Abstract
Background
Measuring social adjustment (including attachment style and current social adaptation) in late-life depression may support planning secondary prevention, rehabilitation and treatment. Insecure attachment style is a risk factor for developing new depression, and social adjustment may constitute a problem after symptoms abatement. Few studies have examined attachment style and social adjustment in late-onset depression.
Design
Subjects 50 years of age and older with early-onset (n=35), late-onset DSM-IV unipolar depression (n=38) and never depressed volunteers (n=47) were assessed with a widely-used measure of attachment style (the Experiences in Close Relationship Scale). Social adjustment was measured using the Social Adjustment Scale.
Results
Both early- and late-onset patients with depression showed greater insecure attachment and poorer social adaptation compared to never depressed volunteers. No difference was found between early- and late-onset patients with depression on attachment style or social adjustment. There were no significant differences between late-life depression in remission or current on attachment or social adaptation.
Conclusion
Insecure attachment style may be a risk factor for late-life depression irrespective of the age of onset. Social maladaptation may persist among individuals with late-life depression in remission.
Keywords: Late-life depression, social adjustment, attachment, romantic attachment, remission
Depression may occur for the first time in later life but older persons may also have suffered their first episode of depression in their youth. Depending on the age of onset differing etiopathology has been posited (Baldwin and Tomenson, 1995, Blazer, 2003, Heun et al., 2000). Late-onset depression is widely believed to have a strong vascular component whereas psychological, social and genetic factors have greater influence on the onset of early-onset depression (Blazer and Hybels, 2005, Herrmann et al., 2008). Continuing research efforts to distinguish the mechanisms of early from late-onset late life depression may be relevant to establish treatment and predict outcome.
The findings that insecure attachment styles (i.e., anxious and avoidant dimensions) are predictors of adult psychopathology have increased interest in attachment theory in depression (Bifulco et al., 2006, Haggerty et al., 2009, Roberts et al., 1996). Early parent-child social interactions mold working models of future relationships between self and others (i.e., attachment styles) (Atkinson, 1997, Grossmann et al., 2005). Memories of these childhood interactions influence the social interaction with life-time significant figures including romantic partners (Atkinson, 1997). Comprehensive assessment of social proclivity would not be complete without measuring vocational and family functioning and during leisure activities. These are indicators of current social engagement, while attachment style is an indicator of lifetime social inclinations that are rooted in past developmental history.
Perhaps because the findings on vascular etiology are relatively consistent, attachment style in late-onset depression has been understudied. Same can be said for social adjustment. To expand, it is currently not known the extent to which developmentally based individual differences in attachment styles are potential vulnerability factors in depression with onset in later in life as they are for depression of young adulthood onset (Marazziti et al., 2007). While on the one hand the relative stability of attachments styles would suggest an association with depression at any age, delayed onset, cerebrovascular findings and risk to develop cognitive impairment have supported the view that late-onset depression may have a differing set of etiological factors relative to depression with onset in younger age (Baldwin and Tomenson, 1995, Blazer, 2003, Heun et al., 2000). For these reasons, it would also be important to verify if late-onset depression carries additional social adjustment burden in comparison to early-onset depression (Brodaty et al., 1993).
In the present research, individuals with early- and late-onset depression, and never-depressed age comparable volunteers were assessed using measures of attachment style and social adjustment. The Experiences in Close Relationship Scale was used to assess lifetime social attitudes with figures of attachment, and the Social Adjustment Scale was used to assess current social functioning in multiple domains including family, work and leisure. Based on the extant literature (Alexopoulos et al., 1997, Bifulco et al., 2006) predictions were made that early-onset depression would show greater insecure attachment than late-onset depression and never-depressed volunteers. Both early- and late-onset depression were predicted to carry greater risk for social impairment based one on the longer duration of the illness and the other on its purported association with vascular brain damage. To ascertain the influence of mood on reports of social adaptation and attachment (Fincham and Bradbury, 1993), patients were examined during an episode of depression and while others were examined during a phase of remission. It was expected that individuals with current depression would show greater impairment in social adjustment compared to individuals with depression in remission and never-depressed volunteers (Marazziti et al., 2007).
Methods
Subjects
The present report focuses on subjects who were 50 and older at the time of enrollment in the University of Iowa research program on social and emotional perception over the life span and unipolar depression. A group of patients (N=35, mean age=58.5 SD=7.3) with onset of depression before age 50 (early-onset), and a group of patients with onset of depression after age 50 (late-onset) (N=38, mean age=61.8 SD=8.5) were compared to a group of nondepressed volunteers (N=47, mean age 70.2, SD=9.4). Late onset was defined as onset of the first episode of depression occurring after age 50 based on established literature (Krishnan et al., 1995). Age at onset of the first episode of depression was determined based on patients’ report and corroborated, when available, by medical records. Participants were recruited from the University of Iowa Departments of Psychiatry (inpatient and outpatient services) and Internal Medicine (outpatient services), the VA medical center in Iowa City, IA, and community advertisements.
Study participants were from a larger database aimed at examining several constructs of emotional and social functioning and social cognition in depression as a function of age and age of onset. Subjects in the database were enrolled as a result of the following procedures. Five hundred and twenty seven candidate subjects were screened between November 2005 and April 2009. A first (including telephone) screening was carried out to exclude individuals with a history of co-morbid psychiatric, neurological disorders, or general medical conditions impairing cognition, vision or hearing. Two-hundred and twenty seven eligible participants (age range 19–90, mean age=52.37, SD=18.43, 61.2% women) provided informed consent according to the regulations of the Institutional Review Board (IRB) of the University of Iowa. These subjects completed a second office screening which included an assessment using the Structured Clinical Interview for DSM-IV-TR (SCID) (First et al., 2002) used to confirm the diagnosis of unipolar major depression. Exclusionary criteria ascertained at his stage during the office interview were: a) history or presence of compulsive obsessive disorder, psychosis other than accompanying depression, bipolar affective disorder, primary anxiety disorder, eating disorder or somatoform and related disorders or substance misuse disorders within the past 5 years; b) history of brain injury or other neurological disease; c) clinical evidence of preexisting dementia as defined by DSM-IV criteria; d) Mini-Mental State Examination [MMSE; (Folstein et al., 1975)] score of 25 and below. Of these 227 eligible participants only subjects aged 50 and older were examined in the present study (n=120). Among patients with history of or current depression (n=73), 63 (85.5%) were examined as outpatients.
Measures
The Experiences in Close Relationship Scale (ECRS), a well-validated 36-item self-report questionnaire was administered to measure adult attachment (Simpson and Rholes, 1998). The ECRS assesses two dimensions of lifetime attitudes within primary romantic relationships (i.e., avoidance and anxiety of abandonment). Items are scored on a seven point scale ranging from strongly disagree to strongly agree. Sample items include “I prefer not to be too close to my romantic partner” and “I worry a fair amount about losing my partner.”
Social adjustment over the previous two weeks was assessed using the Social Adjustment Scale – Self Report (SAS-SR), a widely-used self-report scale measuring six social domains (work, social and leisure time, extended family, primary relationship, parental and family unit) based on overt behavior, inner feelings and satisfaction (Weissman, 1999). The SAS-SR consists of 42 items and is rated on a 5-point scale with higher scores indicating greater impairment. Sample items from the work and social and leisure time domains include “Have you had any arguments with people at work in the last 2 weeks?” and “How many times in the last two weeks have you gone out socially with other people?” The work domain contained sub-categories that corresponded to applicable stage of life (work outside the home, housework, and school work). A single score for the work domain that corresponded to the life stage of the subject was used. If a subject answered to multiple work categories, the category chosen for the work score was based upon the subject’s own definition of their work environment and role (a worker for pay, a house wife, a student, retired, unemployed). Because of the age range in the study, the sample included many retired subjects. Rather than exclude them from the work domain altogether, responses concerning the housework domain were used based on the notion that these activities are worthy of gratification equal to those who consider housework a primary role. Subjects who defined themselves as unemployed were excluded from analyses of the work domain because scores obtained from unemployed subjects did not reflect social impairment in the work domain. Due to the social nature of the attachment and social adjustment measurements, mild correlations between SAS-SR and avoidant (Spearman’s rho = .36, p<.001) and anxious (Spearman’s rho = .45, p<.001) attachment styles were expected. Depression severity was measured using the 24-item Hamilton Depression Rating Scale (Hamilton, 1960). The 14-item Hamilton Anxiety Rating Scale (Ham-A) was used to assess general anxiety level (Hamilton, 1960). General intelligence was measured using the Wechsler Abbreviated Scale of Intelligence (WASI) (Wechsler, 1999).
Statistical Analysis
Relationship between depression status on attachment style and social functioning were computed using means, standard deviations and ANOVA with illness status (depression versus remission versus never-depressed) as fixed factor. Early and late onset depression subjects and healthy volunteers were compared using means, standard deviations, ANOVA and ANCOVA. Follow up tests were computed only when the omnibus test was statistically significant. Pearson’s Chi-Square was used to analyze nominal data, and Spearman’s rho to examine strength of associations for continuous variables. All analyses were completed using SPSS 17 software (SPSS Inc.).
Results
Demographic and clinical data
Demographic and clinical variables describing early-onset depression, late-onset depression and non-depressed volunteers are provided in Table 1 and Table 2. There were significant group effects of age, sex, employment status (Table 1). Early-onset depression, late-onset depression and non-depressed volunteers did not differ significantly on FSIQ, education, marital and parental status, or ethnicity (Table 1). The proportion of individuals in remission was not significantly different between early-onset depression and late-onset depression (Table 1). As expected, early-onset depression patients suffered significantly more depressive episodes and had earlier onset of depression compared to late-onset depression patients (Table 2). Individuals in remission (n=43) had been free of significant depressive symptoms for a mean of 44.7 months (SD= 48.7).
Table 1.
Demographic and clinical variables
| Early Onset (n=35) | Late Onset (n=38) | Volunteers (n=47) | |
|---|---|---|---|
| Age** | 58.5 (7.3) | 61.8 (8.5) | 70.2 (9.4) |
| Gender: Female (%)** | 30 (85.7) | 14 (36.8) | 28 (59.6) |
| Education: ≥12 yrs (%) | 25 (71.4) | 27 (71.1) | 31 (66.0) |
| Relationship Status: In Rel. (%) | 29 (82.9) | 35 (92.1) | 43 (91.5) |
| Employment Status: employed (%)* | 16 (45.7) | 18 (47.4) | 10 (21.3) |
| Parental Status* | |||
| with no children (%) | 9 (25.7) | 5 (13.2) | 5 (10.6) |
| with 1 child (%) | 2 (5.7) | 6 (15.8) | 7 (14.9) |
| with 2+ children (%) | 24 (68.6) | 27 (71.1) | 35 (74.5) |
| FS IQ | 110.9 (14.1) | 111.5 (11.5) | 116.2 (12.4) |
| HAM-D ** | 9.2 (10.2) | 12.0 (8.5) | 1.8 (2.1) |
| HAM-A** | 6.1 (0.9) | 7.8 (0.8) | 3.3 (0.7) |
| Age of Onset ** | 29.2 (9.8) | 56.2 (8.0) | NA |
| Illness Status | |||
| Depression (%) | 12 (34.3) | 18 (47.4) | NA |
| Remission (%) | 23 (65.7) | 20 (52.6) | NA |
Legend:
indicates statistical significance at p<0.05
indicates statistical significance at p<0.001
Degrees of freedom are expressed below:
Age: F(2, 117)=20.92, p<0.001 Post Hoc: EOD > C (p<0.001), LOD > C (p<0.001)
Gender: χ2(2, N=120) = 18.14, p<0.001
Education: χ2(2, N=120) = 0.37, p=0.83
Relationship Status: χ2(2, N=120) = 2.05, p=0.36
Employment Status: χ2(2, N=120) = 7.90, p=0.02
Parental status: χ2(4, N=120) = 5.07, p=0.28
FS IQ: F(2, 117)=2.24, p=0.11
HAM-D: F(2, 117)=21.85, p<0.001 Post Hoc: EOD > C (p<0.001), LOD > C (p<0.001)
HAM-A: F(2, 117)=8.31, p<0.001 Post Hoc: LOD > C (p<0.001, mean difference=4.47, 95% CI of the mean =2.07 to6.87)
Age of onset: F(1, 70)=164, p<0.001,
Illness Status χ2(1, N=73) = 1.29, p=0.26
Table 2.
Duration of illness and life time episodes
| Early Onset | Late Onset | |
|---|---|---|
| Years Since Onset | ||
| (% <2 Yrs) | 0 | 18.4 |
| (% 2–5 Yrs) | 0 | 44.7 |
| (% 6–15 Yrs) | 8.6 | 28.9 |
| (% 16–30 Yrs) | 48.6 | 7.9 |
| (% >30 Yrs) | 42.9 | 0 |
| Number of Lifetime Episodes | ||
| (% 1 Episode) | 2.9 | 64.9 |
| (% 2 Episodes) | 8.6 | 5.4 |
| (% 3 Episodes) | 11.4 | 16.2 |
| (% 4–10 Episodes) | 11.4 | 0 |
| (% >10 Episodes) | 65.7 | 13.5 |
Legend: Years Since Onset: χ2(4) =53.30, p<0.001; Number of Lifetime Episodes: χ2(4) = 37.30, p<0.001
Attachment and social functioning in current depression and in remission
As expected, subjects with current depression showed greater severity of depression (Ham-D mean score = 20.4, SD= 6.2) compared to subjects in remission (Ham-D mean score = 4.3, SD= 5.0) [t(85)=13.3, p<.001]. Subjects with current depression and in remission showed greater avoidant attachment style [F (2, 64) = 5.1, p=0.008]. But whereas patients with current depression (n=30, mean = 66.7, SD= 21.4) or in remission (n=43, mean = 54.0, SD= 19.1) showed higher or near higher avoidant scores than never-depressed volunteers (n=47, mean = 42.5, SD=15.9) [LSD=21.3, p=.003 and LSD=10.6, p=0.055 respectively], the difference between patients with current depression and in remission was not statistically significant (LSD=10.7, p>.1). The difference on anxious attachment style between current depression (mean = 62.0, SD= 23), and in remission (mean = 70.5, SD= 21) and never-depressed volunteers (mean = 52.3, SD=18.6) failed to reach significance [F (2, 64) = 2.4, p=0.07].
Subjects with both current depression and depression in remission showed poorer social functioning [F (2, 64) = 9.5, p<0.001]. But while patients with current depression (mean SAS = 2.5, SD=.68) or in remission (mean SAS = 1.96, SD=.35) showed greater social impairment than never-depressed volunteers (mean SAS = 1.61, SD=.28) [LSD=.60, p<.001 and LSD=. 34, p=0.005, respectively], patients with current depression did not showed greater impairment than individuals in remission (LSD=. 26, p=0.07). Based on these findings, hypothesis testing comparing early- and late-onset depression was carried out irrespective of illness status.
Adult attachment in early and late-onset depression
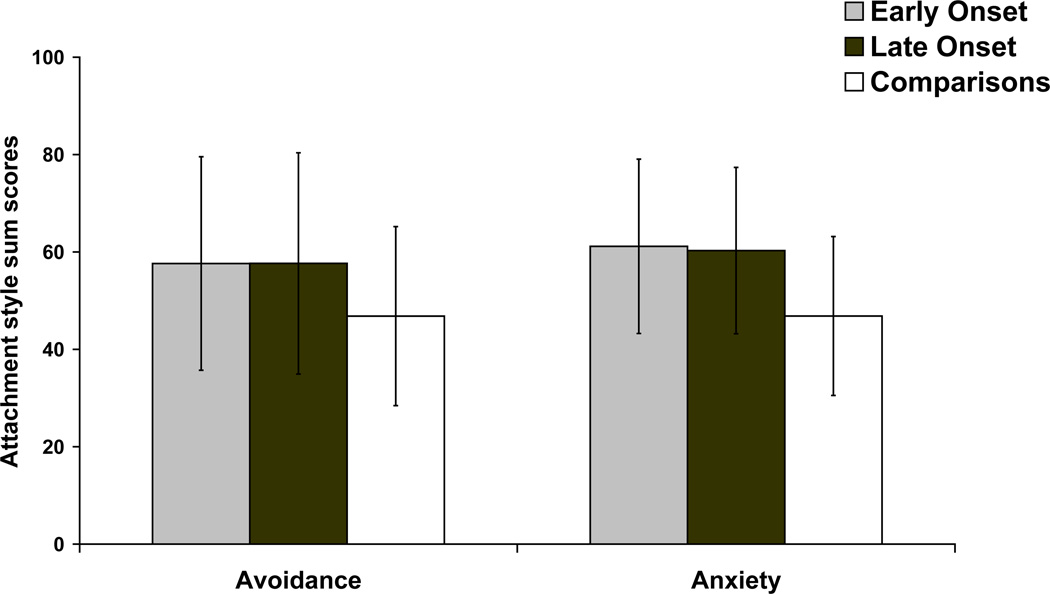
Subjects with early- and late-onset depression also showed greater avoidant attachment scores [F (2, 117) =3.84, p=0.02]. In pairwise comparisons both early- (LSD=-10.8, p=0.02) and late-onset depression (LSD=-10.8, p=0.02) showed significantly greater avoidant attachment scores than never-depressed volunteers, but the difference between early- and late-onset depression (LSD=-0.03, p=1.0) was not significant (Figure 1). Subjects with early- and late-onset depression showed greater anxious attachment style scores [F (2, 117) =9.5, p<.001] than never-depressed volunteers (LSD=-14.3, p<0.001; LSD=-13.4, p<0.001 respectively), but no significant difference was found between early- and late-onset depression (LSD=0.88, p=0.8) (Figure 1).
Figure 1.
Avoidant and anxious attachment scores in depression and non-depressed volunteers.
Note: Statistic details in the text.
Analyses on avoidant [F (2, 116)=3.71, p=0.027] and anxious attachment style scores [F (2, 116)=6.91, p=0.001] using severity of general anxiety as a covariate showed significant group effects with essentially same follow-up tests. In addition, because early- and late-onset depression and never-depressed volunteer groups differed in sex, employment and age, analyses were repeated using these factors as covariates. Group effects for both avoidance [F (2, 114) = 5.14, p=0.007] and anxiety [F (2, 114)=7.28, p=0.001] continued to remain significant and follow up tests were essentially the same.
Because four attachment categories have been proposed based on combination of dimension scores [i.e., secure (low anxiety & avoidance), preoccupied (high anxiety & low avoidance), dismissing (low anxiety & high avoidance) and fearful attachment style (high anxiety & high avoidance] (Ainsworth, 1985), and some studies have suggested a specific association between the preoccupied style and susceptibility to depression (Marazziti et al., 2007), attachment styles were also examined as categories (Table 3). Never-depressed volunteers showed the greatest likelihood of having a secure attachment and the lowest of having a preoccupied attachment compared to subjects with depression [Χ2(6) = 14.9, p=0.02] (Table 3). Analyses showed no significant difference between early and late onset depression [Χ2(3) = 1.1, p>0.7].
Table 3.
Attachment Categories
| Early Onset (%) (n=35) | Early Onset (%) (n=38) | Volunteers (%) (n=47) | |
|---|---|---|---|
| Secure (n=49) | 25.7 | 31.6 | 57.1 |
| Preoccupied (n=18) | 25.7 | 18.4 | 4.3 |
| Dismissive (n=28) | 22.9 | 28.9 | 19.1 |
| Fearful (n=25) | 25.7 | 21.1 | 17.0 |
Legend: Χ2(6) = 14.90, p=0.02
Analyses computed excluding inpatients continued to show significant group effects for avoidant [F (2, 106) = 3.43, p=0.036] and anxious [F (2,106) = 2.18, p<0.001] attachment styles with essentially no change in the post-hoc results. Analyses were also computed using a different age cut-off for late onset depression (i.e., 65 or older) (Kessing, 2006) and yielded significant group effects [avoidant attachment: F (2, 117) = 3.84, p=0.024] – anxious attachment: F (2, 117) = 9.49, p<0.001]. Lastly, among patients 65 years and older (early-onset n=8, late-onset n=14, non-depressed n=32) analyses on anxious attachment showed a significant group effect [F (2, 51) = 4.04, p=0.02) while avoidant attachment failed to reach significance but means and standard deviations closely resembled the parent sample [F (2, 51) = 1.90, p=0.16].
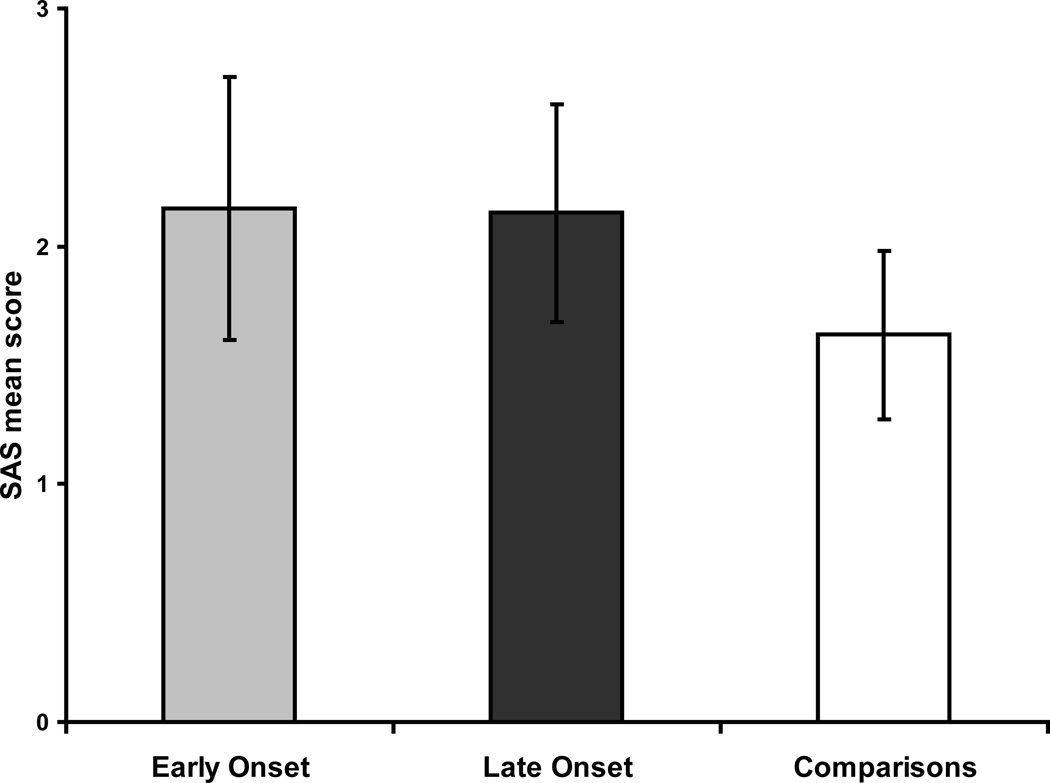
Social adjustment
Significant group effects were found for the SAS-SR total score [F (2, 117)=19.1, p<0.001] (Figure 2), work [F (2, 91)=6.1, p=0.003], social and leisure [F (2,116)=17.0, p<0.001], extended family [F (2, 116)=12.876, p<0.001], and family unit domains [F (2, 117)=8.0, p=0.001] (Table 4). No significant effect were found in marital [F (2, 67)=2.6, p=0.082] and parental domains [F (2, 15)=0.2, p=.8]. Both early- and late-onset depression were significantly more socially impaired than never-depressed volunteers but the difference between early- and late-onset depression never reached statistical significance. Controlling for sex, employment and age left the results unaltered.
Figure 2.
Social adjustment scores in depression and non-depressed volunteers
Note: Statistic details in the text.
Table 4.
Social Adjustment
| EOD (n=35) | LOD (n=38) | Comparisons (n=47) | |
|---|---|---|---|
| Overall (N=120)** | 2.2 (0.6) | 2.1 (0.5) | 1.6 (0.4) |
| Work (N =94)* | 1.9 (0.5) | 1.9 (0.9) | 1.4 (0.4) |
| Social and Leisure (N=119)** | 2.5 (0.7) | 2.5 (0.8) | 1.7 (0.5) |
| Extended Family (N=119)** | 2.0 (0.7) | 1.9 (0.6) | 1.5 (0.3) |
| Marital (N=70) | 2.6 (0.9) | 2.5 (0.6) | 2.2 (0.7) |
| Parental (N=18) | 1.7 (0.6) | 1.9 (0.6) | 1.8 (0.4) |
| Family Unit (N=120)** | 2.1 (1.0) | 2.1 (0.8) | 1.5 (0.6) |
Legend: EOD=Early Onset Depression, LOD=Late Onset Depression, C=Comparisons
indicates statistical significance at p<0.05
indicates statistical significance at p<0.001
Degrees of freedom are expressed below:
Overall: [F (2, 117)=19.13, p<0.001]. Post Hoc: EOD = LOD (p=0.85), EOD > C (p<0.001), LOD > C (p<0.001)
Work: [F (2, 91)=6.12, p=0.003]. Post Hoc: EOD = LOD (p=0.87) EOD > C (p=0.007), LOD > C (p=0.003)
Social and Leisure [F (2, 116)=17.02, p<0.001]. Post Hoc: EOD = LOD (p=0.97), EOD > C (p<0.001), LOD > C (p<0.001).
Extended Family: [F (2, 116)=12.88, p<0.001]. Post Hoc: EOD = LOD (p=0.48), EOD > C (p<0.001), LOD > C (p<0.001)
Marital: [F (2, 67)=2.59, p=0.08]
Parental: [F (2, 15)=0.19, p=0.83)
Family Unit: [F (2, 117)=8.05, p=0.001]. Post Hoc: EOD = LOD (p=0.85), EOD > C (p=0.001), LOD > C (p=0.001)
Analyses computed on outpatients only showed a significant group effect on SAS-SR total score [F (2, 106) = 16.97, p<0.001]. Using 65 and older as age cut-off for late-onset depression (Kessing, 2006) yielded also significant group effect [F (2, 117) = 19.13, p<0.001]. Lastly, comparing only patients 65 years and older yielded a significant group effect on SAS-SR total score [F (2, 51) = 6.04, p=0.004]. Post-hoc analyses were essentially the same as in the parent sample.
Discussion
Measuring social proclivity (including interpersonal attachment attitudes, rooted in social developmental history, and current social adaptation) constitutes a component of the assessment of depression that helps to guide a comprehensive treatment plan, rehabilitation and secondary prevention (Bifulco et al., 2006, Conradi and De Jonge, 2009, Brodaty et al., 1993, Paykel et al., 1978). Assessment of social functioning is critical in clinical scenarios in which a psychiatric disorder (e.g., depression) interacts with a condition (e.g., older age) vulnerable to social disability. The present study examined attachment styles and social functioning among older patients with late-life unipolar depression as a function of age at the time of their first depressive episode and illness status (current depression or remission). Prior studies have shown a relationship between depression and insecure attachment style (Bifulco et al., 2006, Conradi and De Jonge, 2009) and social maladaptation (Brodaty et al., 1993, Paykel et al., 1978), but to our knowledge this is the first study to examine these constructs in late-onset depression. Depression in late-life was associated with greater insecure attachment style and poorer social functioning irrespective of the age of onset. A different cut-off score for late-onset depression (65 and older) (Kessing, 2006), examination only of subjects 65 and older and only outpatients essentially did not change these results. Illness status (i.e., remission or current depression) did not show a significant effect on social functioning or attachment style.
Before examining the significance of these findings some caveats need to be discussed. Due to selection criteria subjects with cognitive impairment were excluded from the study. Consequently, the present findings cannot be generalized to all patients with late-life depression. Dependent variables in this study were self-report measures. Whereas results may vary when using rater assessment or behavioral data, measures of perceived social functioning were shown to have clinically relevant predictive validity (Blazer, 2008, Cacioppo et al., 2010). The present study is cross sectional in nature. For instance, it does not show direct temporal effects of attachment style on age of onset of depression. In addition, whereas measures of attachment and social adaptation were attained on the same day, attachment styles explained between 13 and 20% of the variance in social adjustment. Attachment and social adaptation are only in part overlapping constructs perhaps based on their shared social nature. The SAS-SR has been shown to yield differing scores based on sex (Kornstein et al., 1995). The focus of the present study was not on sex, therefore analyses were conducted controlling for sex.
Depression and social functioning are linked by a two-way street. Depression may impair social adaptation. Poor social (e.g., interpersonal) proclivity may act as a predisposing factor for depression. Chronological age at the time of the first depressive episode is traditionally a clinically relevant factor in the assessment of depression. Most importantly, age of onset may carry etiological and treatment significance. Because depression beginning in early and later life have purported differing genetic and neuroanatomical risk factors (Baldwin and Tomenson, 1995, Blazer, 2003, Heun et al., 2000), the present study aimed at examining the extent to which attachment style and social adjustment parallel the extant conceptualization of early and late-onset depression (Blazer and Hybels, 2005, Herrmann et al., 2008). It was expected that early onset depression would be associated with greater insecure attachment style (i.e., a predisposition factor leading to onset of depression earlier in life) compared to late-onset depression and never-depressed volunteers. Predictions for current social functioning were less definite because if on the one hand poorer social functioning may have been expected in older individuals with onset of depression in youth (based on the longer duration of illness), the widely accepted “cerebrovascular nature” of late-onset depression was believed to potentially carry extra social impairment burden. In addition, it was predicted that current depression would be associated with greater social impairment (but not greater insecure attachment) compared with depression in remission.
Depression and remission
Consistent with the role of attachment style as vulnerability factor for depression both patients with current depression and in remission showed similar avoidant attachment scores (and significantly greater than non-depressed volunteers). Contrary to expectations, whereas patients with depression showed significantly worse current social maladaptation compared to non-depressed volunteers irrespective of their illness status (i.e., current and remission), the difference between current and remission did not reach significance in spite of a large group discrepancy in depression severity. This suggests that social adaptation in late-life depression may not fully recover after symptoms improvement and may require additional clinical attention even after many years after remission. Correlations between severity of depressive symptoms and SAS scores are now shown for comparison with prior research showing a link between severity of residual depressive symptoms and social impairment among patients in remission (Paykel et al., 1978). Results in the present study were consistent with previous research (Paykel et al., 1978). Among patients with current depression severity of symptoms (mean Ham-D severity = 20.4, SD=6.2) showed a Spearman’s rho = .32 (p=.056), whereas among subjects in remission (mean Ham-D severity = 4.3, SD=5.0) the correlation reached rho= .53 (p<.001), confirming that among person in remission residual symptoms carry significant risk for social maladaptation.
Early vs. late-onset depression
Contrary to expectations, while patients with late-life depression showed more insecure attachment and poorer social functioning than never-depressed volunteers, the difference between early- and late-onset depression was not significant. Analysis of the four attachment categories (Ainsworth, 1985) showed that almost 60% of never-depressed volunteers displayed secure attachment, while the insecure styles (preoccupied, dismissive, fearful) constituted about 68% for late-onset and 75% for early-onset depression (Table 3). None among the insecure attachment styles, however, was clearly more strongly associated over the others with early or late-onset depression.
Patients with late-life depression showed significantly greater social maladaptation than non-depressed volunteers in vocational, leisure, and family environments, but no difference between early- and late-onset depression reached statistical significance. These findings are consistent with earlier reports showing impairment in social adjustment in both young and older Australian adults with depression (Brodaty et al., 1993).
Much literature supports the role of cerebrovascular lesions as risk factors for late onset depression (Blazer and Hybels, 2005, Herrmann et al., 2008). It is possible that the consistency of the literature on vascular depression lead to a relative neglect for the role of attachment as a vulnerability factor in late-life depression (Bifulco et al., 2006, Conradi and De Jonge, 2009). The aggregate findings in this study (age of onset and illness status effects) suggest that insecure attachment may be a risk factor for both early- and late-onset depression.
Clinical relevance
Why subjects with late-onset depression who have insecure attachment do not develop depression earlier in life? It may be posited that other factors (including family support, social networks, physical activity) act as buffers in earlier life and prevent the development of depression. Later in life loss of familial and social network support, functional decline and (perhaps most importantly) comorbid medical conditions including cerebrovascular disease may compound with insecure attachment style to increase the susceptibility to develop depression. Therefore, addressing insecure attachment may contribute to primary and secondary prevention of late-life depression.
More research on personality dimensions as potential determinants of the outcome of late life depression has been advocated (Weber et al., 2011). Psychotherapy services (including brief psychodynamic psychotherapy, cognitive behavioral, supportive, grief, problem solving therapy, or a combination) have been reported to be effective for several Axis I disorders in the elderly (Patel et al., 2010, Serfaty et al., 2009, Stanley et al., 2009) but they are often underutilized (Payman, 2011). The role of psychotherapeutic interventions to address insecure attachment style among older persons remains to be tested.
In summary, the present study examining a sample of cognitively unimpaired older patients with depression indicated that anxious and avoidant attachment styles and social maladaptation are associated with depression irrespective of age of onset and illness status. Some results were contrary to expectations: 1. Greater insecure attachment found to be associated both with early- and late-onset depression may signify that attachment style is a risk factor for late-onset as is for early-onset depression; 2. Residual social impairment present in patients with late-life depression in remission warrants further research employing a longitudinal repeated measure design. Poorer social functioning in late-life depression irrespective of age of onset may signify that most disability may occur earlier on in the illness and the longer duration of illness (and number of illness episodes) does not appear to lead to critically worsening of social functioning. These results suggest that attention should be paid to attachment style as a potential risk factor for depression also in late-life, and to social impairment as residual disability even after symptoms remission. They indicate the road to further research on prevention and rehabilitation strategies for depression in late-life.
Key Points.
Determining mechanisms of depression depending on the age of onset (young adulthood versus later life) may be critical for effective treatment, prevention.
Onset depression during later life is widely believed to be associated with cerebrovascular illness. Much less is known on its psychosocial factors.
The present study found that individuals with onset of depression in later life (much like individuals with depression with onset in young adulthood) showed more insecure attachment style and poorer psychosocial adaptation relative to healthy volunteers of comparable age and sex both during the active phase of the illness as well as during remission.
Because attachment style develops during early parent-child interactions and shows relative stability, insecure attachment style may be an additional factor predisposing to late onset depression.
Acknowledgements
Sergio Paradiso was supported by the Dana foundation, the Mallinckrodt foundation, NARSAD and the National Institute on Aging (5K23AG027837).
References
- Ainsworth MD. Attachments across the life span. Bull N Y Acad Med. 1985;61:792–812. [PMC free article] [PubMed] [Google Scholar]
- Alexopoulos GS, Meyers BS, Young RC, Kakuma T, Silbersweig D, Charlson M. Clinically defined vascular depression. Am J Psychiatry. 1997;154:562–565. doi: 10.1176/ajp.154.4.562. [DOI] [PubMed] [Google Scholar]
- Atkinson L. Attachment and Psychopathology. New York: The Guilford Press; 1997. [Google Scholar]
- Baldwin RC, Tomenson B. Depression in later life. A comparison of symptoms and risk factors in early and late onset cases. Br J Psychiatry. 1995;167:649–652. doi: 10.1192/bjp.167.5.649. [DOI] [PubMed] [Google Scholar]
- Bifulco A, Kwon J, Jacobs C, Moran PM, Bunn A, Beer N. Adult attachment style as mediator between childhood neglect/abuse and adult depression and anxiety. Soc Psychiatry Psychiatr Epidemiol. 2006;41:796–805. doi: 10.1007/s00127-006-0101-z. [DOI] [PubMed] [Google Scholar]
- Blazer DG. Depression in late life: review and commentary. J Gerontol A Biol Sci Med Sci. 2003;58:249–265. doi: 10.1093/gerona/58.3.m249. [DOI] [PubMed] [Google Scholar]
- Blazer DG. How do you feel about…? Health outcomes in late life and self-perceptions of health and well-being. Gerontologist. 2008;48:415–422. doi: 10.1093/geront/48.4.415. [DOI] [PubMed] [Google Scholar]
- Blazer DG, 2nd, Hybels CF. Origins of depression in later life. Psychol Med. 2005;35:1241–1252. doi: 10.1017/S0033291705004411. [DOI] [PubMed] [Google Scholar]
- Brodaty H, Harris L, Peters K, Wilhelm K, Hickie I, Boyce P, Mitchell P, Parker G, Eyers K. Prognosis of depression in the elderly. A comparison with younger patients. Br J Psychiatry. 1993;163:589–596. doi: 10.1192/bjp.163.5.589. [DOI] [PubMed] [Google Scholar]
- Cacioppo JT, Hawkley LC, Thisted RA. Perceived social isolation makes me sad: 5-year cross-lagged analyses of loneliness and depressive symptomatology in the Chicago Health, Aging, and Social Relations Study. Psychol Aging. 2010;25:453–463. doi: 10.1037/a0017216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Conradi HJ, De Jonge P. Recurrent depression and the role of adult attachment: a prospective and a retrospective study. J Affect Disord. 2009;116:93–99. doi: 10.1016/j.jad.2008.10.027. [DOI] [PubMed] [Google Scholar]
- Fincham FD, Bradbury TN. Marital satisfaction, depression, and attributions: a longitudinal analysis. J Pers Soc Psychol. 1993;64:442–452. doi: 10.1037//0022-3514.64.3.442. [DOI] [PubMed] [Google Scholar]
- First MB, Spitzer RL, Gibbon M, Williams JBW. Structured Clinical Interview for DSM-IV-TR Axis 1 Disorder, Non-Patient Edition. Washington: American Psychiatric Association; 2002. [Google Scholar]
- Folstein MF, Folstein SE, Mchugh PR. "Mini-mental state". A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975;12:189–198. doi: 10.1016/0022-3956(75)90026-6. [DOI] [PubMed] [Google Scholar]
- Grossmann KE, Grossmann K, Waters E. Attachment from Infancy to Adulthood: The Major Longitudinal Studies. The Guilford Press; 2005. [Google Scholar]
- Haggerty G, Hilsenroth MJ, Vala-Stewart R. Attachment and interpersonal distress: examining the relationship between attachment styles and interpersonal problems in a clinical population. Clin Psychol Psychother. 2009;16:1–9. doi: 10.1002/cpp.596. [DOI] [PubMed] [Google Scholar]
- Hamilton M. A rating scale for depression. J Neurol Neurosurg Psychiatry. 1960;23:56–62. doi: 10.1136/jnnp.23.1.56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Herrmann LL, Le Masurier M, Ebmeier KP. White matter hyperintensities in late life depression: a systematic review. J Neurol Neurosurg Psychiatry. 2008;79:619–624. doi: 10.1136/jnnp.2007.124651. [DOI] [PubMed] [Google Scholar]
- Heun R, Kockler M, Papassotiropoulos A. Distinction of early- and late-onset depression in the elderly by their lifetime symptomatology. Int J Geriatr Psychiatry. 2000;15:1138–1142. doi: 10.1002/1099-1166(200012)15:12<1138::aid-gps266>3.0.co;2-7. [DOI] [PubMed] [Google Scholar]
- Kessing LV. Differences in diagnostic subtypes among patients with late and early onset of a single depressive episode. International journal of geriatric psychiatry. 2006;21:1127–1131. doi: 10.1002/gps.1617. [DOI] [PubMed] [Google Scholar]
- Kornstein SG, Schatzberg AF, Yonkers KA, Thase ME, Keitner GI, Ryan CE, Schlager D. Gender differences in presentation of chronic major depression. Psychopharmacol Bull. 1995;31:711–718. [PubMed] [Google Scholar]
- Krishnan KR, Hays JC, Tupler LA, George LK, Blazer DG. Clinical and phenomenological comparisons of late-onset and early-onset depression. Am J Psychiatry. 1995;152:785–788. doi: 10.1176/ajp.152.5.785. [DOI] [PubMed] [Google Scholar]
- Marazziti D, Dell'osso B, Catena Dell'osso M, Consoli G, Del Debbio A, Mungai F, Vivarelli L, Albanese F, Piccinni A, Rucci P, Dell'osso L. Romantic attachment in patients with mood and anxiety disorders. CNS Spectr. 2007;12:751–756. doi: 10.1017/s1092852900015431. [DOI] [PubMed] [Google Scholar]
- Patel V, Weiss HA, Chowdhary N, Naik S, Pednekar S, Chatterjee S, De Silva MJ, Bhat B, Araya R, King M, Simon G, Verdeli H, Kirkwood BR. Effectiveness of an intervention led by lay health counsellors for depressive and anxiety disorders in primary care in Goa, India (MANAS): a cluster randomised controlled trial. Lancet. 2010;376:2086–2095. doi: 10.1016/S0140-6736(10)61508-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paykel ES, Weissman MM, Prusoff BA. Social maladjustment and severity of depression. Compr Psychiatry. 1978;19:121–128. doi: 10.1016/0010-440x(78)90056-1. [DOI] [PubMed] [Google Scholar]
- Payman V. Psychotherapeutic treatments in late life. Current opinion in psychiatry. 2011 doi: 10.1097/YCO.0b013e32834a58bb. [DOI] [PubMed] [Google Scholar]
- Roberts JE, Gotlib IH, Kassel JD. Adult attachment security and symptoms of depression: the mediating roles of dysfunctional attitudes and low self-esteem. J Pers Soc Psychol. 1996;70:310–320. doi: 10.1037//0022-3514.70.2.310. [DOI] [PubMed] [Google Scholar]
- Serfaty MA, Haworth D, Blanchard M, Buszewicz M, Murad S, King M. Clinical effectiveness of individual cognitive behavioral therapy for depressed older people in primary care: a randomized controlled trial. Archives of general psychiatry. 2009;66:1332–1340. doi: 10.1001/archgenpsychiatry.2009.165. [DOI] [PubMed] [Google Scholar]
- Simpson JA, Rholes W. Attachment Theory and Close Relationships. New York: The Guilford Press; 1998. [Google Scholar]
- Stanley MA, Wilson NL, Novy DM, Rhoades HM, Wagener PD, Greisinger AJ, Cully JA, Kunik ME. Cognitive behavior therapy for generalized anxiety disorder among older adults in primary care: a randomized clinical trial. JAMA. 2009;301:1460–1467. doi: 10.1001/jama.2009.458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weber K, Giannakopoulos P, Canuto A. Exploring the impact of personality dimensions in late-life depression: From group comparisons to individual trajectories. Curr Opin Psychiatry. 2011;24 doi: 10.1097/YCO.0b013e32834a349f. [DOI] [PubMed] [Google Scholar]
- Wechsler D. Wechsler Abbreviated Scale of Intelligence. New York: The Psychological Association; 1999. [Google Scholar]
- Weissman M. Social Adjustment Scale-Self-Report. New York: Multi-Health Systems, Inc.; 1999. [Google Scholar]