Abstract
Context
Acute hemiparesis is a common initial presentation of ischemic stroke. Although hemiparesis due to spontaneous spinal epidural hematoma (SSEH) is an uncommon symptom, a few cases have been reported and misdiagnosed as cerebral infarction.
Design
Case reports of SSEH with acute hemiparesis.
Findings
In these two cases, acute stroke was suspected initially and administration of intravenous alteplase therapy was considered. In one case, the presentation was neck pain and in the other case, it was Lhermitte's sign; brain magnetic resonance imaging (MRI) and magnetic resonance angiography were negative for signs of ischemic infarction, hemorrhage, or arterial dissection. Cervical MRI was performed and demonstrated SSEH.
Conclusion
Clinicians who perform intravenous thrombolytic treatment with alteplase need to be aware of this possible contraindication.
Keywords: Spontaneous spinal epidural hematoma, Hemiparesis, Tetraparesis, Lhermitte's sign, Cerebral infarction, Intravenous thrombolytic treatment, Magnetic resonance imaging, Computerized tomography, Alteplase
Introduction
Spontaneous spinal epidural hematoma (SSEH) is a very rare condition requiring urgent diagnosis.1–12 The incidence of SSEH is estimated to be 0.1 patient per 100 000 individuals.3 SSEH typically presents acute onset of severe back pain and signs of compression of the spinal cord rapidly develop.1–12 Although hemiparesis due to SSEH is a relatively uncommon symptom compared with tetraparesis, a few cases of hemiparesis due to SSEH have been reported.1,2,4–11 Patients with hemiparesis due to SSEH have often been misdiagnosed as cerebral infarction and treated with anti-platelet therapy or anticoagulation.1,4,6,9–11 This is one of the pitfalls in emergency stroke cases. Therefore, physicians, especially those who perform intravenous thrombolytic treatment with alteplase, need to be aware of this possibility because alteplase may worsen SSEH and result in the patient's death. We describe two cases of SSEH with acute hemiparesis mimicking ischemic stroke in which intravenous thrombolytic treatment with alteplase was considered.
Case report
Case 1
A 71-year-old woman had sudden onset of neck and back pain followed by rapidly progressive right hemiparesis. She arrived at our hospital 90 minutes after the onset of her symptoms with suspected acute stroke. Neurological examination revealed right hemiparesis (muscle strength scored as 0/5 in upper limb and 2/5 in lower limb) with neither facial palsy nor sensory impairment. Deep tendon reflex (DTR) on the right side was exaggerated. The NIH Stroke Scale (NIHSS) score was 8. We suspected acute stroke and performed clinical examinations necessary for intravenous thrombolytic treatment with alteplase, brain magnetic resonance imaging (MRI) and magnetic resonance angiography (MRA) of the head, neck, and aorta. MRI was negative for signs of ischemic infarction or hemorrhage. MRA showed neither aortic nor arterial dissection. She met the conditions for intravenous alteplase therapy. Although administration of intravenous alteplase therapy was considered on suspicion of hyperacute cerebral infarction, spinal lesions needed to be excluded prior to administration because of back pain. Cervical MRI demonstrated an epidural hematoma causing compression of the spinal cord at levels C2 to T4 on the right (Fig. 1A–D). SSEH was diagnosed as the cause of right hemiparesis and intravenous alteplase therapy was cancelled. The patient was treated conservatively with steroids and glycerine so that she could undergo an emergent surgical decompression at any time. MRI 7 days after admission revealed no signs of epidural hematoma or abnormal enhancement (Fig. 1E and F) and the patient was discharged home following a complete recovery.
Figure 1.
Cervical MRI in case 1. Sagittal T1- (A) and T2- (C) weighted MRI immediately after the onset showed a longitudinal posterior epidural hematoma from C2 to Th4 (arrow head). Axial T1- (B) and T2- (D) weighted MRI immediately after the onset showed an ovoid epidural hematoma (arrow) in the right postero-lateral aspect and spinal cord (asterisk) compression. T1-weighted sagittal (E) and axial (F) with contrast MRI showed that the hematoma disappeared without abnormal enhancement following conservative treatment at 1 week after the onset.
Case 2
A 54-year-old woman had sudden onset of neck pain followed by rapidly progressive right hemiparesis. She arrived at the hospital 45 minutes after onset of symptoms with suspected acute stroke. She had a previous history of hypertension and alcoholic liver disease. Neurological examination revealed right hemiparesis (muscle strength scored as 3/5) and hyperesthesia in the right upper limb without facial palsy. DTR on the right side was exaggerated. The NIHSS score was counted as 5. Acute stroke was suspected and clinical examinations were performed in preparation intravenous thrombolytic treatment with alteplase, e.g. brain MRI and MRA. MRI and MRA were negative for signs of ischemic infarction, hemorrhage, or arterial dissection. She met the conditions for intravenous alteplase therapy. However, while being transferred from a stretcher to a bed, bending her neck forward caused an electrical sensation running down her back and into the limbs, indicating a positive Lhermitte's sign. Hence, cervical MRI was added on suspicion of spinal lesion. Cervical MRI demonstrated an epidural hematoma causing compression of the spinal cord at levels C3 to T2 on the right (Fig. 2A–D). Intravenous alteplase therapy was cancelled. The patient was treated conservatively so she could undergo emergency surgical decompression at any time. MRI 7 days after admission revealed resolution of the epidural hematoma (Fig. 2E and F) and the patient was discharged home completely recovered.
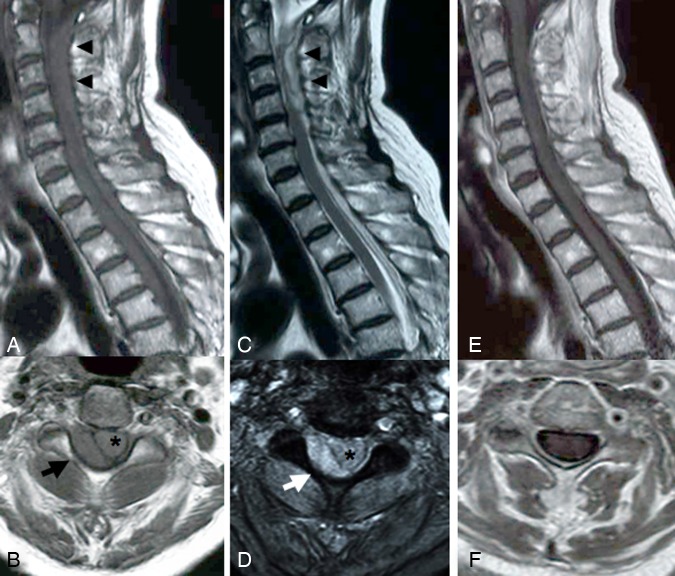
Figure 2.
Cervical MRI in case 2. Sagittal T1- (A) and T2- (C) weighted MRI immediately after the onset showed a longitudinal posterior epidural hematoma from C3 to Th2 (arrow head). Axial T1- (B) and T2- (D) weighted MRI immediately after the onset showed an ovoid epidural hematoma (arrow) in the right postero-lateral aspect and spinal cord (asterisk) compression. T1-weighted sagittal (E) and axial (F) MRI showed that the hematoma disappeared following conservative treatment at 1 week after the onset.
Discussion
Hemiparesis is generally caused by lesions of the corticospinal tract. The most common cause of hemiparesis is a cerebrovascular incident such as cerebral infarction.4 Although hemiparesis due to spinal cord disorders is rare, injury of the unilateral corticospinal tract in the cervical spinal cord causes hemiparesis.4,11 Hence, cervical SSEH, in which tetraparesis is a common symptom, can cause hemiparesis. In both these cases, an ovoid hematoma in the right postero-lateral aspect compressed only the right corticospinal tract and may have caused right hemiparesis.
Patients with hemiparesis due to SSEH have often been misdiagnosed as having cerebral infarction and been treated with anti-platelet therapy or anticoagulation.1,4,6,9–11 As a result, the hemiparesis worsened, and only then were they diagnosed with SSEH. Hence, physicians, especially those who perform intravenous thrombolytic treatment with alteplase, need to be aware of this possibility because alteplase may be contraindicated. Alteplase administration in the person with SSEH can be fatal.2
How can one distinguish the symptoms of SSEH with hemiparesis from cerebral infarction? SSEH is typically characterized by the sudden onset of neck and back pain followed by motor and sensory dysfunction.1–11 Table 1 summarizes the clinical features of recent reported cases of SSEH with hemiparesis. All cases had neck pain initially. Although there is a possibility of cerebral infarction due to vertebral artery dissection in cases of hemiparesis with neck pain,10 it is very important to ask patients whether they have back or neck pain. Lhermitte's sign may be useful for diagnosis of SSEH as in Case 2. Because the sign suggests a lesion of the dorsal columns of the cervical spinal cord,13 we suspected cervical spinal lesions. However, Tanaka et al. reported that Horner's syndrome could be an important sign for the diagnosis of SSEH in some cases.9 In fact, two cases in Table 1 showed Horner's syndrome in the clinical course. Moreover, 5 of the 13 cases showed Brown-Séquard's syndrome initially or during the clinical course.9,12 Although these two patients displayed neither Brown-Séquard's syndrome nor Horner's syndrome, clinicians should be aware that these syndromes may also indicate the possibility of SSEH.
Table 1.
Summary of recent reported cases of SSEH with hemiparesis
| Author (years) | Age (years) | Sex (M/F) | Initial symptoms | Misdiagnosis of CI (treatment for CI) | Reasons why SSEH was suspected | Treatment for SSEH | Outcome (GOS) |
|---|---|---|---|---|---|---|---|
| Adamson et al.1 | 63 | M | Neck pain, rt hemiparesis, and C5 B-S syndrome | + (Heparin) | Worsening of hemiparesis and B-S syndrome | Surgery | GR |
| Hsieh et al.4 | 65 | M | Neck pain and rt hemiparesis | + (Heparin) | Newly presented tetraparesis, urine retention, and B-S syndrome | Surgery | SD |
| Kadota et al.6 | 74 | F | Neck pain and rt hemiparesis | + (ND) | Worsening of hemiparesis newly presented rt sensory disturbance | Surgery | Dead |
| 64 | F | Neck pain and rt hemiparesis | – | Initial symptoms | Surgery | GR | |
| D'souza et al.2 | 62 | M | Neck pain, rt shoulder∼arm pain, rt hemiparesis, C4 B-S syndrome, and exaggeration of bilateral DTR | – | Initial symptoms | Surgery | GR |
| So et al.8 | 42 | F | Neck pain and lt hemiparesis | + (Aspirin) | Newly presented Horner's syndrome and C6 B-S syndrome | Surgery | MD |
| Tanaka et al.9 | 74 | F | Neck pain, lt hemiparesis and lt Babinski reflex | + (Argatroban) | Newly presented Horner's syndrome | Conservative | GR |
| Usami et al.10 | 80 | M | Neck pain, rt hemiparesis and rt paraesthesia | + (Heparin) | Newly presented tetraparesis | Surgery | SD |
| Ishikawa et al.5 | 82 | M | Neck pain and lt hemiparesis | – | Initial symptoms | Surgery | GR |
| Ofluoglu et al.7 | 63 | M | Neck pain, rt hemiparesis, and C5 B-S syndrome | – | Initial symptoms | Surgery | GR |
| Wang et al.11 | 69 | M | Neck and shoulder pain and rt hemiparesis | + (Heparin) | Worsening of hemiparesis newly presented lt sensory disturbance and exaggeration of bilateral DTR | Surgery | GR |
| Our cases | 71 | F | Neck and back pain, rt hemiparesis and exaggeration of rt DTR | – | Initial symptoms | Conservative | GR |
| 54 | F | Neck pain, rt hemiparesis, rt sensory disturbance, exaggeration of rt DTR and Lhermitte's sign | – | Initial symptoms | Conservative | GR |
B-S, Brown-Séquard; CI, cerebral infarction; DTR, deep tendon reflex; GOS, Glasgow outcome scale; GR, good recovery; MD, moderate disability; ND, not described; SSEH, spontaneous spinal epidural hematoma.
Recently, intravenous thrombolytic treatment with alteplase initiated within 3 hours of symptom onset has been approved in most countries for treatment of acute ischemic stroke.14 To perform the thrombolytic treatment, patients need to satisfy several conditions. To rule out intracranial hemorrhage or early ischemic signs pretreatment computed tomography (CT) is of the highest priority. MRI is not necessary to detect an ischemic lesion. This may be the pitfall in the emergent stroke cases in which intravenous thrombolytic treatment with alteplase is considered. It is well known that MRI is superior to CT in diagnosis of acute cerebral infarction because cerebral infarction can be detected by diffusion-weighted images within a few minutes of onset.15 If MRI is negative for signs of ischemic infarction, the physicians should consider not only hyperacute cerebral infarction but also cervical spinal lesions such as SSEH, especially when patients have back and neck pain.
Conclusion
In conclusion, although hemiparesis due to SSEH is very rare, physicians, especially those who perform intravenous thrombolytic treatment with alteplase, need to be aware of this possible contraindication. When patients with hemiparesis present with neck and back pain, SSEH should be considered. In such cases, Lhermitte's sign may be useful for diagnosis of SSEH.
References
- 1.Adamson DC, Bulsara K, Bronec PR. Spontaneous cervical epidural hematoma: case report and literature review. Surg Neurol 2004;62(2):156–9, discussion 159–60 [DOI] [PubMed] [Google Scholar]
- 2.D'Souza M, Gass A, Lyrer P, Ott HW, Baumann T. Intravenous thrombolysis cancelled in acute right hemiparesis. Cerebrovasc Dis 2008;26(6):665–6 [DOI] [PubMed] [Google Scholar]
- 3.Holtas S, Heiling M, Lonntoft M. Spontaneous spinal epidural hematoma: findings at MR imaging and clinical correlation. Radiology 1996;199(2):409–13 [DOI] [PubMed] [Google Scholar]
- 4.Hsieh CF, Lin HJ, Chen KT, Foo NP, Te AL. Acute spontaneous cervical spinal epidural hematoma with hemiparesis as the initial presentation. Eur J Emerg Med 2006;13(1):36–8 [DOI] [PubMed] [Google Scholar]
- 5.Ishikawa E, Saito A, Kujiraoka Y, Matsumura A. Recovery of increased signal intensity of the cervical cord on magnetic resonance imaging after surgery for spontaneous spinal epidural hematoma causing hemiparesis. Neurol India 2008;56(1):98–100 [DOI] [PubMed] [Google Scholar]
- 6.Kadota T, Abe T, Aihara H, Nishio S, Kawauchi M, Matsumoto Y. Spontaneous spinal epidural hematoma presenting with neck pain and hemiparesis. Neurosurg Emerg 2007;12:212–5 [Google Scholar]
- 7.Ofluoglu E, Ozdemir A, Toplamaoglu H, Sofuoglu E. Spontaneous cervical epidural hematoma causing Brown-Sequard syndrome: case report. Turk Neurosurg 2009;19(1):99–102 [PubMed] [Google Scholar]
- 8.So G, Debata A, Baba S, Tsunoda K, Suyama K, Nagata I. Spontaneous cervical epidural hematoma presenting with hemiparesis following neck extension: a case report. No Shinkei Geka. 2008;36(8):731–4 [PubMed] [Google Scholar]
- 9.Tanaka A, Nagakane Y, Hosomi A, Kuriyama N, Tokuda T, Nakagawa M. A case of acute spontaneous spinal epidural hematoma with sudden onset of hemiplegia under consideration for intravenous alteplase. Jpn J Stroke 2008;30:60–3 [Google Scholar]
- 10.Usami K, Tokumoto K, Ino T, Ozawa K, Kimura T, Nakamura S. Cervical epidural hematoma mimicking stroke: case report. Jpn J Stroke 2008;30:516–20 [Google Scholar]
- 11.Wang CC, Chang CH, Lin HJ, Lin KC, Kuo JR. Misdiagnosis of spontaneous cervical epidural haemorrhage. Eur Spine J 2009;18Suppl. 2:210–2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Cai HX, Liu C, Zhang JF, Wan SL, Uchida K, Fan SW. Spontaneous epidural hematoma of thoracic spine presenting as Brown-Séquard syndrome: report of a case with review of the literature. J Spinal Cord Med 2011;34(4):432–6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Garcia-Moreno JM, Izquierdo G. [Lhermitte's sign]. Neurologia 2002;17(3):143–50 Spanish [PubMed] [Google Scholar]
- 14.Hacke W, Kaste M, Bluhmki E, Brozman M, Davalos A, Guidetti D, et al. Thrombolysis with alteplase 3 to 4.5 hours after acute ischemic stroke. N Engl J Med 2008;359(13):1317–29 [DOI] [PubMed] [Google Scholar]
- 15.Chalela JA, Kidwell CS, Nentwich LM, Luby M, Butman JA, Demchuk AM, et al. Magnetic resonance imaging and computed tomography in emergency assessment of patients with suspected acute stroke: a prospective comparison. Lancet 2007;369:293–8 [DOI] [PMC free article] [PubMed] [Google Scholar]