Sir,
Conventional teaching recommends the immediate administration of palliative thoracic radiotherapy (PTR) for superior vena caval obstruction (SVCO) by lung cancer (LCa). On the other hand, superior vena caval syndrome gradually develops over several weeks and, therefore, is unlikely to be a life-threatening condition unless the patient presents with airway obstruction, hemodynamic instability, or increased intracranial pressure. Some experiences have employed a short delay in the initiation of PTR while others have not.[1–4] This study investigates the timing of PTR in patients with SVCO by LCa and how the onset of this therapeutic intervention influenced patient outcomes.
Forty-two consecutive individuals (30 men and 12 women with a mean age of 53.5 years) treated by PTR for SVCO-LCa between 1981 and 2009 are the subjects of this retrospective analysis. SVCO was present when patients exhibited a plethoric facies, swelling of the face/neck/upper extremities, or visibly dilated collateral superficial veins in the anterior part of the trunk with or without dyspnea and radiological evidence of superior vena caval compression by a mediastinal or paramediastinal mass within the thorax.
Thirteen individuals underwent PTR on the day of referral and 29 people were treated several days after the radiation oncology consultation. Delay in the initiation of PTR was ≤1 week (20 patients), >1 to 2 weeks (5 patients), and >2 weeks to 1 month (4 patients).
PTR (usually 30 Gy/10 fractions) meant megavoltage external beam irradiation of the intrathoracic neoplasm and the mediastinum. Ten individuals were treated with high daily dose fractions of 3 to 4 Gy for the initial 3 days. Chemotherapy (Cyclophosphamide or Cisplatin with Etoposide) was administered in three patients with stage IIIB LCa. Survival was estimated from the time of diagnosis until death or last follow-up. Responses (significant resolution of SVCO manifestations and/or a 50% reduction in size of the imaging-shown tumor) to treatment were assessed after completion of PTR.
The duration of symptoms and signs prior to referral for irradiation (information available in only 34 individuals) ranged from 2 to 112 days (median 26.2 days). Stridor or mental obtundation was not observed in a single patient. The overall median survival was 4.5 months (95% confidence interval [CI], 3 to 10 months) and 1-year survival rate was 24% (95% CI, 11% to 37%). The achieved (complete plus partial) palliation and absent objective response rates were 84% and 16%, respectively.
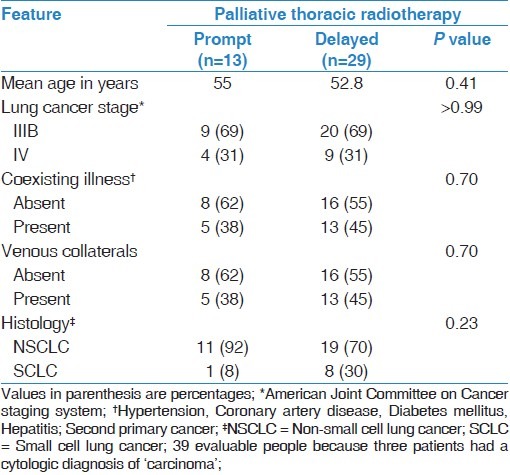
Demographic information was not significantly different between the compared groups [Table 1]. The number of promptly treated people obtaining palliation was no different to the number of responders among individuals whose PTR was delayed (86% and 83%, respectively); the corresponding 1-year survival rates and median survival times were 15% (95% CI, 0% to 34%) and 4 months (95% CI, 3 to 7 months), respectively, for the patients treated without delay and 28% (95% CI, 11% to 44%) and 6 months (95% CI, 3 to 10 months) for the delayed PTR group (P = 0.37).
Table 1.
Comparisons between patients with different timing of palliative thoracic radiotherapy for superior vena caval obstruction by lung cancer
Delay in starting radiotherapy is unacceptable to many oncologists because it may affect outcomes by permitting tumor progression through the proliferation of clonogenic cells, retarding the benefits of PTR and causing psychological suffering. Theoretically, the risk of death may be increased by the prolongation of venous obstruction with the potential for laryngeal edema, thrombosis, encephalopathy, and irreversible central nervous system damage. Two pivotal reports about this disease condition concluded that SVCO does not constitute a radiotherapeutic emergency because there is little shown evidence that venous obstruction has caused life-threatening situations (i.e., cerebral or laryngeal edema) and the patient's demise was the direct result of SVCO.[2,5] Furthermore, it has been observed that individuals have survived despite unrelieved blockage. Albeit the issue of PTR timing for SVCO may be contentious, we believe that treatment should not be initiated without a histological diagnosis of malignancy. Furthermore, we agree with the prevalent opinion that PTR is urgently required when stridor, cyanosis, tachypnea in an upright position in the absence of congestive heart failure, hemodynamic instability, or altered state of consciousness from cerebral edema are manifested in patients with SVCO-LCa.
In conclusion, our retrospective study suggests that a short delay in the onset of PTR may not be harmful. Moreover, it highlights the efficacy of PTR in the alleviation of SVCO by LCa. Consensus guidelines (based on the balance of evidence from retrospective studies and expert opinion) are needed considering the fact that the disturbing acute clinical manifestations of SVCO would negate undertaking a clinical trial.
References
- 1.Egelmeers A, Goor C, van Meerbeck J, van den Weyngaert D, Scalliet P. Palliative effectiveness of radiation therapy in the treatment of superior vena cava syndrome. Bull Cancer/Radiother. 1996;83:153–7. doi: 10.1016/0924-4212(96)81747-6. [DOI] [PubMed] [Google Scholar]
- 2.Gauden SJ. Superior vena cava syndrome induced by bronchogenic carcinoma: Is this an oncological emergency? Australas Radiol. 1993;37:363–6. doi: 10.1111/j.1440-1673.1993.tb00096.x. [DOI] [PubMed] [Google Scholar]
- 3.Lonardi F, Gioga G, Agus G, Coeli M, Campostrini F. Double-flash Large- fraction radiation therapy as palliative treatment of malignant superior vena cava syndrome in the elderly. Support Care Cancer. 2002;10:156–60. doi: 10.1007/s00520-001-0313-4. [DOI] [PubMed] [Google Scholar]
- 4.Rodrigues CI, Njo KH, Karim AB. Hypofractionated radiation therapy in the treatment of superior vena cava syndrome. Lung Cancer. 1993;10:221–8. doi: 10.1016/0169-5002(93)90182-w. [DOI] [PubMed] [Google Scholar]
- 5.Schraufnagel DE, Hill R, Leech JA, Pare JAP. Superior vena caval obstruction - is it a medical emergency? Am J Med. 1981;70:1169–74. doi: 10.1016/0002-9343(81)90823-8. [DOI] [PubMed] [Google Scholar]


