Abstract
Background
Few studies have examined theoretically informed constructs related to hepatitis B (HBV) testing, and comparisons across studies is challenging due to lack of uniformity in constructs assessed. This analysis examines relationships among Health Behavior Framework factors across four Asian American groups to advance the development of theory-based interventions for HBV testing in at-risk populations.
Methods
Data were collected from 2007–2010 as part of baseline surveys during four intervention trials promoting HBV testing among Vietnamese-, Hmong-, Korean- and Cambodian-Americans (n = 1,735). Health Behavior Framework constructs assessed included: awareness of HBV, knowledge of transmission routes, perceived susceptibility, perceived severity, doctor recommendation, stigma of HBV infection, and perceived efficacy of testing. Within each group we assessed associations between our intermediate outcome of knowledge of HBV transmission and other constructs, to assess the concurrent validity of our model and instruments.
Results
While the absolute levels for Health Behavior Framework factors varied across groups, relationships between knowledge and other factors were generally consistent. This suggests similarities rather than differences with respect to posited drivers of HBV-related behavior.
Discussion
Our findings indicate that Health Behavior Framework constructs are applicable to diverse ethnic groups and provide preliminary evidence for the construct validity of the Health Behavior Framework.
Keywords: Health Behavior Framework, liver cancer control, HBV testing, Asian American, health behavior theory
Introduction
As many as two million people (Cohen et al., 2011) with chronic hepatitis B virus (HBV) infection live in the U.S., with Asian and Pacific Islanders making up the largest proportion of those infected (Lok and McMahon, 2009; Mast et al., 2006). Among Asian Americans, HBV accounts for 80% of liver cancer cases compared to 19% for non-Latino Whites (Hwang et al., 1996). Because of HBV infection, Asian Americans have much higher rates of liver cancer than non-Hispanic whites, making liver cancer the most important health disparity for Asian Americans (Chen, 2005). HBV testing can lead to earlier detection and hence potentially reduce the onset of serious sequelae of chronic liver disease. In addition, testing and, if indicated, vaccination can reduce HBV transmission (Weinbaum et al., 2009).
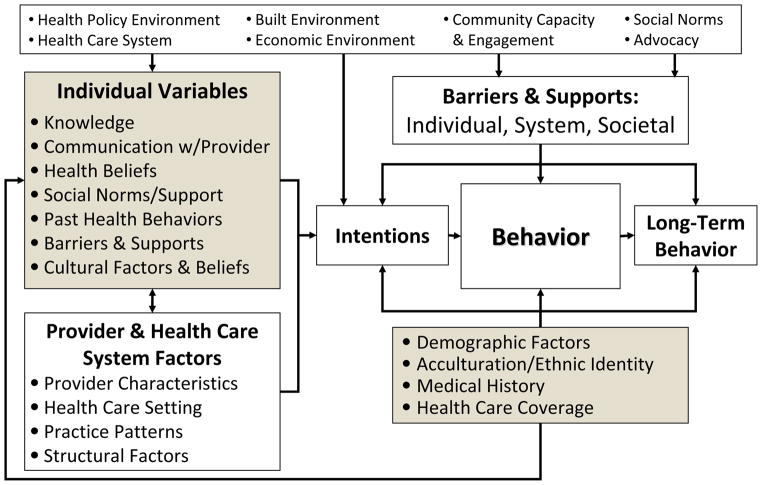
Studies conducted in Asian American populations have reported on various factors related to HBV testing and vaccination, such as knowledge, doctor recommendation, and demographics (Bastani et al., 2007; Choe et al., 2006; Hwang et al., 2008; Ma et al., 2007; Taylor et al., 2006; Wu et al., 2007). However, many studies have not been theory-guided, and because studies do not always assess the same theoretical constructs, comparing findings across studies is challenging. To facilitate a systematic examination of findings across studies and populations, we and others have advocated for the use of common conceptual frameworks for community-based intervention research (Bastani et al., 2010; Painter et al., 2008). The Health Behavior Framework (see Figure 1) is one such conceptual model and represents a synthesis of some of the major theoretical formulations in the area of health behavior (Bastani et al., 2010). We have used this conceptual model extensively in our prior work (Bastani et al., 1999; Bastani et al., 2004; Maxwell et al., 2010; Maxwell et al., 1998), and are currently using it in four intervention trials promoting HBV testing in four different Asian American populations (Nguyen et al., 2010; Taylor et al., 2011). All four trials utilized a common core questionnaire, based on the Health Behavior Framework, to assess hepatitis B knowledge, beliefs and barriers to testing as well as demographic information (Maxwell et al., 2010).
Figure 1.
Health Behavior Framework
The purpose of this paper is to examine the inter-relationships among a few constructs of the Health Behavior Framework across four population groups and in the context of four different intervention trials. We are interested in examining similarities and differences in these relationships across the four Asian American groups to advance health behavior theory and the development of programs to promote testing in these and other high risk populations. We rarely have the opportunity to compare findings in members of different Asian American groups who have all completed the same assessment instrument. We decided to examine correlates of knowledge of HBV transmission, because many studies have shown that knowledge is significantly associated with HBV testing (Bastani et al., 2007; Ma et al., 2008; Taylor et al., 2004; Taylor et al., 2008; Thompson et al., 2003; Wu et al., 2007).
Methods
Sampling and survey administration
Data for this analysis were collected during baseline surveys of four separate intervention trials among Vietnamese, Hmong, Korean and Cambodian communities in California, the Washington DC area, and Washington State in 2007–2010 (see Table 1). All four trials had the goal of increasing HBV testing among adults who had no prior history of testing (self-reported) for HBV. All aspects of the four trials, including sampling strategies, survey approach and incentives, and intervention approach and implementation were designed and conducted based on extensive community input. As outlined in Table 1, the Vietnamese study identified individuals using Vietnamese telephone surname lists (Nguyen et al., 2010) and the Hmong study sampled households from a list compiled through community and organizational contacts and telephone directories. Employing cluster sampling, the Korean study sampled Korean churches, and the Cambodian study sampled households using a Cambodian surname list (Taylor et al., 2011), and individuals were sampled within each cluster. All surveys included a common core questionnaire that assessed constructs from the Health Behavior Framework (Bastani et al., 2010; Maxwell et al., 2010). This core questionnaire was developed in English, Vietnamese, Hmong, Korean and Khmer.
Table 1.
Sampling and survey details of 4 community trials (2007–2010)
| Vietnamese | Hmong | Korean | Cambodian | |
|---|---|---|---|---|
| Eligibility criteria | 18–64 years old; Self-identified Vietnamese | 18–64 years old; Self-identified Hmong; Never tested for HBV | 18–64 years old; Self-identified Korean; Never tested for HBV | 18–64 years old; Self- identified Cambodian |
| Total number interviewed | 1,704 | 260 | 555 long interviews, 568 short interviews | 667 |
| Geographic Area | Northern California, Greater Washington, DC area | Greater Sacramento, CA Area (5 counties) | Los Angeles, CA | King County and South Snohomish County, Washington (Greater Seattle area) |
| Sampling Frame | Vietnamese surname list applied to telephone directories in geographic areas | Listing of Hmong households from community & organizational contacts and telephone directories | 179 Korean churches stratified by size & location | Households identified through Cambodian surname list applied to database of telephone listings; up to 1 man and 1 woman per household |
| Year of Survey | 2007–2008 | 2007–2010 | 2007–2010 | 2010 |
| Attempts to increase participation | Up to 15 telephone attempts | 2 public service announcements about the study via radio for one month in 2008 | Church bulletins, posters, staffed tables before and after church services | Introductory letter to household followed by up to 5 door to door attempts |
| Survey Medium | Telephone | In-person | In-person | In-person |
| Survey Language | 93% Vietnamese 7% English |
91% Hmong 9% English |
98% Korean 2% English |
75% Khmer 25% English |
| Duration | 24 minutes | 39 minutes** | 20–25 minutes | 30 minutes |
| Incentives | None | 25 lb bag of rice | $15 cash | $20 gift certificate |
| Cooperation Rate* | 63% | 59% | Churches: 36% Participants: 94% |
Households: 71% |
| IRB approval | University of California, San Francisco & San Francisco State University | University of California, Davis & University of California, San Francisco | University of California, Los Angeles | Fred Hutchinson Cancer Research Center |
Number completed/number of contacted and eligible
Length of visit, including height and weight measurement
Because the Hmong and Korean studies only recruited adults who had not been tested in the past, we restricted the analytical sample for this analysis to individuals who had never been tested. In addition, the Korean study administered the complete baseline survey only to a random half of the participants, resulting in the following sample sizes for this analysis: 653 Vietnamese, 260 Hmong, 493 Korean and 329 Cambodian.
Measures
Assessments focused on individual variables of the Health Behavior Framework (which are shaded in Figure 1) rather than on provider and health care system factors or broader socio-ecological factors, because the interventions in all 4 trials attempted to modify individual variables such as knowledge and health beliefs. We assessed the following Health Behavior Framework constructs: Demographic characteristics including length of residency in the United States and English fluency; access and use of health care (e.g., has health insurance, doctor’s visit during the past 12 months, see Table 2); awareness of hepatitis B, knowledge of seven potential transmission routes (sharing toothbrush, sharing food or eating utensils, coughing or sneezing, sexual intercourse, sharing needles, childbirth, spread by someone who looks and feels healthy), perceived susceptibility, perceived severity, doctor recommendation, stigma of HBV infection, and efficacy of testing (see items in Table 3). We created a summary score of knowledge of transmission by summing the number of correct responses to the seven knowledge items; “don’t know” responses were always considered incorrect.
Table 2.
Demographic characteristics for four study samples (2007–2010)
| Vietnamese | Hmong | Korean | Cambodian | |
|---|---|---|---|---|
| N=653 | N=260 | N=493 | N=329 | |
| % | % | % | % | |
| Gender | ||||
| Men | 44 | 40 | 35 | 48 |
| Women | 56 | 60 | 65 | 52 |
| Age | ||||
| 18–29 | 11 | 28 | 15 | 16 |
| 30–49 | 51 | 45 | 43 | 43 |
| 50–64 | 39 | 27 | 41 | 41 |
| Years in US | ||||
| ≤10 years | 19 | 38 | 38 | 11 |
| >10 years | 78 | 57 | 59 | 82 |
| US born | 3 | 6 | 3 | 7 |
| Marital Status | ||||
| Married or living as married | 72 | 72 | 73 | 72 |
| Education | ||||
| No formal education | 2 | 64 | 0 | 7 |
| Did not complete high school | 23 | 17 | 3 | 54 |
| High school graduate | 30 | 10 | 27 | 15 |
| Some college | 17 | 7 | 16 | 15 |
| College graduate | 29 | 3 | 54 | 8 |
| Annual household income | ||||
| <20,000 | 17 | 60 | 7 | 20 |
| 20–30,000 | 11 | 21 | 14 | 11 |
| 30–50,000 | 16 | 13 | 27 | 22 |
| >50,000 | 34 | 3 | 35 | 28 |
| Don’t know/Refused | 23 | 3 | 18 | 19 |
| Employment | ||||
| Employed | 71 | 28 | - | 66 |
| Unemployed | 29 | 72 | - | 34 |
| English fluency | ||||
| Fluently | 13 | 7 | 8 | 13 |
| Well | 19 | 9 | 12 | 9 |
| So-so | 44 | 20 | 52 | 41 |
| Poorly | 17 | 17 | 26 | 33 |
| Not at all | 7 | 47 | 3 | 5 |
| Has health insurance (yes) | 79 | 91 | 41 | 67 |
| Has place to go when sick/need advice | 67 | 78 | 48 | 75 |
| Saw a doctor during past 12 months | 60 | 62 | 51 | 63 |
| Saw a traditional healer/practitioner during past 12 months | 6 | 34 | 34 | 2 |
| Has family history of hepatitis B | 11 | - | 12 | 5 |
- = Not assessed
Table 3.
Health Behavior Framework Factors among 4 Asian American samples (2007–2010)
| Vietnamese | Hmong | Korean | Cambodian | |
|---|---|---|---|---|
| N=653 | N=260 | N=493 | N=329 | |
| Knowledge of Transmission Score | ||||
| Mean (Range 0–7) | 4 | 3.3 | 4.5 | 4.2 |
| Standard Deviation | 1.5 | 1.7 | 1.3 | 1.4 |
| % | % | % | % | |
| Awareness: Heard of Hepatitis B | 72 | 45 | 79 | 66 |
| Perceived susceptibility | ||||
| How likely do you think you are to get Hepatitis B during lifetime? | ||||
| Extremely/very likely | 13 | - | 2 | - |
| Somewhat likely | 27 | - | 59 | - |
| Not at all/not likely | 31 | - | 14 | - |
| Don’t know/RF | 29 | - | 24 | - |
| Which group is most likely to be infected? | ||||
| Hmong/Korean/Cambodian | - | 10 | 58 | 21 |
| White American | - | 5 | 5 | 8 |
| Both equally | - | 40 | 18 | 54 |
| Don’t know/RF | - | 45 | 20 | 17 |
| Perceived severity | ||||
| Do you think people can be infected for life? | ||||
| Y | 48 | - | 51 | 57 |
| N | 31 | - | 30 | 23 |
| DK/RF | 21 | - | 20 | 20 |
| Do you think Hepatitis B causes liver cancer? | ||||
| Y | 75 | 59 | 82 | 69 |
| N | 5 | 3 | 5 | 8 |
| DK/RF | 20 | 38 | 12 | 23 |
| Do you think there is treatment for Hep B? | ||||
| Y | 75 | - | 83 | 62 |
| N | 12 | - | 8 | 13 |
| DK/RF | 13 | - | 10 | 25 |
| Doctor recommendation (yes) | 17 | - | 3 | 19 |
| Stigma: People avoid people with Hep B | ||||
| Y | 38 | 55 | 47 | 70 |
| N | 47 | 17 | 41 | 23 |
| DK/RF | 14 | 28 | 12 | 7 |
| Efficacy of testing: Testing can prevent problems with liver | ||||
| Y | - | 68 | 94 | - |
| N | - | 8 | 2 | - |
| DK/RF | - | 23 | 4 | - |
- variables were not assessed
Statistical Analysis
Because the four samples were so different with respect to demographic characteristics and their immigration history, we did not make formal statistical comparisons across groups. Instead, we assessed the associations of our intermediate outcome of knowledge of HBV transmission with Health Behavior Framework constructs within each ethnic group. We compared the mean knowledge score across categories of each variable shown in Table 4, using analysis of variance for variables with more than two categories (age group and English fluency) and t-tests for binary variables (all others). In order to account for potential confounding, we created a separate multiple regression model of knowledge score as a function of each Health Behavior Framework construct, controlling for the seven demographic factors shown in Table 4. Additional analyses were performed for the Korean and Cambodian data using mixed effects models to account for clustering by church and by household, respectively. Because results were virtually identical when clustering and/or demographic factors were taken into account, only results from the simple bivariate analyses are presented.
Table 4.
Bivariate relationships between knowledge of hepatitis B virus (HBV) transmission and other Health
| Knowledge score | |||||
|---|---|---|---|---|---|
| Vietnamese | Hmong | Korean | Cambodian | ||
| (N=653) | (N=260) | (N=493) | (N=329) | ||
| Demographics/Background | Gender** | ||||
| Male | 4.0 + 1.5 | 3.6 ± 1.6* | 4.5 ± 1.4 | 4.4 ± 1.4* | |
| Female | 4.0 + 1.5 | 3.2 ± 1.7 | 4.4 ± 1.2 | 4.0 ± 1.3 | |
| Age (ANOVA - GLM)** | |||||
| 18–29 | 4.6 + 1.3* | 3.8 ± 1.6* | 4.9 ± 1.2* | 4.7 ± 1.4* | |
| 30–49 | 3.9 + 1.6 | 3.3 ± 1.6 | 4.5 ± 1.3 | 4.4 ± 1.2 | |
| 50–64 | 4.0 + 1.5 | 2.9 ± 2.0 | 4.3 ± 1.3 | 3.8 ± 1.4 | |
| Years in US** | |||||
| ≤10 years | 4.0 + 1.4 | 3.2 + 1.7 | 4.6 ± 1.3* | 3.8 ± 1.3 | |
| >10 years, US born | 4.0 + 1.5 | 3.4 + 1.7 | 4.4 ± 1.3 | 4.3 ± 1.4* | |
| Marital Status | |||||
| Married/Living as married | 4.0 + 1.5 | 3.3 + 1.7 | 4.4 ± 1.3 | 4.2 ± 1.3 | |
| Other | 4.1 + 1.6 | 3.5 + 1.7 | 4.7 ± 1.4* | 4.2 ± 1.5 | |
| Education** | |||||
| High | 4.3 ± 1.4* | 3.8 ± 1.6* | 4.5 ± 1.3 | 4.6 ± 1.4* | |
| Low | 3.8 ± 1.6 | 3.1 ± 1.7 | 4.4 ± 1.4 | 4.0 ± 1.3 | |
| Annual household income | |||||
| High | 4.3 ± 1.4* | 3.5 ± 1.7 | 4.5 ± 1.2 | 4.4 ± 1.4* | |
| Low | 4.0 ± 1.5 | 3.2 ± 1.7 | 4.4 ± 1.3 | 4.0 ± 1.3 | |
| Employment | |||||
| Employed | 4.0 + 1.4 | 3.4 ± 1.5 | - | 4.2 ± 1.3 | |
| Unemployed | 3.9 + 1.7 | 3.3 ± 1.8 | - | 4.3 ± 1.4 | |
| English fluency (ANOVA - GLM)** | |||||
| Fluently/Well | 4.3 ± 1.5* | 4.2 ± 1.4* | 4.6 ± 1.2* | 4.9 ± 1.3* | |
| So-so | 4.0 ± 1.4 | 3.4 ± 1.7 | 4.5 ± 1.3 | 4.2 ± 1.3 | |
| Poorly/Not at all | 3.7 ± 1.7 | 3.1 ± 1.7 | 4.2 ± 1.4 | 3.8 ± 1.3 | |
| Health insurance** | |||||
| Yes | 4.0 + 1.5 | 3.3 + 1.7 | 4.5 ± 1.3 | 4.2 ± 1.4 | |
| No/DK/RF | 4.1 + 1.6 | 3.8 ± 1.8 | 4.4 ± 1.3 | 4.2 ± 1.4 | |
| Saw a doctor in past 12 months** | |||||
| Yes | 4.0 ± 1.5 | 3.2 ± 1.7 | 4.5 ± 1.3 | 4.1 ± 1.4 | |
| No/DK/RF | 4.0 ± 1.5 | 3.5 ± 1.8 | 4.4 ± 1.3 | 4.3 ± 1.2 | |
| Family History of HepB | |||||
| Yes | 4.4 ± 1.3* | - | 4.3 ± 1.2 | 4.1 ± 1.6 | |
| No/DK/RF | 4.0 ± 1.5 | - | 4.5 ± 1.3 | 4.2 ± 1.4 | |
| Awareness | Heard of HBV | ||||
| Yes | 4.2 ± 1.4* | 3.6 ± 1.7 | 4.5 ± 1.2 | 4.4 ± 1.3* | |
| No/DK/RF | 3.5 ± 1.6 | 3.2 ± 1.7 | 4.2 ± 1.5 | 3.7 ± 1.4 | |
| Perceived susceptibility | Likely to get HB during lifetime | ||||
| High | 4.3 ± 1.3* | - | 4.6 ± 1.2* | - | |
| Low | 3.8 ± 1.6 | - | 4.2 ± 1.5 | - | |
| Group most likely to be infected | |||||
| Respondent’s ethnic group | - | 3.9 ± 1.3 | 4.6 ± 1.1* | 4.4 ± 1.4 | |
| Other/DK | - | 3.3 ± 1.7 | 4.3 ± 1.5 | 4.2 ± 1.3 | |
| Perceived severity | Can be infected for life | ||||
| Yes | 4.4 ± 1.4* | - | 4.5 ± 1.2 | 4.5 ± 1.1* | |
| No/DK/RF | 3.7 ± 1.5 | - | 4.4 ± 1.4 | 3.7 ± 1.5 | |
| HBV can cause liver cancer | |||||
| Yes | 4.2 ± 1.4* | 3.9 ± 1.4* | 4.4 ± 1.2 | 4.4 ± 1.2* | |
| No/DK/RF | 3.4 ± 1.7 | 2.5 ± 1.8 | 4.5 ± 1.5 | 3.6 ± 1.5 | |
| HBV can be treated | |||||
| No | 4.5 ± 1.6* | - | 4.6 ± 1.1 | 4.7 ± 1.3* | |
| Yes/DK/RF | 3.9 ± 1.5 | - | 4.4 ± 1.3 | 4.1 ± 1.4 | |
| Stigma | People avoid people with HBV | ||||
| Yes | 4.3 ± 1.3* | 3.7 ± 1.6* | 4.6 ± 1.1 | 4.3 ± 1.2* | |
| No/DK/RF | 3.8 ± 1.6 | 2.9 ± 1.7 | 4.4 ± 1.5 | 3.9 ± 1.6 | |
| Testing efficacy | Testing can prevent liver problems | ||||
| Yes | - | 3.6 ± 1.6* | 4.5 ± 1.3* | - | |
| No/DK/RF | - | 2.8 ± 1.7 | 3.8 ± 1.7 | - | |
Within each group, knowledge scores were significantly different p<0.05) and the highest knowledge score is bolded.
these factors were controlled for in the multivariate analysis (data not shown)
- not assessed
Categories of Health Behavior Framework variables were combined for bivariate analyses as shown in Table 4. The same categories were used for all four groups with the exception of education and income, which were categorized as high or low based on group-specific approximate medians.
Results
As shown in Table 2, the four Asian American groups varied with respect to many demographic characteristics. All groups were predominantly female (52–65%), immigrants (93–97%), and married (72%). The Hmong sample was the youngest and had the lowest levels of education, household income and English fluency, consistent with Census data. The Vietnamese and Cambodian samples had the highest proportions of long-term residents in the United States (>10 years). The Korean sample had the highest level of education, followed by Vietnamese. The Korean sample had the least access to health care based on health insurance and regular provider and about one-third of the Hmong and Korean, but very few Vietnamese and Cambodian saw a traditional healer during the past 12 months.
Awareness of hepatitis B varied considerably among the four groups, ranging from 45% of Hmong who had heard of hepatitis B to 79% of Korean Americans. Knowledge of specific transmission routes varied within and between the groups. The majority of respondents in all groups correctly identified sharing needles and child birth as transmission channels (67–95%). Only 43–69% knew that HBV can be transmitted during sexual intercourse. Large proportions in all four groups incorrectly thought that HBV can be transmitted by coughing or sneezing and by sharing food, drink, or eating utensils. The knowledge score ranged from 3.3 among Hmong to 4.5 among Korean Americans (on a scale of 0–7).
Perceived susceptibility was highest among Korean Americans and lowest among Hmong, based on two questions shown in Table 3. Perceived severity of hepatitis B varied considerably depending on the specific question that was asked. One question that was asked in all four studies “Do you think hepatitis B causes liver cancer?” was most often answered affirmatively by Korean Americans and least often by Hmong. As one might expect, only small proportions of respondents (who never had a HBV test per inclusion criteria for this analysis) reported receipt of a doctor’s recommendation to get tested for HBV in the 3 groups that were asked this question. Thirty-eight percent of Vietnamese, but 70% of Cambodian believed that people avoid people with HBV (stigma). Sixty-eight percent of Hmong but 94% of Koreans believed that testing was efficacious for preventing liver problems.
Bivariate relationships between the knowledge score and other Health Behavior Framework factors are shown in Table 4. Age was consistently related to knowledge scores and 18–29 year olds had the highest knowledge scores in each sample. Length of stay in the United States was not related to knowledge scores in the Vietnamese and Hmong samples, while higher knowledge scores were found among more recent Korean American immigrants and long-term Cambodian American immigrants. In three of the four samples, higher education was associated with higher knowledge scores, and English fluency was consistently positively related to knowledge scores in all four samples.
As expected, respondents who had heard of hepatitis B prior to this survey had higher knowledge scores than those who were not aware of hepatitis B in all four samples. Knowledge scores were consistently higher among respondents who expressed higher perceived susceptibility to getting infected with HBV. Higher perceived severity was also associated with higher knowledge scores, except in the Korean sample, which had the highest knowledge scores overall. Respondents with higher knowledge scores were more likely to agree that people avoid people with HBV (stigma). Those with higher knowledge scores were also more likely to agree that testing can prevent liver problems. Not all of these relationships were statistically significant and some of the differences we observed within samples were small (see Table 4).
These relationships were robust and did not change when we conducted analyses taking into account clustering in the Korean and the Cambodian sample. Additionally, the relationships between knowledge scores and other health beliefs (awareness, perceived susceptibility, severity, stigma, perceived efficacy of testing) did not change when we controlled for demographic characteristics within each sample, with one exception: After controlling for demographic characteristics in the Korean sample, the knowledge scores among people reporting stigma were significantly higher than among people who did not report stigma (data not shown).
Discussion
This paper adds to the literature because it examines relationships among theoretically based constructs related to HBV testing, among four Asian American populations who all completed a common core questionnaire. We found that the relationships between knowledge scores and demographic variables are generally consistent among the four samples included in our analysis and consistent with the literature, with higher knowledge scores among respondents with higher levels of education, income and English fluency (Bastani et al., 2007; Taylor et al., 2008; Taylor et al., 2002; Thompson et al., 2003). The relationships between knowledge scores and Hepatitis B awareness are also in the expected direction, with higher knowledge scores among those who had heard of Hepatitis B prior to the study.
Although our data are from cross-sectional surveys, which preclude causal inferences, we suspect that increased knowledge of HBV transmission routes and knowing that the virus can be transmitted by someone who looks and feels healthy may increase respondents’ perceived susceptibility. Those who are more knowledgeable about the transmission routes may also be more knowledgeable about other aspects of HBV infection, thereby increasing perceived severity and the belief in the efficacy of testing. Similarly, respondents with higher knowledge scores may be more aware of the stigma that is associated with HBV infection than respondents who know very little about the virus. The relationships that we found in the four samples between knowledge, perceived susceptibility, perceived severity, stigma and efficacy of testing are consistent with these assumptions. The fact that these relationships are in the expected directions and can easily be explained provides reassurance that items were correctly interpreted by respondents in all language groups.
The fact that the relationships between different constructs are quite consistent among the four Asian American groups suggests similarities rather than differences with respect to posited drivers of health behavior. Pending future research, this in turn suggests that interventions should attempt to influence similar beliefs across the four Asian American groups.
When comparing knowledge and health beliefs with respect to HBV testing across the four samples, despite all being Asian American, one has to keep in mind that the samples differ in demographic characteristics, most notably education and income, length of stay in the U.S., English fluency, and access to health care. Comparison of our Korean and Vietnamese samples with data from the population-based 2009 California Health Interview Survey (which was also conducted in Korean and Vietnamese languages) suggests that these samples reflect population characteristics (data not shown). Similar comparisons were not made for our Cambodian and Hmong samples since the CHIS does not administer surveys in those languages, and our Cambodian sample was not from California. However, the demographic characteristics of our Cambodian and Hmong samples generally agree with Census data for those populations. Our analyses are limited to individuals who had not been previously tested (based on self-report) for HBV and the four samples differed with respect to recruitment strategy and mode of survey administration. In addition, some items reported here were not administered to all groups. These differences are due to the population characteristics and the community input we received for all four trials, which influenced the study design and the assessment instruments.
CONCLUSION
While the absolute levels of Health Behavior Framework factors varied among the four ethnic groups, the relationships between knowledge of transmission routes of the HBV and other Health Behavior Framework factors are generally consistent across groups and in the direction predicted by our conceptual framework. This suggests that constructs of the Health Behavior Framework are applicable to diverse ethnic groups and that valid assessment tools can be developed for different groups based on the Health Behavior Framework. These findings provide preliminary evidence for the construct validity of the Health Behavior Framework.
Acknowledgments
The preparation of this article was funded in part through P01 CA109091-01A1 funded jointly by the National Cancer Institute and the National Institute on Minority Health and Health Disparities, National Cancer Institute grants U54 CA 153449 and 1R01CA134245, and the UCLA Kaiser Permanente Center for Health Equity.
Footnotes
Conflict of Interest
The authors declare that there are no conflicts of interest.
References
- Bastani R, Glenn BA, Maxwell AE, et al. Hepatitis B testing for liver cancer control among Korean Americans. Ethn Dis. 2007;17:365–73. [PubMed] [Google Scholar]
- Bastani R, Glenn BA, Taylor VM, et al. Integrating theory into community interventions to reduce liver cancer disparities: The Health Behavior Framework. Prev Med. 2010;50:63–7. doi: 10.1016/j.ypmed.2009.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bastani R, Maxwell AE, Bradford C, et al. Tailored risk notification for women with a family history of breast cancer. Prev Med. 1999;29:355–64. doi: 10.1006/pmed.1999.0556. [DOI] [PubMed] [Google Scholar]
- Bastani R, Yabroff KR, Myers RE, et al. Interventions to improve follow-up of abnormal findings in cancer screening. Cancer. 2004;101:1188–200. doi: 10.1002/cncr.20506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen MS., Jr Cancer health disparities among Asian Americans: what we do and what we need to do. Cancer. 2005;104:2895–902. doi: 10.1002/cncr.21501. [DOI] [PubMed] [Google Scholar]
- Choe JH, Taylor VM, Yasui Y, et al. Health care access and sociodemographic factors associated with hepatitis B testing in Vietnamese American men. J Immigr Minor Health. 2006;8:193–201. doi: 10.1007/s10903-006-9322-1. [DOI] [PubMed] [Google Scholar]
- Cohen C, Holmberg SD, McMahon BJ, et al. Is chronic hepatitis B being undertreated in the United States? J Viral Hepat. 2011;18:377–83. doi: 10.1111/j.1365-2893.2010.01401.x. [DOI] [PubMed] [Google Scholar]
- Hwang JP, Huang CH, Yi JK. Knowledge about hepatitis B and predictors of hepatitis B vaccination among Vietnamese American college students. J Am Coll Health. 2008;56:377–82. doi: 10.3200/JACH.56.44.377-382. [DOI] [PubMed] [Google Scholar]
- Hwang SJ, Tong MJ, Lai PP, et al. Evaluation of hepatitis B and C viral markers: clinical significance in Asian and Caucasian patients with hepatocellular carcinoma in the United States of America. Journal of Gastroenterology and Hepatology. 1996;11:949–54. [PubMed] [Google Scholar]
- Lok AS, McMahon BJ. Chronic hepatitis B: update 2009. Hepatology. 2009;50:661–2. doi: 10.1002/hep.23190. [DOI] [PubMed] [Google Scholar]
- Ma GX, Shive SE, Fang CY, et al. Knowledge, attitudes, and behaviors of hepatitis B screening and vaccination and liver cancer risks among Vietnamese Americans. J Health Care Poor Underserved. 2007;18:62–73. doi: 10.1353/hpu.2007.0013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ma GX, Shive SE, Toubbeh JI, et al. Knowledge, attitudes, and behaviors of Chinese hepatitis B screening and vaccination. Am J Health Behav. 2008;32:178–87. doi: 10.5555/ajhb.2008.32.2.178. [DOI] [PubMed] [Google Scholar]
- Mast EE, Weinbaum CM, Fiore AE, et al. A comprehensive immunization strategy to eliminate transmission of hepatitis B virus infection in the United States: recommendations of the Advisory Committee on Immunization Practices (ACIP) Part II: immunization of adults. MMWR Recomm Rep. 2006;55:1–33. quiz CE1-4. [PubMed] [Google Scholar]
- Maxwell AE, Bastani R, Chen MS, Jr, et al. Constructing a theoretically based set of measures for liver cancer control research studies. Prev Med. 2010;50:68–73. doi: 10.1016/j.ypmed.2009.10.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maxwell AE, Bastani R, Danao LL, et al. Results of a community-based randomized trial to increase colorectal cancer screening among Filipino Americans. Am J Public Health. 2010;100:2228–34. doi: 10.2105/AJPH.2009.176230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maxwell AE, Bastani R, Warda US. Mammography utilization and related attitudes among Korean-American women. Women Health. 1998;27:89–107. doi: 10.1300/J013v27n03_07. [DOI] [PubMed] [Google Scholar]
- Nguyen TT, McPhee SJ, Stewart S, et al. Factors associated with hepatitis B testing among Vietnamese Americans. J Gen Intern Med. 2010;25:694–700. doi: 10.1007/s11606-010-1285-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Painter JE, Borba CP, Hynes M, et al. The use of theory in health behavior research from 2000 to 2005: a systematic review. Ann Behav Med. 2008;35:358–62. doi: 10.1007/s12160-008-9042-y. [DOI] [PubMed] [Google Scholar]
- Taylor V, Yasui Y, Burke N, et al. Hepatitis B testing among Vietnamese American men. Cancer Detect and Prevention. 2004;28:170–177. doi: 10.1016/j.cdp.2004.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor VM, Bastani R, Burke N, et al. Factors Associated with Hepatitis B Testing Among Cambodian American Men and Women. J Immigr Minor Health. 2011 doi: 10.1007/s10903-011-9536-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor VM, Coronado G, Acorda E, et al. Development of an ESL curriculum to educate Chinese immigrants about hepatitis B. J Community Health. 2008;33:217–24. doi: 10.1007/s10900-008-9084-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor VM, Jackson JC, Chan N, et al. Hepatitis B knowledge and practices among Cambodian American women in Seattle, Washington. J Community Health. 2002;27:151–63. doi: 10.1023/a:1015229405765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor VM, Talbot J, Do HH, et al. Hepatitis B Knowledge and Practices among Cambodian Americans. Asian Pac J Cancer Prev. 2011;12:957–61. [PMC free article] [PubMed] [Google Scholar]
- Taylor VM, Tu SP, Woodall E, et al. Hepatitis B knowledge and practices among Chinese immigrants to the United States. Asian Pac J Cancer Prev. 2006;7:313–7. [PubMed] [Google Scholar]
- Thompson MJ, Taylor VM, Yasui Y, et al. Hepatitis B knowledge and practices among Chinese Canadian women in Vancouver, British Columbia. Can J Public Health. 2003;94:281–6. doi: 10.1007/BF03403606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weinbaum CM, Mast EE, Ward JW. Recommendations for identification and public health management of persons with chronic hepatitis B virus infection. Hepatology. 2009;49:S35–44. doi: 10.1002/hep.22882. [DOI] [PubMed] [Google Scholar]
- Wu CA, Lin SY, So SK, et al. Hepatitis B and liver cancer knowledge and preventive practices among Asian Americans in the San Francisco Bay Area, California. Asian Pac J Cancer Prev. 2007;8:127–34. [PubMed] [Google Scholar]