Abstract
Introduction:
With better health care facilities and nutritional levels the average life expectancy of Indian population has been on the rise over the years. Most of the geriatric population is under long-term medication.
Aim:
The aim of this study was to evaluate the synergistic effect of multiple xerostomia drugs.
Materials and Methods:
Unstimulated saliva was measured in 60 geriatric patients, and xerostomia questionnaire and quality-of-life scale were also administered.
Results:
There was a very highly significant reduction in the salivary flow rates of patients under multiple xerostomia-inducing drugs.
Conclusion:
The synergistic effect of the xerostomia inducing medication could be the possible factor responsible for reduced salivary flow in elderly individuals using such drugs
Keywords: Quality of life, synergistic, xerostomia
Introduction
The average life expectancy of an Indian has gone up from 32 years in 1951 to around 60 years in 1993. It is expected that nearly 14% of Indian population will be above the age of 60 years by the year 2025 that means nearly 177 million elderly people in the country.[1] Better health care facilities and improvement in standard of living have been the key factors responsible for the increase in life expectancy. Forty-five percent of the older Indians have chronic diseases and disabilities.[1] Studies have revealed that the most common health-related problem among elderly Indians are hypertension, arthritis, diabetes, and constipation.[2] Several of these diseases and the medications used for them can cause reduction in the salivary flow. Reduced salivary flow or xerostomia is associated with oral dryness, taste loss, dysphagia, increased dental caries, and periodontal disease, ultimately deteriorating the quality of life.[3] Geriatric oral health care has not received the same amount of importance as in the western countries.[4] Studies linked to xerostomia have been sparsely carried out in the Indian geriatric population. Considering this fact, we conducted a cross-sectional study involving 60 geriatric age group patients attending the outpatient department in an institutional setup. Unstimulated saliva was collected from these patients after obtaining a thorough drug history and administering them xerostomia questionnaire and quality-of-life (QoL) scale. This study is intended to evaluate the salivary flow in individuals consuming single drug known to induce xerostomia with those consuming multiple drugs capable of inducing xerostomia.
Review of Literature
Xerostomia is a common debilitating condition, which causes problems such as dysphagia, taste loss, and oral pain.[5] It also increases the risk of dental caries and oral infection.[6] Histologic studies have revealed age-related changes in major salivary gland.[7] It has been reported that taking prescribed medications and experiencing a stressful life change had a significant effect on the subjective oral dryness.[8] Many dental patients may have more than one disease, which complicates evaluation of the adverse effects on salivary flow, both of the disease itself and of the medication(s) prescribed to deal with it.[9,10]
Objectives
Evaluate the salivary flow rate in elderly individuals with and without the intake of xerostomia-inducing medications.
To evaluate the salivary flow rate in elderly individuals with intake of single xerostomia-inducing medication.
To evaluate salivary flow rate in individuals with intake of multiple-xerostomia–inducing medication.
To compare salivary flow rate in individuals with intake of single- and multiple-xerostomia–inducing medication.
Materials and Methods
A cross-sectional study involving 60 patients above the age of 60 years reporting to the Department of Oral Medicine and Radiology, AB Shetty Memorial Institute of Dental Sciences, Nitte University, Mangalore, were enrolled into the study. They were divided into three groups.
Group A
Twenty patients above the age of 60 years without any systemic disease and long-term medication.
Group B
Twenty patients above the age of 60 years with intake of a single drug known to cause xerostomia.
Group C
Twenty patients above the age of 60 years with intake of more than one drug known to cause xerostomia.
Inclusion criteria
For the control group, the age group of above 60 years; not under long-term medication; and without any systemic disease.
Exclusion criteria
Patients with salivary gland aplasia or hypoplasia, Sjogren syndrome, sarcoidosis, or amyloidosis, patients who have undergone head and neck radiotherapy, chemotherapy, or salivary gland surgery.
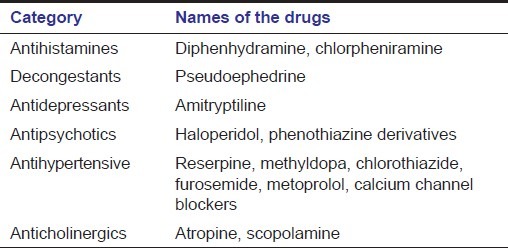
A detailed case history and thorough clinical examination of the patient was performed and the patient was administered a xerostomia questionnaire in local language. Patients using the following medication were included in the study [Table 1].
Table 1.
List of xerostomia including medications
Unstimulated saliva was collected from each patient using the spit method from 8 am. to 2 pm. Saliva samples were collected from patients who had not consumed any food or beverages, chewing gum, brushed teeth, used mouthwashes, or any form of tobacco 2 h prior to collection. Following a thorough mouth rinse using distilled water, saliva was allowed to accumulate in his or her mouth for 5 min. Accumulated saliva collected by spit method was measured using graduated test tube (VENSIL 5 mL). The data obtained was subjected to statistical evaluation using one-way analysis of variance (ANOVA) by Statistical Package for Social Sciences (SPSS) version 17. Ethical clearance was obtained from the concerned authorities.
Results
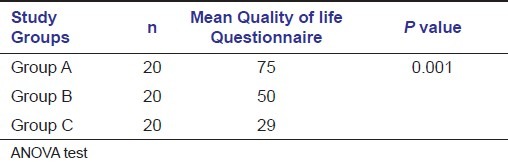
In our study, Group A had equal gender distribution, whereas groups B and C had 76.2% and 61.9% males, respectively. Unstimulated salivary flow of females in groups A and C was less when compared with males. In Group B 55% of the study subjects used oral hypoglycemics, 25% of them used cardiovascular drugs, 10% of them used antidepressants, and 10% of them used other drugs mentioned in the inclusion criteria. In Group C, 50% of the study subjects used the combination of oral hypoglycemics and cardiovascular drugs, 20% of them used the combination of cardiovascular and antidepressant drugs, 15% of them used the combination of oral hypoglycemics and antidepressant drugs, and 15% of them used other combinations. The mean unstimulated salivary flow rate was 1.5 mL/5 min in Group A, 0.7 mL/5 min in Group B, and 0.3 mL/5 min in Group C. There was a very highly significant difference in the unstimulated salivary flow rate among the three groups [Table 2]. Xerostomia questionnaire scale score was 2, 6.1, and 8.2 in groups A, B, and C, respectively [Table 3]. There was a very highly significant difference (P < 0.001) among the three groups when compared using the ANOVA test. The QoL scale scores were 75, 50, and 29 for groups A, B, and C, respectively. There was a very highly significant difference of the mean score among the groups when ANOVA test was performed [Table 4].
Table 2.
Intercomparison of mean Unstimulated Saliva Flow Rate in the study groups
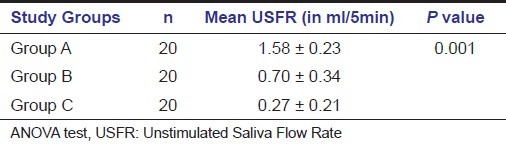
Table 3.
Intercomparison of Mean Xerostomia Questionnaire Scores in the study groups
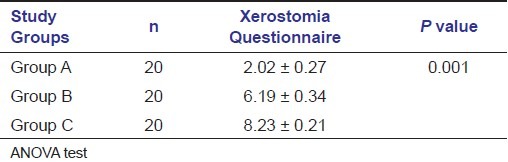
Table 4.
Intercomparison of mean Quality of life Questionnaire Scores in the study groups
Discussion
Xerostomia or dry mouth is the abnormal reduction of saliva and can be a symptom of certain diseases or be an adverse effect of certain medications. Xerostomia is a subjective sensation that was considered to be another expression of age-related physiologic deterioration.[11] Xerostomia is a subjective feeling of dry mouth, and can therefore be assessed only by directly questioning individuals along with sialometry. In our study, xerostomia questionnaire and QoL scale score were used. Normal salivary flow rates at rest are 0.3 mL/min. To date, xerostomia has been associated with more than 500 medications. In addition, the synergistic effects of medications have been recognized and are increasingly common in elderly patients taking multiple medications.[12] In the present study, the unstimulated salivary flow rate explained the synergistic effect of multiple medication on salivary flow. The unstimulated salivary flow rate, in women in groups A and C was less when compared with that of men, which is in accordance with Narhi et al and Porter et al.'s studies.[11,13] The study groups B and C also complained of oral dryness, oral pain, and taste loss when compared with the controls. The values were highly significant. Similar findings were noted by Bergdahl et al, and thus they concluded that medications play an important role in reducing unstimulated salivary flow.[14] The study groups B and C also reported of decreased quality of life when compared with the controls with highly significant values. This is in accordance with Dirix et al.[3]
Drug-induced xerostomia is one of the common causes for oral health-related problems in elderly individuals who are on long-term drug therapy. Recent studies have come up with contrasting results regarding the reduced salivary flow in individuals who are on more than one xerostomia-inducing drug. The aim of the study was to evaluate whether a synergistic effect on the salivary flow exists when more than one xerostomia-inducing drug are administered. If such a synergistic effect exists then one of the drugs could be replaced by a counterpart that does not induce xerostomia. Hence xerostomia-associated oral health problems can be drastically reduced in the elderly.
Conclusion and Summary
Studies have indicated that the severity of the xerostomia increases among the elderly due to a synergistic effect when taking multiple medications. But, however, xerostomia-associated oral health complications can be reduced by
Elimination or reduction of the selected drugs;
Change in the manner in which they are taken;
Substitution of one drug for another with less xerogenic effects.
Several medications lead to reduction in salivary flow. The aim of the study was to evaluate the salivary flow rate in elderly individuals with intake of single- and multiple-xerostomia–inducing medications. On this basis 60 subjects older than 60 years were divided into 3 groups. The saliva from the subjects was collected by spit method and statistical analysis was done. The result showed that the mean unstimulated salivary flow rate was significantly reduced in case of subjects on multiple-xerostomia–inducing drugs. The study concluded that synergistic effects of xerostomia-inducing medications were observed in elderly patients taking multiple medications. However, the intensity of xerostomia can be reduced by the substitution of drugs or by change in the manner in which they are taken.
Footnotes
Source of Support: ICMR-STS.
Conflict of Interest: None declared.
References
- 1.Swami HM, Bhatia V. Primary health care geriatric in India. Indian J Prev Soc Med. 2003;34:148–52. [Google Scholar]
- 2.Elango S. A study of health and health related social problems in the geriatric population in a rural area of Tamil Nadu. Indian J Public Health. 1998;42:7–8. [PubMed] [Google Scholar]
- 3.Dirix P, Nuyts S, Poorten VV, Delaere P, Bogaert WV. Efficacy of the Bioxtra dry mouth care system in the treatment of radiotherapy–induced xerostomia. Support Care Cancer. 2007;15:1429–36. doi: 10.1007/s00520-006-0210-y. [DOI] [PubMed] [Google Scholar]
- 4.Lehl G, Lehl SS. Oral health care in the elderly. J Ind Acad Geriatr. 2005;1:25–30. [Google Scholar]
- 5.Grotz KA, Genitsariotis S, Vehling D, Al-Nawas B. Long term oral candida colonization, mucositis and salivary function after head and neck radiotherapy. Support Care Cancer. 2003;11:717–21. doi: 10.1007/s00520-003-0506-0. [DOI] [PubMed] [Google Scholar]
- 6.Momm F, Voegova-Neher NJ, Schulte-Monting J, Guttenberger R. Different saliva substitutes for treatment of xerostomia following radiotherapy. Strahlenther Onkol. 2005;181:231–6. doi: 10.1007/s00066-005-1333-7. [DOI] [PubMed] [Google Scholar]
- 7.Scott J. Quantitative changes in histological structure of the human submandibular salivary glands. Arch Oral Biol. 1977;22:221–7. doi: 10.1016/0003-9969(77)90158-3. [DOI] [PubMed] [Google Scholar]
- 8.Locker D. Subjective reports of oral dryness in an older adult population. Community Dent Oral Epidemiol. 1993;21:165–8. doi: 10.1111/j.1600-0528.1993.tb00744.x. [DOI] [PubMed] [Google Scholar]
- 9.Sreebny LM, Valdini A, Yu A. Xerostomia. Part II: Relationship to nonoral symptoms, drugs, and diseases. Oral Surg Oral Med Oral Pathol. 1989;68:419–27. doi: 10.1016/0030-4220(89)90140-0. [DOI] [PubMed] [Google Scholar]
- 10.Navazesh M, Brightman VJ, Pogoda JM. Relationship of medical status, medications, and salivary flow rates in adult of different ages. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1996;81:172–6. doi: 10.1016/s1079-2104(96)80410-0. [DOI] [PubMed] [Google Scholar]
- 11.Porter SR, Scully C, Hegarty AM. An update of the etiology and management of Xerostomia. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2004;97:28–46. doi: 10.1016/j.tripleo.2003.07.010. [DOI] [PubMed] [Google Scholar]
- 12.Porter SR, Scully C. Adverse drug reactions in the mouth. Clin Dermatol. 2000;18:525–32. doi: 10.1016/s0738-081x(00)00143-7. [DOI] [PubMed] [Google Scholar]
- 13.Narhi TO, Meurman JH, Ainamo A, Nevalainen JM, Schmidt-Kaunisaho KG, Siukosaari P, et al. Association between salivary flow rate and the use of systemic medication among 76-, 81-, and 86-year old inhabitants in Helsinki, Finland. J Dent Res. 1992;71:1875–80. doi: 10.1177/00220345920710120401. [DOI] [PubMed] [Google Scholar]
- 14.Bergdahl M, Bergdahl J. Low unstimulated salivary flow and subjective oral dryness: Association with medication, anxiety, depression and stress. J Dent Res. 2000;79:1652–8. doi: 10.1177/00220345000790090301. [DOI] [PubMed] [Google Scholar]


