Abstract
Objective. To design, implement, and evaluate an interprofessional learning workshop on pediatric prescribing.
Design. An interactive workshop on pediatric prescribing was designed and delivered by pediatricians and pharmacists to fourth-year medical and pharmacy students on 3 university campus settings. Students were assigned to either interprofessional workshop groups (pharmacy and medical students) or non-interprofessional workshop groups (medical students only).
Assessment. Two hundred thirty students completed the workshops and 92% returned both the pre- and post-workshop questionnaires. Attitudes toward interprofessional learning significantly improved among students in the interprofessional workshop groups (p< 0.001) and confidence in prescribing for pediatric patients significantly improved among all students (p< 0.001).
Conclusions. The workshop improved medical and pharmacy students’ knowledge and confidence in pediatric prescribing and significantly improved their attitudes toward working and learning with other professionals.
Keywords: interprofessional learning, prescribing, pediatrics
INTRODUCTION
Because of their lower body weight and other physiological characteristics, children are more vulnerable than adults to prescribing errors and to mistakes made during dosage calculation of neonatal and pediatric medicines. 1-4 Many reports emphasize the complexity of prescribing for children and encourage specific training for and assessment of students in medical school.5,6 Maxwell and Walley created a syllabus that was appropriate to support this aim, while noting that prescribing is a generic skill that is also performed by non-physician prescribers, including pharmacists, nurses, and optometrists.7 The ability to prescribe safely is a culmination of the practitioner having background knowledge, diagnostic and clinical decision-making skills, and an understanding of the potential positive and negative effects of a particular medication on an individual. These are skills learned over time, and built on experiences attained throughout undergraduate and postgraduate training.
Because medical, pharmacy, and nursing professionals are increasingly involved in prescribing, monitoring, checking, and dispensing medications, health professionals and health professions educators have recognized the benefits of multidisciplinary cooperation and interprofessional learning in teaching these areas. The Kennedy Report recommends that “greater priority be given to the development of teamwork and shared learning across professional boundaries.”8 Health professions programs also are facilitating interprofessional learning through workshops.9 Interprofessional education of health professions students leads to increased knowledge as well as more positive attitudes toward working together in the future.”
Parsell and Bligh identified 5 key conditions important for effective interprofessional learning to occur: the subject must be relevant to all involved; the subject must be taught at a level that is understandable and interesting to all; small groups and interactive forums should be used; participants must be secure in their respective professional identities; and participants must feel themselves to be on an equal footing.10
The Centre for the Advancement of Interprofessional Education defines interprofessional education as that which occurs when 2 or more professions learn with, from, and about each other, and state that the benefits of successful interprofessional education include: improved collaboration, which fosters mutual respect; improved quality of care; and enhanced respect for the integrity and contribution of each profession.11
The University of Wisconsin designed a pharmacist-practitioner--led workshop to increase medical students’ knowledge of and skills in prescription writing; to increase their use of a formulary; and to reduce prescribing errors.12 This workshop for medical students seemed a useful basis for the development of an interprofessional workshop for undergraduate medical and pharmacy students on prescribing in pediatrics.
As prescribing is a skill that many healthcare professionals are now required to have, there was a need to add training in prescribing skills to both undergraduate curricula, particularly skills and knowledge specific to safer pediatric prescribing. Thus, the objective of this study was to design and implement a pediatric prescribing workshop for undergraduate medical and pharmacy students that introduced the principles of prescribing for children, and to evaluate whether teaching the workshop in an interprofessional environment affected participants’ knowledge, skills, and attitudes.
DESIGN
Participants in the study were all fourth-year medical students from the University of Bristol and all final-year pharmacy students from the University of Bath. The medical students had previously been randomly assigned to 1 of 8 University of Bristol medical academies based on secondary-care hospital sites. Three of the academies had access to both medical and pharmacy students but the other 5 had access only to medical students. This provided an opportunity for the non-interprofessional learning sites to act as a control for the interprofessional learning workshops. Prior to this workshop, development of the specific skills of pediatric prescribing had not been taught at the medical undergraduate level.
We wanted to embed the learning workshop into each profession’s curricula in such a way as to contribute towards the medical students’ Child Health course and the pharmacy students’ Clinical Pediatric Skills unit. The learning objectives for the workshop were that by the end of the workshop the student should be able to:
• Describe and understand the ways in which children are different from adults and the implications of this for safe prescribing;
• Describe and understand the professional skills involved in safe prescribing in pediatrics, including consent, compliance, route of administration, and licensing;
• Use the accepted pediatric prescribing formulary; and
• Complete an inpatient prescription chart and an outpatient prescription form accurately and legibly.
The workshop content was developed by a team of pediatric pharmacists and medical clinicians working in primary- and secondary-care settings and in academia. The original workshop was pilot tested with third-year medical and pharmacy students, and comments from participants and facilitators’ were used to revise the original workshop prior to implementation.
The workshop was evaluated during the 2004-2005 academic year. The local University Ethics Committee advised that no formal approval was needed for conducting the study. At the start of each workshop, the students were informed that it was a pilot program and that pre- and post-workshop questionnaires would be used to assess their attitudes towards interprofessional learning. Students were assured that their responses would remain anonymous and confidential.
A pediatrician and pharmacist with experience in pediatrics jointly facilitated each workshop, using standardized teaching materials. The facilitators used an unstructured teaching style that was not lecture-based to enable students to learn with, from, and about each other and avoided lecturing to encourage a learner focused approach to learning.11 The students worked in small groups of 2 to 4 (with both medical and pharmacy students in each group in the interprofessional workshops) and discussed and debated possible clinical options prior to presenting their findings to the wider group. These discussions were moderated by facilitators and students were given model answers after each discussion. Providing this formative feedback throughout the workshop enabled students to check their own learning and where appropriate to identify areas where further study was required to achieve good standards of prescribing practice.
Student groups were provided with a calculator and a copy of the then Royal College of Paediatrics and Child Health Medicines for Children Formulary (a specialist prescribing reference used prior to publication of the British National Formulary for Children).13 In preparation for group discussions in class, students were encouraged to complete assigned readings on the ways in which children differ from adults and on the theory of prescribing for children.14 The assigned readings also included the use of licensed, unlicensed, and off-license medicines in children, as well as the pharmacokinetic and pharmacodynamic changes associated with the different age classifications for children. In the United Kingdom, a licensed medicine is a medicine prescribed according to its registered licensed indications. An unlicensed medicine is a medication that is not licensed in the United Kingdom, but has been prescribed for an individual and has to be imported. An off-license medicine is one that is licensed in the United Kingdom but has been prescribed for something other than for its registered licensed indications. Most commonly occurring in pediatric and intensive care settings, licensed medicines for adults are used “off-license” in terms of dosage, indication, and age-related factors as there are no alternative licensed pediatric medicines available. Off-license and unlicensed prescribing also infers full responsibility of patient outcome on the prescriber and not the pharmacy or pharmacist.
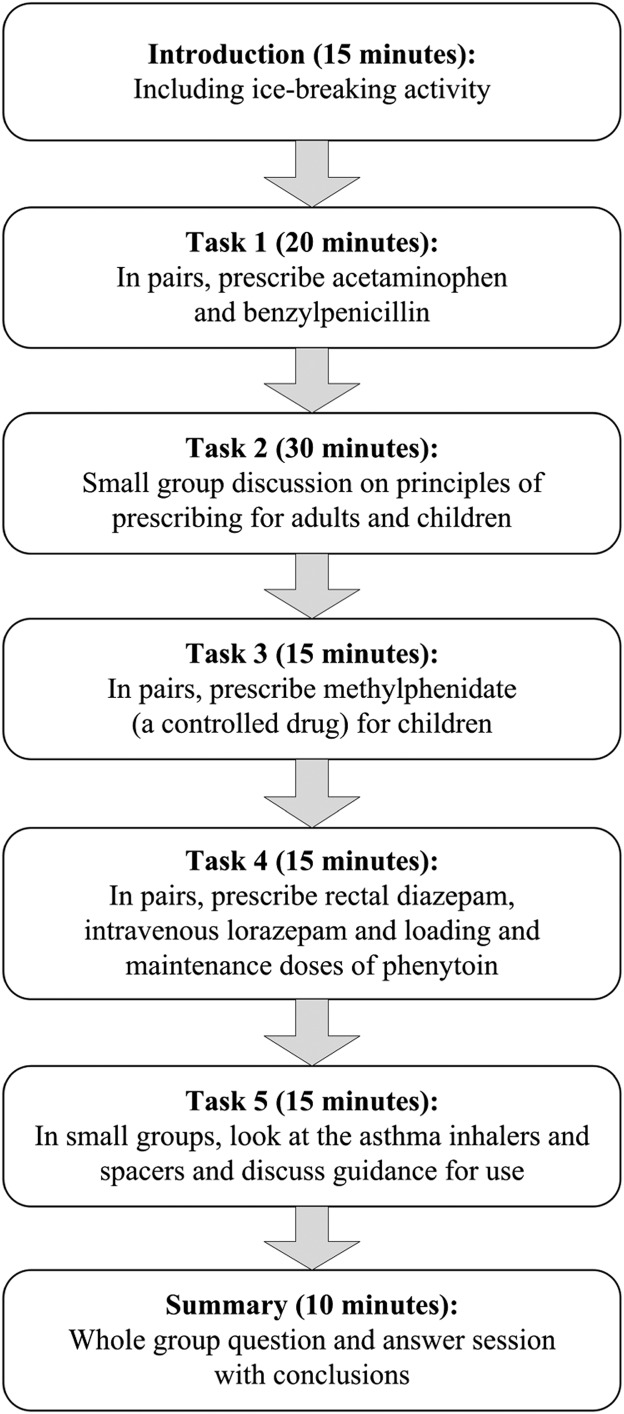
The students followed a worksheet that contained several common clinical prescribing scenarios from primary and secondary care settings. After group discussions, student practiced completing standard hospital prescription charts and outpatient prescription forms. For example, one scenario involved a child with a chest infection and required the student to select the appropriate antibiotic and dose, while another scenario involved a child with attention deficit disorder and required the student to prescribe a controlled substance, methylphenidate. The workshop program is illustrated in Figure 1.
Figure 1.
Pediatric Prescribing Workshop Overview
EVALUATION AND ASSESSMENT
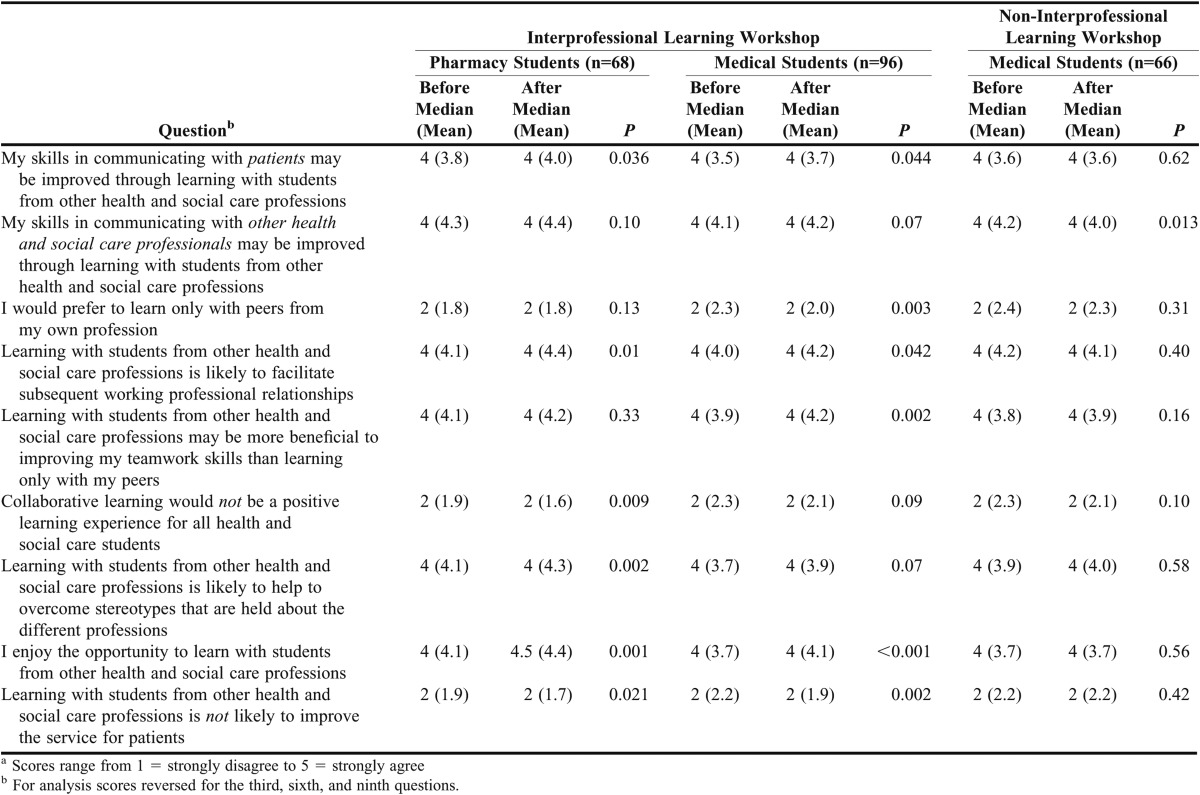
Previous medical undergraduate interprofessional learning sessions had been evaluated with a validated attitude to interprofessional learning questionnaire. 15 This consisted of 9 questions (Table 1) with response options on a 5-point modified Likert scale on which 1 = strongly disagree and 5 = strongly agree. We added a second section that contained 5 additional items to assess confidence in prescribing skills for adults and children (Table 2). Finally, students were asked to list 2 perceived strengths and weaknesses of interprofessional learning and to add further comments if they wished.
Table 1.
Changes in Attitude Towards Interprofessional Learning Before and After Attending a Prescribing Workshopa
Table 2.
Changes in Perceived Confidence in Prescribing Before and After Participation in a Prescribing Workshopa
All students were asked to complete a questionnaire immediately before and after the workshop. For the analysis, the scores were reversed for questions 3, 6, 9, and 13. Thus, high scores on questions 1-9 indicated a more positive attitude towards interprofessional learning, and high scores on questions 10-14 indicated a greater confidence in prescribing. Changes in response to each question from pre- to post-training were assessed using non-parametric, Wilcoxon matched-pairs signed-ranks tests (with adjustment for tied ranks). Medians and ranges were used for data summary but, because of the tied observations, means were added to better indicate the direction of change.
Medical students’ knowledge of prescribing was assessed using extended matching questions, which formed part of their standard end-of-year written examination. The range of grades for a test using extended matching questions was 0 to 5. Each extended matching question had a lead-in phrase. For example: “for each of the following patients with chest pain, please select the most appropriate treatment from the 26 options above.” There were 5 questions, or stems, for which the candidate had to select an answer from the options list. Each option could be used once, more than once, or not at all. The questions required the student to use the Medicines for Children Formulary to select the correct medication and calculate the appropriate dose.
The objective structured clinical examination (OSCE) contained a station that assessed students’ prescription-writing skills. Using the Medicines for Children Formulary provided, the student had to select an appropriate medication for a given clinical situation (for example an antibiotic for a urinary tract infection in a child with a penicillin allergy) and enter it on a standard hospital prescription chart.
The EMQ and OSCE scores of the interprofessional learning and non-professional learning medical students were compared using Mann-Whitney U tests. A student’s scores were eliminated from the analysis if either the pre- or post-workshop questionnaire was not completed or if the student’s name was missing from either of the questionnaires.
The pharmacy students’ knowledge of pediatric prescribing was not assessed by the same EMQ and OSCE method because of the inability to change pharmacy assessment procedures within the timeframe of the study. Prescribing knowledge for pharmacy students was assessed during final dispensing examinations.
Two hundred thirty students participated in 19 workshops. Nine sessions were interprofessional learning and attended by 96 medical students and 68 pharmacy students, with 10 or 11 medical and 7 or 8 pharmacy students at each workshop. The other 10 workshops were non-interprofessional learning (only medical students attended). The 2.4 ratio of medical students to pharmacy students meant that there were usually 1 pharmacy student and 2 or 3 medical students in each small group.
Of the 230 students, 211 completed the pre- and post-workshop questionnaires (92% response rate); 11 (5%) completed 1 of the questionnaires, and 8 did not submit either questionnaire. However, not all students completed every question on the questionnaires. The changes from pre- to post-workshop for individual attitude questions (questions 1-9) and the total overall change in attitude to interprofessional learning are shown in Table 1.
After the workshop, the participants were more likely to think that interprofessional learning would enhance communication skills, especially with regard to patients (p=0.044 and p=0.036, respectively, for medical and pharmacy students). After interprofessional learning, medical students were less likely to prefer to work only with other medical students (p=0.003) and both medical and pharmacy students reported increased enjoyment with working with other professions (p=0.001). Medical students were more likely to think interprofessional learning improved team-working skills (p=0.002).
Overall, attitudes toward interprofessional learning significantly improved among medical and pharmacy students in the interprofessional learning group (p<0.001 for both; Table 2). There was no significant change in the scores of medical students who were in the non-interprofessional learning groups (p=0.191).
One of the learning outcomes was to determine whether there was a change in students’ confidence in skills such as writing prescriptions. The prescribing workshops significantly increased overall confidence in prescribing among students in both the interprofessional and non-interprofessional learning groups (p<0.001; Table 2). The changes in scores from pre- to post-workshop for individual skill-related questions (questions 10-14) and overall change in scores are shown in Table 2.
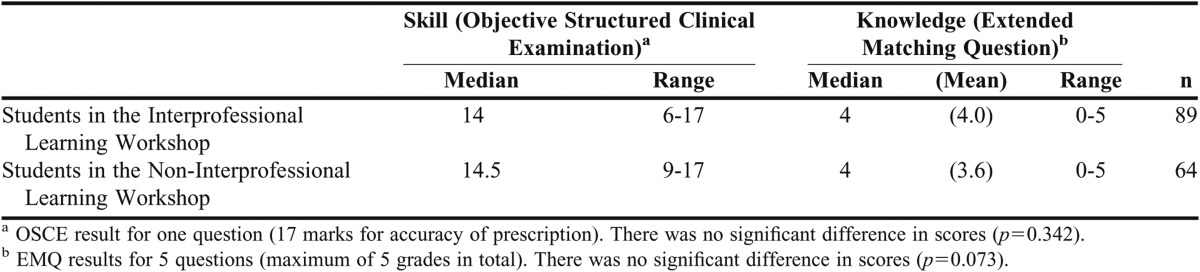
Medical students’ knowledge about prescribing for children was tested on the end-of-year examinations. No differences in scores on prescribing questions were apparent between students who attended interprofessional and non-interprofessional learning workshops (Table 3).
Table 3.
Assessment of Medical Students’ Knowledge After Participation in a Pediatric Prescribing Workshop
Written comments on the post-workshop feedback forms highlighted students’ perceived strengths and weaknesses of interprofessional learning. Some of the strengths of interprofessional learning identified by a medical student included its ability to break down stereotypes and facilitate future relationships, while a pharmacy student described feeling pride in being able to share knowledge about prescribing and the issues surrounding drug selection and dosage.
Weaknesses identified by the students centred on the lack of “a horizontal and vertical approach” to interprofessional learning within each profession’s curricula. Students stated they would prefer that interprofessional learning be included in each year of the curriculum (horizontal), with each year’s content increasing in difficulty (vertical) and covering a range of clinical areas. One medical student commented that interprofessional learning should be included much earlier in the curriculum, when learning basic sciences and clinical skills.
DISCUSSION
The students who participated in the interprofessional learning groups not only enjoyed the experience, but also underwent a significant, positive attitudinal change as a result. Benefits included: meeting a group of health professions students with whom they had limited prior interaction; discovering similarities in training and roles; and finding ways in which their professions could work together more effectively in practice.
Students felt that interprofessional learning should be a core part of their undergraduate curriculum and happen regularly enough that professional relationships could be established. Interestingly, 1 medical student listed learning from pharmacy students as a weakness of the workshop, when actually it was the fundamental aim of the workshop that both professionals learn with, from, and about each other.
Much of the literature on interprofessional learning is of poor quality, typically consisting of a description of an educational event or program, with outcomes often limited to the results of a survey of learner satisfaction or participants’ knowledge, but no survey of a comparison group.16 Our workshop was compulsory, had a control group, and assessed participants’ perceived knowledge, skills, and attitudes. A study by Stewart and colleagues of the impact of an interprofessional workshop demonstrated findings similar to ours, with increased knowledge among medical students about the causes of medication errors in pediatric cases and improved interprofessional attitudes towards working with nursing professionals.17 Conroy and Carroll suggest that education is the key to safer prescribing in pediatrics and that educators and researchers should remember the following points when designing interprofessional learning curriculum: that the timing of the teaching in relation to examinations is key, that content should be relevant to practice, and that involving pharmacists in interprofessional learning may result in higher student satisfactions scores.18
Our study has several limitations. Equal numbers of medical and pharmacy students should have been randomly allocated to interprofessional learning and non-interprofessional learning groups; as it was, medical students outnumbered pharmacy students by 2.4 to 1. Also, for logistical reasons, the interprofessional learning workshops were restricted to 3 academy sites. Although more interprofessional sites would have strengthened the data on the workshop’s impact on students’ attitudes about interprofessional learning, having the non-interprofessional sites validated the workshop’s use with medical students. We would have liked to assess the attitudes, knowledge, and skills of pharmacy students in annual examinations in the same way as medical students; however, differences in the assessment methods used at the 2 academic sites precluded this. The questionnaire used a modified Likert scale for responses and, for statistical analysis, scores were added together.15 It was not possible to measure the consistency of teaching styles across sites and differences in facilitator attitudes, knowledge, and teaching styles may have affected outcomes. Finally, there is no way of knowing whether the attitudinal change that we identified will persist or be clinically relevant. Health professionals exposed to a single interprofessional learning event prospectively followed-up over a 2-year period exhibited mixed results to the longevity of the learning and attitudinal changes.19 Other longitudinal interprofessional learning studies demonstrate difficulties in follow-up and retention of study participants over time.20 Interestingly, a higher-education institution with an embedded culture of interprofessional education has shown that positive attitudes towards interprofessional learning decreased over time.21 However, students graduating from an institution with an interprofessional learning curriculum felt more positive about their professional relationships when they entered practice than those who graduated without exposure to interprofessional learning.15
There is a need for longitudinal studies of health professions graduates’ attitudinal changes and the knowledge and skills they gained in interprofessional learning environments to determine whether these persist after entering practice. However, relocation of undergraduate participants after graduation makes such studies a challenge.
The interprofessional learning workshops could be adapted for use by recent health professions graduates (eg, physicians, pharmacists, and nurses) just entering the workforce and also be used to enhance learning and understanding of other health professionals who are non-prescribers working in the area of pediatrics. Kidd et al suggest that ongoing educational interventions on prescribing for health professionals throughout training and registration are a necessary component of reducing errors, especially in pediatric prescribing. We recommend that not only should such educational events be required but that individual prescribing practices be monitored over time to ensure competence continues to improve.22
SUMMARY
An interactive interprofessional pediatric prescribing workshop increased medical and pharmacy students’ perceived knowledge, skills, and confidence in prescribing for children, which is essential for improving patient safety. We demonstrated that interprofessional learning had a significant positive impact on participants’ attitudes toward working and learning with other health professions students and on working with other healthcare professionals in the future.
REFERENCES
- 1.Kohn L, Corrigan J, Donaldson M, editors. To Err is Human: Building a Safer Health System. Washington, DC: National Academy Press; 2000. [PubMed] [Google Scholar]
- 2.Greiner AC, Knebel, editors. Health Professions Education: A Bridge to Quality. Washington, DC: National Academy Press; 2003. [PubMed] [Google Scholar]
- 3.American Council for Pharmacy Education. Accreditation standards and guidelines for the professional program in pharmacy leading to the Doctor of Pharmacy degree. Chicago: Accreditation Council for Pharmacy Education; 2007. [Google Scholar]
- 4.Association of American Medical Colleges. Report V: Contemporary Issues in Medicine: Quality of Care. http://laico.org/v2020resource/files/quality_of_care.pdf. Accessed June 6, 2012.
- 5.Maddox PJ, Wakefield M, Bull J. Patient safety and the need for professional and educational change. Nurs Outlook. 2001;49(1):8–13. doi: 10.1067/mno.2001.113642. [DOI] [PubMed] [Google Scholar]
- 6.American Association of Colleges of Nurses. The essentials of baccalaureate education for professional nursing practice. doi: 10.1016/j.profnurs.2011.04.009. Washington, DC: 2008. http://www.aacn.nche.edu/education/pdf/BaccEssentials08.pdf. Accessed June 6, 2012. [DOI] [PubMed]
- 7.Cohen MR, editor. Medication Errors. 2nd ed. The American Pharmacists Association; Washington, DC: 2007. [Google Scholar]
- 8.Johnson MS, Latif DA, Gordon B. Medication error instruction in schools of pharmacy curricula: a descriptive study. Am J Pharm Educ. 2002;66(4):364–371. [Google Scholar]
- 9.Holdford DA, Warholak TL, Malone DC, Murphy JE, Strum-West D, Bentley JP. A baseline evaluation of the integration of the “Science of Safety” into the curriculum of the doctor of pharmacy degree in US colleges and schools of pharmacy. doi: 10.5688/ajpe757141. http://www.aacp.org/resources/research/Documents/A%20Baseline%20Evaluation%20SOS%20Final.pdf. Accessed June 6, 2012. [DOI] [PMC free article] [PubMed]
- 10.West-Strum D, Basak R, Bentley JP, et al. The science of safety curriculum in US colleges and schools of pharmacy. Am J Pharm Educ. 2011;75(7):Article 141. doi: 10.5688/ajpe757141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Karl KA, O’Leary-Kelly AM, Martocchio JJ. The impact of feedback and self-efficacy on performance in training. J Org Behav. 1993;14(4):379–394. [Google Scholar]
- 12.Sukkari SR, Sasich LD, Tuttle DA, Abu-Baker AM, Howell H. Development and evaluation of a required patient safety course. Am J Pharm Educ. 2008;72(3):Article 65. doi: 10.5688/aj720365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Jackson TL. Application of quality assurance principles: teaching medication error reduction skills in a “real world” environment. Am J Pharm Educ. 2004;68(1):Article 17. [Google Scholar]
- 14.The National Prescribing Centre. Prescribing for children. MeReC Bulletin. 2000;11(2):5–8. [Google Scholar]
- 15.Pollard K, Miers ME, Gilchrist M. Second year scepticism: pre-qualifying health and social care students midpoint self-assessment, attitudes and perceptions concerning interprofessional learning and working. J Interprofessional Care. 2005;19(3):251–268. doi: 10.1080/13561820400024225. [DOI] [PubMed] [Google Scholar]
- 16.Mattick K, Bligh J. Interprofessional learning involving medical students or doctors. Med Educ. 2003;37(11):1008–1011. doi: 10.1046/j.1365-2923.2003.01681.x. [DOI] [PubMed] [Google Scholar]
- 17.Stewart M, Purdy J, Kennedy N, Burns A. An interprofessional approach to improving paediatric medication safety. BMC Medical Education. 2010;10:19. doi: 10.1186/1472-6920-10-19. http://www.biomedcentralcom/1472-62920/10/19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Conroy S, Carroll WD. Prescribing in paediatrics. Arch Dis Child Educ Pract Ed. 2008;95:55–58. doi: 10.1136/adc.2008.141754. [DOI] [PubMed] [Google Scholar]
- 19.Hylin U, Nyholm H, Mattiasson AC, Ponzer S. Interprofessional training in clinical practice on a training ward for healthcare students: a two-year follow-up. J Interprofessional Care. 2007;21(3):277–288. doi: 10.1080/13561820601095800. [DOI] [PubMed] [Google Scholar]
- 20.Freeth D. Effective Interprofessional Education: Development, Delivery and Evaluation. Oxford: Blackwell; 2005. Centre for the Advancement of Interprofessional Education in Primary Health and Community Care. [Google Scholar]
- 21.Pollard K, Miers ME, Gilchrist M, Sayers A. Health Soc Care Comm. 2006;14(6):541–542. doi: 10.1111/j.1365-2524.2006.00642.x. [DOI] [PubMed] [Google Scholar]
- 22.Kidd L, Shand E, Beavis R, Taylor Z, Dunstan F, Tuthill D. Prescribing competence of junior doctors: does it add up? Arch Dis Child. 2010;95:219–221. doi: 10.1136/adc.2008.156042. [DOI] [PubMed] [Google Scholar]