Abstract
Aim
Patients with neuromuscular diseases such as cerebral palsy (CP) and meningomyelocele (MMC) are prone to develop fixed knee flexion contracture. Distal femoral extension osteotomy allows acute correction of the deformity, but it is an extensive surgical procedure, and the complication rate is rather high. Immobilization can prolong the rehabilitation period, and may even result in deteriorated walking ability. The aim of this retrospective study was to evaluate the results of using anterior hemiepiphysiodesis of the distal femur to treat fixed flexion contracture of the knee.
Materials and methods
We studied 21 patients in our department from 2003 to 2009. Mean age was 10 years (5–15). Twelve suffered from MMC, five from CP, two from arthrogryposis, one had an enzyme defect, and one had Down’s syndrome. Thirteen patients had a bilateral and eight a unilateral procedure. None of the patients underwent any other procedures. Two staples or 8-plates were inserted using two parapatellar incisions. Nine were operated on with staples and 12 with 8-plates. The plates or staples were removed when the desired effect of full knee extension was achieved or the patient reached skeletal maturity.
Results
Mean fixed flexion contracture was 20° (10°–40°). Staples or 8-plates were removed after a mean of 24 (6–42) months. Mean fixed flexion contracture at removal was 10° (0°–30°). Two complications were seen: one infection and one supracondylar fracture.
Conclusion
Anterior distal femoral hemiepiphysiodesis using 8-plates or staples seems to be effective for correcting fixed knee flexion deformity in skeletally immature individuals. The complication rate is low (10 %). Our results are comparable to those of Kramer, Klatt, and Stevens. This procedure should be the primary treatment for fixed knee flexion contractures in neuromuscular patients with sufficient remaining growth.
Keywords: Anterior femur, Neuromuscular, Fixed knee contracture
Introduction
Fixed flexion contracture of the knee in patients suffering from neuromuscular disease is a common problem that can be caused by contracture of the hamstrings, weak knee extensors, and (later) contracture of the posterior part of the capsule. Untreated, it can lead to painful crouch gait and loss of gait function [1–5]. These contractures are commonly treated by physiotherapy, bracing, casting, or tenotomy of the hamstring tendons. Results can be disappointing, especially in older children, due to contracture of the posterior capsule of the knee joint [1, 2, 4, 5]. In 2001, Kramer and Stevens published the first work on the treatment of fixed flexion knee contractures using anterior distal femoral epiphysiodesis [3]. This article describes our experience using this technique and compares the results obtained when performing it using 8-plates or staples.
Materials and methods
We reviewed the medical records of 21 patients (14 males and 7 females), all of whom were treated at the Odense University Hospital from 2003 to 2009. Mean age was 10 years (5–15). Twelve patients were diagnosed with meningomyelocele (MMC), five patients with cerebral palsy (CP), two patients had arthrogryposis, one had an enzyme defect, and one had Down’s syndrome. In the CP group, we had one patient with spastic hemiplagia of the left side and four patients with spastic diplegia (GMFCS I–III). Nine patients were ambulatory and 12 were nonambulatory. We used the goniometer to measure the degree of fixed knee flexion deformity. The flexion contracture angle was defined as the angle between the neutral position corresponding to 0° and the maximum extension of the knee. This was measured with the patient lying supine with the hip extended. The indication for surgical treatment was a fixed flexion contracture of greater than 10° in both ambulatory and nonambulatory patients. Nonambulatory patients were treated so as to avoid progressive contractures, which can lead to seating and hygienic difficulties. Anteroposterior radiographs of the knee joint were taken to document an open femoral physis. Thirteen patients (62 %) had a bilateral and eight patients (38 %) had a unilateral procedure; this makes a total of 34 knees. Nine patients (43 %) were operated with staples and 12 patients (57 %) with 8-plates. Patients who would not benefit from the procedure can be operated on with supracondylar osteotomy. As the contractures were of the fixed type, a procedure such as medial hamstring lengthening was not done, as this would have only addressed the dynamic part. The plates or staples were removed when the desired effect—improving knee extension—was achieved, or when the patient reached skeletal maturity.
Techniques
All cases were operated on as outpatient procedures. The operation was performed under general anesthesia with the patient supine using tourniquet hemostasis. With the aid of fluoroscopic imaging, the physis was localized. A longitudinal (3 cm) incision on both sides of the patella was made, centered on the physis. The retinaculum and synovium of the knee joint was incised to expose the distal femur, but care was taken not to disturb the periosteum. Under fluoroscopic guidance, a 1.6 mm K-wire was inserted into the physis as a marker. A Richards staple was impacted, centered over the distal femur physis and just lateral and medial to the sulcus (trochlear groove). The position was discerned by fluoroscopy and the impaction was completed. 8-plates were then placed using the center hole of each plate, slipping them over the K-wire. Two 1.6 mm K-wires were inserted into the screw holes in each plate. The position was checked using fluoroscopy, the cortex was drilled, and two self-tapping cannulated screws were inserted.
Mobilization with full weight-bearing was allowed as tolerated immediately. The patients were followed up at 3–6 month intervals. Clinical and/or radiological evaluation of the effect of the procedure took place during the follow-up. The staples or 8-plates were left in place until skeletal maturity or until the deformity was corrected. As all of these patients suffered from chronic diseases, follow-up continued after hardware removal.
Results
The mean fixed flexion contracture was 20° (range 10°–40°). Staples or 8-plates were removed after a mean of 24 (6–42) months. Mean follow-up time was 24 (6–42) months. Mean correction of fixed flexion contracture was 10°. The resulting residual contracture was 10° (0°–30°). This can be explained by the fact that some of the patients had negligible remaining growth at the time of hemiepiphysiodesis. Two patients who were treated with 8-plates complained of knee pain. After 3 months, the pain had disappeared in both patients, and the hardware was left in place.
One minor and one major complication were seen; one patient had a superficial infection that responded to antibiotic treatment, and one had a supracondylar femur fracture. The fracture occurred 2 months postoperatively through the proximal screws and was considered a stress-related fracture. The fracture was treated with closed reduction and percutaneous internal fixation with two Steinmann pins, and a back slap was applied for six weeks. The fracture healed uneventfully and the 8-plates were left in situ. This previously unknown complication after treatment with the 8-plate was published as a case report [6].
Nine cases were treated with Richard staples: five bilateral, three on the left side, and one on the right side. Twelve patients were treated with 8-plates; eight bilateral, two on the left side, and two on the right side. This makes 14 knees treated with staples and 20 knees treated with 8-plates (Table 1; Figs. 1, 2). These two groups were comparable in terms of numbers and the diagnoses. The mean age was 11 years (range 5.5–15) for the staples group and 9.6 years (range 7.5–15) for the 8-plates group (P = 0.31). We found no significant difference regarding the primary deformity (with a mean of approximately 20°) or the correction (P = 0.52 and 0.68, respectively). The time for correction was significantly lower in the 8-plates group (20 months) compared to the staples group (30 months) (P = 0.03). This could be also seen by looking at the mean correction rate per month, which was 0.3° for the staples group and 0.5° in the 8-plate group.
Table 1.
Patient demographics
| Pt. no. | Age at operation | Gender | Hardware | Side | Contracture before | Contracture after | Correction time (months) | Complications | Diagnosis |
|---|---|---|---|---|---|---|---|---|---|
| 1 | 11 | M | Staples | B | 15 R, 10 L | 0 B | 24 | NON | MMC |
| 2 | 12.5 | F | Staples | L | 20 L | 10 L | 39 | NON | MMC |
| 3 | 8.5 | M | 8-plates | L | 30 L | 15 L | 12 | NON | CP |
| 4 | 13 | M | 8-plates | B | 15 R, 25 L | 5 R,10 L | 25 | NON | Downs |
| 5 | 7 | M | 8-plates | B | 20 R, 15 L | 0 R,10 L | 20 | NON | MMC |
| 6 | 7.5 | M | 8-plates | L | 20 L | 0 L | 20 | NON | MMC |
| 7 | 8 | F | Staples | L | 20 L | 0 L | 24 | NON | MMC |
| 8 | 13 | M | Staples | R | 20 R | 10 R | 29 | NON | ARG |
| 9 | 10 | M | Staples | B | 35 R, 20 L | 10 R,0 L | 29 | NON | MMC |
| 10 | 7.5 | F | 8-plates | L | 30 L | 30 L | 42 | Infection | MMC |
| 11 | 5.5 | F | Staples | B | 25 B | 10 B | 36 | NON | MMC |
| 12 | 9 | M | 8-plates | B | 15 B | 10 B | 10 | NON | MMC |
| 13 | 15 | M | 8-plates | B | 40 B | 15 B | 12 | NON | ED |
| 14 | 10.5 | M | 8-plates | B | 30 B | 0 B | 12 | NON | MMC |
| 15 | 8 | F | 8-plates | B | 15 B | 0 B | 14 | Knee pain | CP |
| 16 | 13.5 | M | 8-plates | B | 20 B | 0 B | 12 L, 27 R | NON | CP |
| 17 | 5 | F | 8-plates | R | 20 R | 5 R | 36 | NON | ARG |
| 18 | 11 | F | 8-plates | B | 20 B | 0 B | 18 | Knee pain | CP |
| 19 | 15 | M | Staples | B | 10 L,20 R | 5 L,10 R | 36 | NON | MMC |
| 20 | 13.5 | M | Staples | B | 20 B | 20 B | 12 | NON | CP |
| 21 | 13 | M | Staples | L | 25 L | 10 L | 42 | SC fracturea | MMC |
R right, L left, B bilateral, MMC meningomyelocele, ARG arthrogryposis, CP cerebral palsy, ED enzyme defect
aSupracondylar femur fracture
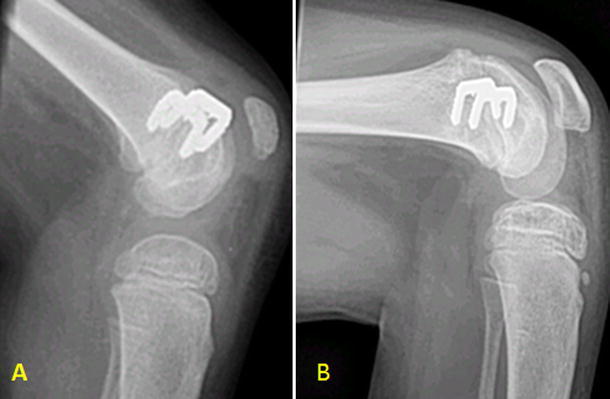
Fig. 1.

a A patient with CP and fixed knee flexion contracture treated with anterior distal femoral epiphysiodesis using 8-plates;b the same patient after 20 months of treatment
Fig. 2.
Patient with arthrogryposis and fixed knee flexion contracture treated with Richards staples: just postoperative (a) and 14 months postsurgery (b)
Discussion
The development of fixed flexion knee contracture (FFKC) is a very common occurrence in MMC, arthrogryposis, and CP patients [1–5, 7, 8]. Although physiotherapy and bracing is used to avoid this, contracture development appears to be inevitable, and it considered to be part of the natural history of these diseases [1, 3–5, 7]. A few degrees of flexion contracture can be tolerated, but when it exceeds 10° it has a negative effect on gait function and can give rise to the development of painful crouch gait [7]. Medial hamstring tenotomies are well practiced, but do not give the full extension expected, as they only address the dynamic part of the deformity, not the fixed part [1, 2, 8, 9]. Posterior release—in the form of posterior capsulotomy combined with recession of the gastrocnemius and posterior cruciate ligament—gives more extension, but it is an extensive and demanding surgical procedure that carries a risk of destabilizing the knee as well as neurovascular injuries [1, 8]. Furthermore, it can lead to weakness of the quadriceps, as the extensor mechanism is unintentionally and indirectly lengthened [4].
Extension supracondylar osteotomy, usually combined with shortening of the extensor mechanism, is another possible solution to this problem. This is a major operation that corrects the contracture but creates a deformity in the form of recurvatum of the distal femur [8, 10, 11]. Besides, complications in the form of neurovascular compromise, fracture, loss of correction, and varus/valgus deformities have been reported for it [10].
The use of Ilizarov as a distractor to treat FFKC is well described [8]. In one study, the authors stated that treating patients with arthrogryposis and knee flexion contractures of >40° cannot be done without the use of Ilizarov distraction and posterior release [12]. Treatment with an Ilizarov fixator is not, however, a procedure that is well suited to these patients, as the apparatus is cumbersome, the procedure is lengthy, and the complication rate is high [12].
The introduction of anterior distal femoral epiphysiodesis has changed the treatment of this deformity [1]. This is a minor operation that can be performed as an outpatient procedure and does not require any immobilization [1].
Previous studies have described this treatment using either staples or 8-plates [1–3, 7]. In our series, we started using staples and shifted to 8-plates later in the series. This gave us the opportunity to compare the two principles. We found that a significantly faster correction was achieved using 8-plates than staples. Upon comparing two different studies, one using staples [7] and the other using 8-plates [2], the correction rate appears to favor the use of 8-plates. This might be explained by the fact that the 8-plate system is flexible and that divergence occurs without a great deal of resistance. Stevens and coauthors explained that the 8-plate acts as a tension band that evidently restricts the growth to a greater degree. The divergence of the screws is evidence that this tension band effect occurs primarily at the surface of the epiphyseal plate. Besides, the axis correction angle (ACA) for an 8-plate lies at the cortex, under the 8-plate; for staples, it lies between the ends of the two arms (Fig. 3). In this way, the correction arm is longer for the 8-plate, which could contribute to the faster correction.
Fig. 3.
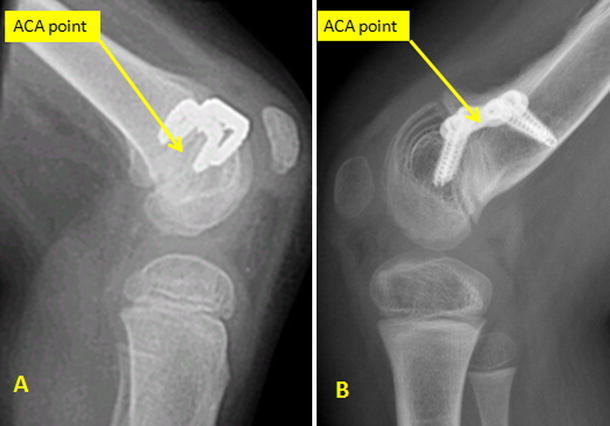
The ACA points for staples and 8-plates
We did not achieve complete correction in all our cases. Some rather old children were probably treated too late—they were near to reaching skeletal maturity at the time of surgery, and the remaining growth did not allow sufficient correction. In one patient (no. 10), we did not get any correction. This is very interesting, but could be due to progressive contracture during the correction time. As the patients had different etiologies, we divided them into smaller groups, although this shows that this technique can be used for etiologies other than CP. Another drawback of our series is that some of the patients had the hardware removed before full correction had occurred. We did not perform a long-term follow-up in our study, as our aim was to demonstrate the effect of anterior distal femur epiphysiodesis on FFKC in neuromuscular patients. Obviously, the young group studied here would have had a higher risk of recurrence than patients who have reached skeletal maturity.
Conclusion
FFKC of the knee is an insidious and sometimes incapacitating problem seen in children and adolescents with a variety of neuromuscular conditions. Although prompt recognition and early intervention via physical therapy and bracing is helpful, the natural history of this deformity is typically one of progression. Growth manipulation by means of anterior distal femoral stapling is reasonable, safe, and effective. The use of 8-plates seems to lead to faster correction than staples, but further studies of this aspect are needed. More extensive surgical procedures such as supracondylar extension osteotomy of the distal femur may then be reserved for adolescents with insufficient growth potential.
Footnotes
Conflict of interest
None of the authors received financial support for this study.
References
- 1.Kramer A, Stevens PM. Anterior femoral stapling. J Pediatr Orthop. 2001;21(6):804–807. [PubMed] [Google Scholar]
- 2.Klatt J, Stevens PM. Guided growth for fixed knee flexion deformity. J Pediatr Orthop. 2008;28(6):626–631. doi: 10.1097/BPO.0b013e318183d573. [DOI] [PubMed] [Google Scholar]
- 3.Palocaren T, Thabet AM, Rogers K, Holmes L, Jr, Donohoe M, King MM, Kumar SJ. Anterior distal femoral stapling for correcting knee flexion contracture in children with arthrogryposis—preliminary results. J Pediatr Orthop. 2010;30(2):169–173. doi: 10.1097/BPO.0b013e3181d07593. [DOI] [PubMed] [Google Scholar]
- 4.Beals RK. Treatment of knee contracture in cerebral palsy by hamstring lengthening, posterior capsulotomy, and quadriceps mechanism shortening. Dev Med Child Neurol. 2001;43(12):802–805. doi: 10.1017/S0012162201001451. [DOI] [PubMed] [Google Scholar]
- 5.Wright JG, Menelaus MB, Broughton NS, et al. Natural history of knee contractures in myelomeningocele. J Pediatr Orthop. 1991;11:725–730. doi: 10.1097/01241398-199111000-00005. [DOI] [PubMed] [Google Scholar]
- 6.Al-Aubaidi Z, Engell V, Lundgaard B. Stress fracture following femoral epiphysiodesis. Ugeskr Laeger. 2010;172(41):2847–2848. [PubMed] [Google Scholar]
- 7.Spiro AS, Babin K, Lipovac S, Rupprecht M, Meenen NM, Rueger JM, Stuecker R. Anterior femoral epiphysiodesis for the treatment of fixed knee flexion deformity in spina bifida patients. J Pediatr Orthop. 2010;30(8):858–862. doi: 10.1097/BPO.0b013e3181f10297. [DOI] [PubMed] [Google Scholar]
- 8.Herzenberg JE, Davis JR, Paley D, et al. Mechanical distraction for treatment of severe knee flexion contractures. Clin Orthop Relat Res. 1994;301:80–88. [PubMed] [Google Scholar]
- 9.Dias LS. Surgical management of knee contractures in myelomeningocele. J Pediatr Orthop. 1982;2:127–131. doi: 10.1097/01241398-198202020-00002. [DOI] [PubMed] [Google Scholar]
- 10.Asirvatham R, Mukherjee A, Agarwal S, Rooney RJ, Ellis RD, Watts HG. Supracondylar femoral extension osteotomy: its complications. J Pediatr Orthop. 1993;13(5):642–645. doi: 10.1097/01241398-199313050-00016. [DOI] [PubMed] [Google Scholar]
- 11.Zimmerman MH, Smith CF, Oppenheim WL. Supracondylar femoral extension osteotomies in the treatment of fixed flexion deformity of the knee. Clin Orthop Relat Res. 1982;171:87–93. [PubMed] [Google Scholar]
- 12.van Bosse HJ, Feldman DS, Anavian J, et al. Treatment of knee flexion contractures in patients with arthrogryposis. J Pediatr Orthop. 2007;27:930–937. doi: 10.1097/bpo.0b013e3181594cd0. [DOI] [PubMed] [Google Scholar]


