Abstract
We tested the applicability of the IMB model in predicting condom use among sexually active secondary school students in Mbarara, Uganda. Three hundred and ninety adolescents across five secondary schools completed a self-report survey about their health and sexual experiences. Based upon results from structural equation modeling, the IMB model partially predicts condom use. Condom use was directly predicted by HIV prevention information and behavioral skills regarding having and using condoms. It was indirectly predicted (through behavioral skills regarding having and using condoms) by behavioral intentions regarding using condoms and talking to one‘s partner about safer sex. Aspects of one‘s first sexual experience (i.e., age at first sex, having discussed using condoms with first sex partner, willingness at first sex) are hugely influential of current condom use; this is especially true for discussing condoms with one‘s first partner. Findings highlight the importance of providing clear and comprehensive condom use training in HIV prevention programs aimed at Ugandan adolescents. They also underscore the importance of targeting abstinent youth before they become sexually active to positively affect their HIV preventive behavior at their first sexual experience.
Keywords: IMB Model, Uganda, adolescents, condom use
INTRODUCTION
An estimated 4.3% of females and 1.1% of males between the ages of 15 and 24 years are HIV positive in Uganda (1). Despite an impressive decrease in HIV incidence rates, recent data suggest stabilization and perhaps even an increase in national rates of new cases (1). Many adolescent behavioral trends are encouraging (e.g., age at first sex is increasing, teen pregnancy is decreasing), but data suggest that condom use may be decreasing among 13–19 year olds in recent years (2). This may be because only 15% of Ugandan schools provide life skills-based HIV education (1). Given that heterosexual transmission contributes to 76% of new HIV infections (2), this limited access to HIV prevention programs for adolescents is concerning. Increasing availability of evidence-based HIV prevention programs for young people in Uganda is urgently needed and may have an impact on future incidence rates.
Effective HIV prevention programs are guided by strong theoretical models (3). One of the most comprehensive efforts to review research conducted between 1996 and 2009 on HIV prevention is synthesized in a compendium documenting the evidence of efficacy and effectiveness across 73 behavioral interventions (4). This work focuses primarily on U.S. based HIV prevention research and illustrates the utility of utilizing a theoretical model to guide interventions. The use of theory allows intervention planners to focus on specific areas to target in interventions, including such things as knowledge, attitudes, norms, skills, confidence, intentions, social support, and access to resources. It also allows evaluators and researchers the opportunity to measure effects by focusing on these specific areas, and ultimately provides the field with an evidence base of areas that are particularly salient and useful to target when conducting prevention interventions.
The most commonly utilized model in effective HIV prevention and intervention programs is the Social Learning Theory, also known as Social Cognitive Theory (SLT/SCT) (5), which has been used in 33 of the interventions documented in the compendium. There were 13 interventions utilizing the Theory of Reasoned Action or its extension, Theory of Planned Behavior (TRA/TPB) (6, 7), and 11 that utilized the Information, Motivation and Behavior Model (IMB) (8, 9). Other theoretical models widely utilized include the Transtheoretical Model of Behavior Change (10), the Health Belief Model (11), Diffusion of Innovations Theory (12), and the Theory of Gender and Power (13). Table 1 identifies key constructs from these theoretical models and identifies similarities across constructs.
Table 1.
Constructs utilized in the most commonly employed theoretical frameworks in HIV prevention intervention with evidence of efficacya
| Theory | Selected Constructs | Definition |
|---|---|---|
| Social Learning/Social Cognitive Theory (5, 63) | Reciprocal Determinism | The interaction between internal cognitive processes and the external environment that facilitate behavior change |
| Self-Efficacy | The confidence to perform a behavior, even given difficult or challenging circumstances | |
| Observational Learning | Having an important other, someone you admire (e.g. adult such as a coach or teacher) perform a behavior, thereby making it attractive | |
| Behavioral Capability | The skills to perform a behavior | |
| Expectations and Expectancies | The expected outcome of performing a behavior; appraisal of what good or bad things will happen once it is enacted— influenced by behavioral beliefs | |
| Emotional Coping Responses | Strategies utilized in response to emotional triggers | |
| Theory of Reasoned Action/Theory of Planned Behavior (6) | Attitudes (Positive and Negative Outcome Expectancies) | The expected outcome of performing a behavior; appraisal of what good or bad things will happen once it is enacted— influenced by behavioral beliefs |
| Subjective Norms | Perception of the behaviors that others like you would adopt or reject- influenced by normative beliefs (values) and motivation to be like a peer | |
| Intentions | Specific plans to enact a behavior | |
| Perceived Behavioral Control | The extent to which an individual believes they have the power to change | |
| Information, Motivation and Behavior (64) | Information | Information about how to perform a behavior and on why it is desirable and necessary for change |
| Motivation | Impetus or desire to change must be present in order for change to occur | |
| Skills | Individuals must have specific skills to enact behavior change; specific to the desired behavior |
Shown across numerous studies including meta analyses to be related to changes in behavioral outcomes and to consistently explain a high proportion of variance in behavioral outcomes.
In the work reported here, we focus on the IMB model, primarily because it has been tested for applicability in research on HIV prevention in resource-limited settings, mostly among adults. Also, the IMB offers evidence of efficacy in increasing HIV preventive behavior among adolescents (8, 9, 14–18). According to the IMB model, HIV preventive behavior is influenced by: 1) information about how to prevent HIV, 2) motivation to consistently engage in non-risky behaviors, and 3) behavioral skills to correctly enact these behaviors. The effects of information and motivation on onset and sustainability of one‘s HIV preventive behavior are mediated by behavioral skills. For example, improving one‘s motivation to engage in preventive behaviors is expected to lead to an increase in HIV preventive behavioral skills, which then leads to an increase in enactment of HIV preventive behavior.
As shown in Table 1, IMB has elements that are similar to other theoretical models commonly utilized in HIV prevention research, but also includes unique constructs. For example, IMB includes some elements similar to those of TRA/TPB. Creators of this theory posited that awareness (analogous to information) as well as subjective norms and intentions, both of which are subsumed under the construct of motivation in the IMB model, contributed to health behavioral outcomes. In addition, self-efficacy is a construct present in both the TRA/TPB and SLT/SCT; this is defined as the ability to perform a given behavior and have the confidence you can do so under varying and sometimes challenging conditions (5). The skills construct, by contrast, identified as a key element of the IMB, does not emphasize confidence.
Across those studies reviewed in the compendium and others, behavioral skills consistently predict HIV preventive behavior (16, 18–20). In most cases, motivation also is noted as predictive of HIV preventive behavior, including among Chinese female entertainment workers (19), primary school students in Kenya (20), Chennai India truck drivers with married partners, but not among truck drivers with non-married partners (16), but not among adults in a public health clinic in Cape Town, South Africa (18). A component of motivation (behavioral intentions) is, however, indirectly related to HIV preventive behavior through self-efficacy in this last population (18).
In contrast to behavioral skills and motivation, information is not predictive of condom use except in one study (16). In another study, information mediates condom use, and self-efficacy for condom use; as well as condom use and motivation (19). Researchers have posited that when HIV information is uniformly high, information is necessary but not sufficient to affect HIV preventive behavior. In settings with low HIV information, it is likely more influential (16). Given that HIV information is generally low across these studies however, the lack of association does not seem to support this hypothesis.
Research about the sexual experience has been conducted to better understand why some young people use condoms and others do not. Data from South Africa suggest that the strongest predictors of current condom use are condom use at first sex and talking about condoms with one‘s first sexual partner (21). On the other hand, having a history of sexually coercive experiences (e.g., being unwilling at first sex), is strongly predictive of HIV risk behavior, including unprotected intercourse (22–32). There also is some indication that adolescent sexual activity, and perhaps condom use, may be affected by caregiver social support (33). Together, these factors must be included in an investigation of condom use predictors in order to understand the full context.
Given the variability in findings of tests of the IMB model across resource-limited settings, the theoretical model should be tested within any new population before it is used to guide the development of an HIV prevention program targeted to that population. Such a test is particularly important for an adolescent-focused program, as none of the research identified by the authors examined the applicability of the IMB model in this age group in a resource-limited setting. In this paper, we examine how well HIV preventive information, motivation, and behavioral skills predict HIV preventive behavior, defined by current condom use, among sexually active secondary school student in Mbarara, Uganda. In addition, we examine how aspects of the sexual experience, in particular age of first sex, talking with first partner about condoms, and sexual coercion predict HIV preventive behavioral skills.
METHODS
IRB approval for the Mbarara Adolescent Health survey was received from Mbarara University Institution Review Board in Uganda as well as Chesapeake IRB in the United States. Data were collected between September and October, 2008 and March and April, 2009. Parents provided permission for day students and headmasters provided permission for boarding students to take part. All students provided informed assent.
Participants
Survey data were collected as part of CyberSenga, a study aimed at developing and testing an Internet-based HIV prevention program for adolescents in Uganda. Five secondary schools in Mbarara, Uganda participated. Mbarara municipality, with a population of 69,000 (based on the 2002 census), is the sixth largest urban center in Uganda (34). Access to education in Mbarara is mixed. Mbarara University of Science and Technology is the 18th largest of Uganda‘s 53 tertiary institutions (34). Data at the district level indicate that Mbarara district‘s 2004 net secondary enrollment rate was slightly lower than the national average (11.3% versus 14.6%) (34).
The five secondary schools were purposefully selected to represent a wide range of school and student characteristics (see Table 2 for more details). All five schools provide education to students in classes Secondary 1 through Secondary 6 (roughly equivalent to grades 8–12 in the U.S.). Eligibility for the study included 1) current enrollment in grades Secondary 1 (S1) through Secondary 3 (S3) in one of the five participating secondary schools; 2) caregiver/adult permission; and 3) youth assent. Because the main aim of the survey was to identify youth popular opinion leaders for a Youth Advisory Council, the survey was conducted twice: among S1-S3 at the end of the school year (September-October) and among new S1 at the beginning of the next school year (March - April). To distinguish between the two groups - the S1’s especially - we will refer to the four groups as follows: S1Early, S1End, S2End, and S3End. Power analyses were conducted to determine the size of the sample from each class needed to accurately identify popular opinion leaders in the class. Based upon these power analyses and, consequently, the total class size in each of the schools, 312 students were randomly selected to participate in each of four schools; and 248 students in the fifth school (n=1,496). When participants were not available or they chose not to participate, they were replaced with the next name on the randomly ordered list of students. As a result, 1,738 students 12–18 years of age were invited to participate, and 1,523 completed surveys were received. [Seventeen of the 1,523 respondents completed the survey without being invited.6] Ten participants were initially deemed ineligible because of lack of parental consent and were replaced with another student. When they subsequently produced their parental consent however, they were allowed to take the survey. Of the 232 students who were invited and did not participate: one actively refused to participate and 183 passively refused by not showing up at the time of the survey; 22 students started the survey but walked out before completing it; 23 were not eligible on the day of the survey because of lacking parental permission; and three were expelled from school between the time they were recruited and the survey was implemented. Thus, of the 1,738 students invited, 1,506 completed the survey and 232 did not. The overall response rate was 86.7%. Per-school response rates ranged from 67.7% – 99.4%.
Table 2.
Characteristics of youth by school (n = 1,503)
| Characteristic | Participating schools
|
|||||
|---|---|---|---|---|---|---|
| A | B | C | D | E | ||
|
| ||||||
| Eligible enrolled students | 763 | 1,148 | 391 | 1,122 | 935 | |
| Male : Female ratio | 56:44 | 100:0 | 58:42 | 100:0 | 0:100 | |
|
| ||||||
| Percentage of all students | Participating students | |||||
|
| ||||||
| (n = 1,503) | (n=313) | (n=321) | (n=248) | (n=309) | (n=312) | |
| Section | ||||||
| Boarding | 86 (1288) | 45 (141) | 100 (321) | 83 (205) | 100 (309) | 100 (312) |
| Day | 14 (215) | 55 (172) | 0 | 17 (43) | 0 | 0 |
| Class | ||||||
| S.1Early | 24 (368) | 24 (76) | 23 (75) | 25 (62) | 25 (76) | 25 (79) |
| S.1End | 25 (382) | 24 (76) | 28 (89) | 25 (62) | 25 (77) | 25 (78) |
| S.2End | 25 (374) | 25 (80) | 24 (78) | 25 (61) | 25 (78) | 25 (77) |
| S.3End | 25 (379) | 26 (81) | 25 (79) | 25 (63) | 25 (78) | 25 (78) |
| Biological Sex (boys) | 62 (933) | 53 (166) | 100 (321) | 55 (137) | 100 (309) | 0 |
| Father’s education | ||||||
| Less than secondary school | 12 (176) | 20 (64) | 12 (39) | 16 (39) | 5 (17) | 5 (17) |
| Secondary school (A & O) | 33 (497) | 52 (163) | 24 (77) | 42 (105) | 27 (85) | 21 (67) |
| Tertiary institution | 17 (255) | 9 (30) | 21 (67) | 10 (24) | 16 (49) | 27 (85) |
| University graduate | 38 (575) | 18 (56) | 43 (138) | 32 (80) | 51 (158) | 46 (143) |
| Mother’s education | ||||||
| Less than secondary school | 19 (282) | 29 (92) | 21 (66) | 21 (52) | 13 (39) | 11 (33) |
| Secondary school (A & O) | 43 (653) | 55 (172) | 36 (117) | 50 (123) | 38 (117) | 40 (124) |
| Tertiary institution | 16 (242) | 6 (18) | 18 (57) | 12 (30) | 20 (61) | 24 (76) |
| University graduate | 22 (326) | 10 (31) | 25 (81) | 17 (43) | 30 (92) | 25 (79) |
Procedures
Headmasters provided the project coordinator with current class enrollment lists for students from Secondary 1 to Secondary 3 (n = 4,359). The class lists were arranged in alphabetic order and a random sample was generated using a computer random sequencing program (http://www.random.org/sequences/). The project coordinator addressed the entire student body prior to sample selection to explain the study. Then an appointment was made to meet with the selected students to further explain the study. If the student could not be located or was not reachable on the day of the survey, in most cases, they were given a second opportunity to complete the survey. Students who could not be located were replaced with the next student on the randomization list.
The survey was written in English. This is the official language of Uganda but is the non-primary language of all students (35). Nonetheless, English is the language of instruction in schools and is the language that students routinely are required to use to read and comprehend exams. Given the sensitivity of the survey content, measures were taken to ensure participants‘ privacy: when possible, students sat at least 3 feet from each other; names were not collected on the survey instrument nor could the survey be linked to the name or the assent forms with an ID; and surveys were completed in the absence of the teachers and school administrators. The self-administered pencil-and-paper survey took an average of one hour to complete.
Identifying the analytical sample
The Community Advisory Board, comprised of the five school headmasters, deemed inappropriate many of the survey items regarding attitudes and beliefs about sex and condom use (main predictor variables in the IMB model) for youth who had never had sex. Consequently, only youth who reported having had sex completed the full battery of measures related to the IMB model. Analyses presented herein are restricted to participants who reported having had sex (n = 390).
Measures
Scale items are shown in Table 3
Table 3.
Description of multiple-item measures
| Construct | Variable in Analyses | Items |
|---|---|---|
| HIV related information (36, 37) | HIV related information |
|
| Subjective norms (36) | Subjective norms regarding using condoms and talking to partner about safer sex (Cronbach‘s alpha = .88) |
|
| Subjective norms regarding having condoms available to use (Cronbach‘s alpha = .83) |
|
|
| Behavioral intentions (36) | Behavioral intentions regarding using condoms and talking to partner about safer sex (Cronbach‘s alpha = .68) |
|
| Behavioral skills (36) | Behavioral skills regarding having and using condoms (Cronbach‘s alpha = .76) |
|
| Social support (41) | Social support from family (Cronbach‘s alpha = .64) |
|
| Social support from special person (Cronbach‘s alpha = .75) |
|
|
| Sexual self-agency (38, 39) | Sexual self-agency (Cronbach‘s alpha = .70) |
|
Our main outcome measure was frequency of condom use. Participants were asked how often they use a condom when they have sex on a 5-point scale [1(never) -5 (always)].
Components of the IMB model
HIV-related information was measured with eight items. Four of these items (one with a slight modification) were used in the Teen Health Survey, designed to measure key components of the IMB model (36). The other four items were written to assess knowledge of information commonly misconstrued in the target population and were from the Uganda Demographic Health Survey (37). Participants were asked to respond using a 4-point scale [1(definitely false) - 4 (definitely true)]. Responses of definitely true‘ and probably true‘ for accurate items were coded as correct‘; as were definitely false‘ and probably false‘ for inaccurate statements. An information score was then created to reflect the percent of correct answers across the eight items. The higher the score, the greater the HIV-related information one had.
Two components of motivation related to condom use were measured: 1) subjective norms and 2) behavioral intentions. Participants were asked to respond using a 5-point scale [1(very untrue)-5(very true)]. A sum variable was created for each subjective norm variable, with larger numbers reflecting stronger subjective norms favoring HIV preventive behavior.
Behavioral intentions to use condoms and to talk to one‘s partner about using condoms was measured with 4 items (two with slight modifications) from the Teen Health Survey (36). Each item stated a planned behavior. Participants responded using a 5-point scale [1(very untrue)-5(very true)]. Again, a sum variable was created such that larger numbers reflected stronger intentions to use condoms and talk to one‘s partner about safer sex.
Behavioral skills for having and using condoms were measured with 6 items (36). Each item stated a behavior in an incomplete sentence (e.g., —During the next two months, carrying condoms with me would be… ) and asked participants to complete the sentence indicating how difficult the behavior would be [1(very difficult) - 5(very easy)]. A composite variable was created such that larger numbers reflected stronger skills to have and use condoms.
Aspects of the sexual experience
Based upon previous research among adolescents in sub-Saharan Africa, six aspects of the sexual encounter were analyzed: 1) age at first sexual intercourse; 2) whether (yes or no) the youth talked to their first sexual partner about condoms before they had sex; 3) willingness at first sexual intercourse [1(not at all willing) – 3 (very willing)]; 4) the age of the youth‘s most recent partner (noting whether the partner is 5 or more years older than the youth); 5) whether the youth has engaged in transactional sex (i.e., received anything, such as money, gifts, clothes, or a mobile phone so the youth would play sex); and 6) sexual self-agency. Sexual self-agency was assessed using 5-items based upon Bryan‘s Control over the sexual encounter scale (38, 39). The items asked level of agreement [1(Strongly disagree) – 5(Strongly agree)] with each statement. For this multiple-item variable, a composite score was created with higher numbers reflecting greater sexual agency.
Other potentially influential factors
If one‘s physical health is poor, he or she may be less motivated to behave in preventive ways and to use condoms. Physical health was assessed with one item that asked how participants would rate their physical health (i.e., poor, fair, good, or excellent) with responses coded so that larger numbers reflected better perceived health (40).
Social support was measured using the 8-item Multidimensional Scale of Perceived Social Support (41). Each item included a statement related to the availability of social support from either —family or —a special person . Participants responded using a 7-point scale [1(strongly disagree) - 7 (strongly agree)]. Scores on the four items referring to family were summed to create the familial social support variable scores and scores on the four items referring to a special person were summed to create the social support from a special person variable scores.
Additional scales were included in the survey but did not perform well within the sample and, therefore, were not included in the analysis. Self-esteem was measured using the 10-item Rosenberg Self-Esteem scale (42) (Cronbach‘s alpha = .48). Orientation towards the future was measured using Bryan‘s 7-item scale (43, 44) (Cronbach‘s alpha = .10).
Data cleaning
All surveys were double data entered by project staff to ensure accuracy. Any discrepancies were reconciled by returning to the original survey for confirmation on the correct response. Missing and non-responsive (don't know) data were imputed using best-set regression(45) multiple imputation, which imputes data based on the best available subset of specified predictors (46). To protect against imputing truly non-responsive surveys (e.g., participants who dropped out halfway through the survey), a two-stage data validity check was put into place. At the first step, each case was required to have valid data for at least 50% of all of the variables in the dataset that were assessed for all participants. This permissive requirement was applied to identify youth who seemed truly unwilling to provide a necessary amount of data needed to support valid imputation, while also retaining as many respondents as possible. Based on this criterion, 20 respondents were dropped. At the second step, responsivity within each scale was examined. Variables within scales were imputed only for those cases that had valid data for at least 80% of those variables. This threshold is one that has been used by the research team in previous research [47–49]. Ten respondents were dropped at this step because they did not meet the data criterion for any of the variables reflecting the main components of the IMB model. This two-stage effort maximized the amount of data available for analyses. For example, if the entire sample had been subjected to an 80% valid data requirement across the entire survey, more than half of respondents would have been dropped. The final analytical sample size was 360 (390–30).
Data Analysis
A structural equation modeling (SEM) package, i.e., Analysis of Moment Structures (AMOS) (50),was used to estimate the hypothesized meditational model. The covariances among the indicators of motivation to engage in HIV preventive behavior (e.g., subjective norms regarding using condoms and talking to partner about safer sex and behavioral intentions regarding abstaining from sex) were included in the model and estimated. An initial model was estimated to examine the utility of the covariates (e.g., perceived health and age of first sex) in predicting behavioral skills and frequency of condom use. Paths determined to be zero, (i.e., those that did not statistically significantly predict frequency of condom use, p > .05), were eliminated from the model.
Following identification of the trimmed model, it was tested for variance by biological sex using multiple-group analysis and a chi-square difference test comparing the unconstrained model to the constrained model (i.e., where all model parameters were constrained to be invariant by biological sex). Finally, we used the Sobel test (51) to determine if the indirect, mediated, paths from the putative causal variables to the main outcome of frequency of condom use were statistically significant.
The statistical model included only a structural model (i.e., detailing the paths between measured variables), not a hybrid model containing both a structural model and a measurement model (i.e., detailing latent variables). This type of model is a relatively simple model to test and therefore requires a relatively small sample size. According to Kline (52), a sample size of 360 (as used in the current study) is large and is adequate for the proposed analysis.
RESULTS
The majority of participants were male (73.8%) versus female, and were boarding (84.1%) rather than day students. Mean age was 15.4 years. The subsample included 23% S1early, 27% S2late, 34% S3late, and 15% S4late students.
Bivariate associations between variables
As shown in Table 4, the average age at first sex was 12.7 years. Less than one in three (29%) reported talking with their first partner about using condoms. Interestingly, females were significantly more likely than males to report discussing condoms with their first partner (41% vs. 25%, respectively) t(319) = −2.72, p = .007. Although sex with an adult seems uncommon (9% of youth reported a current sexual relationship with someone more than five years older than them), transactional sex is reported by almost one in three youth (29%). It should be noted that in both cases, females were significantly more likely to report these relationships compared to males (21% vs. 4%; and 49% vs. 21%, respectively) t(248) = −4.56, p < .001 and t(284) = −5.19, p < .001, respectively.
Table 4.
Description of participants and overall differences by biological sex and condom use
| Characteristics | Comparisons by biological sex
|
Comparisons by frequency of condom use
|
|||
|---|---|---|---|---|---|
| Total | Males | Females | Never use condoms | Use condoms at least some times | |
| Main outcome (mean) | |||||
| Frequency of condom use | 1.2 | 1.2 | 1.3 | 0 | 2.5~ |
| IMB Model | Mean | Mean | Mean | Mean | Mean |
| HIV related information | 59.3 | 60.1 | 56.9 | 58.8 | 61.6 |
| Subjective norms regarding using condoms and talking to partner about safer sex | 15.6 | 15.2 | 16.7 | 13.4 | 17.7~ |
| Subjective norms regarding having condoms available to use | 6.9 | 6.9 | 6.7 | 5 | 8.7~ |
| Behavioral intentions regarding using condoms and talking to partner about safer sex | 8.6 | 8.6 | 8.6 | 7.4 | 9.9~ |
| Behavioral skills regarding having and using condoms | 12 | 12.1 | 11.8 | 10 | 13.9~ |
| Cultural and social aspects of HIV preventive behavior | |||||
| Age at first sex (Mean) | 12.7 | 12.7 | 12.9 | 11.8 | 13.9~ |
| Talked to first sexual partner about using condomsa | 29 | 25 | 41.0* | 7 | 52.0~ |
| Willingness to have sex the first time had sex (Mean) | 1.3 | 1.5 | 0.8* | 1.2 | 1.5~ |
| Most recent partner is more than 5 years older a | 8.8 | 4 | 21.4* | 7.6 | 9.9 |
| Transactional sexa | 29 | 21 | 49.0* | 27 | 35 |
| Perceived physical health (Mean) | 2.2 | 2.2 | 2.3 | 2.2 | 2.3 |
| Social support from family (Mean) | 12.8 | 12.8 | 12.8 | 12.7 | 12.9 |
| Social support from special person (Mean) | 11.8 | 11.8 | 11.8 | 11.5 | 12.1 |
| Sexual self-agency (Mean) | 12 | 11.7 | 12.9* | 11.6 | 12.4 |
Means reflect percent of participants who responded in the affirmative.
Statistically significant difference by gender at p ≤ .05.
Statistically significant difference by never use/use condoms at p ≤ .05.
Results of path analysis
Model building
Only sexual self-agency statistically significantly predicted behavioral skills related to having and using condoms. Three of the nine covariates expected to predict frequency of condom use were found to be statistically significantly related to condom use: age at first sex, discussion of using condoms with first sex partner, and willingness at first sexual intercourse. Consequently, these paths were retained in the model; the ones determined to be zero were eliminated.
The chi-square difference test indicated that the model did not vary by biological sex, χ2(13) = 6.23, p = .937. As such, the hypothesized model was estimated for the entire sample without sub-grouping by biological sex.
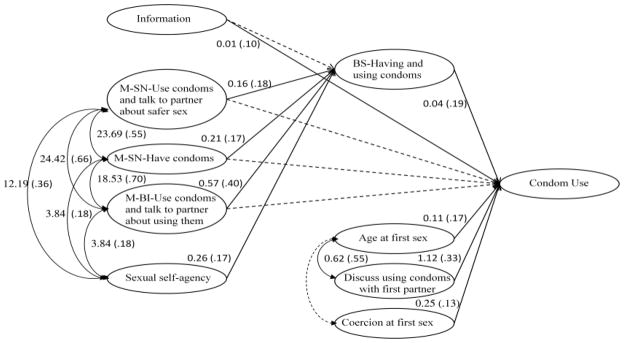
The final model fit the data well, χ2(24, N = 390) = 52.71, p< .001, Comparative Fit Index was 0.97, and Root Mean Square Error of Approximation was .06. Unstandardized and standardized path coefficients are shown in Figure 1.
Figure 1.
IMB Model Predicting Condom Use.
Statistically significant paths are indicated by solid lines. Unstandardized (standardized, or beta) weights are presented for statistically significant directional paths only. Covariances (correlations) are presented for statistically significant curved paths only.
M=Motivation
SN=Subjective norm
BI=Behavioral intention
BS=Behavioral skills
HIV preventive behavioral skills
Behavioral skills regarding having and using condoms positively predicted condom use directly, Z = 2.49, p = .013. As behavioral skills increased, use of condoms increased.
HIV preventive information
Information positively predicted condom use directly, Z = 2.09, p= .036. However, it did not indirectly predict condom use through behavioral skills as it did not predict behavioral skills.
HIV preventive motivation
None of the components of motivation predicted condom use directly. Behavioral intentions regarding using condoms and talking to one‘s partner about safer sex did, however, predict condom use indirectly through behavioral skills. Behavioral intentions predicted behavioral skills, Z = 5.97, p< .001, which in turn predicted condom use. The Sobel test (51) indicated that this mediating effect was statistically significant, Z = 2.19, p = .029.
Although both subjective norms for using condoms and talking to one‘s partner about using condoms, and subjective norms regarding having condoms available for use positively predicted behavioral skills (Z = 2.93, p = .003 and Z = 2.76, p = .006, respectively), they did not predict condom use through behavioral skills. The Sobel test (51) indicated that these mediating effects were unreliable, Z = 1.86, p = .063 and Z = 1.80, p = .072, respectively.
Characteristics of the sexual experience
Three of the characteristics of the sexual experience positively predicted condom use directly: 1) age at first sex, Z = 2.96, p = .003; 2) discussion of using condoms at first sex, Z = 5.76, p< .001; and 3) willingness at first sexual intercourse, Z = 2.64, p = .008.
Sexual self-agency did not predict condom use directly. However, it did predict condom use indirectly through behavioral skills, Z = 3.58, p< .001. The Sobel test (51) indicated that this mediating effect was statistically significant, Z = 1.97, p = .049.
In addition, also shown in Figure 1, sexual self agency is positively correlated with each of the three components of motivation. Furthermore, age at first sex is strongly and positively correlated with discussing using condoms at first sex. Contrary to expectations, age at first sex was not correlated with willingness at first sex.
DISCUSSION
Among secondary school students in Mbarara, Uganda who report a history of sexual intercourse, the Information, Motivation, and Behavioral Skills Model is partially able to predict frequency of current condom use. Consistent with previous research in resource-limited settings (16, 19, 20) as well as the United States (53, 54), behavioral skills to use condoms is positively and significantly associated with frequency of condom use. It should be noted however, that the measure in the current study reflects one‘s appraisal of how difficult or easy it would be to use condoms, rather than an objective measure of one‘s ability to enact correct condom use. Nonetheless, its association with the frequency of condom use highlights the need for HIV prevention programs, particularly those for adolescents, to focus on providing specific and actionable information on how to use condoms to positively affect related behavioral skills.
Motivation is not directly related to frequency of condom use among sexually active adolescents in the current study sample. While unexpected given previous research in resource-limited settings (16, 19, 20), and the United States (54), this finding is consistent with some previous studies among adults (16, 18). Behavioral intentions to use condoms and talk to one‘s partner about using condoms are indirectly associated with the outcome however, through behavioral skills. Given the strength of association among subjective norms and behavioral intentions (rs of .66 and .70), and between these aspects of motivation and behavioral skills (βs of .18, .17, and .40), the clinical importance of subjective norms is strongly suggested in the model despite its lack of statistical significance. This is supported by findings from a prospective study of men who have sex with men (MSM) in Switzerland, in which subjective norms were the only component of the IMB Model that predicted increased condom use. Factors such as drug use, low social support from friends, and a high satisfaction with one‘s sexuality were more influential (55).
It has been posited that HIV information may be more influential in settings where information is uniformly low (16). Although this is unsupported by most previous research in resource-limited settings (16, 18–20), information is directly associated with condom use in the current study. It is not a particularly strong association, however, and it is the lowest beta weight in the model (.10). Consistent with the findings reported by Yang et al. (19) among female Chinese entertainment workers, we expected also that information would be indirectly related to condom use. This expectation was not supported by the data. Together, these findings suggest that information is important in affecting condom use but is perhaps not the most central component driving the model.
A recent review of behavioral interventions that reduce HIV risk among MSM reports that having a theoretical model is associated with significant outcomes whereas not having a theoretical model is associated with non-significant outcomes (3); but the specific theoretical model seems to be less influential. Reviews of the IMB model can be found elsewhere (9, 56). Our data suggest that the IMB Model may be partially useful as a guide in developing an HIV prevention program for school-attending adolescents in Uganda, but that additional factors also need to be taken into account.
Influences of the sexual experience
Consistent with work in South Africa (21), one‘s first sexual experience is hugely influential on one‘s current condom use behavior in the current study sample. Age at first sex, willingness at first sex (as opposed to coercion (22–32)), and having discussed using condoms with one‘s first sex partner are positively associated with frequency of condom use among adolescent respondents. Indeed, similar to the South Africa findings (21), discussing condoms with one‘s first sex partner is by far the strongest predictor of condom use behavior in the model. This highlights the importance of intervention programs that target youth before they are sexually active to teach them communication skills so that they can have a conversation about condoms with their first partner. Clearly, in addition to behavioral skills related to condom use, communication skills to talk about condoms need to be a key component of adolescent-focused HIV prevention programs in Uganda (57).
Other potentially influential factors
Contrary to expectations, social support either from one‘s family or a special person‘ is not predictive of frequency of condom use among sexual active adolescents in our study sample. This is in contrast to social norms, which center on one‘s peers‘ attitudes and beliefs about condoms, which are predictive of HIV preventive behavioral skills. Thus, in our sample, it seems less important whether an adolescent feels like he or she has support from family and friends on emotional matters, and more important that peers with whom they surround themselves endorse condom use.
Physical health status also appears to be unrelated to frequency of condom use among Mbararan youth in the current survey. This suggests that even youth who have poor health (e.g., HIV, other chronic diseases) are equally likely to engage in HIV protective sexual behavior.
Perhaps even more surprising given the difference in some sexual risk behaviors by biological sex (e.g., number of sex partners in the past year, use of condom at last sex (2)) is that both boys and girls who participated in the survey have the same predictors of condom use and that these predictors affect boys‘ and girls‘ use of condoms similarly. Although intervention content should be tailored by biological sex so that it is salient and personally relevant, these findings suggest that the intervention components should be the same for adolescent boys and girls.
Transactional sex is unrelated to the outcome in the current analyses; the high prevalence rate bears noting, however. Almost half (49%) of sexually active females and one in five sexually active males (21%) who took part in the survey report receiving something such as money, gifts, clothes, or a mobile phone in order to have sex at some point in their lives. This high percentage of involved youth is mirrored by a national study of 12–19 year olds where 75% of Ugandan females and 35% of males reported receiving money or materials for sex (25). Our rates may be comparatively lower because we focused on a school-based sample versus their community-based sample. The most common goods exchanged in Moore et al.‘s study were money, clothes, and jewelry and cosmetics. As in our study, in the national study, transactional sex was unrelated to the likelihood of unprotected sex (25). Moore et al.‘s focus group data revealed that the exchange of gifts can be coercive, or non-coercive as part of a relationship where girls demand gifts (25). There are some data to suggest that transactional sex is associated with negative outcomes (25, 58–60): it is concurrently associated with depressive sympotomatology in adults (61); and transactional sex motivated by food insecurity increases the likelihood of risky sex (62). Thus, regardless of whether transactional sex is directly related to condom use, adolescent HIV prevention programs should integrate a discussion of gift giving, and examples of healthy (non-coercive) and unhealthy (coercive, transactional) exchanges of goods within and outside of sexual relationships. These findings also indicate the need for structural interventions, such as economic development, facilitating food security, engaging with patriarchy, and enhancing egalitarian gender dynamics.
Limitations
Findings should be interpreted within the context of study limitations. First, data are from five purposefully chosen secondary schools in Mbarara, Uganda. How these data generalize to other sub-Saharan African countries or even greater Uganda, and youth not enrolled in secondary schools is unknown. Second, sexual behavior is highly stigmatized among adolescents in Uganda. It is possible that some youth misreported their sexual activity, leading to an underestimate of the true level of sexual activity among respondents. Similarly, given the stigma associated with condom use, it is possible that self-reports of this behavior were over- or under-reported.
CONCLUSIONS
Similar to previous examinations of the IMB model in resource-limited settings (16, 18–20), data support partial applicability of the model for frequency of condom use among sexually active secondary school students in Mbarara, Uganda. Specifically, HIV prevention programs aimed at increasing condom use among adolescents who are sexually active should be especially focused on providing behavioral skills related to using condoms. This includes not just clear and specific instructions on accurate use, but also communication skills to talk about condoms with one‘s partner. Also, given that age at first sex is strongly associated with current condom use, intervention programs should not only include abstinent youth in their programming but should include behavioral skills for these youth.
Acknowledgments
The project described was supported by Award Number R01MH080662 from the National Institute of Mental Health. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute of Mental Health or the National Institutes of Health. We would like to thank the entire CyberSenga Study team from Internet Solutions for Kids, Internet Solutions for Kids – Uganda, Mbarara University of Science and Technology, the University of Colorado, and Harvard University, who contributed to the planning and implementation of the study. Finally, we thank the schools and the students their time and willingness to participate in this study.
Footnotes
In the first school the survey was fielded, students were not matched to the recruitment list to protect anonymity. This process was subsequently changed after it was discovered that youth not on the list had shown up, provided assent, and completed the survey. Because the surveys were completely blind to protect participants' anonymity; it was impossible to identify the errant surveys. Although we could have randomly deleted 17 surveys, we chose to keep all completed surveys to maximize the amount of data available.
References
- 1.Government of Uganda. UNGASS Country Progress Report Uganda: January 2008-December 2009. Available at: http://data.unaids.org/pub/Report/2010/uganda_2010_country_progress_report_en.pdf.
- 2.Biraro S, Shafer LA, Kleinschmidt I, et al. Is sexual risk taking behaviour changing in rural south-west Uganda? Behaviour trends in a rural population cohort 1993–2006. Sex Transm Infect. 2009;85(Suppl 1):i3–i11. doi: 10.1136/sti.2008.033928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Johnson WD, Diaz RM, Flanders WD, et al. Behavioral interventions to reduce risk for sexual transmission of HIV among men who have sex with men. Cochrane Database Syst Rev. 2008;(3):Article No. CD001230. doi: 10.1002/14651858.CD001230.pub2. [DOI] [PubMed] [Google Scholar]
- 4.Centers for Disease Control and Prevention. Compendium of HIV Prevention Interventions with Evidence of Effectiveness from CDC's HIV/AIDS Prevention Research Synthesis Project. Atlanta, GA: Centers for Disease Control and Prevention; Available at: http://www.cdc.gov/hiv/resources/reports/hiv_compendium/index.htm. [Google Scholar]
- 5.Bandura A. Social Foundations of Thought and Action: A Social Cognitive Theory. Englewood Cliffs, NJ: Prentice Hall; 1986. [Google Scholar]
- 6.Azjen I, Fishbein M. Understanding attitudes and predicting social behavior. Englewood Cliffs, NJ: Prentice Hall; 1980. [Google Scholar]
- 7.Azjen I. From intentions to actions: A theory of planned behavior. In: Kuhl J, Beckman J, editors. Action-control: From cognition to behavior. Heidelberg, Germany: Springer; 1985. pp. 11–39. [Google Scholar]
- 8.Fisher JD, Fisher WA. Changing AIDS-risk behavior. Psychol Bull. 1992;111:455–74. doi: 10.1037/0033-2909.111.3.455. [DOI] [PubMed] [Google Scholar]
- 9.Fisher JD, Fisher WA. Theoretical approaches to individual-level change in HIV risk behavior. In: Peterson JL, DiClemente RJ, editors. Handbook of HIV prevention. New York, NY: Kluwer Academic/Plenum Press; 2000. pp. 3–55. [Google Scholar]
- 10.Prochaska JO, Redding CA, Harlow LL, Rossi JS, Velicer WF. The transtheoretical model of change and HIV prevention: a review. Health Educ Q. 1994 Winter;21(4):471–86. doi: 10.1177/109019819402100410. [DOI] [PubMed] [Google Scholar]
- 11.Rosenstock IM. Historical origins of the health belief model. Health Educ Monogr. 1974;2(4):328–35. doi: 10.1177/109019817800600406. [DOI] [PubMed] [Google Scholar]
- 12.Rogers EM. Diffusion of innovations. New York, NY: Free Press; 1995. [Google Scholar]
- 13.Wingood GM, DiClemente RJ. Application of the theory of gender and power to examine HIV-related exposures, risk factors, and effective interventions for women. Health Educ Behav. 2000;27(5):539–65. doi: 10.1177/109019810002700502. [DOI] [PubMed] [Google Scholar]
- 14.Fisher JD, Fisher WA, Williams SS, Malloy TE. Empirical tests of an information-motivation-behavioral skills model of AIDS-preventive behavior with gay men and heterosexual university students. Health Psychol. 1994;13(3):238–50. doi: 10.1037//0278-6133.13.3.238. [DOI] [PubMed] [Google Scholar]
- 15.Fisher JD, Fisher WA, Bryan AD, Misovich SJ. Information-motivation-behavioral skills model-based HIV risk behavior change intervention for inner-city high school youth. Health Psychol. 2002;21(2):177–86. [PubMed] [Google Scholar]
- 16.Bryan AD, Fisher JD, Benziger TJ. HIV prevention information, motivation, behavioral skills and behaviour among truck drivers in Chennai, India. AIDS. 2000;14(6):756–8. doi: 10.1097/00002030-200004140-00021. [DOI] [PubMed] [Google Scholar]
- 17.Linn JG, Garnelo L, Husaini BA, Brown C, Benzaken AS, Stringfield YN. HIV prevention for indigenous people of the Amazon basin. Cell Mol Biol (Noisy-le-grand) 2001;47(6):1009–15. [PubMed] [Google Scholar]
- 18.Kalichman SC, Simbayi LC, Cain D, Jooste S, Skinner D, Cherry C. Generalizing a model of health behaviour change and AIDS stigma for use with sexually transmitted infection clinic patients in Cape Town, South Africa. AIDS Care. 2006;18(3):178–82. doi: 10.1080/09540120500456292. [DOI] [PubMed] [Google Scholar]
- 19.Yang X, Xia G, Li X, Latkin C, Celentano D. Social influence and individual risk factors of HIV unsafe sex among female entertainment workers in China. AIDS Educ Prev. 2010;22(1):69–86. doi: 10.1521/aeap.2010.22.1.69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Maticka-Tyndale E, Tenkorang EY. A multi-level model of condom use among male and female upper primary school students in Nyanza, Kenya. Soc Sci Med. 2010;71(3):616–25. doi: 10.1016/j.socscimed.2010.03.049. [DOI] [PubMed] [Google Scholar]
- 21.Hendriksen ES, Pettifor A, Lee SJ, Coates T, Rees H. Predictors of condom use among young adults in South Africa: The Reproductive Health and HIV Research Unit National Youth Survey. Am J Public Health. 2007;97(7):1241–8. doi: 10.2105/AJPH.2006.086009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Koenig MA, Zablotska I, Lutalo T, Nalugoda F, Wagman J, Gray R. Coerced first intercourse and reproductive health among adolescent women in Rakai, Uganda. Int Fam Plan Perspect. 2004;30(4):156–63. doi: 10.1363/3015604. [DOI] [PubMed] [Google Scholar]
- 23.Kalichman SC, Simbayi LC. Sexual assault history and risks for sexually transmitted infections among women in an African township in Cape Town, South Africa. AIDS Care. 2004;16(6):681–9. doi: 10.1080/09540120410331269530. [DOI] [PubMed] [Google Scholar]
- 24.Varga C. How gender roles influence sexual and reproductive health among South African adolescents. Stud Fam Plann. 2003;34(3):160–72. doi: 10.1111/j.1728-4465.2003.00160.x. [DOI] [PubMed] [Google Scholar]
- 25.Moore A, Biddlecom A, Zulu E. Prevalence and meanings of exchange of money or gifts for sex in unmarried adolescent sexual relationships in sub-Saharan Africa. Afr J Reprod Health. 2007;11(3):44–61. [PMC free article] [PubMed] [Google Scholar]
- 26.Ajuwon A. Attitudes, norms and experiences of sexual coercion among young people in Ibadan, Nigeria. In: Jejeebhoy S, Shah I, Thapa S, editors. Sex without consent: Young people in developing countries. New York: Zed Books; 2005. pp. 96–104. [Google Scholar]
- 27.Erulkar A. The experience of sexual coercion among young people in Kenya. Int Fam Plan Perspect. 2004;30(4):182–9. doi: 10.1363/3018204. [DOI] [PubMed] [Google Scholar]
- 28.Dunkle KL, Jewkes RK, Brown HC, Gray GE, McIntryre JA, Harlow SD. Gender-based violence, relationship power, and risk of HIV infection in women attending antenatal clinics in South Africa. Lancet. 2004;363(9419):1415–21. doi: 10.1016/S0140-6736(04)16098-4. [DOI] [PubMed] [Google Scholar]
- 29.Luke N, Kurz KM. Cross-generational and transactional sexual relations in Sub-Saharan Africa: Prevalence of behavior and implications for negotiating safer sexual practices. Washington, DC: International Center for Research on Women, Population Services International; 2002. [Google Scholar]
- 30.Campbell JC, Baty ML, Ghandour RM, Stockman JK, Francisco L, Wagman J. The intersection of intimate partner violence against women and HIV/AIDS: a review. Int J Inj Contr Saf Promot. 2008;15(4):221–31. doi: 10.1080/17457300802423224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Jewkes R, Morrell R. Gender and sexuality: emerging perspectives from the heterosexual epidemic in South Africa and implications for HIV risk and prevention. J Int AIDS Soc. 2010;13(1):6. doi: 10.1186/1758-2652-13-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Maman S, Yamanis T, Kouyoumdjian F, Watt M, Mbwambo J. Intimate partner violence and the association with HIV risk behaviors among young men in Dar es Salaam, Tanzania. J Interpers Violence. 2010;25(10):1855–72. doi: 10.1177/0886260509354498. [DOI] [PubMed] [Google Scholar]
- 33.Puffer E, Meade C, Drabkin A, Broverman S, Ogwang-Odhiambo R, Sikkema K. Individual- and family-level psychosocial correlates of HIV risk behavior among youth in rural Kenya. AIDS Behav. 2010;15(6):1264–74. doi: 10.1007/s10461-010-9823-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Uganda Bureau of Statistics (UBOS) 2005 Statistical Abstract. Kampala: Uganda Bureau of Statistics; 2005. [Google Scholar]
- 35.Intersol Inc. Languages of Africa. Brea, CA: Intersol, Inc; Available at: http://www.intersolinc.com/newsletters/africa.htm. [Google Scholar]
- 36.Misovich SJ. The Teen Health Survey. Storrs, CT: Center for Health, Intervention, and Prevention, University of Connecticut; Available at: http://www.chip.uconn.edu/research/measurement-instruments/ [Google Scholar]
- 37.Uganda Bureau of Statistics (UBOS), ORC Macro. Uganda Demographic and Health Survey 2006. Calverton, MD: UBOS and Macro International Inc; Available at: http://www.measuredhs.com/publications/publication-FR194-DHS-Final-Reports.cfm. [Google Scholar]
- 38.Bryan A, Schindeldecker MS, Aiken LS. Sexual self-control and male condom-use outcome beliefs: Predicting heterosexual men's condom-use intentions and behavior. J Appl Soc Psychol. 2001;31(9):1911–38. [Google Scholar]
- 39.Bryan AD, Aiken LS, West SG. Young women's condom use: The influence of acceptance of sexuality, control over the sexual encounter, and perceived susceptibility to common STDs. Health Psychol. 1997;16(5):468–79. doi: 10.1037//0278-6133.16.5.468. [DOI] [PubMed] [Google Scholar]
- 40.Ware JE, Kosinski M. SF-36 Physical and Mental Health Summary Scales: A Manual for Users of Version 1. Lincoln, RI: QualityMetric Inc; 2001. [Google Scholar]
- 41.Zimet GD, Dahlem NW, Zimet SG, Farley GK. The Multidimensional Scale of Perceived Social Support. J Pers Assess. 1988;52(1):30–41. doi: 10.1080/00223891.1990.9674095. [DOI] [PubMed] [Google Scholar]
- 42.Rosenberg M. Society and the adolescent self-image. Princeton, NJ: Princeton University Press; 1965. [Google Scholar]
- 43.Whitaker DJ, Miller KS, Clark LF. Reconceptualizing adolescent sexual behavior: Beyond did they or didn't they? Fam Plann Perspect. 2000;32(3):111–7. [PubMed] [Google Scholar]
- 44.Bryan A, Kagee A, Broaddus M. Condom use among South African adolescents: Developing and testing theoretical models of intentions and behavior. AIDS Behav. 2006;10(4):387–97. doi: 10.1007/s10461-006-9087-5. [DOI] [PubMed] [Google Scholar]
- 45.StataCorp. Stata Statistical Software. Release 11. College Station, TX: StataCorp LP; 2009. [Google Scholar]
- 46.Rubin DB. Multiple imputation for nonresponse in surveys. New York, NY: John Wiley and Sons, Inc; 1987. [Google Scholar]
- 47.Ybarra ML, Mitchell KJ. Youth engaging in online harassment: Associations with caregiver-child relationships, Internet use, and personal characteristics. J Adolesc. 2004;27(3):319–36. doi: 10.1016/j.adolescence.2004.03.007. [DOI] [PubMed] [Google Scholar]
- 48.Ybarra M, Mitchell K, Wolak J, Finkelhor D. Examining characteristics and associated distress related to Internet harassment: Findings from the Second Youth Internet Safety Survey. Pediatrics. 2006;118(4):e1169–e77. doi: 10.1542/peds.2006-0815. [DOI] [PubMed] [Google Scholar]
- 49.Ybarra ML, Espelage DL, Mitchell KJ. The co-occurrence of Internet harassment and unwanted sexual solicitation victimization and perpetration: Associations with psychosocial indicators. J Adolesc Health. 2007;41(6 Suppl 1):S31–41. doi: 10.1016/j.jadohealth.2007.09.010. [DOI] [PubMed] [Google Scholar]
- 50.Arbuckle JL. Amos user's guide. Chicago, IL: Small Waters; 1997. [Google Scholar]
- 51.Sobel ME. Asymptotic confidence intervals for indirect effects in structural models. In: Leinhardt S, editor. Sociological methodology. San Francisco, CA: Jossey-Bass; 1982. pp. 290–312. [Google Scholar]
- 52.Kline RB. Principles and practice of structural equation modeling. 3. New York, NY: Guildford Press; 2011. [Google Scholar]
- 53.Walsh J, Senn T, Scott-Sheldon L, Vanable P, Carey M. Predicting condom use using the Information-Motivation-Behavioral Skills (IMB) model: A multivariate latent growth curve analysis. Ann Behav Med. 2011;42(2):235–44. doi: 10.1007/s12160-011-9284-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Anderson ES, Wagstaff DA, Heckman TG, et al. Information-Motivation-Behavioral Skills (IMB) Model: Testing direct and mediated treatment effects on condom use among women in low-income housing. Ann Behav Med. 2006;31(1):70–9. doi: 10.1207/s15324796abm3101_11. [DOI] [PubMed] [Google Scholar]
- 55.Nideröst S, Gredig D, Roulin C, Rickenbach M Swiss HIV Cohort Study, Eurosupport 5 Study Group. Predictors of HIV-protection behaviour in HIV-positive men who have sex with casual male partners: a test of the explanatory power of an extended Information-Motivation-Behavioural Skills model. AIDS Care. 2011;23(7):908–19. doi: 10.1080/09540121.2010.538661. [DOI] [PubMed] [Google Scholar]
- 56.Fisher JD, Fisher WA, Shuper PA. The Information-Motivation-Behavioral Skills model of HIV preventive behavior. In: DiClemente R, Crosby R, Kegler M, editors. Emerging theories in health promotion practice and research. San Francisco, CA: Jossey Bass Publishers; 2009. pp. 22–63. [Google Scholar]
- 57.MacPhail C, Pettifor A, Pascoe S, Rees H. Predictors of dual method use for pregnancy and HIV prevention among adolescent South African women. Contraception. 2007;75(5):383–9. doi: 10.1016/j.contraception.2006.12.020. [DOI] [PubMed] [Google Scholar]
- 58.Moore AM, Awusabo-Asare K, Madise N, John-Langba J, Kumi-Kyereme A. Coerced first sex among adolescent girls in sub-Saharan Africa: Prevalence and context. Afr J Reprod Health. 2007;11(3):62–82. [PMC free article] [PubMed] [Google Scholar]
- 59.Råssjö E-B, Kiwanuka R. Views on social and cultural influence on sexuality and sexual health in groups of Ugandan adolescents. Sex Reprod Healthc. 2010;1(4):157–62. doi: 10.1016/j.srhc.2010.08.003. [DOI] [PubMed] [Google Scholar]
- 60.Wagman J, Baumgartner JN, Waszak Geary C, et al. Experiences of sexual coercion among adolescent women. J Interpers Violence. 2009;24(12):2073–95. doi: 10.1177/0886260508327707. [DOI] [PubMed] [Google Scholar]
- 61.Nduna M, Jewkes R, Dunkle K, Shai N, Colman I. Associations between depressive symptoms, sexual behaviour and relationship characteristics: a prospective cohort study of young women and men in the Eastern Cape, South Africa. J Int AIDS Soc. 2010;13(1):44. doi: 10.1186/1758-2652-13-44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Miller C, Bangsberg D, Tuller D, et al. Food insecurity and sexual risk in an HIV endemic community in Uganda. AIDS Behav. 2011;15(7):1512–9. doi: 10.1007/s10461-010-9693-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Bandura A. Self-Efficacy: The exercise of control. New York, NY: W.H. Freeman; 1997. [Google Scholar]
- 64.Fisher JD, Fisher WA, Misovich SJ, Kimble DL, Malloy TE. Changing AIDS risk behavior: Effects of an intervention emphasizing AIDS risk reduction information, motivation, and behavioral skills in a college student population. Health Psychol. 1996;15(2):114–23. doi: 10.1037//0278-6133.15.2.114. [DOI] [PubMed] [Google Scholar]