Abstract
Introduction:
The assessment of micronuclei in exfoliated cells is a promising tool for the study of epithelial carcinogens and can be used to detect chromosome breakage or mitotic interference, thought to be relevant to carcinogenesis.
Aim:
The present study aimed to detect micronuclei in exfoliated oral mucosal cells in individuals using various tobacco forms from the last 5 years.
Materials and Methods:
A total of 75 healthy male subjects (25 smokeless tobacco users, 25 smokers, and 25 non–tobacco users) were selected for the study. Smears were obtained with moistened wooden spatula from buccal mucosa and fixed with 95% alcohol. All the cytologic smears were stained by Papanicolaou technique. From each slide, ~1000 cells were examined under the 400× magnification and where micronucleated (MN) cells were located, they were examined under the 1000× magnification.
Result:
MN cells were found to be significantly higher in smokeless tobacco users than in smokers and controls.
Conclusion:
A positive correlation is found between increased micronucleus frequency and tobacco-using habits. So micronucleus assay can be used as a biomarker of genotoxicity.
Keywords: Chromosomal aberrations, exfoliative cytology, genotoxic agents, micronuclei, Papanicolaou stain
Introduction
Cancer is one of the most common causes of morbidity and mortality today. The global burden of cancer continues to increase mostly because of increasing adoption of cancer-causing behaviors, particularly smoking and smokeless tobacco forms in economically developing countries. Globally, about 5,00,000 new oral and pharyngeal cancers are diagnosed annually and three quarters of these are seen in the developing world, including about 65,000 cases reported in India. The World Health Organization (WHO) estimated that the proportion of deaths that result from tobacco-related diseases will rise in India from 1.4% of all deaths in 1990 to 13.3% of all deaths in 2020. The number of persons consuming tobacco is also likely to rise, according to the models presented in the 2002 report of the Economic and Social Council (ECOSOC) of the United Nations.[1,2]
Oral carcinomas are characterized by complex karyotypes that involve many chromosomal deletions, translocations, and structural abnormalities. Cells often have errors in chromosome segregation that lead to the formation of a lagging chromosome or chromosome parts that become lost during the anaphase stage of cell separation and are excluded from the reforming nuclei. The laggards are observed in the cytoplasm as micronuclei.[3]
The micronuclei are extranuclear cytoplasmic bodies associated with chromosomal aberrations. These are induced in oral exfoliated cells by a variety of substances, including genotoxic agents and carcinogenic compounds in tobacco, betel nut, and alcohol. The induction of micronucleated (MN) cells by carcinogens and mutagens is a sign of the genotoxic effect of such substances.[4] These are also observed in exfoliated buccal cells, from people who are exposed to organic solvents, antineoplastic agents, diesel derivatives, polycyclic aromatic hydrocarbons, lead-containing paints and solvents, and drinking water, which is contaminated with arsenic.[3]
The assessment of micronuclei in exfoliated cells is a promising tool for the study of epithelial carcinogens and can be used to detect chromosome breakage or mitotic interference, thought to be relevant to carcinogenesis.[5] Due to its association with chromosomal aberrations, micronuclei have been used since 1937 as an indicator of genotoxic exposure based on the radiation studies conducted by Brenneke and Mather.[6] The direct correlation between the micronuclei formation and genomic damage make the micronuclei assay an efficient alteration to the metaphase analysis.[4]
Aim
The present study aimed to detect micronuclei in exfoliated buccal mucosal cells in healthy tobacco users and healthy nontobacco users.
Materials and Methods
A total of 75 healthy male subjects (25 smokeless tobacco users, 25 smokers, and 25 non–tobacco users) who attended the outpatient department of Dental Institute, were examined and were selected for the study. The study group comprised smokeless tobacco chewers who chewed five or more packets daily for at least 5 years. The smokers included smoked every day for at least 5 years and consumed 20 or more bidis/cigarettes in a day. The control group persons were not habituated to any form of tobacco consumption. Individuals who were alcoholics, had a recent viral infection, had undergone radiation therapy, or those who had been under medication were excluded from the study.
Cytologic preparation
Before sampling, each individual rinsed his mouth thoroughly with tap water. The exfoliated cells were obtained by scraping the buccal mucosa with a moistened wooden spatula and the scraped cells were placed on the clean glass slides and smears were prepared. The smears were fixed with 95% ethyl alcohol. All the cytologic smears were stained by Papanicolaou technique using a commercially available staining kit RAPIDPAP. From each slide, ~ 1000 cells were examined under the ×400 magnification and where MN cells were located, they were examined under the 1000× magnification. The criterion which was developed by Tolbert et al was used for counting the micronuclei.
Tolbert et al criteria[5] parameters for identifying micronucleus are as follows:
Rounded smooth perimeter suggestive of a membrane.
Less than a third the diameter of associated nucleus, but large enough to discern shape and color.
Staining intensity similar to nucleus.
Texture similar to nucleus.
Same focal plane as nucleus.
Absence of overlap with or bridge to nucleus.
Dead or degenerating cells (karyolysis, karyorrhexis, nuclear fragmentation) were excluded from evaluation. Nuclear blebbings (micronucleus-like structure connected with the main nucleus with a bridge) were also not considered.
Results and Analysis
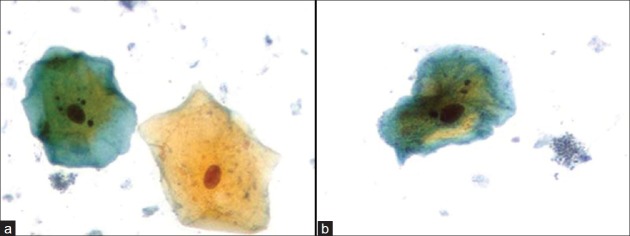
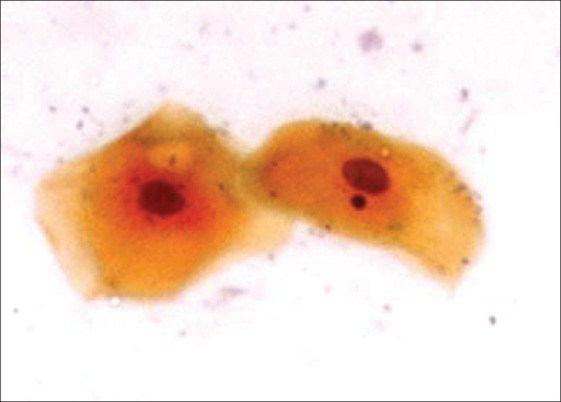
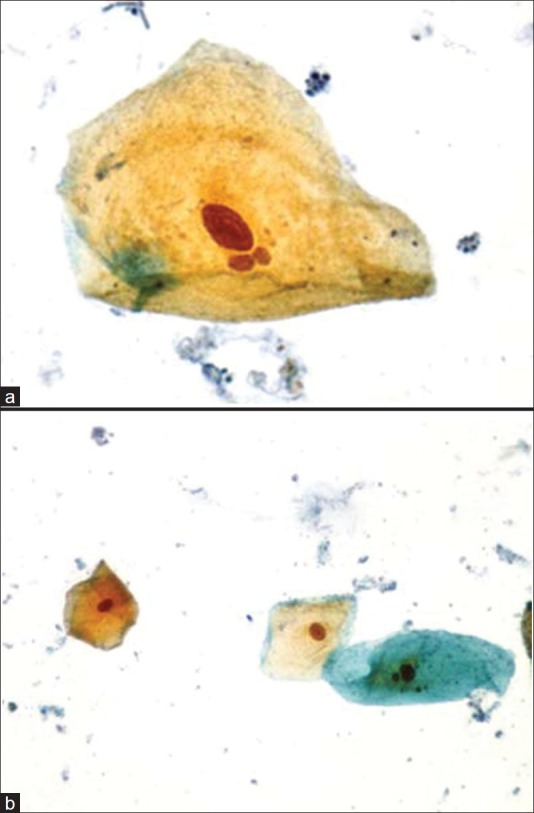
The MN cells observed are shown in Figures 1–3.
Figure 1.
Cell with a micronucleus Pap (×1000)
Figure 3.
(a) Cell with three micronuclei Pap (×1000); (b) cell with three micronuclei Pap (×1000)
Figure 2.
(a) Cell with two micronuclei Pap (×1000); (b) cell with two micronuclei Pap (×1000)
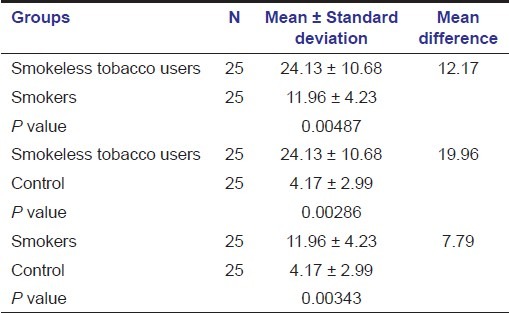
The frequency of distribution of micronuclei in the three study groups are shown in Figures 4–5.
Figure 4.
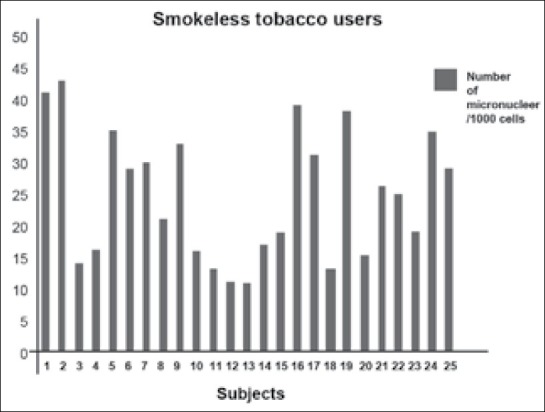
Number of micronuclei/1000 cells in smokeless tobacco users
Figure 5.
Number of micronuclei/1000 cells in smokers
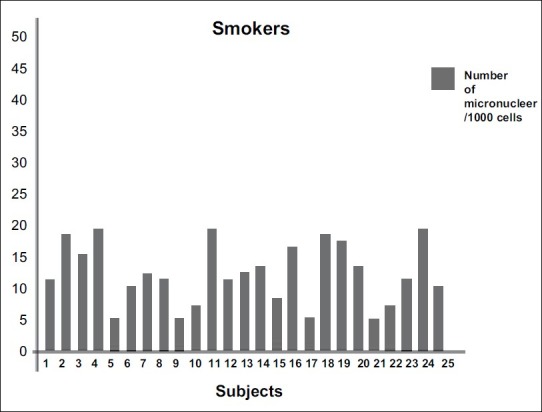
The mean number of micronuclei observed in the three groups are presented in table 1. The mean number of micronuclei in smokeless tobacco chewers, smokers, and controls were 24.13 ± 10.68, 11.96 ± 4.23, and 4.17 ± 2.99, respectively. The mean number of micronuclei found were more in smokeless tobacco chewers as compared with smokers and controls [Table 1].
Table 1.
Mean number of micronuclei in three study groups
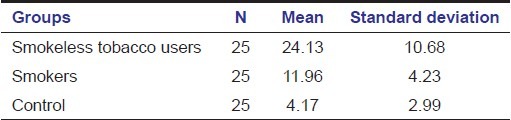
The mean values and the mean differences, which were obtained from the smokeless tobacco chewers, the smokers, and the controls were compared and are shown in table 2. In comparison, the mean difference between the number of micronuclei in smokeless tobacco chewers and smokers was 12.17 and was statistically significant (P < 0.05). The mean difference between the number of micronuclei in smokeless tobacco chewers and controls was 19.96 and was highly statistically significant (P < 0.05). The mean difference between the number of micronuclei in smokers and controls was 7.79 and was statistically significant (P < 0.05) [Table 2].
Table 2.
Multiple comparison of micronuclei in three study groups
Discussion
Oral carcinogenesis is a multistep process of accumulated genetic damage leading to cell dysregulation with disruption in cell signaling, DNA-repair, and cell cycle events, which are fundamental to hemostasis. These events can be conveniently studied in the buccal mucosa, which is an easily accessible tissue for sampling cells in a minimally invasive manner and does not cause undue stress to study subjects.[5]
Oral exfoliative cytology has been used extensively for screening cellular alterations, such as karyolysis, karyorrhexis, micronucleus formation, pyknosis, binucleation, broken egg nucleus, anucleation, and so on[5]. Micronuclei in oral exfoliated cells is a biomarker of chromosomal damage caused by genotoxic agents from tobacco and tobacco-related substances, alcohol, and so on. When the target tissue of interest is epithelial tissue, the exfoliated cell micronucleus assay has been used to assess the genotoxic damage in oral premalignancies and oral squamous cell carcinoma.[7,8]
The present study evaluated the mean number of micronuclei in smokeless tobacco users, smokers, and the healthy control group. The result showed that the overall level of mean number of micronuclei in smokeless tobacco were higher (24.13 ± 10.68) as compared with smokers (11.96 ± 4.23) and controls (4.17 ± 2.99). This observation was similar to those reported by Palaskar et al.,[3] Ozkul et al,[9] and Patel et al,[10] when all the groups were further compared with each other for the mean difference, the result was highly statistically significant (P < 0.05), which was in accordance with the previous studies by Palaskar et al.[3] and Patel et al.,[10] whereas Ozkul et al found no difference between the mean percentage of MN cells for the groups considered (P > 0.05).[9]
The incidence of micronuclei has been analyzed by various studies in normal patients, oral premalignancies, and OSCCs.[7] Casartelli et al observed micronuclei frequencies in exfoliated buccal cells in normal oral mucosa, precancerous lesions, and squamous cell carcinoma. They concluded that the gradual increase in micronucleus counts from normal mucosal to precancerous lesions to carcinoma suggested a link of this biomarker with neoplastic progression.[11] A significant rise was also observed in the percentage of MN cells and micronuclei from control to precancer patients, and from precancer to cancer patients in a study by Saran et al.[12] In the present study, the mean number of micronuclei was higher in smokeless tobacco users indicating more genotoxic effect of smokeless tobacco as compared with smoking.
Conclusion
From the present study, increase in the number of micronuclei provides the evidence that smokeless tobacco chewers and smokers may be at a high risk for developing oral cancer. In comparison, the cellular changes associated with smokeless tobacco use were more than that in smokers, thus indicating more carcinogenic potential of smokeless tobacco. Micronucleus assay can be used as a biomarker of genotoxicity and epithelial carcinogenic progression. However, more research is required to establish it as a potential biomarker for oral carcinogenesis.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
References
- 1.Global cancer facts and figures. 2nd ed. Atlanta: American Cancer Society; 2011. International agency for research on cancer; pp. 1–57. [Google Scholar]
- 2.Jandoo T, Mehrotra R. Tobacco control in India: Present scenario and challenges ahead. Asian Pac J Cancer Prev. 2008;9:805–10. [PubMed] [Google Scholar]
- 3.Palaskar S, Jindal C. Evaluation of micronuclei using Papanicolaou and may Grunwald–Giemsa stain in individuals with different tobacco habits: a comparative study. J Clin Diagn Res. 2011;4:3607–13. [Google Scholar]
- 4.Halder A, Chakraborty T, Mandal K, Gure PK, Das S, Raychowdhury R, et al. Comparative study of exfoliated oral mucosal cell micronuclei frequency in normal, precancerous and malignant epithelium. Int J Hum Genet. 2004;4:257–60. [Google Scholar]
- 5.Jois HS, Kale AD, Mohan Kumar KP. Micronucleus as potential biomarker of oral carcinogenesis. Indian Journal of Dental Advancements. 2010;2:1–5. [Google Scholar]
- 6.Heddle JA, Hite M, Kirkhart B, Mavournin K, MacGregor JT, Newell GW, et al. The induction of micronuclei as a measure of genotoxicity. A report of the U.S. Environmental Protection Agency Gene-Tox Program. Mutat Res. 1983;123:61–118. doi: 10.1016/0165-1110(83)90047-7. [DOI] [PubMed] [Google Scholar]
- 7.Palve DH, Tupkari JV. Clinico-pathological correlation of micronuclei in oral squamous cell carcinoma by exfoliative cytology. J Oral Maxillofac Pathol. 2008;12:2–7. [Google Scholar]
- 8.Ramesh T, Ratnatunga N, Mendis BR, Rajapaksa S. Exfoliative cytology in screening for malignant and precancerous lesions in buccal mucosa. Ceylon Med J. 1998;43:206–9. [PubMed] [Google Scholar]
- 9.Ozkul Y, Donmez H, Erenmemisoglu A, Demirtas H, Imamoglu N. Induction of micronuclei by smokeless tobacco on buccal mucosa cells of habitual users. Mutagenesis. 1997;12:285–7. doi: 10.1093/mutage/12.4.285. [DOI] [PubMed] [Google Scholar]
- 10.Patel BP, Trivedi PJ, Brahmbhatt MM, Shukla SN, Shah PM, Bakshi SR. Micronuclei and chromosomal aberrations in healthy tobacco chewers and controls: A study from Gujrat, India. Arch Oncol. 2009;17:7–10. [Google Scholar]
- 11.Casartelli G, Bonatti S, De Ferrari M, Scala M, Mereu P, Marqarino G, et al. Micronucleus frequencies in exfoliated buccal cells in normal mucosa, precancerous lesions and squamous cell carcinoma. Anal Quant Cytol Histol. 2000;22:486–92. [PubMed] [Google Scholar]
- 12.Saran R, Tiwari RK, Reddy PP, Ahuja YR. Risk assessment of oral cancer in patients with pre-cancerous states of the oral cavity using micronucleus test and challenge assay. Oral Oncol. 2008;44:354–60. doi: 10.1016/j.oraloncology.2007.05.002. [DOI] [PubMed] [Google Scholar]