Abstract
Adenoid cystic carcinoma (ACC) of salivary glands is a slow-growing malignant tumor, characterized by wide local infiltration, perineural spread, a propensity to local recurrence and late distant metastasis. Although ACC is the second most common malignant salivary gland neoplasm and constitutes approximately one-third of all salivary gland malignancies, it is relatively rare in parotid gland. Here, we present a case report of a cribriform type of ACC involving parotid salivary gland in a 66-year-old female.
Keywords: Adenoid cystic carcinoma, cribriform pattern, parotid gland
Introduction
Adenoid cystic carcinoma (ACC) is a slow-growing, but aggressive neoplasm with a remarkable capacity for recurrence. It forms about 1% of all malignant tumors of the oral and maxillofacial region and 21.9% of all salivary gland malignancies.[1,2]
It can arise in any salivary gland site, but approximately 50–60% develops within the minor salivary glands. In the parotid gland, the ACC is relatively rare, constituting only 2–3% of all tumors.[3] Although it presents a widespread age distribution, peak incidence occurs predominantly among women, between the 5th and 6th decades of life.[4] It is clinically deceptive by virtue of its small size and slow growth, which belies its extensive subclinical invasion relentlessly into adjacent structures. ACC has three histopathologic patterns, viz., tubular, cribriform and a solid pattern. Solid pattern is associated with increased local recurrence, high metastatic rate and higher mortality.[5]
The treatment of ACC is chiefly surgical, although in some cases it has been successfully coupled along with X-ray radiation. ACC remains an extremely difficult disease to treat due to high predisposition for recurrence and metastasis if a patient lives long enough, and this occurs even when radical excision has been performed.[6]
Here, we report a case of ACC on the right side of the face, originating from parotid gland, in a 66-year-old woman.
Case Report
A 66-year-old, systemically healthy female patient presented with a complaint of pain and swelling on the right side of the face since 5–6 months. The patient reported a rapid increase in size of the lesion over the past 2 months.
Past dental history revealed that the patient had got her maxillary right first molar(16) extracted from some local dentist about 3 months ago.
Extraoral examination of the patient revealed an ill-defined swelling on the right side of the face in the superficial part of the parotid, with an intact surface, measuring approximately 3-4 cm in size, that caused an unilateral bulging of the canine fossa and zygomatic process with no facial nerve palsy [Figure 1]. The lesion was not fixed to the underlying bone and was entirely within the soft tissues of the right buccal mucosa.
Figure 1.

66-year-old female with ill-defined swelling on the right side of the face, appearing to be in the superficial part of the parotid
The nasolabial fold on the right side of the face was unobliterated. Right submandibular lymph node, less than 2 cm in size and oval in shape, was enlarged, palpable and minimally tender.
On intraoral clinical examination, an ovoid, firm, sessile nodule, measuring approximately 3 × 4 cm, in relation to 16 within the soft tissues of the right buccal mucosa was observed. The overlying mucosa was intact and normal in color with no signs of inflammation, ulceration or pus discharge.
Hematological investigations revealed a normal complete blood count, erythrocyte sedimentation rate, and blood chemistry.
Based on the patient's history and clinical examination associated with a rapid growth of the observed lesion, diagnosis of a malignant neoplasm was hypothesized and further investigations were carried out.
Plain and contrast-enhanced scans with axial and coronal sections revealed a heterogeneous enhancing soft tissue mass, measuring approximately 4 × 3 × 3 cm in size, seen in the parotid region on the right side of the face [Figure 2]. Erosion of the adjacent alveolar margin of the maxilla was noted. The mass was extending inferiorly in the buccal region adjacent to the mandible. No fat plane was seen separating the mass from the masseter muscle. There was no extension in the oral cavity. Minimal mucosal thickening was seen along the floor of the right maxillary sinus. The overall features were suggestive of a neoplastic lesion.
Figure 2.
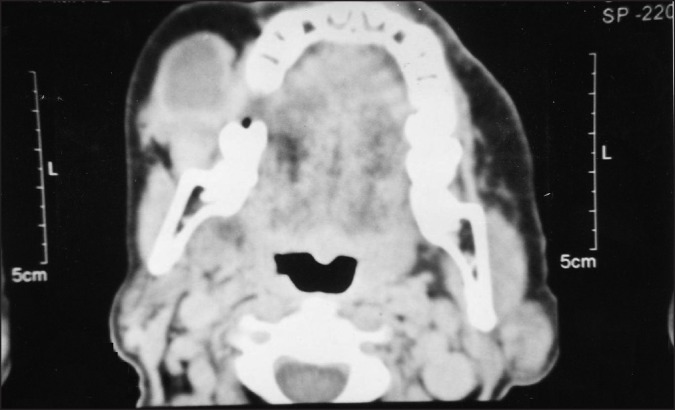
CT scan revealing a heterogeneous enhancing soft tissue mass measuring approximately 4 × 3 × 3 cm in size, seen in the parotid region on the right side of the face
Incisional biopsy was carried out and histopathologic analysis demonstrated a neoplastic proliferation of dark-staining epithelial cells with basophilic nuclei and scant cytoplasm enclosing circular spaces, arranged in a cribriform pattern. The lumina of few ductal structures contained a mucinous substance that was faintly eosinophilic. The hyalinized eosinophilic product was also seen surrounding these cribriform islands [Figure 3]. At the periphery, epithelial cells were arranged as single ductal structures formed by layers of isomorphic cells [Figure 4]. However, the cribriform pattern appeared to dominate, giving the entire structure a typical “swiss-cheese” appearance. The histopathologic impression was that of an ACC of cribriform pattern.
Figure 3.
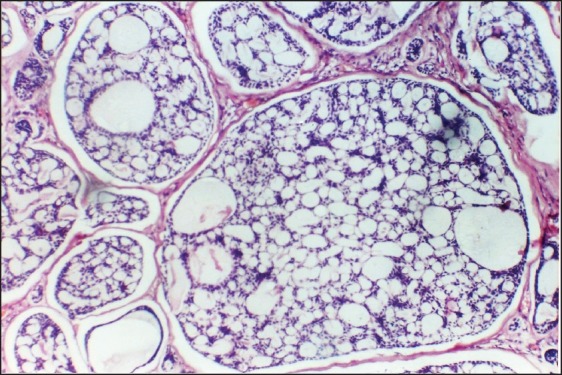
Photomicrograph demonstrating cribriform pattern(H&E, ×40)
Figure 4.
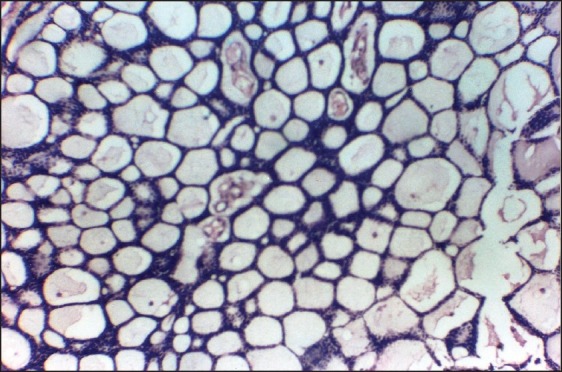
Photomicrograph demonstrating theductal pattern of adenoid cystic carcinoma, seen only at the periphery of the lesion (H&E, ×200)
Subsequently, the patient was referred to the Department of Oral and Maxillofacial Surgery, where she underwent a radical parotidectomy. Infraorbital nerve and masseter muscle were sacrificed and modified radical neck dissection was performed under general anesthesia after metastatic work up. 60 Gy adjuvant external beam radiotherapy with 2 Gy fractions was administered postoperatively to the parotid area and the neck.
No local recurrence of the lesion was observed 6 months after the treatment, during which time X-ray chest was repeated which revealed no pleural or parenchymal abnormalities.
Discussion
ACC is one of the common and best recognized salivary gland malignancies. The term “adenoid cystic carcinoma” was introduced by Ewing in 1954. This tumor was named as “cylindroma” earlier by Billroth in 1859 because the epithelial and connective tissue elements formed a system of intertwining cylinders. The term “basalioma” was coined by Krompecher in 1908, who considered this type of tumor to be of analogous nature to the basal cell growths of the skin.[7] It is a relentless tumor that is prone to local recurrence and eventual distant metastases .[3]
Evesson and Cawson[8] found a discrete predominance of ACC cases in women (F:M = 1.2:1) with age varying from 24 to 78 years. However, most occurrences took place in the 7th decade of life, with an average age of 66.3 years (+13.1). The presently described case agrees with the observations made by these authors regarding age and gender.
Clinically, it appears as a slow-growing mass with early local pain, facial nerve paralysis in the case of parotid tumors, fixity to deeper structures and local invasion.
Histologically, ACC is composed of a mixture of epithelial and ductal cells which are arranged in three characteristic patterns – cribriform, tubular and solid – with most tumors being composed of a mix of these.[9] Tumor nuclei are typically small, angulated and hyperchromatic with scanty cytoplasm. Mitotic figures are generally scarce in cribriform and tubular areas; however, they are easily visualized in solid standards that have been associated with the worst prognosis.[8]
The relationship between histological pattern and prognosis of ACC has been studied.[8] Huang et al. observed survival rates of 16.7% after a 10-year treatment for cases where solid variable was observed and 47.4% for lesions where cribriform and tubular standards were found. The authors concluded that the main factors associated with patient survival were tumor location, clinical stage and the observed histological variable.[5]
ACC has been histologically graded as follows:[10]
Grade I: The tumor consists only of cribriform and tubular histomorphology.
Grade II: A mixture of cribriform, tubular and solid growth patterns, with solid growth pattern less than 30% of the tumor.
Grade III: Tumors with predominantly solid features (>30% or more of the tumor).
In our case, the cribriform pattern was predominant while ductal or tubular pattern was less evident, hence it falls under the Grade I category.
Currently, stage and tumor location are the only factors considered prognostically significant.[11]
ACC may undergo dedifferentiation to a high-grade tumor with necrosis, a high mitotic rate and loss of the distinction between ductal and myoepithelial cells. In such cases, immunohistochemical markers like CD43, which are diagnostic for ACC, can be an adjuvant.[12] In our case, histological evaluation was diagnostic of cribriform pattern of ACC, which excludes the need for immunohistochemistry.
Distant metastasis is the most common presentation of treatment failure. The lung is by far the most common site of metastasis, with the liver being the second most common site. Bone metastases usually indicate a fulminant clinical course. Another unusual feature of ACC is that unlike most carcinomas, it seldom metastasizes to regional lymph nodes.
The cornerstone of treatment is surgery, while radiotherapy has been considered for advanced stages and as adjuvant in the presence of positive microscopic margins. A total conservative or a radical parotidectomy is advocated for tumors occurring in parotid, though the main intent is to obtain a tumor-free area of at least 1 cm.[13] Because metastasis to regional lymph nodes is uncommon, neck dissection is typically not indicated.[3] Some authors suggest that advanced and non-resectable tumors may be treated only with radiotherapy.
ACC has well-known prognosis profile. The 5-year survival rate after effective treatment is 75%, but long-term survival rates are low (10 years – 20% and 15 years – 10%). Postoperative radiotherapy combined with more aggressive surgeries increases the long-term survivals to 30–40% range. Clinical size greater than 4 cm indicates greater subclinical spread. Delayed diagnosis and delayed treatment also worsen the prognosis. Close or unclear surgical margins are indicators of the requirement of wider excision. Multiple local recurrences are also associated with grave prognosis.
Conclusion
ACC is a rare malignant tumor of the parotid gland. The primary treatment objective in ACC patients is local control, normal functionality and distant metastasis prevention. Metastasis can manifest very late, and hence a long-term follow-up and a high index of suspicion are necessary to diagnose it early in order to enable a more favorable prognosis and better quality of life.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
References
- 1.Kokemueller H, Eckardt A, Brachvogel P, Hausamen E. Adenoid cystic carcinoma of the head and neck: A 20 years experience. Int J Oral Maxillofac Surg. 2004;33:25–31. doi: 10.1054/ijom.2003.0448. [DOI] [PubMed] [Google Scholar]
- 2.Luo XL, Sun MY, Lu CT, Zhou ZH. The role of Schwann celldifferentiation in perineural invasion of adenoid cystic andmucoepidermoid carcinoma of the salivary glands. Int J Oral Maxillofac Surg. 2006;35:733–9. doi: 10.1016/j.ijom.2006.01.012. [DOI] [PubMed] [Google Scholar]
- 3.Neville, Damm, Allen, Bouquot . Oral and Maxillofacial Pathology. 2nd ed. pp. 426–8. [Google Scholar]
- 4.Waldron CA, El-Mofty SK, Gnepp DR. Tumors of the intraoral minor salivary glands: A demographic and histologic study of 426 cases. Oral Surg Oral Med Oral Pathol. 1988;66:323–33. doi: 10.1016/0030-4220(88)90240-x. [DOI] [PubMed] [Google Scholar]
- 5.Huang MX, Ma DQ, Sun KH, Yu GY, Guo CB, Gao F. Factors influencing survival rate in adenoid cystic carcinoma of the salivary glands. Int J Oral Maxillofac Surg. 1997;26:435–9. doi: 10.1016/s0901-5027(97)80008-2. [DOI] [PubMed] [Google Scholar]
- 6.Jones AS, Hamilton JW, Rowley H, Husband D, Helliwell TR. Adenoid cystic carcinoma of the head and neck. Clin Otolaryngol. 1997;22:434–43. doi: 10.1046/j.1365-2273.1997.00041.x. [DOI] [PubMed] [Google Scholar]
- 7.Lucas RB. Pathology of tumors of the oral tissues. 4th ed. pp. 330–5. [Google Scholar]
- 8.Eveson JW, Cawson RA. Tumours of the minor (oropharyngeal) salivary glands: A demographic study of 336 cases. J Oral Pathol. 1985;14:500–9. doi: 10.1111/j.1600-0714.1985.tb00522.x. [DOI] [PubMed] [Google Scholar]
- 9.Perez-Ordonez B. Selected topics in salivary gland tumour pathology. Curr Diagn Pathol. 2003;9:355–65. [Google Scholar]
- 10.Dardick I. Color atlas/text of salivary gland tumor pathology. :149–57. [Google Scholar]
- 11.Mendenhall WM, Morris CG, Amdur RJ, Werning JW, Hinerman RW, Villaret DB. Radiotherapy alone or combinated with surgery for adenoid cystic carcinoma of the head and neck. Head Neck. 2004;26:154–62. doi: 10.1002/hed.10380. [DOI] [PubMed] [Google Scholar]
- 12.Hotte SJ, Winquist EW, Lamont E, MacKenzie M, Vokes E, Chen EX, Brown S, Pond GR, Murgo A, Siu LL. Imatinib mesylate in patients with adenoid cystic cancers of the salivary glands expressing c-kit: a Princess Margaret Hospital phase II consortium study. J Clin Oncol. 2005 Jan 20;23:585–90. doi: 10.1200/JCO.2005.06.125. [DOI] [PubMed] [Google Scholar]
- 13.Marx RE, Stern D. Oral and maxillofacial pathology, A rational for diagnosis and management. :550–3. [Google Scholar]


