Abstract
Background
Infective spondylodiscitis usually occurs in patients of older age, immunocompromisation, co-morbidity, and individuals suffering from an overall poor general condition unable to undergo reconstructive anterior and posterior surgeries. Therefore, an alternative, less aggressive surgical method is needed for these select cases of infective spondylodiscitis. This retrospective clinical case series reports our novel surgical technique for the treatment of infective spondylodiscitis.
Methods
Between January 2005 and July 2011, among 48 patients who were diagnosed with pyogenic lumbar spondylodiscitis or tuberculosis lumbar spondylodiscitis, 10 patients (7 males and 3 females; 68 years and 48 to 78 years, respectively) underwent transpedicular curettage and drainage. The mean postoperative follow-up period was 29 months (range, 7 to 61 months). The pedicle screws were inserted to the adjacent healthy vertebrae in the usual manner. After insertion of pedicle screws, the drainage pedicle holes were made through pedicles of infected vertebra(e) in order to prevent possible seeding of infective emboli to the healthy vertebra, as the same instruments and utensils are used for both pedicle screws and the drainage holes. A minimum of 15,000 mL of sterilized normal saline was used for continuous irrigation through the pedicular pathways until the drained fluid looked clear.
Results
All patients' symptoms and inflammatory markers significantly improved clinically between postoperative 2 weeks and postoperative 3 months, and they were satisfied with their clinical results. Radiologically, all patients reached the spontaneous fusion between infected vertebrae and 3 patients had the screw pulled-out but they were clinically tolerable.
Conclusions
We suggest that our method of transpedicular curettage and drainage is a useful technique in regards to the treatment of infectious spondylodiscitic patients, who could not tolerate conventional combined anterior and posterior surgery due to multiple co-morbidities, multiple level infectious lesions and poor general condition.
Keywords: Spondylodiscitis, Curettage, Drainage, Surgery, Transpedicular
Infective spondylitis involves mainly the vertebral body and sometimes adjacent disc space.1) Standard treatment includes administration of sensitive antimicrobial agents, after proper identification of the organism, and external mechanical support.1-5) However, in cases non-responsive to medical treatment, further collapse of the vertebral body and newly developed neurologic symptoms necessitate prompt surgical treatment.6-8) Classical surgery was a corpectomy, an anterior strut bone graft with or without posterior instrumentation.9-12)
Infective spondylodiscitis usually occurs in patients of older age, immunocompromisation, co-morbidity, and individuals suffering from an overall poor general condition unable to undergo reconstructive anterior and posterior surgeries.2,13-15) Therefore, an alternative, less aggressive surgical method is needed for these selected cases of infective spondylodiscitis.
That being said, surgical techniques, which should comprise treatment principles of osteomyelitis, although less aggressive, must be developed. Treatment principles can be drainage, curettage of the infected bone and sound mechanical support.2,16) A transpedicular approach is widely used for biopsy of the vertebral body and cement augmentation in osteoporotic vertebral fractures.17,18) A pedicular screw system also provides sufficient mechanical support when applied to a healthy vertebral column.19)
By adopting the two above-mentioned techniques, the transpedicular approach and the pedicular screw fixation system, a novel surgical technique was developed, called transpedicular drainage and curettage with posterior instrumentation for infective spondylodiscitis. This technique not only provides a less aggressive approach without the necessity of an anterior approach and bone harvesting but also sufficient drainage and curettage of the infected vertebral body and posterior mechanical support. Hence, in the present study, the detailed surgical technique and its clinical results were demonstrated.
METHODS
Between January 2005 and July 2011, 48 patients diagnosed with pyogenic or tuberculosis lumbar spondylodiscitis were enrolled. To reflect the friable conditions of enrolled patients, only spontaneous spondylodiscitis patents were enrolled except iatrogenic spondylodiscitis. Failure of conservative treatments was considered when erythrocyte sedimentation rate (ESR), C-reactive protein (CRP) and pain severity did not decrease for more than 2 weeks, in spite of intravenous antibiotics administration. Indications regarding these surgical procedures basically met the classical surgical indications including 1) intolerable back and/or radiating pain caused by infective spondylodiscitis, 2) progressive neurologic deficit due to the formations of an epidural abscess, 3) for histologic biopsy to confirm the pathogen. However, when patients were thought to be intolerable to the conventional classical anterior and posterior combined surgery due to the patients' poor general condition, these transpedicular curettage and drainage procedures were applied preferentially when no significant structural destruction necessitating the anterior structural reconstruction existed. Finally, ten patients (7 males and 3 females; 68 years and 48 to 78 years, respectively), who were considered to be intolerable underwent novel transpedicular curettage and drainage. The mean postoperative follow-up period was 29 months (range, 7 to 61 months).
Electronic medical records of the patients were reviewed thoroughly. In all cases, standard serologic tests including white blood cell counts, ESR, CRP, and blood chemistry profiles were conducted on a weekly basis. Radiographic studies including plain X-rays of the afflicted spine area, computed tomography (CT), whole body bone scan (WBBS), and magnetic resonance image (MRI) were performed. In most of the patients, empirical antibiotics were started with initial diagnoses of infective spondylitis. All statistical analyses such as the Friedman test were performed by using the SPSS ver. 12.0.1 (SPSS Inc., Chicago, IL, USA).
Surgical Technique
After general endotracheal anesthesia, patient was turned prone on a table (Jackson Spinal Table System, Osi, Union City, CA, USA), and all pressure points were carefully padded. The whole back and upper buttocks was prepared and draped in the usual sterile orthopedic manner. A skin incision was made over the posterior midline of the designated lumbar vertebrae level longitudinally. The dissection was progressed as a conventional method with level confirmation by a portable lateral X-ray until bilateral transverse processes were exposed partially as a landmark of the pedicle entry point.
Although the transpedicular approach technique is not quite a challenging task, all radiographic studies were preoperatively reviewed in order to select an appropriate approach in regards to the most effective pedicle entrances and pathways for drainage. The convergence and the lordotic angle along the pedicle could be slightly modified to ensure effective curettage and drainage. After dissection to expose the vertebra, we usually confirmed the proper entry points, using the K-wire guidance technique.20) The K-wire was inserted to the pedicle on the planned pedicle screw insertion level of the vertebrae. Additionally, extra K-wires were inserted to the pedicle of the infected vertebra(e) in order to confirm the appropriate drainage pathway. Then a single series of posterior and lateral radiographs were taken to ensure the proper location of the K-wire. Next, the pedicle screws were inserted to healthy vertebrae. After insertion of pedicle screws, the drainage pedicle holes were made on the infected vertebra(e) in order to prevent the possible seeding of infection or emboli to the healthy vertebra, as the same instruments and utensils are used for both pedicle screws and the drainage holes. The pedicle drainage hole widening procedure including curettage with a pedicle screw tapper and curette was added. At least 15,000 mL of sterilized normal saline was used for continuous irrigation through the pedicular pathways until the drained fluid looked clear using a various sized nelatone catheter, 24 gauge spinal needled syringes and a T shape handled pedicular bone biopsy set to secure the direction of irrigation flow (Figs. 1-4). Depending on the presence of an epidural abscess causing neurologic deficits and co-existing spinal stenosis, additional decompression procedures including laminectomy, flavectomy and/or pediculectomy can be applied. Afterwards, 2 rods, which were bent laterally to facilitate pedicular drainage, were assembled to pedicle screws. After additional copious irrigation and meticulous hemostasis, the operative wound was closed layer-by-layer leaving two wings of a hemovac drain into the main drain site bilaterally. The hemovac was not removed until the amount of postoperative drainage was less than 30 mL to encourage drainage of the remaining unhealthy discharge from the infected vertebra(e).
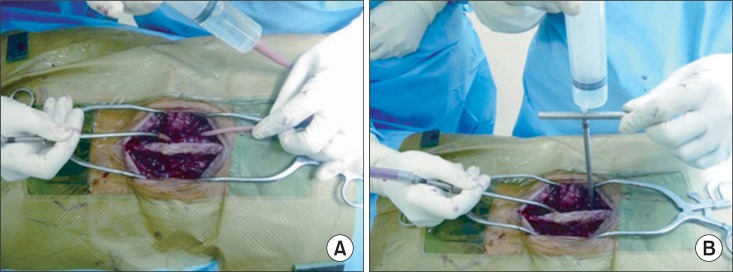
Fig. 1.
(A, B) The various sized nelatone catheter, 24 gauge spinal needled syringes, and the T shape handled pedicular bone biopsy set could be used to secure the direction of irrigation flow.
Fig. 4.
The rods were assembled to the pedicular screws in a lateral bent form to encourage the remnant infective drainage through the punched pedicles.
RESULTS
Total hospitalization was for 44.3 days (range, 16 to 100 days) including 19.9 days (range, 14 to 34 days) of postoperative hospitalization. Hemovac suction drain was removed between postoperative 7 and 18 days. Ambulation while wearing a body-pit hard brace was encouraged at postoperative 4.9 days (range, 3 to 10 days). All patients' symptoms markedly improved clinically between postoperative 2 weeks and postoperative 3 months and they were satisfied with their clinical results.
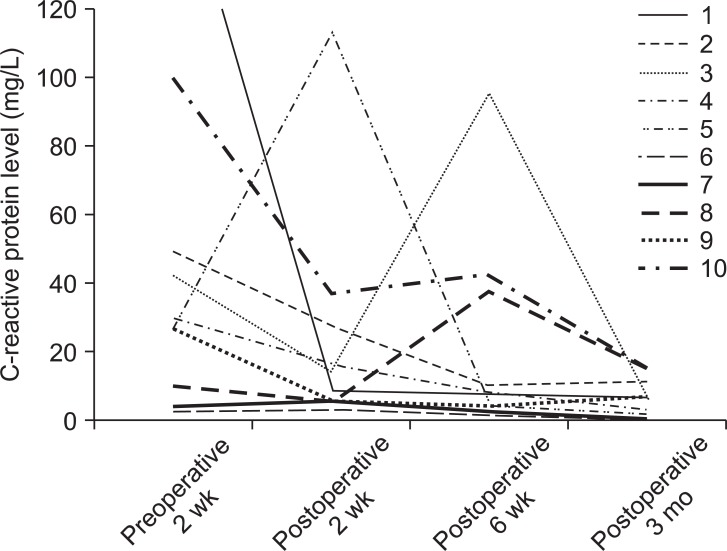
Two patients had postoperative morbidities including postoperative delirium and postoperative arrhythmia. The pulling-out of a pedicle screw at the distal segment was detected during an outpatient clinic follow-up in one patient due to poor osteoporotic bone quality. However, no additional surgical procedure was required. Other data are shown in Table 1. CRP reduced significantly after operation (Table 2, Fig. 5). Serial improvement on MRI and spontaneous fusion of infective vertebrae regarding case no. 9 was shown in Figs. 6 and 7.
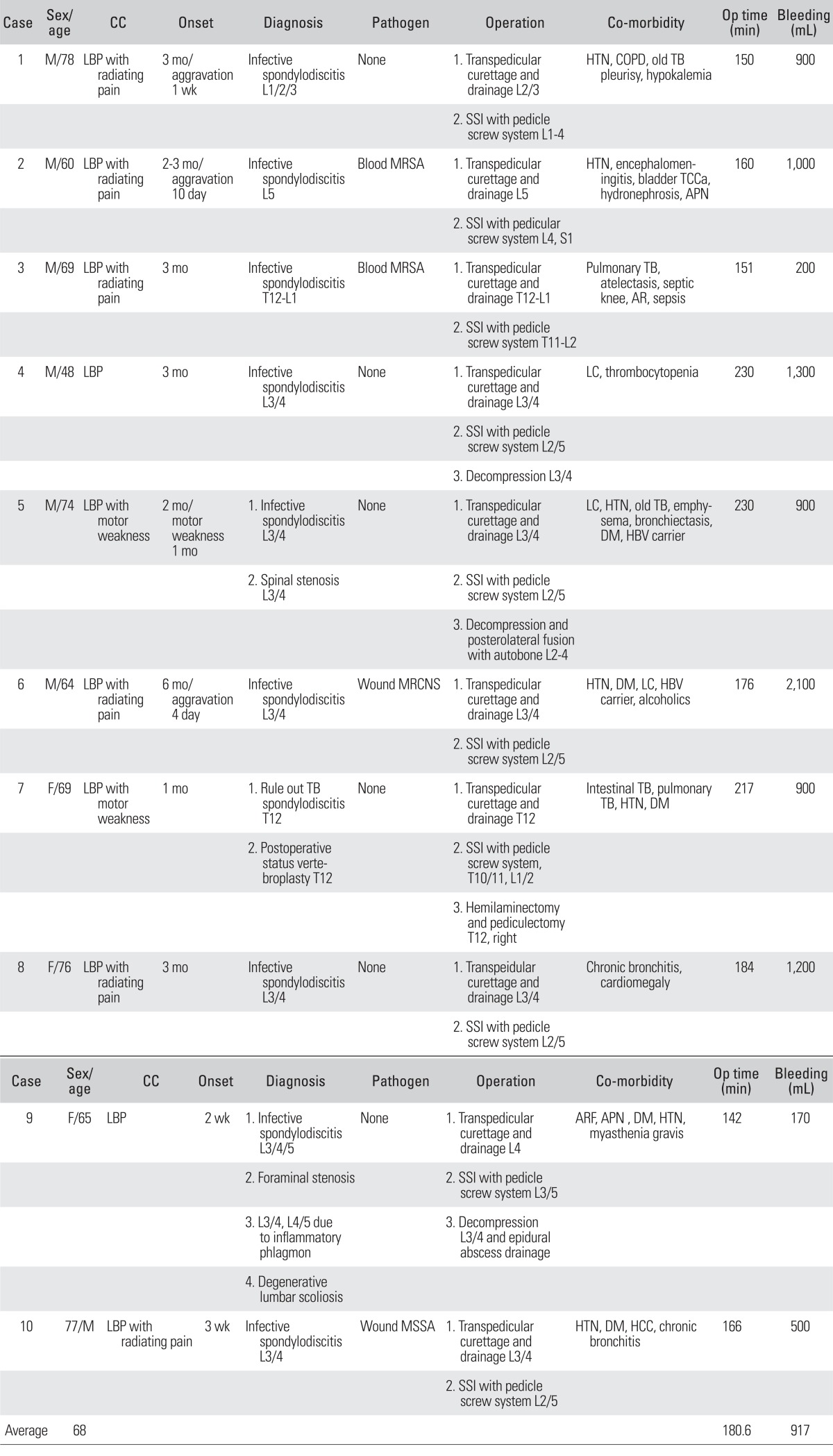
Table 1.
Demographics and Characteristics of Enrolled Patients
CC: chief complaint, Op: operation, LBP: low back pain, HTN: hypertension, COPD: chronic obstructive lung disease, TB: tuberculosis, SSI: spinal segmental instrumentation, MRSA: methicillin resistant staphylococcus aureus, TCCa: transitional cell cancer, APN: acute pyelonephritis, AR: aortic regurgitation, LC: liver cirrhosis, DM: diabetes mellitus, HBV: hepatitis B virus, MRCNS: methicillin resistant coagulase negative streptococcus, ARF: acute renal failure, MSSA: methicillin sensitive staphylococcus aureus, HCC: hepatocellular carcinoma.
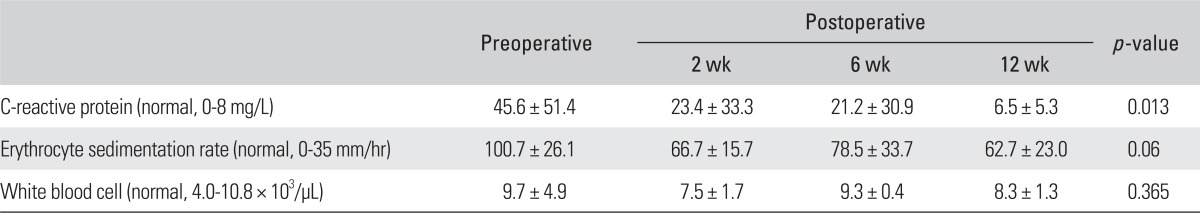
Table 2.
Serologic Inflammatory Marker Changes after Surgery
Statistical analysis by Friedman test, p < 0.05 considered statistically significant.
Fig. 5.
C-reactive proteins were normalized or reduced to the level of upper normal limits until postoperative 3 months (p = 0.013, Friedman test).
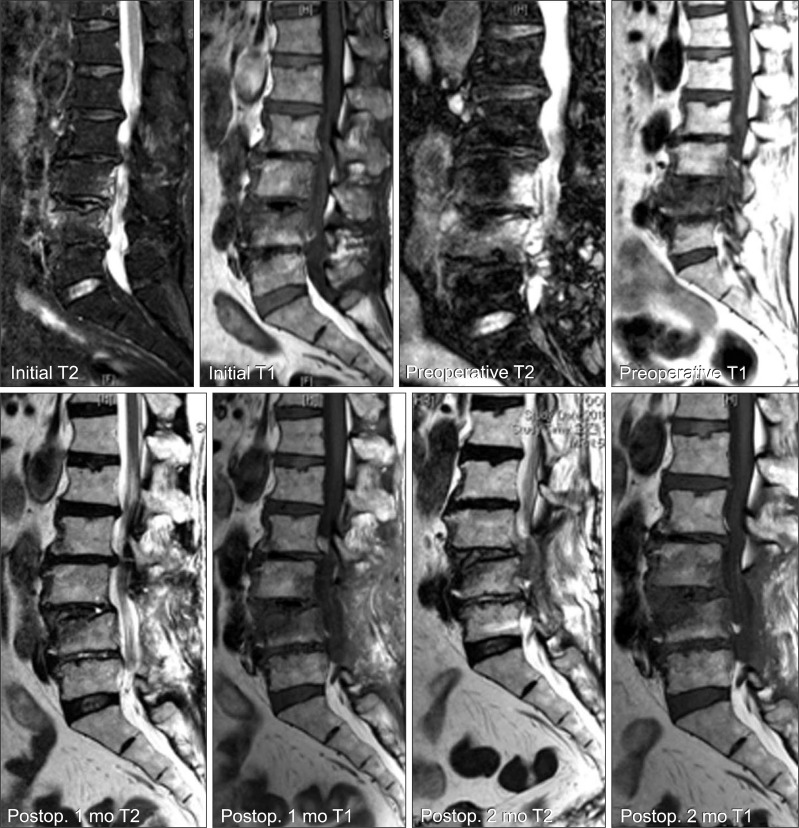
Fig. 6.
A 65-year-old female (case 9) treated conservatively with intravenous antibiotics. However, her symptoms and serologic tests worsened for 1 month. She underwent transpedicular curettage and drainage and was markedly better on postoperative 1-month magnetic resonance image. At postoperative 3 months, her serologic tests were improved to the normal limit level.
Fig. 7.
Preoperative X-rays (A, B) of case 9 show spontaneous fusion of the infective vertebrae without implant failure at postoperative 6 months (C, D).
Radiologically, all patients reached the spontaneous fusion between the infected vertebrae and 3 patients had the screw pulled-out but they were clinically tolerable and did not complaint of those related symptoms. One patient (case no. 4) was re-admitted for administration of intravenous antibiotics after hospital discharge, because a fever had developed again. After an additional 2 weeks of parenteral antibiotics therapy, he left the hospital without any other pyretic event. Only two patients had positive results of vertebral wound culture with methicillin resistant coagulase negative streptococcus and methicillin sensitive staphylococcus aureus. The others all reported negative vertebral wound cultures, but two patients had positive blood cultures with methicillin resistant staphylococcus aureus. Parenteral antibiotics such as 1st and 3rd generation cephalosporin, vancomycin, and aminoglycoside depending on the pathogen were used for 30 days (range, 0 to 106 days) preoperatively and 21.3 days (range, 2 to 33 days) postoperatively. Oral antibiotics of 3rd generation cephalosporin were administered for 40.6 days (range, 14 to 105 days) postoperatively after discharge.
DISCUSSION
In infectious spondylodiscitis, transpedicular curettage and drainage is recommended for patients who have multiple co-morbidities, poor general condition, and who are unable to undergo complex surgery. In this study, patients with multiple vertebral lesions had at least two to nine co-morbidities. Among current surgical treatments for infectious spondylodiscitis, posterior decompression and fusion with or without posterior instrumentation, in which anterior debridement is omitted, can be used for patients with poor general condition and with paralysis due to posterior compression by an extradural abscess.10,21) Also, transpedicular curettage and drainage to the established posterior operation procedure were added to the conventional treatment. Curettage, histologic biopsy, pathogen culture, and direct drainage of infective discharge are possible through the current novel procedure.
It has been reported that clinical and radiological outcomes were poor if anterior debridement and reconstruction of the anterior column were not performed.22) However, in this current procedure, the remaining normal anatomical structures, distinguishable from corpectomy, were strong enough that no additional anterior column support was necessary. Rather, spontaneous fusion after control of spondylodiscitis was expected.
It can be postulated that the current transpedicular drainage procedure has several effects on the infected vertebrae. First, there is removal and drainage of sticky pus-like materials, which plugged into the cancellous scaffold structure. Second, there is lowering of intra-vertebral pressure through pedicle holes. As a result, the blocked arterial blood flow, which contains the antibiotic component, could run through the infected vertebra(e) and deliver an effective dose of antibiotics with mechanical stability.
The hospitalization periods and administration of antibiotics were longer than expected, 6 to 8 weeks in four patients. They derived from the existing co-morbidity of other infective diseases such as septic knee arthritis, acute pyelonephritis, and perioperative complication.
This study has some limitations in our paper. There were only 10 cases enrolled in the present study, which treated with our procedure. Although spinal infections have been more frequent recently,23) most patients with spinal infections can be treated conservatively with intravenous antibiotic medication, bed rest, and external immobilization alone.1-3,6,20,24) Among patients who belonged to surgical indication during the investigated period of the present study, two thirds of patients were treated through conventional anterior interbody fusion with posterior instrumentation, especially in patients with iatrogenic spondylodiscitis, which presented the rapid progression of their clinical symptom and anatomical structural destruction. In future studies, we will compare the clinical and radiologic results between these two groups.
Another limitation is that there were no quantified clinical results for the visual analogue scale and the Owestry disability index score. The frequent transfer of patients depending on the main morbidity made it difficult to measure the consistent clinical results on time.
Despite these limitations, we suggest our transpedicular curettage and drainage procedure as a useful technique for treatment of infectious spondylodiscitic patients, who are unable to undergo the conventional combined anterior and posterior surgery due to multiple co-morbidities, multiple level infectious lesions, and poor general condition.
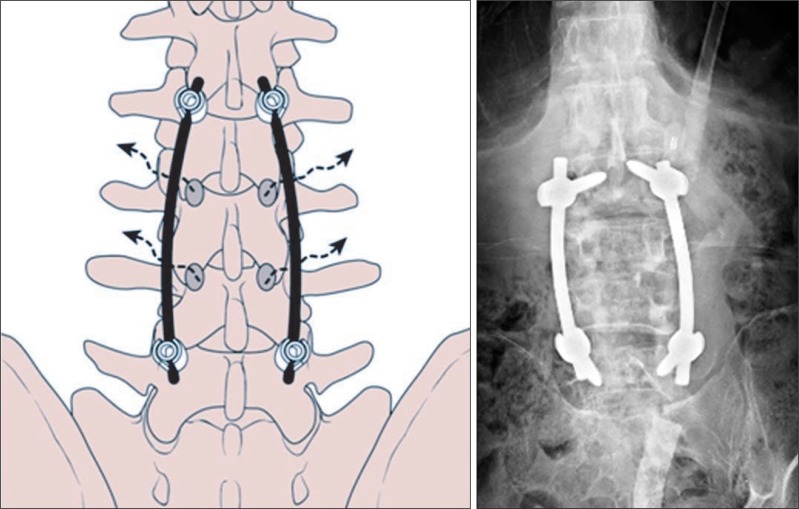
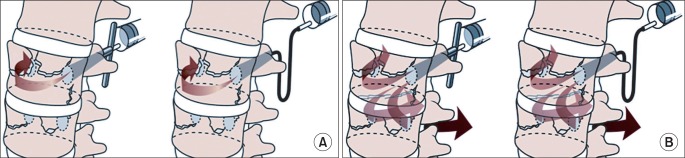
Fig. 2.
(A) Diagram shows drainage of the irrigation flow streams. The irrigation flow drained through the contralateral pedicle of the vertebra. (B) Diagram shows the multi-directional drainage of the irrigation flow streams. If communication was made through disc space between vertebrae as a result of spondylodiscitis progression, the irrigation fluids were drained through multiple pedicles of the adjacent vertebrae via disorganized disc cracks.
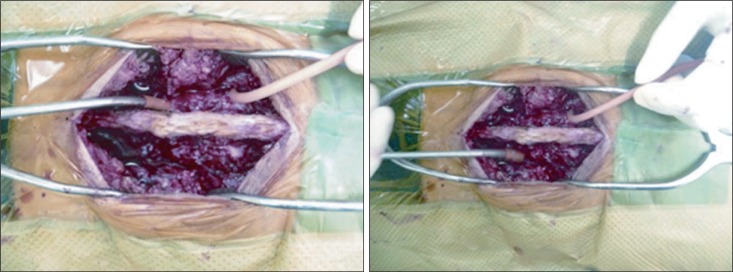
Fig. 3.
Photograph shows drainage of the irrigation fluid through the ipsilateral and contralateral pedicle of upper vertebra.
Footnotes
No potential conflict of interest relevant to this article was reported.
References
- 1.Calderone RR, Larsen JM. Overview and classification of spinal infections. Orthop Clin North Am. 1996;27(1):1–8. [PubMed] [Google Scholar]
- 2.Muller EJ, Russe OJ, Muhr G. Osteomyelitis of the spine. Orthopade. 2004;33(3):305–315. doi: 10.1007/s00132-003-0603-2. [DOI] [PubMed] [Google Scholar]
- 3.McGuire RA, Eismont FJ. The fate of autogenous bone graft in surgically treated pyogenic vertebral osteomyelitis. J Spinal Disord. 1994;7(3):206–215. doi: 10.1097/00002517-199407030-00002. [DOI] [PubMed] [Google Scholar]
- 4.Ghanayem AJ, Zdeblick TA. Cervical spine infections. Orthop Clin North Am. 1996;27(1):53–67. [PubMed] [Google Scholar]
- 5.Graziano GP, Sidhu KS. Salvage reconstruction in acute and late sequelae from pyogenic thoracolumbar infection. J Spinal Disord. 1993;6(3):199–207. doi: 10.1097/00002517-199306030-00003. [DOI] [PubMed] [Google Scholar]
- 6.Abramovitz JN, Batson RA, Yablon JS. Vertebral osteomyelitis: the surgical management of neurologic complications. Spine (Phila Pa 1976) 1986;11(5):418–420. [PubMed] [Google Scholar]
- 7.Dimar JR, Carreon LY, Glassman SD, Campbell MJ, Hartman MJ, Johnson JR. Treatment of pyogenic vertebral osteomyelitis with anterior debridement and fusion followed by delayed posterior spinal fusion. Spine (Phila Pa 1976) 2004;29(3):326–332. doi: 10.1097/01.brs.0000109410.46538.74. [DOI] [PubMed] [Google Scholar]
- 8.Fukuta S, Miyamoto K, Masuda T, et al. Two-stage (posterior and anterior) surgical treatment using posterior spinal instrumentation for pyogenic and tuberculotic spondylitis. Spine (Phila Pa 1976) 2003;28(15):E302–E308. doi: 10.1097/01.BRS.0000083318.40123.5E. [DOI] [PubMed] [Google Scholar]
- 9.Carragee EJ. Instrumentation of the infected and unstable spine: a review of 17 cases from the thoracic and lumbar spine with pyogenic infections. J Spinal Disord. 1997;10(4):317–324. [PubMed] [Google Scholar]
- 10.Chen WJ, Wu CC, Jung CH, Chen LH, Niu CC, Lai PL. Combined anterior and posterior surgeries in the treatment of spinal tuberculous spondylitis. Clin Orthop Relat Res. 2002;(398):50–59. doi: 10.1097/00003086-200205000-00008. [DOI] [PubMed] [Google Scholar]
- 11.Dietze DD, Jr, Fessler RG, Jacob RP. Primary reconstruction for spinal infections. J Neurosurg. 1997;86(6):981–989. doi: 10.3171/jns.1997.86.6.0981. [DOI] [PubMed] [Google Scholar]
- 12.Fayazi AH, Ludwig SC, Dabbah M, Bryan Butler R, Gelb DE. Preliminary results of staged anterior debridement and reconstruction using titanium mesh cages in the treatment of thoracolumbar vertebral osteomyelitis. Spine J. 2004;4(4):388–395. doi: 10.1016/j.spinee.2004.01.004. [DOI] [PubMed] [Google Scholar]
- 13.Lee MC, Wang MY, Fessler RG, Liauw J, Kim DH. Instrumentation in patients with spinal infection. Neurosurg Focus. 2004;17(6):E7. doi: 10.3171/foc.2004.17.6.7. [DOI] [PubMed] [Google Scholar]
- 14.Rath SA, Neff U, Schneider O, Richter HP. Neurosurgical management of thoracic and lumbar vertebral osteomyelitis and discitis in adults: a review of 43 consecutive surgically treated patients. Neurosurgery. 1996;38(5):926–933. doi: 10.1097/00006123-199605000-00013. [DOI] [PubMed] [Google Scholar]
- 15.Perronne C, Saba J, Behloul Z, et al. Pyogenic and tuberculous spondylodiskitis (vertebral osteomyelitis) in 80 adult patients. Clin Infect Dis. 1994;19(4):746–750. doi: 10.1093/clinids/19.4.746. [DOI] [PubMed] [Google Scholar]
- 16.Klockner C, Valencia R. Sagittal alignment after anterior debridement and fusion with or without additional posterior instrumentation in the treatment of pyogenic and tuberculous spondylodiscitis. Spine (Phila Pa 1976) 2003;28(10):1036–1042. doi: 10.1097/01.BRS.0000061991.11489.7F. [DOI] [PubMed] [Google Scholar]
- 17.Erkan S, Wu C, Mehbod AA, Cho W, Transfeldt EE. Biomechanical comparison of transpedicular versus extrapedicular vertebroplasty using polymethylmethacrylate. J Spinal Disord Tech. 2010;23(3):180–185. doi: 10.1097/BSD.0b013e31819c48a4. [DOI] [PubMed] [Google Scholar]
- 18.Chen L, Yang H, Tang T. Unilateral versus bilateral balloon kyphoplasty for multilevel osteoporotic vertebral compression fractures: a prospective study. Spine (Phila Pa 1976) 2011;36(7):534–540. doi: 10.1097/BRS.0b013e3181f99d70. [DOI] [PubMed] [Google Scholar]
- 19.Suk SI, Lee CK, Min HJ, Cho KH, Oh JH. Comparison of Cotrel-Dubousset pedicle screws and hooks in the treatment of idiopathic scoliosis. Int Orthop. 1994;18(6):341–346. doi: 10.1007/BF00187077. [DOI] [PubMed] [Google Scholar]
- 20.Suk SI. Pedicle screw instrumentation for adolescent idiopathic scoliosis: the insertion technique, the fusion levels and direct vertebral rotation. Clin Orthop Surg. 2011;3(2):89–100. doi: 10.4055/cios.2011.3.2.89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Okada Y, Miyamoto H, Uno K, Sumi M. Clinical and radiological outcome of surgery for pyogenic and tuberculous spondylitis: comparisons of surgical techniques and disease types. J Neurosurg Spine. 2009;11(5):620–627. doi: 10.3171/2009.5.SPINE08331. [DOI] [PubMed] [Google Scholar]
- 22.Chen YC, Chang MC, Wang ST, Yu WK, Liu CL, Chen TH. One-stage posterior surgery for treatment of advanced spinal tuberculosis. J Chin Med Assoc. 2003;66(7):411–417. [PubMed] [Google Scholar]
- 23.Beronius M, Bergman B, Andersson R. Vertebral osteomyelitis in Goteborg, Sweden: a retrospective study of patients during 1990-95. Scand J Infect Dis. 2001;33(7):527–532. doi: 10.1080/00365540110026566. [DOI] [PubMed] [Google Scholar]
- 24.Patzakis MJ, Rao S, Wilkins J, Moore TM, Harvey PJ. Analysis of 61 cases of vertebral osteomyelitis. Clin Orthop Relat Res. 1991;(264):178–183. [PubMed] [Google Scholar]