Abstract
Purpose
The treatment of unstable slipped capital femoral epiphysis (SCFE) remains controversial. Surgical dislocation and open reduction has the potential to significantly reduce the rate of avascular necrosis (AVN) by allowing direct preservation of the femoral head blood supply. The purpose of this study was to determine if open reduction of the unstable SCFE by means of surgical hip dislocation reduced the risk of AVN compared with closed reduction and percutaneous pinning.
Methods
We reviewed the medical records and radiographs of patients treated at our institution between the years 2000 and 2008. Sex, age, side of slip, precipitating event, pre- and post-operative anterior physeal separation (APS) and slip angle, slip severity, time between inciting event and surgical treatment, number of screws used, development of AVN, and need for subsequent surgery were evaluated. Statistical analysis was performed to compare risk factors and occurrence of AVN.
Results
From 2004 to 2008, we treated 12 patients with unstable SCFEs: six had closed reduction and percutaneous pinning and six underwent open reduction by means of surgical hip dislocation. There were no statistically significant differences between the two groups regarding sex, age, slip angle, APS, time to surgery, and AVN rate. At follow-up, 4 (66.7 %) patients had AVN in the group which had open reduction, while 2 (33.3 %) patients had AVN in the group which underwent closed reduction. (p = 0.57).
Conclusions
Open reduction of the unstable SCFE by means of surgical dislocation of the hip does not decrease the rate of AVN when compared to closed reduction.
Keywords: Slipped capital femoral epiphysis, Closed reduction, Open reduction, Surgical dislocation of the hip, Percutaneous pinning, Avascular necrosis
Introduction
Slipped capital femoral epiphysis (SCFE) is a common hip disorder of unclear etiology that affects adolescents, with an incidence of 0.2 (Japan) to 10 (United States) per 100,000 [1]. According to Loder et al., patients with unstable SCFE have such severe pain that weight-bearing is not possible, even with crutches [2, 3]. The risk of avascular necrosis (AVN) of the femoral head, the most significant complication following an SCFE, is increased in patients with unstable slips and also by the physeal separation, defined as the amount of separation of the anterior lip of the epiphysis from the metaphysis on the frog lateral view [4]. Other factors possibly playing a role in the development of AVN include the delay from presentation to surgery, capsular decompression, and surgical technique. The treatment of unstable SCFE is controversial [5], ranging from closed reduction and percutaneous pinning [6, 7], open reduction, and smooth Kirschner wire fixation [8] to open reduction with subcapital correction osteotomy by means of surgical hip dislocation [9–12]. This latter approach has the potential to eliminate or reduce the risk of AVN due to direct preservation of the femoral head blood supply.
The purpose of this study was to determine if open reduction with subcapital correction osteotomy of the unstable SCFE by means of surgical hip dislocation was better than closed reduction and percutaneous pinning for preventing the development of AVN.
Methods
Ethics Review Board approval was obtained to review the medical records and radiographs of all patients with an unstable SCFE treated at our institution between the years 2000 and 2008.
Patients with unstable SCFEs were identified based on their inability to bear weight, as per Loder’s definition: slips were considered to be unstable when the patient had such severe pain that weight-bearing was not possible, even with crutches [2, 3]. We only included in this study patients with truly unstable SCFEs. Intra-operatively, free motion was observed between the femoral head and neck, either under live fluoroscopy or at the time of open reduction. Patients undergoing open reduction through means of surgical dislocation had an active role in selecting this treatment, as they were also given the option of undergoing closed reduction and discussed the benefits and risks of both managements with their surgeon.
Descriptive variables were obtained from the patient’s medical records: sex, age at slip, side of slip, and inciting incident. Radiographic data were obtained from lateral and anteroposterior (AP) films: pre- and post-operative anterior physeal separation (APS) as described by Ballard et al. [4], pre- and post-operative slip angle (in degrees) as described by Southwick [13], and slip severity (grades 1, 2, and 3) as described by Boyer et al. [14]. APS was measured from the best lateral films available. Translation of the epiphysis on the metaphysis was measured as a percentage of the physeal width. AP and frog lateral radiographs from the post-operative visit closest to 6 weeks after surgery were used to measure the post-operative slip angle and translation percentage. Available follow-up images (radiographs, magnetic resonance images, bone scans) were reviewed to determine the presence or absence of AVN. AVN was confirmed by bone scan and defined as the lack of blood supply in an area of the femoral head. Other variables relating to the surgical treatment were: time (h) between inciting event and surgical treatment, number of screws used for fixation, development of AVN, need for subsequent surgery, and length (months) of follow-up.
Statistical analysis with SAS software (version 9.2) was used to determine whether the development of AVN was associated with either surgical procedure or with any risk factors previously identified by other authors, such as APS, slip angle and slip severity. Fisher’s exact test was used for categorical variables, whereas two-sided t-tests were used for continuous data. A p-value < 0.05 was considered to be significant.
Surgical techniques
For patients treated with closed reduction, the affected limb was gently positioned on the fracture table with the hip in extension, neutral abduction, and gentle internal rotation. The unaffected limb was positioned in a way as to allow image intensifier access to the affected hip. While positioning the patient on the fracture table, there was no attempt of forceful or anatomical reduction, but inadvertent reduction may have occurred. Percutaneous pinning with one fully threaded 7.3-mm screw was performed, under image intensifier guidance. We did not perform any capsulotomy or aspiration of the hip joint. Patients were instructed not to weight-bear until returning to the clinic at around 6 weeks after the surgery.
For patients treated with open reduction by means of surgical dislocation, the technique described by Ganz and Leunig was followed [11, 15, 16]. The patient was positioned on the lateral decubitus, with the affected limb freely draped and a sterile bag along the opposite side of the table to receive the leg during the dislocation of the hip. A straight lateral incision was performed, centered over the greater trochanter. The fascia lata was incised and the mobile tissue over the greater trochanter incised close to its dorsal edge. The posterior margin of the gluteus medius was superficially and carefully exposed, so that the posterosuperior tip of the greater trochanter and the tendinous insertions of the gluteus medius was seen and palpated. A trochanteric osteotomy was performed with an oscillating saw, so that a trochanteric fragment about 1.5 cm thick was mobilized. The tendinous origin of the vastus lateralis was undercut distally and a residual layer of gluteus medius fibers left intact at the tip of the trochanter, protecting the underlying piriformis tendon and, thus, the anastomosis between the inferior gluteal artery and the deep branch of the medial circumflex artery. The mobile trochanteric fragment was flipped anterosuperiorly. The capsule was exposed through dissection between the tendons of the piriformis and gluteus minimus. A Z-shaped capsulotomy was performed. The femoral epiphysis was stabilized by the insertion of 2 or 3 threaded Kirschner wires. Dislocation of the femoral head was gently performed, after cutting the ligamentum teres with scissors. The portion of the trochanter proximal to the visible growth plate was carefully mobilized with a chisel. A soft-tissue flap containing the retinaculum and external rotators was developed. The periosteum of the femoral neck was incised on the axis of the femoral neck and the dissection was then continued so that the posterior and anteromedial portions of the femoral neck were visualized. The threaded Kirschner wires were removed and the obviously unstable femoral epiphysis with its soft-tissue attachments was allowed to gently fall posteriorly, exposing the femoral neck. The posterior callus spur of the femoral neck was removed with an osteotome and a mild shortening of the femoral neck performed, using an oscillating saw. Residual growth plate tissue was removed from the femoral head with a curette. The head was aligned with the femoral neck, so that a proper offset is achieved. In two cases, fully threaded Kirschner wires were drilled through the fovea in a retrograde way, exiting in the lateral cortex, just below the greater trochanter. In four cases, according to the surgeon’s preference, a 7.3-mm fully threaded cannulated screw was used instead of one of the fully threaded Kirschner wires, as a mean of fixation. The periosteal flap and capsule were restored with Vicryl tension-free sutures. Refixation of the trochanter was achieved with 4.5-mm screws. The fascial layer was sutured and layer-by-layer reconstruction of the soft tissues performed. Patients were instructed not to weight-bear, adduct the hip, or flex it beyond 70° and to use crutches with toe-touch weight-bearing until coming to the clinic, approximately 6 weeks after the surgery. At this point, patients were advised to progressively bear weight and return to normal daily activities, as tolerated.
Results
From 2000 to 2008, we treated 189 patients diagnosed with SCFE. Of these, 12 patients (Table 1) had unstable SCFEs (2, 3) and received one of two treatments: six had closed reduction and percutaneous pinning and six underwent subcapital correction osteotomy by means of surgical hip dislocation (Table 2). There were three males and three females in each group.
Table 1.
Characteristics of the patients with unstable slipped capital femoral epiphysis (SCFE)
| Patient | Sex | Age at slip (years) | Side of acute SCFE | Inciting incident | Slip angle (°) | Severity | APS (mm) | Time to surgery (h) | Operative procedure | AVN | Follow-up (days) |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | F | 12 | R | Fall | 34 | 2 | 3 | 20 | Open reduction via surgical dislocation | No | 369 |
| 2 | F | 12 | R | Fall | 12 | 1 | 5.5 | 39 | Open reduction via surgical dislocation | Yes | 515 |
| 3 | M | 13 | R | Fall | 3 | 17 | Open reduction via surgical dislocation | Yes | 719 | ||
| 4 | F | 11 | L | Fall | 33 | 2 | 6.5 | 16 | Open reduction via surgical dislocation | Yes | 777 |
| 5 | M | 12 | L | Running | 50 | 2 | 9 | 18 | Open reduction via surgical dislocation | Yes | 789 |
| 6 | M | 15 | L | Walking up stairs | 56 | 3 | 12 | 23 | Open reduction via surgical dislocation | No | 510 |
| 7 | M | 9 | L | Fall | 3 | 56 | Closed reduction and percutaneous pinning | Yes | 2,063 | ||
| 8 | M | 11 | L | Fall | 32 | 2 | 4.5 | 13 | Closed reduction and percutaneous pinning | Yes | 1,651 |
| 9 | M | 14 | L | Fall | 28 | 1 | 10 | 8 | Closed reduction and percutaneous pinning | No | 915 |
| 10 | F | 11 | R | Fall | 14 | 1 | 1.5 | 39 | Closed reduction and percutaneous pinning | No | 2,301 |
| 11 | F | 14 | R | Fall | 47 | 2 | 8.5 | Closed reduction and percutaneous pinning | No | 1,337 | |
| 12 | F | 12 | L | Fall | 21 | Closed reduction and percutaneous pinning | No | 2,807 |
Table 2.
Comparison of patients who underwent surgical dislocation and patients who had closed reduction
| Patients with unstable SCFEs treated by means of surgical dislocation (n = 6) | Patients with unstable SCFEs treated by means of closed reduction (n = 6) | |
|---|---|---|
| Male:female | 3:3 | 3:3 |
| Age (years) | 12.5 (±1.4) | 11.8 (±1.9) |
| Slip angle | 37° (±17.17°) | 30,25° (±13.57°) |
| APS | 6.5 (±3.21°) | 4.75 (±3.71°) |
| Time to surgery | 22.16 h (±7.86 h) | 24.25 h (±7.86 h) |
| AVN | 4 | 2 |
In the group who underwent closed reduction, the mean age was 11.8 years. The average slip angle was 30.3° (±13.6°) and APS was 4.8° (±3.7°). The time between the injury (patient having a traumatic precipitating event) and surgery was 24.3 h (±7.9 h). Three different surgeons performed the surgeries. Post-operatively, two patients (33.3 %) had AVN and underwent removal of the hardware. No other procedure was needed for these two patients.
In the group who underwent open reduction by means of surgical dislocation, the mean age was 12.5 years. The average slip angle was 37.0° (±17.2°) and APS was 6.5° (±3.2°). The time between the injury (patient having a traumatic precipitating event) and surgery was 22.2 h (±7.9 h). In this group, four different surgeons performed the operations and, while none of them had previous experience with this specific procedure, except for training in the cadaver lab, all surgeons are pediatric orthopedic surgeons with extensive experience in pediatric and adolescent hip surgery. One femoral head was not bleeding at the time of the procedure. Four patients (66.7 %) had AVN.
In the group undergoing surgical dislocation, one patient (case 1) had a concomitant contralateral chronic SCFE, which was fixed in situ; two patients were diagnosed with a contralateral acute stable SCFE after 1 year (case 6) and after 1 year and 3 months (case 3), respectively and also underwent in situ fixation.
We could not find any statistically significant difference between the two groups for sex, age, slip angle, APS, and time between injury and surgery. Although four patients (66.7 %) had AVN in the group who underwent surgical hip dislocation, compared to two patients (33.3 %) in the group who had closed reduction, this difference was not statistically significant. (p = 0.57).
Complications
In the group who had surgical hip dislocation, one patient (case 1) returned to the operative room after 2 months for a revision of the fixation, as one Kirschner wire had broken (Fig. 1). This was partially removed and a 7.3-mm screw was put in. This patient had no AVN. One patient (case 3) fell down while in the hospital, 5 days after surgery, and the K-wire and screw used for fixation was bent. After 9 months, the screw and K-wire were broken and there was evident re-displacement between the epiphysis and femoral neck. This patient underwent new surgical dislocation and revision of fixation. At this point, the femoral head was not bleeding intra-operatively and the patient went on to have AVN.
Fig. 1.
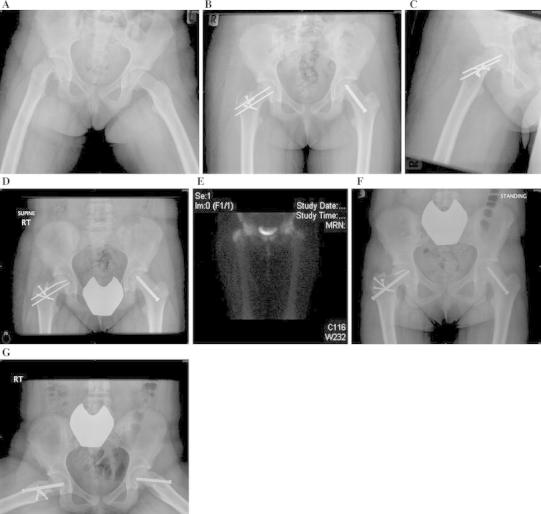
a A 12-year-old girl was diagnosed with right unstable slipped capital femoral epiphysis (SCFE) and left chronic SCFE. b–c The patient underwent right subcapital corrective osteotomy and open reduction through means of surgical dislocation of the hip and left in situ fixation with a 7.3-mm fully threaded screw. d Six weeks after surgery, one of the K-Wires was broken. The patient had no pain. e A bone scan revealed that both femoral heads were perfused and the patient was taken to the operating room for hardware revision, performed percutaneously. The two Kirschner wires were removed and a 7.3-mm screw was put in place. f–g At 13 months of follow-up, there were no signs of avascular necrosis (AVN) and the patient did not have any limitations or hip pain
Furthermore, in the surgical dislocation group, one patient (case 4) underwent an arthrodiastasis of the affected hip and a later contralateral distal femur and proximal tibia epiphysiodesis to compensate for the predicted limb length discrepancy (Fig. 2). Also in the surgical dislocation group, one patient (case 5) underwent a femoral head resection. This patient was taken to the operating room for a redo surgical dislocation and femoral head realignment. Intra-operatively, it was observed that the femoral head was already misshaped and not bleeding. The surgeon decided to interrupt the surgery and to discuss the remaining options with the family. Given the fact that the patient had pain, femoral head resection and hip arthroplasty were offered. The parents preferred to go ahead with the femoral head resection and leave arthroplasty as an option for the future.
Fig. 2.
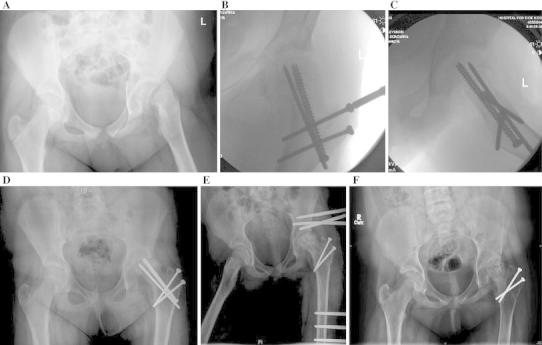
a An 11-year-old girl was diagnosed with a left unstable SCFE, after falling on ice. b–c The patient underwent subcapital corrective osteotomy and open reduction through means of surgical dislocation of the hip. d Left hip AVN was noticed at 6 months follow-up. e The hardware was removed and a hinged hip distractor external fixator was applied for 7 months. f At 2 years follow-up, the patient has hip pain and restricted motion. A contralateral distal femoral epiphysiodesis was performed to partially address the limb length discrepancy
Discussion
The cause of AVN following an SCFE is unknown. Furthermore, the rate of AVN in SCFEs is difficult to establish, as most papers report on a mixture of stable and unstable SCFEs, which are conditions with different prognoses.
AVN may result from the traumatic precipitating event [17]. We observed that one of the patients who underwent surgical dislocation in our series had no soft-tissue connection between the femoral head and neck. Alternatively, AVN may be due to a tamponade effect from increased intracapsular pressure [18] or the stretch of retinacular vessels when attempting to reduce the epiphysis over the posterior femoral neck callus [9, 12].
Treatment of unstable SCFE with subcapital correction osteotomy by means of surgical hip dislocation theoretically avoids AVN by preserving the blood perfusion to the femoral epiphysis. The other potential advantage is the prevention of femoroacetabular impingement (FAI) by achieving an anatomical reduction of the epiphysis [9, 10, 12]. Adolfsen and Sucato [9] reported a series of 15 patients with unstable SCFEs, treated with open reduction and fixation of the slipped capital epiphysis by means of surgical hip dislocation, where 1 of 15 patients (6.7 %) had AVN. They hypothesized that the blood flow to the epiphysis would remain intact at the time of the injury and open reduction by means of surgical hip dislocation would provide an opportunity to maintain perfusion. Rebello et al. [10] treated by open reduction five acute SCFEs, not having experienced any case of AVN. Leunig et al. [11] reported no case of AVN, after having treated 30 patients diagnosed with acute SCFE (sudden onset of symptoms and less than 3 weeks of duration) with this technique.
Our study showed a 67 % rate of AVN with open reduction by means of surgical dislocation of the hip. Several factors may explain the difference in results in these series. First, it is possible that there is a difference in the patient populations. Both Rebello et al. [10] and Leunig et al. [11, 12] reported their experience with “acute SCFE”, but it is uncertain as to how many of these cases were “unstable”, as defined by Loder et al. [2]. In our study, patients were unable to arise from the recumbent position, any hip movement was severely painful, and there was free motion between the femoral head and neck, observed either under fluoroscopy or at the time of open reduction. If patients in the other series were unable to bear weight on the affected side but still able to ambulate with crutches, this would presumably affect the rate of AVN with any treatment. Second, in prior studies, there was no control group and this may have lead to different criteria of evaluation (in this study, we have a controlled comparison of standard treatment and surgical dislocation, in the same patient population). Third, patients in our series presented late (more than 8 h after the injury) and this may have increased the rate of AVN—if earlier treatment would have been performed, this might have decreased the rate of AVN in the surgical dislocation group. Fourth, patients who underwent open reduction were operated in the beginning of our learning curve, as all four surgeons had no previous experience with the procedure, except for cadaver lab training. This factor may have contributed to the increase in our number of complications. However, all surgeons are pediatric orthopedic surgeons with extensive experience in pediatric and adolescent hip surgery.
Our study shows a 33.3 % rate for patients with truly unstable SCFEs undergoing closed reduction and percutaneous pinning, which is higher than that reported in recent investigations [19, 20]. Explanations for this may be the length of time between injury and treatment and the fact that we did not perform any attempt of hip joint decompression through capsulotomy or aspiration.
Our study has several potential limitations. First, given our small sample size, this study can only serve as precautionary, suggesting that surgical dislocation does not eliminate the risk of AVN. It is important to note that we were highly selective in only examining truly “unstable” SCFEs, as defined by Loder et al. [2]. Second, our study was retrospective. However, our patients were assessed in exactly the same way, allowing us to make a comparison between the group who had closed reduction (controls) and the group who had open reduction by means of surgical dislocation of the hip. Third, multiple surgeons were involved in the surgeries of these patients, which may have introduced more technical variability. Nonetheless, we believe that this reflects the reality of most clinical practice settings.
In conclusion, although surgical dislocation of the hip has been reported to be a safe and effective procedure in the treatment of several hip conditions [9–11, 15], our experience cannot confirm that it changes the natural history of the unstable SCFE or has any advantage over closed reduction when considering the rate of AVN. This study reports the experience of a center that introduced a new technical approach to the treatment of unstable SCFE. Although we think that our results may improve with time and experience, we also believe that, given the limited number of truly unstable SCFEs, surgeons should acquire adequate training and remain cautious as they adopt this new methodology.
Conflict of interest
None.
References
- 1.Aronsson DD, Loder RT, Breur GJ, Weinstein SL. Slipped capital femoral epiphysis: current concepts. J Am Acad Orthop Surg. 2006;14(12):666–679. doi: 10.5435/00124635-200611000-00010. [DOI] [PubMed] [Google Scholar]
- 2.Loder RT, Richards BS, Shapiro PS, Reznick LR, Aronson DD. Acute slipped capital femoral epiphysis: the importance of physeal stability. J Bone Joint Surg Am. 1993;75(8):1134–1140. doi: 10.2106/00004623-199308000-00002. [DOI] [PubMed] [Google Scholar]
- 3.Aronsson DD, Loder RT. Treatment of the unstable (acute) slipped capital femoral epiphysis. Clin Orthop Relat Res. 1996;322:99–110. [PubMed] [Google Scholar]
- 4.Ballard J, Cosgrove AP. Anterior physeal separation. A sign indicating a high risk for avascular necrosis after slipped capital femoral epiphysis. J Bone Joint Surg Br. 2002;84(8):1176–1179. doi: 10.1302/0301-620X.84B8.12904. [DOI] [PubMed] [Google Scholar]
- 5.Mooney JF, 3rd, Sanders JO, Browne RH, Anderson DJ, Jofe M, Feldman D, et al. Management of unstable/acute slipped capital femoral epiphysis: results of a survey of the POSNA membership. J Pediatr Orthop. 2005;25(2):162–166. doi: 10.1097/01.bpo.0000151058.47109.fe. [DOI] [PubMed] [Google Scholar]
- 6.Aronson DD, Peterson DA, Miller DV. Slipped capital femoral epiphysis. The case for internal fixation in situ. Clin Orthop Relat Res. 1992;281:115–122. [PubMed] [Google Scholar]
- 7.Peterson MD, Weiner DS, Green NE, Terry CL. Acute slipped capital femoral epiphysis: the value and safety of urgent manipulative reduction. J Pediatr Orthop. 1997;17(5):648–654. doi: 10.1097/01241398-199709000-00013. [DOI] [PubMed] [Google Scholar]
- 8.Parsch K, Weller S, Parsch D. Open reduction and smooth Kirschner wire fixation for unstable slipped capital femoral epiphysis. J Pediatr Orthop. 2009;29(1):1–8. doi: 10.1097/BPO.0b013e31818f0ea3. [DOI] [PubMed] [Google Scholar]
- 9.Adolfsen SE, Sucato DJ. Surgical technique: open reduction and internal fixation for unstable slipped capital femoral epiphysis. Oper Tech Orthop. 2009;19:6–12. doi: 10.1053/j.oto.2009.03.004. [DOI] [Google Scholar]
- 10.Rebello G, Spencer S, Millis MB, Kim YJ. Surgical dislocation in the management of pediatric and adolescent hip deformity. Clin Orthop Relat Res. 2009;467(3):724–731. doi: 10.1007/s11999-008-0591-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Leunig M, Slongo T, Kleinschmidt M, Ganz R. Subcapital correction osteotomy in slipped capital femoral epiphysis by means of surgical hip dislocation. Oper Orthop Traumatol. 2007;19(4):389–410. doi: 10.1007/s00064-007-1213-7. [DOI] [PubMed] [Google Scholar]
- 12.Leunig M, Slongo T, Ganz R. Subcapital realignment in slipped capital femoral epiphysis: surgical hip dislocation and trimming of the stable trochanter to protect the perfusion of the epiphysis. Instr Course Lect. 2008;57:499–507. [PubMed] [Google Scholar]
- 13.Southwick WO. Osteotomy through the lesser trochanter for slipped capital femoral epiphysis. J Bone Joint Surg Am. 1967;49(5):807–835. [PubMed] [Google Scholar]
- 14.Boyer DW, Mickelson MR, Ponseti IV. Slipped capital femoral epiphysis. Long-term follow-up study of one hundred and twenty-one patients. J Bone Joint Surg Am. 1981;63(1):85–95. [PubMed] [Google Scholar]
- 15.Leunig M, Slongo T, Ganz R. Subcapital realignment in slipped capital femoral epiphysis: surgical hip dislocation and trimming of the stable trochanter to protect the perfusion of the epiphysis. Instr Course Lect. 2008;57:499–507. [PubMed] [Google Scholar]
- 16.Ganz R, Gill TJ, Gautier E, Ganz K, Krügel N, Berlemann U. Surgical dislocation of the adult hip a technique with full access to the femoral head and acetabulum without the risk of avascular necrosis. J Bone Joint Surg Br. 2001;83(8):1119–1124. doi: 10.1302/0301-620X.83B8.11964. [DOI] [PubMed] [Google Scholar]
- 17.Kennedy JG, Hresko MT, Kasser JR, Shrock KB, Zurakowski D, Waters PM, et al. Osteonecrosis of the femoral head associated with slipped capital femoral epiphysis. J Pediatr Orthop. 2001;21(2):189–193. [PubMed] [Google Scholar]
- 18.Herrera-Soto JA, Duffy MF, Birnbaum MA, Vander Have KL. Increased intracapsular pressures after unstable slipped capital femoral epiphysis. J Pediatr Orthop. 2008;28(7):723–728. doi: 10.1097/BPO.0b013e318186bda3. [DOI] [PubMed] [Google Scholar]
- 19.Chen RC, Schoenecker PL, Dobbs MB, Luhmann SJ, Szymanski DA, Gordon JE. Urgent reduction, fixation, and arthrotomy for unstable slipped capital femoral epiphysis. J Pediatr Orthop. 2009;29(7):687–694. doi: 10.1097/BPO.0b013e3181b7687a. [DOI] [PubMed] [Google Scholar]
- 20.Sankar WN, McPartland TG, Millis MB, Kim YJ. The unstable slipped capital femoral epiphysis: risk factors for osteonecrosis. J Pediatr Orthop. 2010;30(6):544–548. doi: 10.1097/BPO.0b013e3181e4f372. [DOI] [PubMed] [Google Scholar]


