Abstract
Objective. To describe the implementation of an advanced pharmacy practice experience (APPE) in medication therapy management (MTM) designed to contribute to student pharmacists’ confidence and abilities in providing MTM.
Design. Sixty-four student pharmacists provided MTM services during an APPE in a communication and care center.
Assessment. Students conducted 1,495 comprehensive medication reviews (CMRs) identifying 6,056 medication-related problems. Ninety-eight percent of the students who completed a survey instrument (52 of 53) following the APPE expressed that they had the necessary knowledge and skills to provide MTM services. Most respondents felt that pharmacist participation in providing Medicare MTM could move the profession of pharmacy forward and that pharmacists will have some role in deciding the specific provisions of the Medicare MTM program (92% and 91%, respectively).
Conclusion. Students completing the MTM APPE received patient-centered experiences that supplemented their confidence, knowledge, and skill in providing MTM services in the future.
Keywords: medication therapy management, advanced pharmacy practice experience, student pharmacists, patient-centered care
INTRODUCTION
Twenty-one percent of adverse drug events are avoidable, and preventable medication-related problems are a concern in the healthcare system.1 Along with being detrimental to patients’ well-being, medication-related problems have an overwhelming financial impact. In the year 2000, the cost of medication-related morbidity and mortality exceeded $177.4 billion.2 In an attempt to address these issues for Medicare beneficiaries, the Medicare Modernization Act of 2003 required Part D Prescription Drug Plan sponsors to provide MTM services to members meeting certain eligibility requirements.3-5 The goal of MTM is to optimize therapeutic outcomes by improving medication use and reducing the risk of adverse events, including drug-drug interactions. These MTM services may be provided by pharmacists or other qualified providers.3 With MTM being an opportunity for pharmacists to provide patient-centered care, colleges and schools of pharmacy have a responsibility to produce pharmacists who are prepared and confident in their ability to provide MTM services.
The American College of Clinical Pharmacy and the American Association of Colleges of Pharmacy (AACP) promote standards for pharmacy education that incorporate patient-centered experiences to optimize medication therapy, improve outcomes, and promote disease prevention.6,7 AACP presents its ideals for pharmacy education outcomes under the Center for the Advancement of Pharmaceutical Education (CAPE), the guidelines of which emphasize the importance of using patient-centered pharmaceutical care experiences to develop students’ skills in gathering comprehensive patient information, using literature to identify potential drug-related problems, recommending appropriate therapy, and creating a patient-monitoring plan to achieve therapeutic outcomes.7 Both organizations further suggest that student pharmacists use communication and collaboration with the entire healthcare team.6,7 Additionally, the Accreditation Council for Pharmacy Education’s curriculum guidelines require that the goals of a college or school of pharmacy include preparation of students who possess the competencies necessary for the provision of pharmacist-delivered patient care, including MTM services.8 Advanced pharmacy practice experiences (APPEs) in MTM can offer exposure to all of these activities, and many colleges and schools of pharmacy have implemented MTM in their curriculum. By incorporating patient-centered MTM experiences, colleges and schools of pharmacy can provide students with the skill set necessary to perform effective MTM services as independent pharmacy practioners.9,10
In response to the Centers for Medicare & Medicaid Services (CMS) MTM requirements for Medicare Part D plans, WellCare Health Plans, Inc., approached The University of Florida College of Pharmacy about providing MTM services to eligible plan members. The college viewed this as an opportunity to develop a unique practice model to educate fourth-year student pharmacists. Providing the core elements of MTM, as defined by the American Pharmacists Association, would offer students direct patient-care experience and cultivate student self-efficacy in providing MTM services. WellCare and the University of Florida negotiated a 2-year contract, resulting in WellCare funding the MTM Center at a mutually agreeable annual rate. After only 6 months of planning, the first student-staffed MTM Communication and Care Center at the College of Pharmacy campus in Gainesville opened on March 1, 2010. The purpose of this paper is to describe the creation and implementation of an APPE in MTM that provided fourth-year student pharmacists a patient-centered experience using unique technology and introducing exemplary educational opportunities focused on improving student self-efficacy.
DESIGN
In 2010, the college expanded its APPE experiences to include more direct patient care by creating an MTM Communication and Care Center. The objective of this center was to allow student pharmacists the opportunity to apply their pharmaceutical care skills to increase their confidence and abilities in providing MTM services. Upon completion of the APPE, students were expected to be proficient in 3 main areas: understanding, explaining, and providing patient education for core disease states; identifying all medication-related problems found during a comprehensive medication review; and communicating efficiently, appropriately, effectively, and professionally with patients and other healthcare professionals.
Technology was vital to the functionality of the MTM Center, both from an educational standpoint and for providing access to patient data necessary for performing MTM services. Each workspace was outfitted with a headset-equipped telephone. CMS reported in 2010 that 99.9% of MTM programs perform interactive, person-to-person comprehensive medication review (CMR) consultation by phone,6 and patients have proven to be receptive to and positive about telephone MTM.11
Students worked within a virtual desktop infrastructure installed on each computer, which provided a secure working environment for privacy-protected health information. Patient data were contained within Elsevier/Gold Standard’s MTM Exchange (Tampa, FL), Web-based software that provided patient demographic information, diagnosis codes, and prescription refill history. An electronic patient chart was maintained within MTM Exchange to document information collected during the CMR and assisted in creating a medication action plan for the patient as well as physician correspondence by facsimile, as necessary.
The MTM Communication and Care Center focused on creating an environment wherein students had autonomy but also access to preceptors to assist with any urgent issue or patient crisis. The MTM Center used classroom management software by CrossTec called SchoolVue (Boca Raton, FL) to ensure continuous, live, call-center monitoring. SchoolVue enabled MTM Center preceptors to monitor student workstations and phone calls remotely, while allowing students to assume responsibility for patient MTM services. Preceptors and students used a “chat” function within SchoolVue that enabled continuous communication. Telephone interviews were recorded using CallREC (Zoom, Brentwood, TN), a Web-based service. Call monitoring was used in assessing student progress in meeting learning objectives and for student training and quality assurance.12
Faculty preceptors listened to live student calls and provided educational feedback until they were confident that the students were communicating effectively and professionally and providing accurate information. Students were then released to continue handling patient calls independently, with preceptors listening randomly to the interactions to monitor for continued quality of communications. Monitoring was achieved in a live setting during actual calls and by reviewing recorded calls. Any concerns regarding students’ ability to communicate were addressed immediately and used as learning opportunities.
As part of the pharmacy curriculum, students had had previous exposure to MTM concepts. MTM case studies were interspersed throughout the students’ first 3 years of the pharmacotherapy course sequence, and during their third year, they also had a 3-hour skills laboratory experience involving a didactic lecture in MTM and interactive MTM patient-care practice cases. These experiences provided a basic foundation for the MTM APPE. Along with necessary additional training, mentorship was essential for the students. Each month of the year, 12 fourth-year student pharmacists provided MTM services at the center: 6 first-month students and 6 second-month students on a 2-month drug information/geriatric clerkship practice experience. These practice experiences were staggered to allow more experienced students to mentor the newer students.
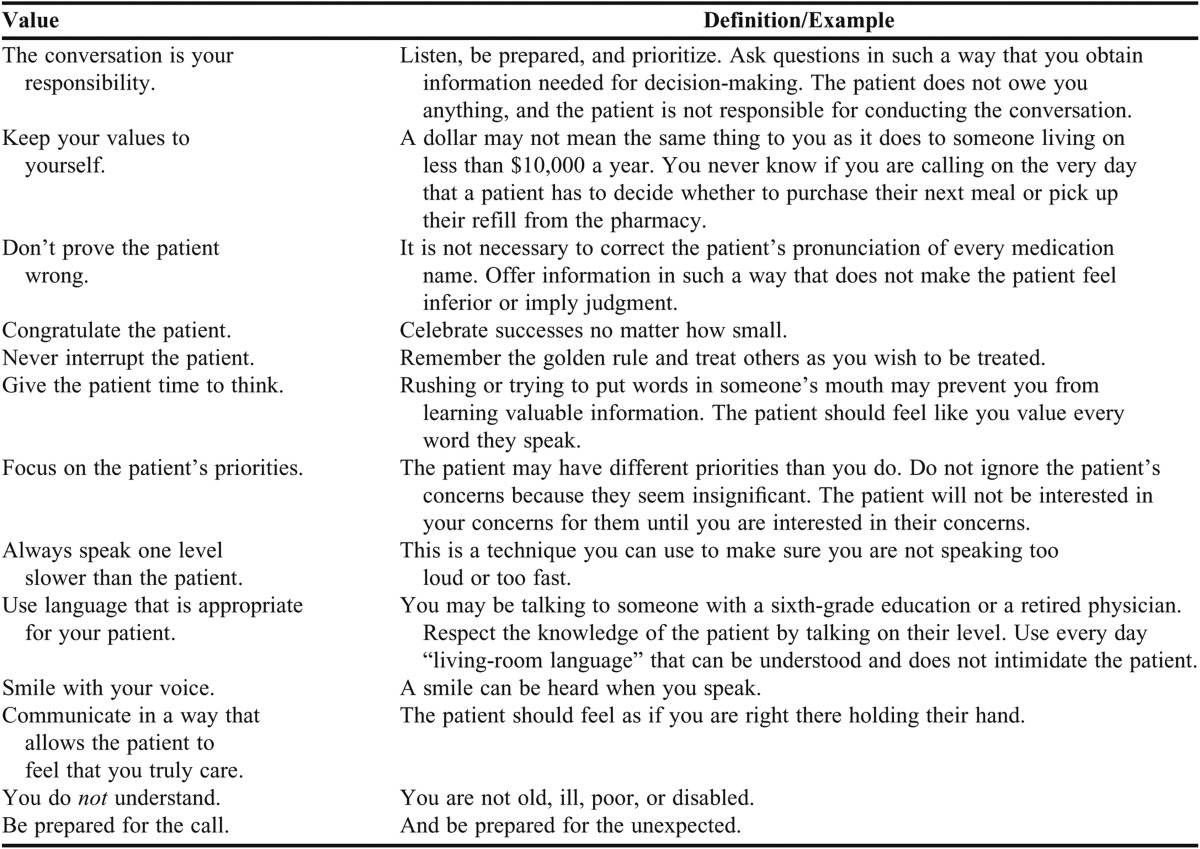
The students began their APPE with a week of intensive training. In addition to introducing the software, the training focused on helping students understand the purpose and requirements for MTM, use effective listening and communication skills, display appropriate empathy, and recognize and overcome the barriers of providing telephonic MTM services (Table 1). Students attended an Aging Sensitivity Training Course, during which they experienced simulated effects of glaucoma, macular degeneration, decreased hand dexterity and sensitivity, decreased stability in ambulation, and other disease-related obstacles.
Table 1.
Important Orientation Points for Student Pharmacists Providing Medication Therapy Management (MTM) Services at Call Center
Crisis Training that was provided has proved beneficial. The students learned how to listen for verbal cues indicating that a patient could be experiencing a crisis and were given the tools to address these situations. One CMR call elicited that a patient had a plan and a means of committing suicide. The student pharmacist assigned to this case followed the crisis protocol and transferred the patient to a crisis counselor to address the situation. During the follow-up call by the student pharmacist, the patient expressed being extremely thankful for the time and information that was provided to him during his ordeal.
The WellCare’s Medicare Part D members who participated in the MTM program were identified based on eligibility requirements set forth in the Affordable Care Act.13 Patient eligibility requirements for WellCare members included having 3 or more chronic disease states, 8 or more medications, and $3,000 or more in annual medication expenditures. WellCare contacted eligible members and forwarded only the names of those who agreed to participate in the CMR to the MTM Communication and Care Center. Each participant was contacted by an administrative employee to schedule an appointment at the patient’s convenience and then the patient was assigned to a student pharmacist.
Once a patient was assigned to the student pharmacist, the student pharmacist began what was termed the pre-CMR process, which involved evaluating information available prior to the telephone interview, such as patient demographics, 180 days of WellCare prescription claim history, and diagnosis codes provided through MTM Exchange. Students spent an average of 40 minutes on each pre-CMR activity identifying potential medication-related problems to be assessed during the CMR call. Potential problems included drug-drug interactions, drug-disease interactions, drug-age interactions, duplicate therapies, drugs missing indications, lack of therapy, and noncompliance. Generic, formulary, and combination options relevant to the patient’s current medication regimen were also considered. Multiple drug-information programs, medical references, and therapeutic guidelines were used by students during the pre-CMR process. After preparing the pre-CMR, students met with their faculty preceptors to discuss methods for effective communication, define appropriate questions, and set priorities for the call. After receiving preceptor approval of their pre-CMRs, students conducted telephone interviews with patients.
Students spent an average of 45 minutes on the phone with patients for each CMR call. During these calls, they collected an accurate list of all current medications, including those not appearing on the patients’ precall medication fill history, as well as indications and dosing regimens for each medication. Students asked their patients to describe any medication side effects they may have experienced as well as any barriers to medication compliance they had faced. Additionally, student pharmacists offered counseling points and educational information specific to each patient’s medication therapy and disease states. Students made a conscious effort not to undermine or devalue the relationship their patients had with their personal physician and local pharmacist and always referred patients to physicians for any specific medication or lifestyle changes.
Following their telephone interviews, student pharmacists practiced decision-making skills by conducting a postcall analysis of information obtained from each patient. They identified any new medication-related problems and prioritized problems that needed to be addressed with each patient’s healthcare team. After completing a full assessment and plan of action, students prepared a personal medication record and a medication action plan within the MTM Exchange software program. This combined document was subsequently mailed to the patient. The medication action plan provided patients with a summary of what had been discussed during the telephone interview and tips and recommendations specific to each patient’s therapeutic goals. Medication-related problems that were determined to require physician correspondence were communicated to the prescriber by means of a facsimile prepared by the student pharmacist within the MTM Exchange software. This physician correspondence provided pertinent patient information that was gathered during the call and related to perceived medication-related problems as well as recommendations with references, if appropriate. A phone call to the physician was made in any situation that required a more timely action.
Quarterly follow-up reviews were performed for each patient to note any resolved interventions and to identify new medication-related problems that may have still needed to be addressed. Students were expected to complete 3 CMRs daily, supplemented by medication reviews for patients residing in long-term care facilities. Medication reviews are conducted in a manner similar to that of CMRs but may not require person-to-person interaction with the patient. Any potential medication-related problems noted during the medication review were then communicated to the facility and the attending providers. Upon completion of the practice experience, students had the opportunity to complete approximately 90 CMRs, in addition to varying numbers of quarterly follow-ups and medication reviews.
Three clinical pharmacists served as faculty preceptors for the students. The call center was organized in a way that afforded students their own space to perform MTM telephone interviews in a private setting while simultaneously allowing direct access to faculty members through technology. Each morning at the center began with faculty preceptors conducting verbal “rounds,” during which they discussed the current day’s patient cases with the student pharmacists. Afterward, preceptors continued with their other case review duties while visually and audibly overseeing the student pharmacists’ work using the SchoolVue program and remaining available to the students throughout the day for consultation, as necessary.
Each participating faculty member was assigned 4 student pharmacists to precept each month. Faculty preceptors and staff pharmacists reviewed all case work and documents created by the students, including precall patient reports and postcall charts, personal medication records, medication action plans, and physician faxes. Documents did not leave the MTM Center until a final review was performed by a licensed pharmacist. This often required multiple editing sessions with the student pharmacist. When the pharmacist had given final approval of the CMR, the physician fax was sent by the pharmacist, and the personal medication record and medication action plan were mailed to the patient by WellCare. Preceptors had a formal one-on-one evaluation with their students at the midpoint and end of the practice experience.
EVALUATION AND ASSESSMENT
The MTM APPE was assessed through 3 mechanisms: an evaluation of the impact of the students’ MTM on patient care, preceptor evaluation of student learning, and a survey of students’ perceptions of MTM after completing the APPE. Between March 1 and December 31, 2010, the MTM Communication and Care Center offered services to 3,339 patients residing throughout the United States. Approximately 45% (n=1,495) of these patients agreed to accept the services and were provided a CMR. For an additional 387 patients who could not participate in the interview portion of a CMR, student pharmacists performed a medication review without a telephone encounter for a total of 1,882 reviews. The balance of our population either refused any services or were unreachable.
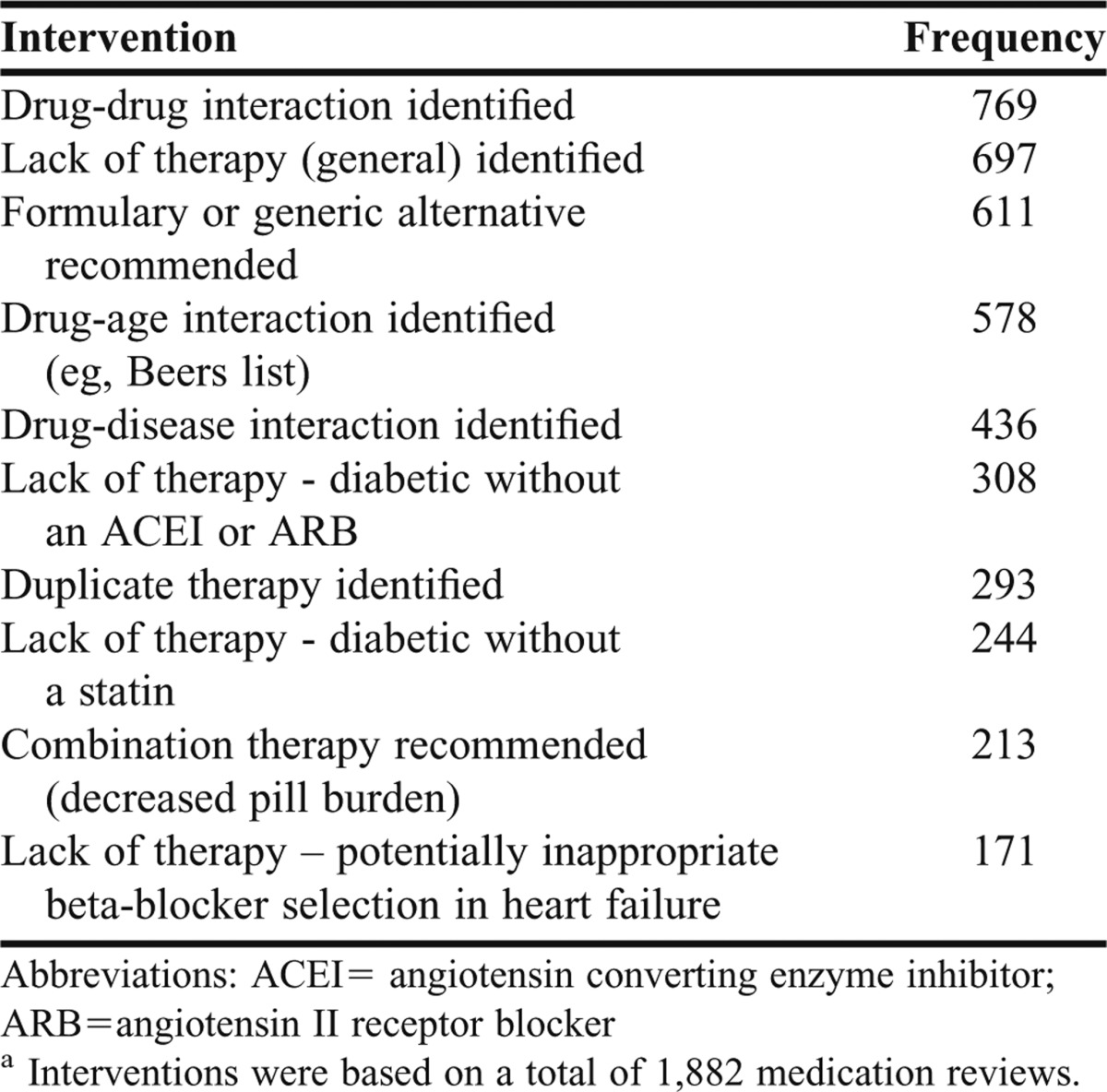
While performing the reviews during the MTM APPE, student pharmacists identified 6,056 medication-related problems (approximately 4 per patient) and communicated them to the patients’ respective healthcare teams. For these medication-related problems, student pharmacists entered 12,590 interventions overall, the most common of which are listed in Table 2. Projections for the 2011 calendar year were that the MTM Center would offer these services to over 10,000 MTM-eligible WellCare members, allowing for expanded opportunities to counsel, educate, and assist a larger population of high-risk patients.
Table 2.
Top Ten Interventionsa for Medication-Related Problems or Opportunities Entered by Student Pharmacists Providing Services at the Medication Therapy Management (MTM) Call Center in 2010
Students were provided daily feedback on all pre-CMR work. During this phase of the experience, a template was created and used by students to organize all potential medication-related problems identified for each patient. The template included the following categories for potential problems noted: drug-drug interactions, drug-age interactions, duplicate therapies, lack of guideline-based therapies, noncompliance issues, excessive duration of medication use, generic and formulary alternatives, potential regimen simplification, and potentially untreated conditions. Students were expected to accurately and completely identify these issues for each patient based on diagnosis codes and prescription claims history. Students’ core knowledge of disease states was easily assessed with this tool, allowing deficiencies to be readily identified and used as educational opportunities during the preceptor-student daily feedback sessions. Constant verbal and written feedback centering on this pre-CMR template allowed for continuous assessment and provided ongoing evidence of student learning throughout the APPE.
Preceptors monitored live calls and recorded calls using CallREC to evaluate students’ ability to communicate with the patients empathically, efficiently, appropriately, and professionally and to assess their skills in educating and counseling patients. Preceptors also reviewed the students’ performance in providing appropriate and accurate information to the patients, communicating at the correct language-level, and asking reflective questions to ensure that patients understood the information or instructions given. Any deficiencies in communication skills were immediately expressed to the students through feedback, followed by a discussion about more appropriate alternatives. Continuous call monitoring ensured that students consistently improved and maintained appropriate patient communication.
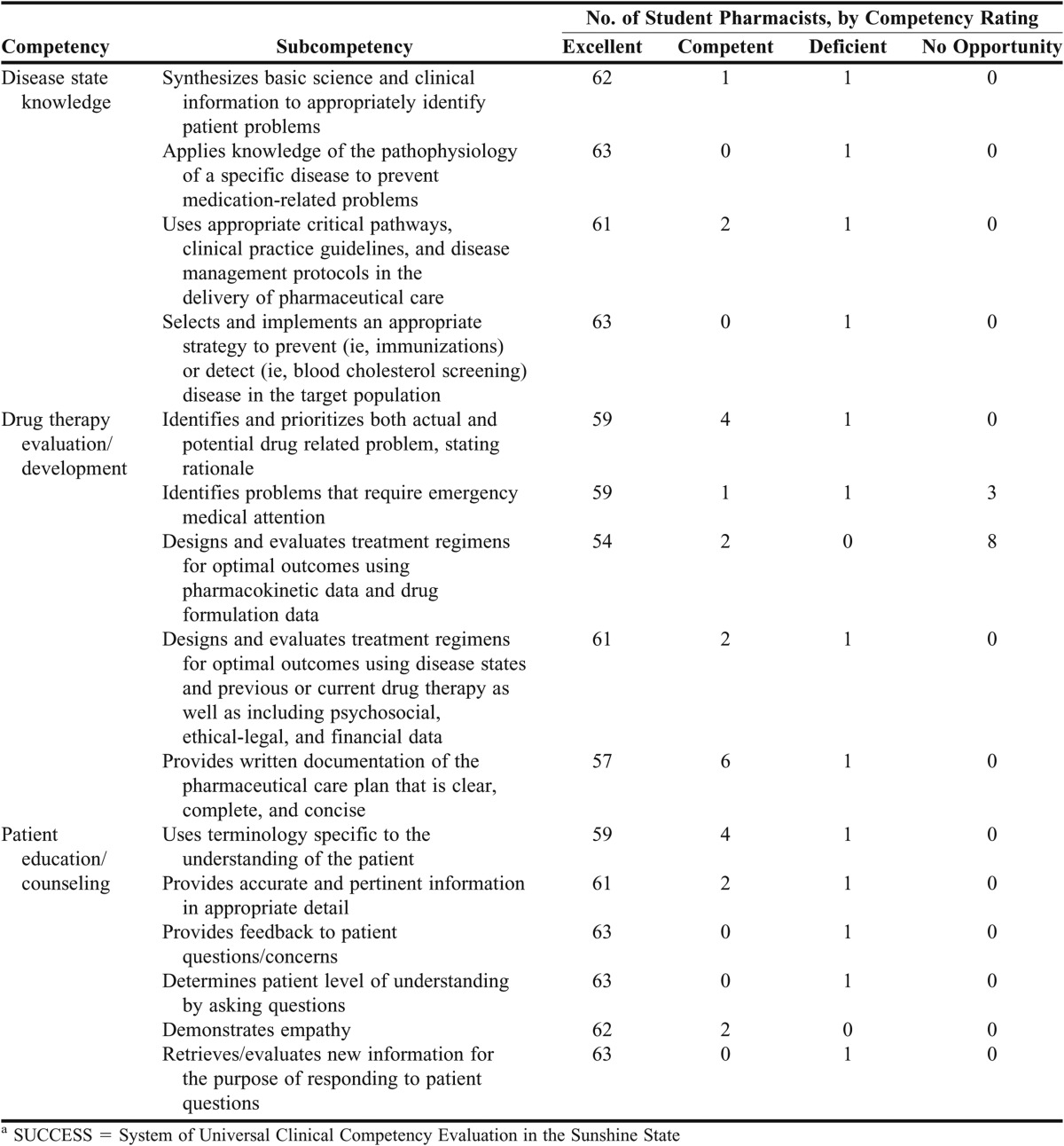
Students were expected to review all collected patient data and use clinical decision-making skills to evaluate drug therapy, address medication-related problems, and make recommendations for optimization of drug regimens. To assess the students’ drug therapy evaluation skills, preceptors reviewed the students’ postcall patient cases, ensuring that all documentation was accurate and complete. Postcall charts were then reviewed to ensure that, for each decision, there was documentation of appropriate action for any issues identified and justification for interventions. Final correspondence documents to the patient and prescriber were reviewed and approved by the preceptor and used to assess the students’ written communication skills. The preceptors used this review of the students’ pre-CMR templates, student calls, and final charts to assess student learning throughout the APPE, provide students feedback, and evaluate students on SUCCESS competencies. SUCCESS, which stands for System of Universal Clinical Competency Evaluation in the Sunshine State, is an online assessment tool for evaluating students during their advanced practice year.
Student performance was addressed formally at midterm and at the APPE culmination in a summative evaluation using the SUCCESS competencies.14 These competencies cover many areas of expectations for successfully completing the APPE. The end-of-term competencies and subcompetency scores for the 2010-2011 APPE students relating to the 3 main objectives are presented in Table 3. A score of “excellent” indicated that the student met the competency criteria consistently and independently; “competent” indicated that the student met the competency criteria consistently but with guidance from the preceptor. A score of “deficient” reflected that, even with guidance from the preceptor, the student was unable to meet these criteria. Items to which the student had no exposure during the APPE were marked “no opportunity” and did not factor into the student’s evaluation score.
Table 3.
Final Competency Ratings of Student Pharmacists (N=64) at the Medication Therapy Management Call Center, by Competency Category of the SUCCESSa Grading Program
Faculty preceptors determined that by the end of the practice experience, the majority of students had excelled at using their knowledge of clinical disease states to correctly identify potential medication-related problems and evaluate drug therapy in the MTM patient population. Preceptors also agreed that students’ interviewing, counseling, and patient education skills greatly improved over the course of the APPE, with most students scoring “excellent” in these subcompetencies as well. One student was found to be deficient in most competencies early in the practice experience and did not complete the APPE.
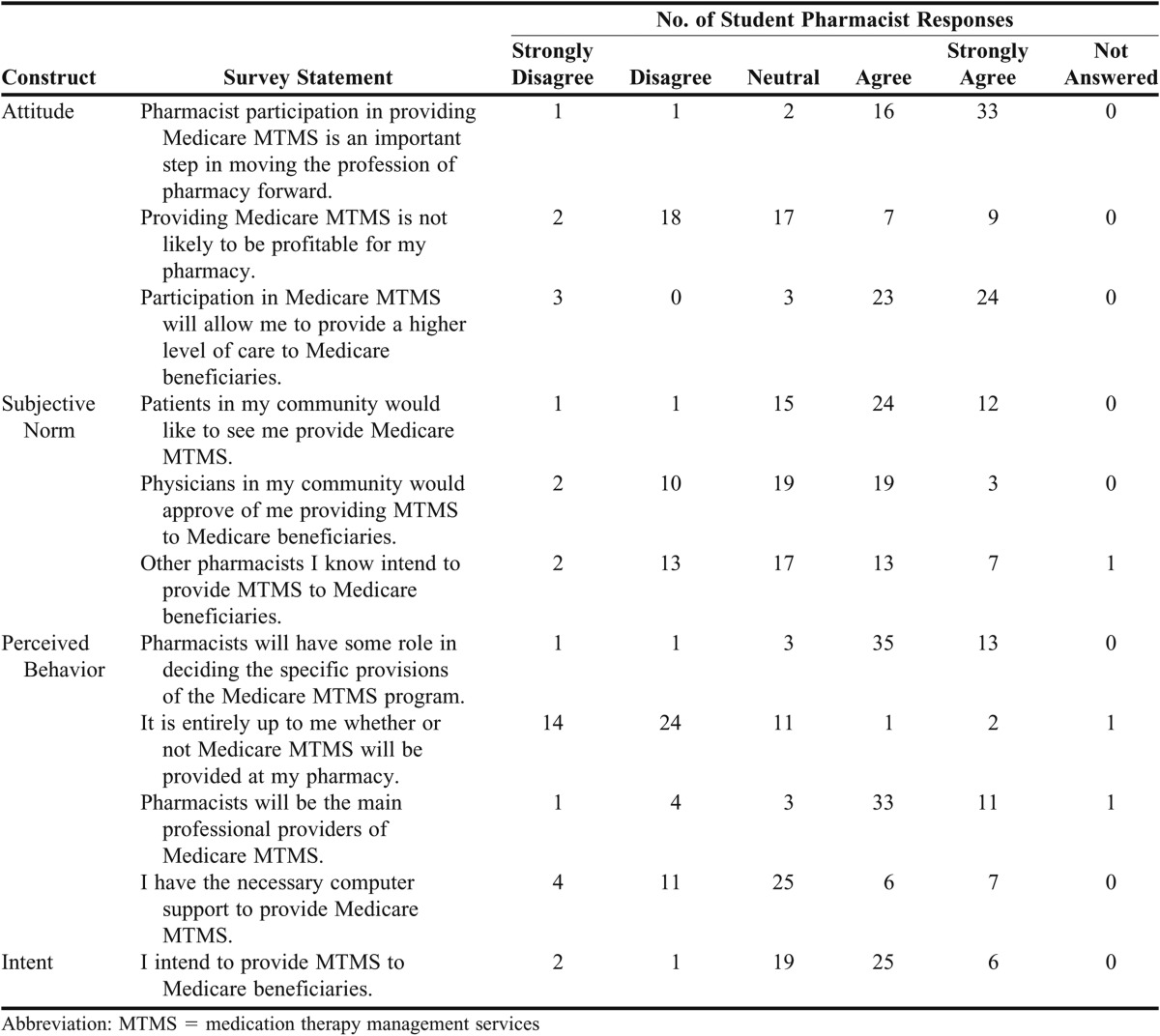
During the spring of 2011, fourth-year student pharmacists who completed the MTM APPE for the 2010-11 school year were offered a 38-question survey instrument to evaluate their attitudes toward providing MTM services as a practicing pharmacist. This survey instrument was modeled after the validated University of Iowa College of Pharmacy Survey on Medicare Medication Therapy Management Services. Five survey items were sociodemographic and the other 33 addressed various aspects of pharmaceutical care. Eleven items specifically evaluated the students’ attitudes, subjective norms, perceived behavioral control, and intention to provide MTM, as defined by the Theory of Planned Behavior. This theory suggests that these attitudes and perceptions will affect a person’s behavior and, therefore, could predict a student’s intent to provide MTM services.15 The summary of responses to the 11 items related to planned behavior are presented in Table 4. All other survey results are available upon request from the corresponding author.
Table 4.
Responses (N=53) to Theory of Planned Behavior Items Included in a Survey of Student Pharmacists’ Perceptions of Medicare Medication Therapy Management Services
Fifty-three (83%) of the 64 student pharmacists polled completed the survey instrument. All but 1 of the respondents either agreed or strongly agreed that they had the necessary knowledge and skills to provide MTM services to Medicare beneficiaries. There was also strong agreement that pharmacist participation in providing Medicare MTM is an important step in moving the profession of pharmacy forward and that pharmacists will have some role in deciding the specific provisions of the Medicare MTM program (92% and 91%, respectively, agreed or strongly agreed).
DISCUSSION
MTM is a platform that allows pharmacists to be at the forefront of individualized patient care by playing a key role in ensuring patient safety: instructing patients on the proper administration of medications; identifying and preventing drug interactions; and detecting duplicate therapies and adverse drug reactions.16 Providing student pharmacists direct patient-care experience in MTM is an important part of preparing them for the challenges and opportunities they will face in their professional careers.
The MTM Communication and Care Center at the University of Florida is an environment where students can have the experience of providing direct patient care autonomously while being continually monitored for performance. This arrangement grants students the freedom to gain experience in making their own decisions in patient care and allows preceptors to monitor the students’ activities and provide guidance and instruction as needed. The technology required for this experience is essential to the process of following MTM Center protocols for managing patient crisis situations.
The SUCCESS Competency data (Table 3) reflect that this MTM APPE was successful in achieving its core objectives. Students succeeded in understanding and assessing core disease states, evaluating medication regimens, educating patients, using this clinical knowledge to identify medication-related problems and appropriately communicating these issues to patients and prescribers. To evaluate the effect of this APPE on students’ attitudes about MTM, we searched for survey instruments that would encompass all the information we intended to capture from our students,17-19 The instrument deemed most appropriate for our purposes was the University of Iowa survey instrument16 However, because of its focus on the perceptions of practicing community pharmacists rather than those of student pharmacists who had yet to become practitioners, we used a modified version of the original survey instrument created in 2005 to assess University of Iowa student pharmacists.20 The results of our survey were comparable to those of the Iowa assessment in that our student cohort and the Iowa students both felt strongly that pharmacist participation in MTM is important to the profession of pharmacy (92% and 93%, respectively). One difference was that the Iowa students had the highest level of agreement with the statement about the importance of MTM to the pharmacy profession, whereas all but 1 of the University of Florida students agreed or strongly agreed regarding the perception that they possessed the necessary knowledge and skills to provide MTM services to Medicare beneficiaries. This finding suggests that the APPE at the MTM Communication and Care Center may have improved the self-efficacy of the participating student pharmacists.
Limitations to our study include the lack of student exposure to certain community pharmacy MTM barriers, such as the need to resolve workflow or economic issues or to address management support for providing MTM services. Time is often a barrier in community pharmacies, whereas in our APPE, there were minimal time constraints and our students were able to spend as much time with each patient as needed. Additionally, our students did not have to convince patients to participate in MTM, as WellCare provided that service. Our student pharmacists most frequently communicate with practitioners by facsimile, whereas community pharmacists often conduct real-time therapeutic interventions with healthcare providers by telephone. Many of the survey questions focused on the above-listed issues, despite the fact that at the time of the survey, our students may not have had exposure to these obstacles. Our survey may be limited in that it was not a pre- and post-APPE assessment. Student pharmacists in our APPE may have had other exposure to MTM in the curriculum and in different practice experiences; thus, the current experience may not be the only contributor to their opinions regarding MTM.
The results of our survey suggest that the University of Florida APPE practice model can lead to student pharmacists’ perception that they have adequate knowledge to provide MTM services in their future careers as well as their intention to do so. It also may increase student pharmacist awareness regarding the impact that pharmacists can achieve in the realm of MTM. Supplying more training and education in MTM may provide student pharmacists the means to overcome barriers to providing MTM services as they enter into their pharmacy careers.18
SUMMARY
This MTM advanced practice experience provided student pharmacists an opportunity to provide patient-centered care using unique technology and to take advantage of exemplary educational opportunities focused on improving student self-efficacy in MTM. As colleges and schools of pharmacy begin to provide more direct patient care experiences in MTM, student pharmacists will have the opportunity to gain confidence in their ability to provide these important services to patients as well as to develop skills that will be useful in overcoming barriers to the provision of MTM that they may encounter in their careers as pharmacists.
REFERENCES
- 1.Thomsen LA, Winterstein AG, Sondergaard B, et al. Systematic review of the incidence and characteristics of preventable adverse drug events in ambulatory care. Ann Pharmacother. 2007;41(9):1411–1426. doi: 10.1345/aph.1H658. [DOI] [PubMed] [Google Scholar]
- 2.Ernst FR, Grizzle AJ. Drug-related morbidity and mortality: updating the cost-of-illness model. J Am Pharm Assoc (Wash) 2001;41(2):192–199. doi: 10.1016/s1086-5802(16)31229-3. [DOI] [PubMed] [Google Scholar]
- 3.Medicare part D medication therapy management (MTM) programs 2009 fact sheet. Centers for Medicare and Medicaid. https://www.cms.gov/Medicare/Prescription-Drug-Coverage/PrescriptionDrugCovContra/downloads/MTMFactSheet_2009_06-2009_fnl.pdf Accessed July 6, 2012.
- 4.2010 Medicare part D medication therapy management (MTM) programs. Centers for Medicare and Medicaid. http://www.amcp.org/WorkArea/DownloadAsset.aspx?id=9525. Accessed July 6, 2012.
- 5.CMS legislative summary: the Medicare prescription drug, improvement, and modernization act of 2003, public law 108-173, summary of HR1. Centers for Medicare and Medicaid. http://www.ruralcenter.org/sites/default/files/MMA2003.PDF. Accessed July 6, 2012.
- 6.Haase KK, Smythe MA, Orlando PL, et al. ACCP white paper: quality experiential education. Pharmacotherapy. 2008;28(10):219e–227e. doi: 10.1592/phco.28.12.1548. [DOI] [PubMed] [Google Scholar]
- 7.Pharmacy practice supplemental educational outcomes based on CAPE 2004. American Association of the Colleges of Pharmacy (AACP) http://www.aacp.org/resources/education/Documents/PharmacyPracticeDEC006.pdf. Accessed May 20, 2012.
- 8.Accreditation standards and guidelines for the professional program in pharmacy leading to the doctor of pharmacy degree. Accreditation Council for Pharmacy Education. http://acpe-accredit.org/pdf/S2007Guidelines2.0_ChangesIdentifiedInRed.pdf. Accessed May 20, 2012.
- 9.Kuhn C, Powwell P, Sterrett J. Elective course on medication therapy management services. Am J Pharm Educ. 2010;74(3):Article 40. doi: 10.5688/aj740340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Eukel HN, Skoy ET, Frenzel JE. Provision of medication therapy management to university faculty and staff members by third-year pharmacy students. Am J Pharm Educ. 2010;74(10):Article 182. doi: 10.5688/aj7410182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Moczygemba L, Barber J, Brown C, et al. Patient satisfaction with a pharmacist-provided telephone medication therapy management program. Res Social Admin Pharm. 2010;6(2):143–154. doi: 10.1016/j.sapharm.2010.03.005. [DOI] [PubMed] [Google Scholar]
- 12.Yang T, Hardin H, Sessions P. The use of technologies to promote autonomy in a student-staffed medication therapy management call center. [Abstract] Am J Pharm Educ. 2011;75(5):Article 105. [Google Scholar]
- 13.Compilation of Patient Protection and Affordable Care Act. US Dept of Health & Human Services. http://docs.house.gov/energycommerce/ppacacon.pdf. Accessed May 20, 2012.
- 14.SUCCESS Competencies, Subcompetencies, Definitions and Weighting Web site. Created by Florida A&M University, Nova Southeastern University, Palm Beach Atlantic University, and University of Florida. 2005. https://copnt17.cop.ufl.edu/ugsp/. Accessed June 12, 2011.
- 15.Herbert K, Urmie J, Newland B, et al. Prediction of pharmacist intention to provide Medicare medication therapy management services using the theory of planned behavior. Res Social Admin Pharm. 2006;2(3):299–314. doi: 10.1016/j.sapharm.2006.02.008. [DOI] [PubMed] [Google Scholar]
- 16.Nester T, Hale L. Effectiveness of a pharmacist-acquired medication history in promoting patient safety. Am J Health Syst Pharm. 2002;59(22):2221–2225. doi: 10.1093/ajhp/59.22.2221. [DOI] [PubMed] [Google Scholar]
- 17.Scott D, Friesner D, Miller D. Pharmacy students’ perceptions of their preparedness to provide pharmaceutical care. Am J Pharm Educ. 2010;74(1):Article 8. doi: 10.5688/aj740108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Blake K, Madhavan S, Scott V, et al. Medication therapy management services in West Virginia: pharmacists’ perceptions of educational and training needs. Res Social Admin Pharm. 2009;5(2):182–188. doi: 10.1016/j.sapharm.2008.06.003. Epub 2009 Jan 21. [DOI] [PubMed] [Google Scholar]
- 19.Macintosh C, Weiser C, Wassimi A, et al. Attitudes toward and factors affecting implementation of medication therapy management services by community pharmacists. J Am Pharm Assoc (2003) 2009;49(1):26–30. doi: 10.1331/JAPhA.2009.07122. [DOI] [PubMed] [Google Scholar]
- 20.Urmie J, Farris K, Herbert K. Pharmacy students’ knowledge of the Medicare drug benefit and intention to provide Medicare medication therapy management services. Am J Pharm Educ. 2007;71(3):Article 41. doi: 10.5688/aj710341. [DOI] [PMC free article] [PubMed] [Google Scholar]