Abstract
Background
The goal of this study was to compare simple radiographic findings and clinical results according to residual ulnar variance following ulnar shortening for ulnar impaction syndrome.
Methods
Forty-five cases of ulnar impaction syndrome, which were treated with ulnar shortening from 2005 to 2008, were studied retrospectively. Group I included 13 cases with positive residual variance after ulnar shortening and group II included 32 cases with negative variance after shortening. The presence of a lunate cystic lesion both preoperatively and at final follow-up and assessments of wrist function based on the modified Mayo wrist score, the disabilities of the arm, shoulder, and hand (DASH) score, as well as the Chun and Palmer score were evaluated.
Results
A cystic lesion of the lunate was present in 4 cases preoperatively and the size decreased in 2 cases at final follow-up in group I, and in 10 and 5 cases, respectively, in group II. No statistical difference was observed between the groups. The modified Mayo wrist score, DASH score, as well as the Chun and Palmer score improved significantly in both groups. No significant differences were observed between the two groups in terms of the proportion of positive cystic lesions at final follow-up or the functional scores.
Conclusions
After ulnar shortening, the degree of radiological change in the cystic lunate lesions and clinical improvement did not differ significantly between the groups with unintended residual positive and negative variance after shortening.
Keywords: Wrist, Residual ulnar variance, Ulnar impaction syndrome, Ulnar shortening
Since the ulnocarpal joint transfers a considerable amount of stress through a comparatively small contact surface, the risk of degenerative change is high. This degenerative process is known as ulnar impaction syndrome and chronic pressure stress is thought to be the primary cause. Treatments for ulna impaction syndrome can either be conservative or surgical. Surgical treatment includes the Wafer procedure, ulnar shortening, hemiresection-interpositional arthroplasty, as well as the Sauve-Kapandji and Darrach techniques. Ever since Chun and Palmer1) reported promising results with ulnar shortening in 1993, it has been used widely for the surgical treatment of ulnar impaction syndrome. Recently, osteotomy methods and various surgical techniques based on internal fixation have been introduced.2-6) In principle, an osteotomy is attempted with the goal of attaining neutral ulnar variance; however, since the actual extent of the osteotomy is only a few millimeters, and even though it is performed using a ruler, there may be some residual positive or negative ulnar variance. Collectively, this was a retrospective study that examined differences in postoperative clinical results and radiological changes after osteotomy and shortening between groups exhibiting both unintended positive or negative ulnar variance.
METHODS
This study enrolled 48 patients who were diagnosed with ulnar impaction syndrome between April 2005 and December 2008, and underwent ulnar shortening using a transverse osteotomy, which was shorter or longer than intended. The inclusion criteria for this study were as follows: 1) symptoms such as pain at the ulnar portion of the wrist, limited range of motion, edema with a positive ulnar impaction sign and a grinding test on physical examination, and the presence of positive ulnar variance on a posteroanterior simple radiograph in neutral rotation, allowing the diagnosis of ulnar impaction syndrome; 2) surgical treatment; 3) more than 1 mm of positive or negative ulnar variance seen on the postoperative posteroanterior radiograph in neutral rotation; and 4) follow-up for at least 2 years.
The exclusion criteria were as follows: 1) a history of trauma to the ulnocarpal joint in the past year; 2) a correlation regarding the onset of symptoms with a history of long fall or sports injury; 3) a fracture of the distal radius or ulna; 4) Kienbock's disease; 5) severe arthritic change in the ulnocarpal or distal radioulnar joint; 6) a comorbid disease such as synovitis; 7) and residual variance after the osteotomy of less than ± 1 mm.
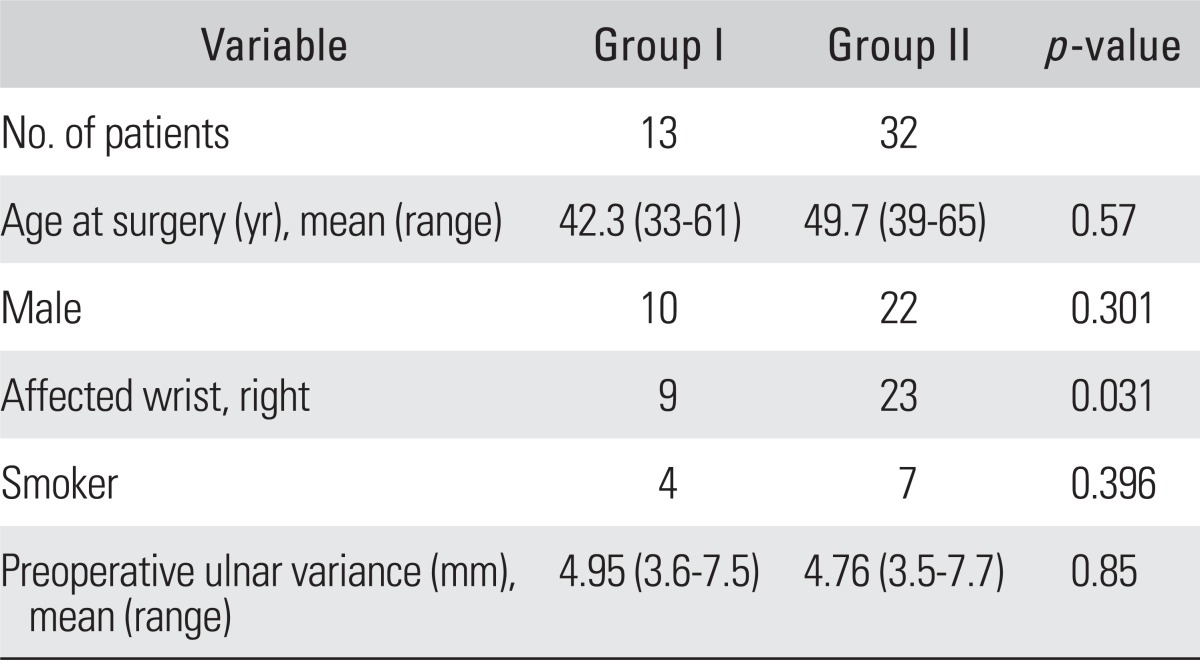
In all cases, the surgery used the transverse osteotomy technique to shorten the ulna; a single 3.5-mm 6-hole compressive metal plate was used to fix the osteotomy portion. For evaluation, a posteroanterior wrist radiograph in neutral rotation was used, and the preoperative variance was measured.7) An osteotomy to achieve neutral ulnar variance was planned (Fig. 1). A single surgeon performed the surgery, and ulnocarpal wrist exercises were started on the second or third postoperative day. We planned to remove the metal plate when union at the osteotomy site was confirmed and this study included patients in whom the metal plate was removed. Of the 48 patients, two cases were lost to follow-up and one died during follow-up. Therefore, we followed 45 cases for at least two years. There were 32 males and 13 females, with a mean age of 48.6 years (range, 33 to 65 years). The duration of symptoms was 25.8 months (range, 10 to 72 months), and the mean follow-up period was 32.6 months (range, 24 to 65 months). Group I included cases with positive ulnar variance after ulnar shortening: 10 males, 3 females; mean age 42.3 years (range, 33 to 61 years); duration of symptoms 26.4 months (range, 12 to 72 months); and mean follow-up 38.4 months (range, 24 to 65 months). Group II included cases with negative ulnar variance after ulnar shortening: 22 males, 10 females; mean age 49.7 years (range, 39 to 65 years); duration of symptoms 25.2 months (range, 10 to 60 months); and mean follow-up 30.2 months (24 to 59 months) (Table 1).
Fig. 1.
The ulnar variance was measured by drawing a line through the volar sclerotic line of the distal radius perpendicular to its longitudinal axis. The variance is the distance between this line and the distal cortical rim of the ulnar dome.
Table 1.
Demographic Data between Two Groups
Two observers evaluated each of the radiographs twice, two weeks apart. In order to evaluate the inter- and intra-observer concordance, the kappa value was calculated. According to the method of Fleiss and Cohen,8) κ ≥ 0.75 was regarded as an excellent agreement, 0.4 ≤ κ < 0.75 as fair to good agreement, and κ < 0.4 as a poor agreement. The measurement of variance was standardized using posteroanterior radiographs in neutral rotation pre- and postoperatively, and at follow-up. Also, to evaluate the wrist preoperatively and at the final follow-up, the modified Mayo wrist score,9) the disabilities of the arm, shoulder and hand (DASH) score,10) and the Chun and Palmer score1) were used. The two groups were compared statistically using SPSS ver. 12.0 (SPSS Inc., Chicago, IL, USA). The size of the cystic lesion was considered to be decreased when it was reduced by at least 50% based on the evaluations of two different observers. To compare cystic changes in the lunate preoperatively, a chi-square test was used. Furthermore, to compare changes in the clinical scores, a Wilcoxon's signed-rank test was used. Lastly, to compare differences in the clinical scores between the two groups, a Mann-Whitney U-test was used and the reliability was set to 95%.
RESULTS
Union of the osteotomy was confirmed in all cases postoperatively, and the metal plate was removed at a mean of 10.4 months (range, 7 to 17 months) postoperatively.
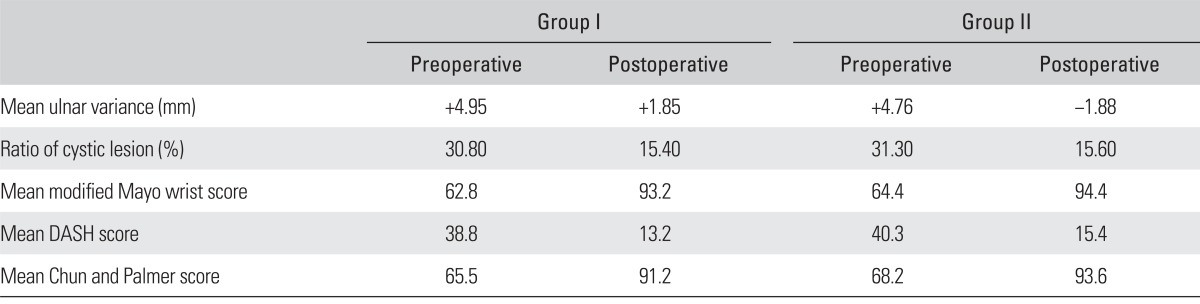
Cystic lesions of the lunate were found in 4 cases (30.8%) in group I preoperatively and the size of cystic lesions were decreased in 2 cases (15.4%) at the final follow-up, versus 10 (31.3%) and 5 (15.6%) cases, respectively, in group II; the difference between the two groups was not significant (p = 0.894). The ulnar variance in group I was 4.95 mm (range, 3.6 to 7.5 mm) preoperatively and 1.85 mm (range, 1.18 to 2.34 mm) at the final follow-up, and the kappa values were excellent being 0.82 and 0.88, respectively. The ulnar variance in group II was 4.76 mm (range, 3.5 to 7.7 mm) and -1.88 mm (range, -1.3 to -2.6 mm), respectively, and the kappa values measured together or alone by the observer were 0.79 and 0.80, respectively; again, both were "excellent" (> 0.75). The modified Mayo wrist score in group I was 62.8 points (range, 50 to 75 points) preoperatively and 93.2 points (range, 75 to 100 points) at the final follow-up and 64.4 points (range, 60 to 75 points) and 94.4 points (range, 75 to 100 points), respectively, in group II; the increases were significant (p = 0.031 and p = 0.040, respectively), while differences between the two groups preoperatively and at the final follow-up were not significant (p = 0.665 and p = 0.747, respectively). Further, the DASH score in group I was 38.8 points (range, 33 to 42 points) preoperatively and 13.2 points (range, 8 to 17 points) at the final follow-up, and 40.3 points (range, 36 to 49 points) and 15.4 points (range, 13 to 17 points), respectively, in group II; the changes were significant (p = 0.029 and p = 0.034, respectively), while differences between the two groups preoperatively and at the final follow-up were not significant (p = 0.45 and p = 0.27, respectively). Moreover, the Chun and Palmer score in group I was 65.5 points (range, 63 to 68 points) preoperatively and 91.2 points (range, 85 to 95 points) at the final follow-up and 68.2 points (range, 60 to 70 points) and 93.6 points (range, 85 to 98 points), respectively, in group II; the changes were significant (p = 0.034 and p = 0.038, respectively), while differences between the two groups preoperatively and at the final follow-up were not significant (p = 0.35 and p = 0.53, respectively) (Table 2). Lastly, neither group had complications, such as infection, periprosthetic fracture, or nonunion.
Table 2.
Summary of Results
DASH: the disabilities of the arm, shoulder, and hand.
DISCUSSION
Ulnar shortening is the most widely used method for treating ulnar impaction syndrome, which is a common cause of ulnocarpal joint pain.1) Pathophysiologically, ulnar impaction syndrome is a degenerative lesion caused by continuous stress on the ulnar column of the wrist, which consists of the lunate, triquetrum, hamate, triangular fibrocartilage complex, and ulnar head. This degenerative change starts with osteomalacia of the articular surface, which is subject to stress, and the triangular fibrocartilage complex.11) Since the majority of patients with ulnar impaction syndrome symptoms have positive ulnar variance, it is thought to be the most common cause of ulnar impaction syndrome.11,12) Cadaveric studies demonstrate that in a wrist with neutral ulnar variance, 82% of the stress is transferred to the radiocarpal joint and 18% to the ulnocarpal joint; if the ulna is 2.5 mm longer, the ulnocarpal joint receives 42% more stress, while if the ulna is 2.5 mm shorter, the joint receives only 4.3% of the stress received in neutral variance.13,14)
Chun and Palmer1) showed that ulnar impaction syndrome occurs not only in neutral ulnar variance, but also in negative ulnar variance.3,12,15) In addition, in ulnar impaction syndrome, sclerosis and cystic lesions of the lunate are seen radiographically,11,16) and the correlation between the disease and these radiological findings is significant. After ulnar shortening, both the clinical symptoms and the cystic lesion or osteomalacia of the ulnar head and lunate are seen on simple radiographs or magnetic resonance imaging improve with time.17,18)
For several years, we have experienced difficulty in performing osteotomies that give exact "neutral variance." Consequently, we wondered whether there is a difference in the clinical and radiological improvement between those cases with an excessive (negative variance) or insufficient (positive variance) osteotomy. Compared with the differences in the neutral position and supination, Nishiwaki et al.19) found the greatest change in pronation; after performing ulnar shortening of 3, 4, 5, and 6 mm, the greater the distal radioulnar joint stability increased by 14%, 24%, 35%, and 44%, respectively. Therefore, we obtain the greatest biomechanical effect when we perform ulnar shortening exceeding 3-4 mm.
In our patients, we shortened the ulna by a mean of 4.65 mm and although there was residual positive or negative variance, the clinical results were satisfactory. Preoperatively, 14 cases (4 in group I and 10 in group II) had cystic lesions versus 7 cases (2 in group I and 5 in group II) at final follow-up. The preoperative cystic lesions within each group decreased significantly at the final follow-up, although the difference between the two groups was insignificant. Therefore, if the osteotomy achieves a decompression and stabilization effect with regards to whether there is residual positive (mean, 1.85 mm) or negative (mean, 1.88 mm) variance does not have a significant clinical effect. Nishiwaki et al.19) proved that the biomechanical stability of the distal radioulnar joint is proportional to the degree of the osteotomy, which not only produces decompression in ulnar impaction syndrome, but also has a "stabilization effect" that improves the clinical symptoms. Overall, we believe that the stabilization effect is as effective as decompression, as demonstrated by the improvement in the cases in which the lunate lesion remains.
One limitation of this study is that it is a retrospective case analysis, and there were few cases, especially with positive residual variance. As a result, we cannot clearly determine the extent of allowable residual variance. It was difficult to measure this, since the amount was very small, in millimeters. A study regarding the relationship between radiologic changes and clinical symptoms after shortening should measure the residual variance in many more cases.
In conclusion, the degree of radiological changes in the lunate cystic lesions and improvements in the clinical results postoperatively (following shortening of the ulna) did not differ significantly between the groups with unintended positive and negative residual variance. Finally, theresults in both groups were satisfactory.
Footnotes
No potential conflict of interest relevant to this article was reported.
References
- 1.Chun S, Palmer AK. The ulnar impaction syndrome: follow-up of ulnar shortening osteotomy. J Hand Surg Am. 1993;18(1):46–53. doi: 10.1016/0363-5023(93)90243-V. [DOI] [PubMed] [Google Scholar]
- 2.Lauder AJ, Luria S, Trumble TE. Oblique ulnar shortening osteotomy with a new plate and compression system. Tech Hand Up Extrem Surg. 2007;11(1):66–73. doi: 10.1097/bth.0b013e3180336cc7. [DOI] [PubMed] [Google Scholar]
- 3.Feldon P, Terrono AL, Belsky MR. Wafer distal ulna resection for triangular fibrocartilage tears and/or ulna impaction syndrome. J Hand Surg Am. 1992;17(4):731–737. doi: 10.1016/0363-5023(92)90325-j. [DOI] [PubMed] [Google Scholar]
- 4.Wehbe MA, Cautilli DA. Ulnar shortening using the AO small distractor. J Hand Surg Am. 1995;20(6):959–964. doi: 10.1016/s0363-5023(05)80143-1. [DOI] [PubMed] [Google Scholar]
- 5.Constantine KJ, Tomaino MM, Herndon JH, Sotereanos DG. Comparison of ulnar shortening osteotomy and the wafer resection procedure as treatment for ulnar impaction syndrome. J Hand Surg Am. 2000;25(1):55–60. doi: 10.1053/jhsu.2000.jhsu025a0055. [DOI] [PubMed] [Google Scholar]
- 6.Loh YC, Van Den Abbeele K, Stanley JK, Trail IA. The results of ulnar shortening for ulnar impaction syndrome. J Hand Surg Br. 1999;24(3):316–320. doi: 10.1054/jhsb.1999.0062. [DOI] [PubMed] [Google Scholar]
- 7.Palmer AK, Glisson RR, Werner FW. Ulnar variance determination. J Hand Surg Am. 1982;7(4):376–379. doi: 10.1016/s0363-5023(82)80147-0. [DOI] [PubMed] [Google Scholar]
- 8.Fleiss JL, Cohen J. The equivalence of weighted kappa and the intraclass correlation coefficient as measures of reliability. Educ Psychol Meas. 1973;33(3):613–619. [Google Scholar]
- 9.Cooney WP, Bussey R, Dobyns JH, Linscheid RL. Difficult wrist fractures. Perilunate fracture-dislocations of the wrist. Clin Orthop Relat Res. 1987;(214):136–147. [PubMed] [Google Scholar]
- 10.Hudak PL, Amadio PC, Bombardier C. Development of an upper extremity outcome measure: the DASH (disabilities of the arm, shoulder and hand): the Upper Extremity Collaborative Group (UECG) Am J Ind Med. 1996;29(6):602–608. doi: 10.1002/(SICI)1097-0274(199606)29:6<602::AID-AJIM4>3.0.CO;2-L. [DOI] [PubMed] [Google Scholar]
- 11.Friedman SL, Palmer AK. The ulnar impaction syndrome. Hand Clin. 1991;7(2):295–310. [PubMed] [Google Scholar]
- 12.Tomaino MM. Ulnar impaction syndrome in the ulnar negative and neutral wrist: diagnosis and pathoanatomy. J Hand Surg Br. 1998;23(6):754–757. doi: 10.1016/s0266-7681(98)80090-9. [DOI] [PubMed] [Google Scholar]
- 13.Palmer AK. Triangular fibrocartilage complex lesions: a classification. J Hand Surg Am. 1989;14(4):594–606. doi: 10.1016/0363-5023(89)90174-3. [DOI] [PubMed] [Google Scholar]
- 14.Palmer AK, Werner FW. Biomechanics of the distal radioulnar joint. Clin Orthop Relat Res. 1984;(187):26–35. [PubMed] [Google Scholar]
- 15.Tomaino MM, Rubin DA. The value of the pronated-grip view radiograph in assessing dynamic ulnar positive variance: a case report. Am J Orthop (Belle Mead NJ) 1999;28(3):180–181. [PubMed] [Google Scholar]
- 16.Escobedo EM, Bergman AG, Hunter JC. MR imaging of ulnar impaction. Skeletal Radiol. 1995;24(2):85–90. doi: 10.1007/BF00198066. [DOI] [PubMed] [Google Scholar]
- 17.Imaeda T, Nakamura R, Shionoya K, Makino N. Ulnar impaction syndrome: MR imaging findings. Radiology. 1996;201(2):495–500. doi: 10.1148/radiology.201.2.8888248. [DOI] [PubMed] [Google Scholar]
- 18.Tatebe M, Nakamura R, Horii E, Nakao E. Results of ulnar shortening osteotomy for ulnocarpal impaction syndrome in wrists with neutral or negative ulnar variance. J Hand Surg Br. 2005;30(2):129–132. doi: 10.1016/j.jhsb.2004.09.005. [DOI] [PubMed] [Google Scholar]
- 19.Nishiwaki M, Nakamura T, Nakao Y, Nagura T, Toyama Y. Ulnar shortening effect on distal radioulnar joint stability: a biomechanical study. J Hand Surg Am. 2005;30(4):719–726. doi: 10.1016/j.jhsa.2005.04.015. [DOI] [PubMed] [Google Scholar]