Abstract
Adrenal myelolipomas are functionally inactive, rare adrenal tumors which are usually small in size and are discovered incidentally. Giant symptomatic myelolipomas have rarely been reported in medical literature. Here, we describe the case of a 40-year-old female patient who presented to the surgical outpatient department with left flank pain. An ultrasonogram of the abdomen suggested a large retroperitoneal tumor which was then surgically resected. Histopathological examination of the resected specimen revealed a giant adrenal myelolipoma with intratumoral hemorrhage. The patient was relieved of symptoms and was free of any complaints in follow-up.
Keywords: Adrenal glands, giant myelolipoma, hemorrhage, sarcoma
INTRODUCTION
Adrenal myelolipomas are rare adrenal tumors and are composed of varying proportions of hematopoietic elements and adipose tissue. First described by Gierke in 1905, the term “myelolipoma” was coined by Oberling in 1929.[1] These benign tumors are functionally inactive, thus rarely causing any clinical problem. They usually measure less than 5 cm in diameter and are detected incidentally in autopsy or imaging studies done for other causes.[2] Hence, they are also loosely called “incidentalomas.” We present a case of a giant adrenal myelolipoma presenting with right flank pain and radiologically diagnosed as a retroperitoneal tumor.
CASE REPORT
A 40-year-old obese female patient presented to the outpatient department with complaint of severe right flank pain for the last 12 hours. On enquiry, she stated the she was suffering from a dull, dragging pain in the right flank for the last 3 months but did not seek any medical advice. On examination, the patient was overweight but appeared mildly pale. However, her pulse rate and blood pressure were stable. On palpation, a lump was felt in the right hypochondrium and lumber region which was tender in nature. She was admitted and routine blood tests, urine routine examination, chest X-ray, electrocardiography, and abdominal ultrasound were performed. The ultrasonogram revealed a large 14 × 10 cm hyperechoic mass with irregular margins below the liver which was pushing the right kidney down. A suspicion of retroperitoneal sarcoma with intralesional hemorrhage was made. The other tests were within normal limits. Serum cortisol, serum catecholamines, serum dopamine, urinary vanillylmandelic acid, 17-ketosteroid, and testosterone levels were done and the results were within normal levels. The patient complained of worsening pain and was operated. The resected specimen was sent for histopathological examination. Grossly the specimen measured 15 × 10 × 8 cm and weighed 1500 gm [Figure 1]. The outer surface was congested and the cut section showed mostly hemorrhage with some preserved yellowish areas. At the periphery there were some grayish areas. Multiple sections were taken from the tumor, routinely processed, stained, and microscopically examined. The sections revealed active hematopoietic elements composed of erythroid, myeloid cells, as well as megakaryocytes admixed with mature adipose tissue. The normal histology of adrenal glands was preserved at the periphery of the lesion [Figure 2]. A final diagnosis of giant adrenal myelolipoma with hemorrhage was made.
Figure 1.
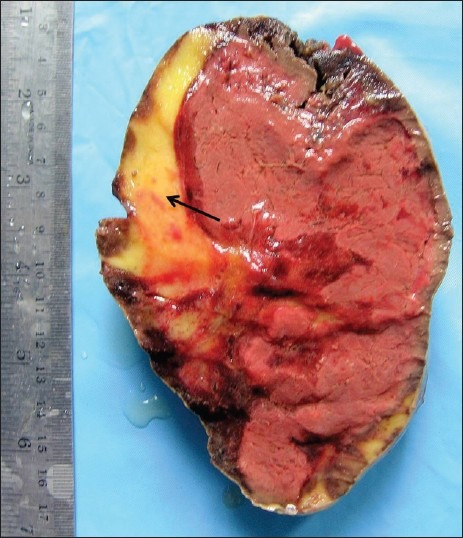
Photograph showing the gross specimen of giant adrenal myelolipoma with hemorrhage. The lipomatous component is seen in the periphery (black arrow)
Figure 2.
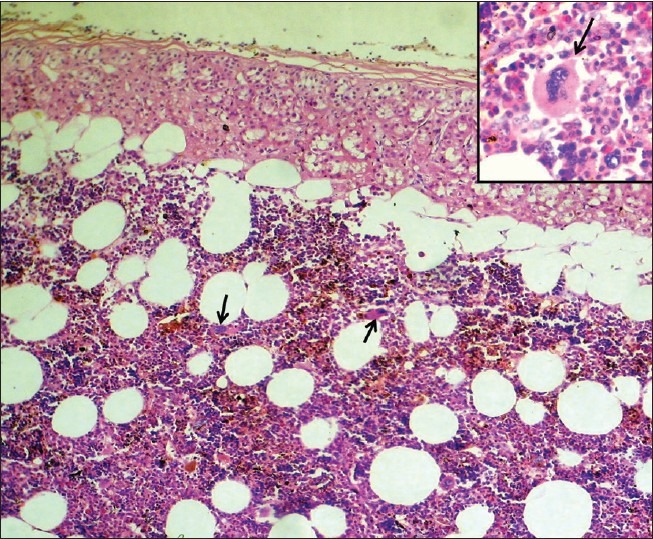
Microphotograph showing admixture of adipose tissue with hematopoietic elements. The preserved adrenal tissue is seen in the upper part of the tumor. (Hematoxylin and eosin stain, ×100 magnification). Inset shows high power view of a megakaryocyte in a background of myeloid and erythroid cells. (Hematoxylin and eosin stain, ×400 magnification). Megakaryocytes are highlighted with black arrows
DISCUSSION
Adrenal myelolipomas are rare tumors of adrenal gland which usually occurs in the 5th to 7th decade with no gender preference. These are usually unilateral tumors slightly more common in the right and rarely do they attain a size more than 5 cm.[3] The tumor, being a small, endocrinologically nonfunctional and benign one, rarely draws attention. They generally get noticed incidentally during imaging studies of abdomen or in autopsy (hence referred to as “incidentalomas”). Although cases of this tumor with associated hypertension, obesity, diabetes mellitus, and hematological abnormalities have been described, no cause–effect relationship is yet to be established. Again, coexistence with a functioning adrenal adenoma may result in endocrinal disturbances like Cushing syndrome, Conn syndrome, adrenogenital syndrome, or Addison's disease.[4,5] Giant adrenal myelolipomas are extremely rare tumors[4,5] with only about 10 reported cases.[6] Giant tumors may cause compressive symptoms and may present with abdominal and flank pain, palpable mass, or hematuria.[7] Presence of sudden intratumoral hemorrhage may cause intractable pain and even hemodynamic shock. Ultrasonography is a rapid and less expensive diagnostic modality showing hyperechoic image in lipid rich tumors while tumors with predominant myeloid elements appear hypoechoic. However, complicated cases may show irregular and infiltrative margins and even retroperitonal hemorrhage like the present one. These tumors show fat attenuation on computed tomography (CT) and are avascular at angiography. They show bright signal intensity in T1-weighted magnetic resonance (MR) images and intermediate signal intensity in T1-weighted MR images.[8] However, this appearance is nonspecific and may be confused with primary adrenal cancers or metastasis.[4] The present case was radiologically diagnosed as retroperitoneal sarcoma which is a common misinterpretation.[6,9] Histologically, extramedullary hematopoiesis is an important differential, the latter being usually associated with anemia, hepatosplenomegaly, bone marrow infiltration by lymphoma/leukemia cells, and often skeletal abnormalities. Treatment for nonfunctioning, asymptomatic myelolipomas < 5 cm is usually conservative with 6–12 monthly follow-up. Surgery is preferably reserved for symptomatic cases and in tumors > 10 cm, due to potential risk of malignant change and hemorrhagic complications.[4,10] Thus to conclude, we emphasize the consideration of this rare tumor as a differential diagnosis of other adrenal tumors as well as retroperitoneal tumors. The management of these tumors should be individualized with radiological follow-up for smaller tumors, while surgical resection is reserved for compressive effects or complications like hemorrhage.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Han M, Burnett AL, Fishman EK, Marshall FF. The natural history and treatment of adrenal myelolipoma. J Urol. 1997;157:1213–6. [PubMed] [Google Scholar]
- 2.Chakraborty J, Paul PCh, Gumta MK, Ghosh G, Goswami B. Adrenal myelolipoma–report of a case. J Indian Med Assoc. 2006;104:148–9. [PubMed] [Google Scholar]
- 3.Bhansali A, Dash RJ, Singh SK, Behra A, Singh P, Radotra BD. Adrenal Myelolipoma: Profile of six patients with a brief review of literature. Int J Endocrinol Metab. 2003;1:33–40. [Google Scholar]
- 4.Lin P, Yang F. Bilateral Giant Adrenal Myelolipomas: a case report and literature review. Chin J Radiol. 2008;33:261–4. [Google Scholar]
- 5.Wrightson WR, Hahm TX, Hutchinson JR, Cheadle W. Bilateral giant adrenal myelolipomas: a case report. Am Surg. 2002;68:588–9. [PubMed] [Google Scholar]
- 6.Fernandes GC, Gupta RK, Kandalkar BM. Giant adrenal myelolipoma. Indian J Pathol Microbiol. 2010;53:325–6. doi: 10.4103/0377-4929.64314. [DOI] [PubMed] [Google Scholar]
- 7.Patel VG, Babalola OA, Fortson JK, Weaver WL. Adrenal myelolipoma: report of a case and review of the literature. Am Surg. 2006;72:649–54. [PubMed] [Google Scholar]
- 8.Asch MR, Poon PY, McCallum RW, Bird BI. Myelolipoma: radiologic findings in seven patients. Can Assoc Radiol J. 1989;40:247–50. [PubMed] [Google Scholar]
- 9.Fernandez-Sanz J, Galera H, Garcia-Donas A, Gonzalez-Campora R, Llamas R, Matilla A. Adrenal myelolipoma simulating a retroperitoneal malignant neoplasm. J Urol. 1981;126:780–2. doi: 10.1016/s0022-5347(17)54746-1. [DOI] [PubMed] [Google Scholar]
- 10.Amendolara M, Barbarino C, Bucca D, Guarnieri F, Novello GB, Romano FM, et al. Giant and bilateral adrenal myelolipoma.Case report. G Chir. 2008;29:85–8. [PubMed] [Google Scholar]


