Abstract
Primary pulmonary sporotrichosis, a rare fungal disease was found in chronic alcoholic farmer from the sub-Himalayan region, an endemic mycoses area. Primary pulmonary sporotrichosis is a hidden entity, at times mimicking tuberculosis, and often under or lately diagnosed due to lack of awareness. We should consider the possibility of pulmonary sporotrichosis in patients with chronic cough and cavitary parenchymal disease, particularly in chronic alcoholics, gardeners, and forest workers. Sputum culture for fungus as a part of diagnostic studies is needed especially in endemic mycoses areas for early detection and management of such fungal diseases.
Keywords: Alcoholism, chronic cough, primary pulmonary sporotrichosis
INTRODUCTION
Pulmonary sporotrichosis is a rare clinical entity caused by the thermally dimorphic fungus Sporothrix schenckii.[1] Pulmonary sporotrichosis is usually a disseminated infection secondary to cutaneous sporotrichosis acquired by traumatic inoculation. Primary pulmonary sporotrichosis, acquired by inhalation of conidia of S. schenckii, often manifests as chronic cavitary fibronodular disease in middle-aged men who have underlying risk factors of alcoholism and chronic obstructive pulmonary disease.[2] The diagnosis of pulmonary sporotrichosis is usually established when bronchoalveolar lavage or sputum culture yields S. schenckii. We report a case of “primary” pulmonary sporotrichosis diagnosed incidentally, in a chronic alcoholic farmer from the sub-Himalayan region with no cutaneous manifestations.
CASE REPORT
A 22-year-old male farmer with history of chronic alcoholism had undergone surgery for duodenal perforation. The patient had complains of cough, breathlessness, and evening rise of temperature. There were no skin lesions or lymphadenopathy. Chest x-ray showed bilateral pleural effusion and pneumonitis; however, CT scan was advised to get more details of any underlying lung pathology. CT scan revealed single thin-walled cavitary lesion in lower-left lung [Figure 1]. Therefore, three consecutive sputum samples were sent for AFB microscopy and fungal microscopy and culture. His hemoglobin was 11.2 gm%, TLC was 7800/mm3 and DLC was P70, L27, E03. Sputum for AFB microscopy was negative.
Figure 1.
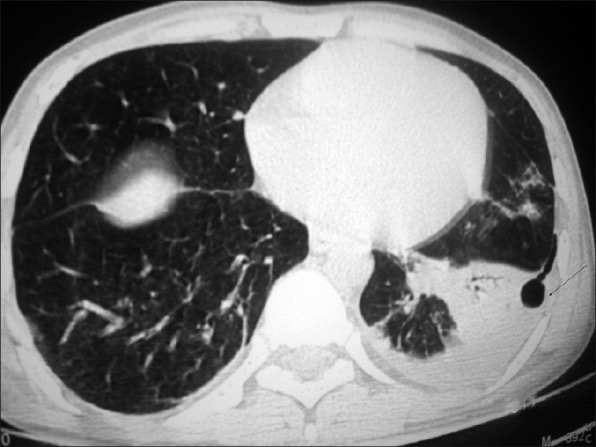
CT scan shows single thin-walled cavity in the lower-left lobe.
Fungal elements were seen on KOH preparation of three consecutive sputum specimens [Figure 2a]. Culture of the sputum specimens was done on Sabouraud's Dextrose Agar and incubated at 35°C and 25°C. The conversion of the mold to the yeast form occurred after 5 days. Definitive identification was made on the demonstration of typical microscopic mold morphology from culture at 25°C [Figure 2b] and cigar-shaped yeast cells at 35°C. The patient was advised itraconazole 200 mg orally twice daily as presentation was not life threatening. The patient has shown a favorable response after 1 month and is still being followed up.
Figure 2.
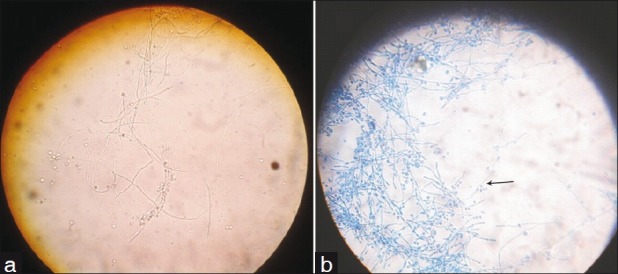
(a) KOH preparation of sputum shows fungal elements. (b) LCB mount of sputum culture shows septate hyphae with many pear-shaped to almost round conidia and forming rosette (arrow) on delicate sterigmata at 25°C.
DISCUSSION
Sporotrichosis, commonly known as rose gardener's disease, caused by S. schenckii, a dimorphic fungus, is an occupational hazard in gardeners and forestry workers that is acquired by minor trauma or inhalation.[3] S. schenckii, usually found in decaying vegetation, sphagnum moss, and soil leads to endemic mycoses. S. schenckii is endemic in the sub-Himalayan region, and commonly exists as mold in the environment.[4]
The cutaneous forms of sporotrichosis presenting as firm verrucose/ulcerative/erythematous nodules are the commonest presentations, but rare visceral forms (pulmonary, meningeal, osteoarticular, and disseminated) are other clinical presentations.[5] Rare manifestations of this disease should be sought in endemic mycoses areas such as ours. The pulmonary form can occasionally occur as primary infection after inhalation of conidia and is often fatal due to delay in diagnosis, such case has been once reported from India.[6] Pulmonary sporotrichosis usually presents as chronic cavitary fibronodular disease mimicking other causes of chronic necrotizing pneumonia.[2] However, rarely classic single thin-walled cavity can be seen associated with pulmonary sporotrichosis as found in our case.[2]
The direct examination of clinical specimens is difficult and rarely helpful to establish the diagnosis of sporotrichosis due to paucity of organism. Serological testing has little role in the diagnosis and is not readily available. Fungal culture of clinical specimens revealing typical dimorphic morphologies; mold form at 25°C and yeast form at 35°C, respectively, is the gold standard for confirmation of sporotrichosis. Primary pulmonary sporotrichosis in this case was confirmed by yield of characteristic dimorphic forms of S. schenckii on culture of three consecutive sputum specimens.
The drug of choice for patients with nonlife-threatening pulmonary sporotrichosis is itraconazole, while for life-threatening or extensive pulmonary lesions the drug of choice is amphotericin B, followed by itraconazole, after a favorable response is seen.[7] The diagnosis of pulmonary sporotrichosis was made early in the presented patient and only focal pulmonary lesions were present, therefore, itraconazole was prescribed.
Primary pulmonary sporotrichosis is hidden entity at times mimicking tuberculosis and is often under or lately diagnosed due to lack of awareness. We should consider the possibility of pulmonary sporotrichosis in patients with chronic cough and cavitary parenchymal disease, particularly in chronic alcoholics, gardeners, and forest workers. Sputum culture for fungus as a part of diagnostic studies is needed especially in endemic mycoses areas for early detection and management of such fungal diseases.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
REFERENCES
- 1.Mehta A, Budev MM, Ranes J, Shrestha R. Primary Pulmonary Sporotrichosis: A Case Report. Chest. 2004;126:945S. [Google Scholar]
- 2.Pluss JL, Opal SM. Pulmonary sporotrichosis: review of treatment and outcome. Medicine (Baltimore) 1986;65:143–53. [PubMed] [Google Scholar]
- 3.Rees RK, Swartzberg JE. Feline-transmitted Sporotrichosis: A case study from California. Dermatology Online J. 2011;17:2. [PubMed] [Google Scholar]
- 4.Agarwal S, Gopal K, Umesh, Kumar B. Sporotrichosis in Uttarakhand (India): a report of nine cases. Int J Dermatol. 2008;47:367–71. doi: 10.1111/j.1365-4632.2008.03538.x. [DOI] [PubMed] [Google Scholar]
- 5.Chander J. Textbook of Medical Mycology. 2nd ed. New Delhi: Mehta Publishers; 2002. Sporotrichosis. [Google Scholar]
- 6.Padhye AA, Kaufman L, Durry E, Banerjee CK, Jindal SK, Talwar P, et al. Fatal pulmonary sporotrichosis caused by Sporothrix schenckii var luriei in India. J Clin Microbiol. 1992;39:2492–4. doi: 10.1128/jcm.30.9.2492-2494.1992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kauffman CA, Bustamante B, Chapman SW, Pappas PG. Clinical Practice Guidelines for the Management of sporotrichosis: 2007 Update by the Infectious Diseases Society of America. Clin Infect Dis. 2007;45:1255–65. doi: 10.1086/522765. [DOI] [PubMed] [Google Scholar]


