep duration and pubertal development among US adolescents.[41] In addition, parental influence on bedtimes appears to decrease with increasing age and it was reported to be nearly absent at the age of 17 years.[42]
In the current study, we did not observe any significant (P = 0.056) difference in sleep duration (hours/day) between males (7.11) and females (7.23). Such finding is similar to those reported by previous research for adolescents from Australia,[4] Switzerland,[6] and Germany.[11] However, the finding that females in the public school but not in the private school obtained longer sleep duration while the opposite was true for males is worth noting. Nevertheless, this finding cannot be fully explained, especially in the light of the absence of socioeconomic data, which were not collected in the present study. Such findings may warrant further research.
Critical reviews of the epidemiological evidence of the relationship between sleep duration and obesity indicate that short sleep duration appears independently associated with weight gain, particularly in younger age groups, as findings from studies in children and adolescents were more consistent than those among adults.[8,12,43,44] The findings of the present study on adolescents 15- to19-year olds confirmed such an inverse association between sleep duration and obesity. Previous local study involving school children aged 10 to 19 years from Riyadh has also shown that sleeping 7 hours or less significantly increases the risk of obesity in both boys and girls (odds ratio = 1.25-1.38, 95% CIs = 1.02-1.89).[23] In European adolescents, short sleep duration was shown to associate with higher adiposity markers, particularly in females.[9] Similar findings were also reported by studies conducted on Indian[33] and Japanese adolescents.[13] In contrast to our findings, Huang et al. found no association between BMI and weekday total sleep time among Taiwanese adolescents.[36]
Several studies have shown that the association between short sleep duration and obesity (or BMI) was significant only in adolescent males[45,46] or females.[14] In the present study, gender effect was not significant (P = 0.788) in the logistic regression model [Table 3]. We even performed separate logistic regression analyses for males and females data, but this did not materially change the observed associations between sleep duration and obesity.
How sleep duration may precisely affect adiposity level is not fully understood; however, hormone regulating appetite and energy expenditure may likely be involved. It was suggested that both lower energy expenditure and an excess of energy intake may be involved in the sleep curtailment.[44] Furthermore, inadequate sleep is associated with alterations in leptin[11] as well as a reduction in insulin sensitivity.[47] The hormonal alteration can lead to increased hunger and appetite, thus raising the risk of overeating and consequently weight gain.[44] Furthermore, short sleep duration could also lead to overweight by increasing the time available to eat and drink.[44,48]
Using dual-energy X-ray absorptiometry, Yu et al. found the association of short sleep duration with WC (P<0.05) to be higher than that with BMI (P = 0.06).[14] In another study, WC was also shown to be higher in short sleepers compared with long sleepers.[11] In the present study, two-way ANCOVA test adjusted for age did not reveal significant differences between adequate and inadequate sleepers in WC or WHtR. However, when the proportions of adolescents above and below 50% of WHtR were contrasted with those having sleep duration above and below the cut-off value of 7 hours, Chi-Square test was significant, as seen in Figure 5.
The findings of the present study should be interpreted in light of their strengths and limitations. Among the strengths of the present study is its large, representative, and geographically diverse sample. We also used two indicators of obesity, namely cut-offs for BMI and for WHtR. However, we must acknowledge some of the potential limitations of the present study. The possible recall bias in the sleep duration questionnaire cannot be completely ruled out. However, self-reported information on sleep duration is an approach that was used in almost all large-scale sleep studies.[4,13,37,45] In addition, findings by Wolfson et al. on sleep patterns in adolescents supported the validity of sleep habit estimates in comparison with diary and actigraphy.[49] Furthermore, the sleep question presented to the participants reflected an average sleeping hours for a typical day of the week and did not distinguish between weekdays and weekends. Several studies have shown that longer sleep duration were reported during weekends than weekdays.[4,32] In addition, this study is of a cross-sectional design, which does not allow us to establish causality or temporality of associations. Short sleep duration may be contributing to obesity, but at the same time sleep curtailment may be a consequence of obesity presence. The later point can be explained by the increased risk of obstructive sleep apnea syndrome found in obese adolescents.[50]
In the current study, adolescent's pubertal stage was not assessed. Previous research have shown that overweight girls were shown to be associated with earlier maturation, while early mature boys were correlated with reduced BMI.[51] Therefore, the differences in sexual maturational patterns between the study's participants and subsequent influences on sleep duration and obesity level cannot be completely ruled out. Sleep duration was shown to inversely relate to pubertal development among US adolescents.[41] However, the age range of the participants in the present study was from 15 to 19 years, something that may have reduced the variations in pubertal stages to a great extent. Finally, it is possibly that lifestyle-related factors, such as physical activity, sedentary behaviors, and dietary habits, might have correlated with both sleep duration and obesity among adolescents in the current study. Caffeine use in particular, which was not assessed in this study, could have also affected sleep duration. Future studies need to consider accounting for such confounders.
In conclusion, the present study observed a high prevalence of short sleep duration among Saudi adolescents 15 to 19 year olds and that short sleep duration was significantly associated with increased risk of overweight and obesity. For the prevention of adolescent obesity, sleep duration must be an important risk factor to be considered. Future interventions should investigate whether adopting a healthy lifestyle by adolescents with short sleep duration would improve their sleeping habits or not.
Acknowledgments
Professor Hazzaa M Al-Hazzaa research was supported by fund from the Educational Research Center, Deanship of Research, King Saud University. The authors also acknowledge the assistance of several male and female research assistants who kindly assisted in the data collection throughout the participating cities. A special thank to Nouf A. Alsulaiman, MSc. for supervising the data collection of female participants in Jeddah.
Footnotes
Source of Support: Educational Research Center, Deanship of Research, King Saud University
Conflict of Interest: None declared.
References
- 1.Chen MY, Wang EK, Jeng YJ. Adequate sleep among adolescents is positively associated with health status and health-related behaviors. BMC Public Health. 2006;6:59. doi: 10.1186/1471-2458-6-59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Dahl RE, Lewin DS. Pathways to adolescent health sleep regulation and behavior. J Adolesc Health. 2002;31(6 Suppl):175–84. doi: 10.1016/s1054-139x(02)00506-2. [DOI] [PubMed] [Google Scholar]
- 3.Banks S, Dinges DF. Behavioral and physiological consequences of sleep restriction. J Clin Sleep Med. 2007;3:519–28. [PMC free article] [PubMed] [Google Scholar]
- 4.Olds T, Maher C, Blunden S, Matricciani L. Normative data on the sleep habits of Australian children and adolescents. Sleep. 2010;33:1381–8. doi: 10.1093/sleep/33.10.1381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Dollman J, Ridley K, Olds T, Lowe E. Trends in the duration of school-day sleep among 10- to 15-year-old South Australians between 1985 and 2004. Acta Paediatr. 2007;96:1011–4. doi: 10.1111/j.1651-2227.2007.00278.x. [DOI] [PubMed] [Google Scholar]
- 6.Iglowstein I, Jenni OG, Molinari L, Largo RH. Sleep duration from infancy to adolescence: reference values and generational trends. Pediatrics. 2003;111:302–7. doi: 10.1542/peds.111.2.302. [DOI] [PubMed] [Google Scholar]
- 7.Cappuccio FP, Taggart FM, Kandala NB, Currie A, Peile E, Stranges S, et al. Meta-analysis of short sleep duration and obesity in children and adults. Sleep. 2008;31:619–26. doi: 10.1093/sleep/31.5.619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Chen X, Beydoun MA, Wang Y. Is sleep duration associated with childhood obesity? A systematic review and meta-analysis. Obesity (Silver Spring) 2008;16:265–74. doi: 10.1038/oby.2007.63. [DOI] [PubMed] [Google Scholar]
- 9.Garaulet M, Ortega FB, Ruiz JR, Rey-López JP, Béghin L, Manios Y, et al. Short sleep duration is associated with increased obesity markers in European adolescents: Effect of physical activity and dietary habits. The HELENA study. Int J Obes (Lond) 2011;35:1308–17. doi: 10.1038/ijo.2011.149. [DOI] [PubMed] [Google Scholar]
- 10.Gupta NK, Mueller WH, Chan W, Meininger JC. Is obesity associated with poor sleep quality in adolescents? Am J Hum Biol. 2002;14:762–8. doi: 10.1002/ajhb.10093. [DOI] [PubMed] [Google Scholar]
- 11.Hitze B, Bosy-Westphal A, Bielfeldt F, Settler U, Plachta-Danielzik S, Pfeuffer M, et al. Determinants and impact of sleep duration in children and adolescents: data of the Kiel Obesity Prevention Study. Eur J Clin Nutr. 2009;63:739–46. doi: 10.1038/ejcn.2008.41. [DOI] [PubMed] [Google Scholar]
- 12.Marshall NS, Glozier N, Grunstein RR. Is sleep duration related to obesity.A critical review of the epidemiological evidence? Sleep Med Rev. 2008;12:289–98. doi: 10.1016/j.smrv.2008.03.001. [DOI] [PubMed] [Google Scholar]
- 13.Sekine M, Yamagami T, Handa K, Saito T, Nanri S, Kawaminami K, et al. A dose-response relationship between short sleeping hours and childhood obesity: Results of the Toyama Birth Cohort Study. Child Care Health Dev. 2002;28:163–70. doi: 10.1046/j.1365-2214.2002.00260.x. [DOI] [PubMed] [Google Scholar]
- 14.Yu Y, Lu BS, Wang B, Wang H, Yang J, Li Z, et al. Shortsleep duration and adiposity in Chinese adolescents. Sleep. 2007;30:1688–97. doi: 10.1093/sleep/30.12.1688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Al Mamun A, Lawlor DA, Cramb S, O’Callaghan M, Williams G, Najman J. Do childhood sleeping problems predict obesity in young adulthood. Evidence from a prospective birth cohort study? Am J Epidemiol. 2007;166:1368–73. doi: 10.1093/aje/kwm224. [DOI] [PubMed] [Google Scholar]
- 16.El Mouzan MI, Foster PJ, Al Herbish AS, Al Salloum AA, Al Omer AA, Qurachi MM, et al. Prevalence of overweight and obesity in Saudi children and adolescents. Ann Saudi Med. 2010;30:203–8. doi: 10.4103/0256-4947.62833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Al-Hazzaa HM. Rising trends in BMI of Saudi adolescents: evidence from three national cross sectional studies. Asia Pac J ClinNutr. 2007;16:462–6. [PubMed] [Google Scholar]
- 18.Barlow SE. Expert Committee. Expert committee recommendations regarding the prevention, assessment, and treatment of child and adolescent overweight and obesity: Summary report. Pediatrics. 2007;120(Suppl 4):S164–92. doi: 10.1542/peds.2007-2329C. [DOI] [PubMed] [Google Scholar]
- 19.Must A, Anderson SE. Effects of obesity on morbidity in children and adolescents. Nutr Clin Care. 2003;6:4–12. [PubMed] [Google Scholar]
- 20.Lobstein T, Baur L, Uauy R. IASO International Obesity Task Force.Obesity in children and young people: a crisis in public health. Obes Rev. 2004;5(Suppl 1):4–85. doi: 10.1111/j.1467-789X.2004.00133.x. [DOI] [PubMed] [Google Scholar]
- 21.BaHammam A, AlFaris E, Shaikh S, Bin Saeed A. Prevalence of sleep problems and habits in a sample of Saudi primary school children. Ann Saudi Med. 2006;26:7–13. doi: 10.5144/0256-4947.2006.7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.BaHammam A, Bin Saeed A, Al-Faris E, Shaikh S. Sleep duration and its correlates in a sample of Saudi elementary school children. Singapore Med J. 2006;47:875–81. [PubMed] [Google Scholar]
- 23.Bawazeer NM, Al-Daghri NM, Valsamakis G, Al-Rubeaan KA, Sabico SL, Huang TT, et al. Sleep duration and quality associated with obesity among Arab children. Obesity. 2009;17:2251–3. doi: 10.1038/oby.2009.169. [DOI] [PubMed] [Google Scholar]
- 24.Bahammam AS. Sleep medicine in Saudi Arabia: Current problems and future challenges. Ann Thorac Med. 2011;6:3–10. doi: 10.4103/1817-1737.74269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Al-Hazzaa HM, Musaiger A ATLS Group. Physical activity patterns and eating habits ofadolescents living in major Arab cities: The Arab Teens Lifestyle Study. Saudi Med J. 2010;31:210–1. [PubMed] [Google Scholar]
- 26.Al-Hazzaa HM, Musaiger A ATLS Group. Arab Teens Lifestyle Study (ATLS): objectives, design, methodology and implications. Diabetes Metab Syndr Obes. 2011;4:417–26. doi: 10.2147/DMSO.S26676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Cole T, Bellizzi M, Flegal K, Dietz W. Establishing a standard definition of child overweight and obesity worldwide: International survey. BMJ. 2000;320:1240–3. doi: 10.1136/bmj.320.7244.1240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.McCarthy HD, Ashwell M. A study of central fatness using waist-to-height ratios in UK children and adolescents over two decades supports the simple message--’keep your waist circumference to less than half your height’. Int J Obes (Lond) 2006;30:988–92. doi: 10.1038/sj.ijo.0803226. [DOI] [PubMed] [Google Scholar]
- 29.Taylor RW, Jones IE, Williams SM, Goulding A. Evaluation of waist circumference, waist-to-hip ratio, and the conicity index as screening tools for high trunk fat mass, as measured by dual-energy X-ray absorptiometry, in children aged 3-19 y. Am J ClinNutr. 2000;72:490–5. doi: 10.1093/ajcn/72.2.490. [DOI] [PubMed] [Google Scholar]
- 30.Washington: National Sleep Foundation; [Last accessed on 2011 Oct21]. National Sleep Foundation. How much sleep do we really need? Available from: http://www.sleepfoundation.org/article/how-sleep-works/howmuch-sleep-do-we-really-need . [Google Scholar]
- 31.Ortega FB, Ruiz JR, Castillo R, Chillón P, Labayen I, Martínez-Gómez D, et al. AVENA study group. Sleep duration and cognitive performance in adolescence. The AVENA study. Acta Paediatr. 2010;99:454–6. doi: 10.1111/j.1651-2227.2009.01618.x. [DOI] [PubMed] [Google Scholar]
- 32.Loessl B, Valerius G, Kopasz M, Hornyak M, Riemann D, Voderholzer U. Are adolescentschronically sleep-deprived? An investigation of sleep habits of adolescents in the Southwest of Germany. Child Care Health Dev. 2008;34:549–56. doi: 10.1111/j.1365-2214.2008.00845.x. [DOI] [PubMed] [Google Scholar]
- 33.Gupta R, Bhatia MS, Chhabra V, Sharma S, Dahiya D, Semalti K, et al. Sleep patterns of urban school-going adolescents. Indian Pediatr. 2008;45:183–9. [PubMed] [Google Scholar]
- 34.Reid A, Maldonado CC, Baker FC. Sleepbehavior of South African adolescents. Sleep. 2002;25:423–7. [PubMed] [Google Scholar]
- 35.Liu X, Zhao Z, Jia C, Buysse DJ. Sleeppatterns and problems among Chinese adolescents. Pediatrics. 2008;121:1165–73. doi: 10.1542/peds.2007-1464. [DOI] [PubMed] [Google Scholar]
- 36.Huang YS, Wang CH, Guilleminault C. An epidemiologic study of sleep problems among adolescents in North Taiwan. Sleep Med. 2010;11:1035–42. doi: 10.1016/j.sleep.2010.04.009. [DOI] [PubMed] [Google Scholar]
- 37.McKnight-Eily LR, Eaton DK, Lowry R, Croft JB, Presley-Cantrell L, Perry GS. Relationships between hours of sleep and health-risk behaviors in US adolescent students. Prev Med. 2011;53:271–3. doi: 10.1016/j.ypmed.2011.06.020. [DOI] [PubMed] [Google Scholar]
- 38.Ohida T, Osaki Y, Doi Y, Tanihata T, Minowa M, Suzuki K, et al. An epidemiologic study of self-reported sleep problems among Japanese adolescents. Sleep. 2004;27:978–85. doi: 10.1093/sleep/27.5.978. [DOI] [PubMed] [Google Scholar]
- 39.Epstein R, Chillag N, Lavie P. Starting times of school: Effects on daytime functioning of fifth-grade children in Israel. Sleep. 1998;21:250–6. doi: 10.1093/sleep/21.3.250. [DOI] [PubMed] [Google Scholar]
- 40.2006 Sleep in America Poll. Washington: National Sleep Foundation; 2006. [Last accessed on 2011 Oct 21]. National Sleep Foundation. Available from: http://www.sleepfoundation.org/sites/default/files/Highlights_facts_06.pdf . [Google Scholar]
- 41.Knutson KL. The association between pubertal status and sleep duration and quality among a nationally representative sample of U. S. adolescents. Am J Hum Biol. 2005;17:418–24. doi: 10.1002/ajhb.20405. [DOI] [PubMed] [Google Scholar]
- 42.Randler C, Bilger S. Associations among sleep, chronotype, parental monitoring, and pubertal development among German adolescents. J Psychol. 2009;143:509–20. doi: 10.3200/JRL.143.5.509-520. [DOI] [PubMed] [Google Scholar]
- 43.Patel SR, Hu FB. Shortsleepduration and weight gain: a systematic review. Obesity (Silver Spring) 2008;16:643–53. doi: 10.1038/oby.2007.118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Van Cauter E, Knutson KL. Sleep and the epidemic of obesity in children and adults. Eur J Endocrinol. 2008;159:S59–66. doi: 10.1530/EJE-08-0298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Eisenmann JC, Ekkekakis P, Holmes M. Sleep duration and overweight among Australian children and adolescents. Acta Paediatr. 2006;95:956–63. doi: 10.1080/08035250600731965. [DOI] [PubMed] [Google Scholar]
- 46.Knutson KL. Sex differences in the association between sleep and body mass index in adolescents. J Pediatr. 2005;147:830–4. doi: 10.1016/j.jpeds.2005.07.019. [DOI] [PubMed] [Google Scholar]
- 47.Javaheri S, Storfer-Isser A, Rosen CL, Redline S. Association of short and long sleep durations with insulin sensitivity in adolescents. J Pediatr. 2011;158:617–23. doi: 10.1016/j.jpeds.2010.09.080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Sivak M. Sleeping more as a way to lose weight. Obes Rev. 2006;7:295–6. doi: 10.1111/j.1467-789X.2006.00262.x. [DOI] [PubMed] [Google Scholar]
- 49.Wolfson AR, Carskadon MA, Acebo C, Seifer R, Fallone G, Labyak SE, et al. Evidence for the validity of a sleep habits survey for adolescents. Sleep. 2003;26:213–6. doi: 10.1093/sleep/26.2.213. [DOI] [PubMed] [Google Scholar]
- 50.Kohler MJ, Thormaehlen S, Kennedy JD, Pamula Y, van den Heuvel CJ, Lushington K, et al. Differences in the association between obesity and obstructive sleep apnea among children and adolescents. J Clin Sleep Med. 2009;5:506–11. [PMC free article] [PubMed] [Google Scholar]
- 51.Wang Y. Is obesity associated with early sexual maturation? A comparison of the association in American boys versus girls. Pediatrics. 2002;110:903–10. doi: 10.1542/peds.110.5.903. [DOI] [PubMed] [Google Scholar]


