According to the Bylaws of AACP, the Professional Affairs Committee is to study:
issues associated with the professional practice as they relate to pharmaceutical education, and to establish and improve working relationships with all other organizations in the field of health affairs. The Committee is also encouraged to address related agenda items relevant to its Bylaws charge and to identify issues for consideration by subsequent committees, task forces, commission, or other groups.
COMMITTEE CHARGE
President Brian Crabtree charged the 2011-2012 American Association of Colleges of Pharmacy (AACP) Standing Committees with issues related to excellence and relevance in pharmacy education.1 Specifically, the 2011-2012 Professional Affairs Committee is charged to:
(1) Embark on an analysis of the concept of “master preceptor.” This should include a discussion of the following elements of a professional development program to cultivate a pharmacy preceptor who excels in experiential teaching: a) content of the program, b) mechanism(s) for program delivery and c) program outcomes and assessment.
(2) Recommend a recognition system for teaching excellence by preceptors. The recognition system should include elements that would be beneficial and motivational for the continued professional development of the preceptor as well as sustaining and maintaining excellence of experiential education provided by colleges and schools of pharmacy.
Members of the Professional Affairs Committee (PAC) included faculty from multiple disciplines from various schools/colleges of pharmacy as well as association representatives from three national pharmacy organizations: The American Pharmacists Association (APhA), the American Society of Health-System Pharmacists (ASHP), and the American College of Clinical Pharmacy (ACCP). Prior to an in-person meeting of the committee, pertinent background information and resource materials were distributed and the sharing of initial methods to address the committee charges was encouraged. Committee members met for a day and a half in Crystal City, Virginia on October 6-7, 2011 to discuss the various facets related to this issue as well as to develop a process for addressing the charge. Following the process development and delegation of assignments related to the committee charges, the Committee communicated via a series of conference calls and electronic communications as well through personal exchanges via telephone and email. The result is the following report, which discusses elements necessary for a development program to cultivate pharmacy preceptors to be the best teachers possible and a recognition system for those preceptors who reach and sustain teaching excellence.
BACKGROUND
Experiential education is a key component of the pharmacy curriculum, comprising approximately 30% of the professional curriculum. The experiential component of pharmacy education currently relies heavily on volunteer and adjunct faculty to provide practical experience in health care settings. It has been estimated that about 82 percent of schools/colleges use faculty who are jointly funded with practice sites and up to 60 percent of the total APPE rotations nationally are provided by adjunct or volunteer faculty.2,3 The need for qualified preceptors is increasing due to new schools/colleges of pharmacy and enrollment growth in existing programs,4 the increased experiential load in the pharmacy school curricula,5 and the necessity of having preceptors available in a variety of pharmacy practice settings.6 This report will focus on volunteer preceptors, defined as individuals who are not full-time employees of a school or college of pharmacy who are responsible for experiential education of student pharmacists.
Several entities have established requirements for pharmacy preceptors. According to the 2011 National Association of Boards of Pharmacy (NABP) Survey of Pharmacy Law, 23 (44%) of the 52 boards of pharmacy require pharmacy preceptors to register or communicate with the board in some matter regarding their role as a pharmacy preceptor.7 In addition, some boards have criteria that specify a minimum number of years of licensure prior to becoming a preceptor and specific training/continuing education or professional development requirements that must be met to remain a preceptor.
Schools/colleges of pharmacy are provided direction regarding preceptor qualifications and preceptor development. Elements of the Accreditation Council for Pharmacy Education (ACPE) Standards and Guidelines8 that pertain to experiential education include Standard 14 (Curricular Core-Pharmacy Practice Experiences), Standard 15 (Assessment and Evaluation of Student Learning and Curricular Effectiveness), Standard 24 (Faculty and Staff—Quantitative Factors), Standard 25 (Faculty and Staff—Qualitative Factors), Standard 26 (Faculty and Staff Continuing Professional Development and Performance Review), and Appendix C (Additional Guidance on Pharmacy Practice Experiences). All faculty should be evaluated as to their teaching abilities, communication skills, and effectiveness related to pharmacy education. These areas can be documented and evaluated utilizing review committees, experiential site visits by trained individuals, and student pharmacist feedback. ACPE Standard 26 states that schools/colleges of pharmacy must have an effective continuing professional development (CPD) program for full-time, part-time, and voluntary faculty. Guideline 26.1 states that schools/colleges of pharmacy must have or provide support for programs and activities for faculty and preceptor CPD commensurate with their responsibilities. It is therefore imperative that schools/colleges of pharmacy develop and maintain preceptor development programs.
While accreditation and other entities have established criteria for preceptor training and development, the perceptions and needs of the preceptor should also be taken into consideration. AACP’s institutional research department gathers, analyzes and summarizes data related to schools/colleges of pharmacy accredited by ACPE.9 The institutional research department has surveyed preceptors, via the administration by schools/colleges and the AACP centralized survey system, annually since 2009.10 While the preceptor response rates have averaged 32% over the past 3 years, the strongly agree and agree responses to questions regarding resources and support received by preceptors have increased during this time.10 Namely, the strongly agree and agree responses for 2009, 2010, and 2011 for ongoing contact with the office of experiential education were 78.7%, 80.5%, and 84.1% respectively, support received from the office of experiential education was 80.5%, 81.9%, and 85.6% respectively, and the college/school having an effective CPD program that is consistent with preceptor responsibilities was 76.4%, 78.4%, and 81.4% respectively.10 Though the differences were modest and the response rate low, the results may indicate some improvement over time.
Accredited pharmacy residency programs have the responsibility for assuring required preceptor qualifications and professional development. Key areas of preceptor development named in the American Society of Health-System Pharmacists (ASHP) accreditation standards for postgraduate year 1 (PGY1)11 pharmacy residences and postgraduate year 2 (PGY2)12 pharmacy residencies include the teaching and professional skills of the residency program director (RPD) and preceptors. Pharmacy residency accreditation standards require that the RPD and preceptors should have a record of contribution and commitment to the profession of pharmacy (Requirement 5.9); they must demonstrate a desire and aptitude for teaching that requires mastery of the four preceptor roles (instructing, modeling, coaching, and facilitation) when used in teaching clinical problem solving; and they must also demonstrate the ability to provide criteria-based feedback and evaluation of the residents performance (requirement 5.10).11,12 In addition, the RPD should assess and provide preceptors opportunities to enhance the quality of their precepting skills (Requirement 4.3).11,12 According to data reported by the ASHP Commission on Credentialing (COC) in August 2011, 72% of PGY1 and 64% of PGY2 pharmacy residency programs surveyed were cited for not having adequate preceptor development.13 ASHP has multiple sessions for the development of residency program directors and preceptors at the ASHP midyear clinical meeting and other designated programs, such as the biennial national ASHP residency preceptors conference.
A study was conducted to determine the training needs and interests of volunteer pharmacy preceptors of six regional APPE programs throughout California.14 Approximately 74% of the study respondents indicated an interest in obtaining additional training. The preferred areas for preceptor development included engaging and motivating students (69%), update on teaching/precepting strategies (60%), questioning students effectively (59%), communicating effectively with students (49%), working effectively with different adult learning styles (49%), assessing student performance (47%), and effectively integrating students into day to day workplace activities (42%). Respondents who had received formal preceptor training were significantly more confident in their abilities to clarify expectations, evaluate a student’s knowledge, and foster skills related to critical thinking and problem solving. This information provides potential areas for future preceptor development programs.
A recent study suggests that being an active pharmacist preceptor is associated with increased job satisfaction among pharmacists, but is not necessarily associated with increased career satisfaction.15 The job satisfaction associated with precepting student pharmacists was independent of the type of pharmacy practice setting. This information may assist schools/colleges of pharmacy as well as pharmacy practice sites in the recruitment, engagement, and retention of pharmacy preceptors.
While the benefits of precepting to preceptors5,16,17 and to practice sites5,16-19 have been well documented, the issue of quality precepting continues to be of paramount importance and discussion in pharmacy and other areas of health care training. Experiential office faculty and staff members are striving to meet quality assurance standards as well as preceptor development needs.6 The responsibility for ensuring quality pharmacy practice experiences for students, defined as a well-planned, outcomes-focused training experience with adequate supervision and assessment by a qualified preceptor within a learning-rich practice environment, resides with schools/colleges of pharmacy.20 Schools/colleges of pharmacy should have requirements established for preceptors and practice sites where precepting occurs that lead to quality pharmacy practice experiences.
Quality in experiential education is pursuant to the preceptor (practitioner-educator), the learning experiences (collaboratively designed by college, preceptor, and student pharmacist), and the practice environment.3 A common thread within this triad is the preceptor. While the focus of many schools/colleges of pharmacy experiential departments is on identifying and sustaining an adequate number of quality preceptors and practice sites, it has been suggested that the goal of every experiential program should be to identify, train, develop and maintain quality preceptors.3 The 2004 AACP PAC report provided the following preceptor characteristics that were thought to be conductive to effective learning:
• Is approachable and establishes a good learning environment
• Is available to the student for interaction and discussion
• Treats the student with trust and respect in their interactions
• Demonstrates interest and enthusiasm in teaching
• Explains the decision-making process to the student and asks questions that promote learning
• Stimulates the student to learn independently and allows autonomy that is appropriate to the student’s level of experience and competence
• Regularly provides meaningful feedback to the student, both positive and negative, in a timely manner
• Is a good role model for the student and inspires student confidence in preceptor’s technical skills
• Is aware of the clerkship goals and objectives and seeks to meet them
These preceptor characteristics are just as germane in today’s pharmacy academic environment as they were at the time of the 2004 AACP PAC report.
Summary of PAC Proposed Policy Statements, Recommendations, and Suggestions
Policy Statement 1 (as amended and voted upon by the 2012 AACP House of Delegates). AACP affirms that preceptor development is essential to enhance the quality of experiential education and believes that preceptors should possess competencies that include, but are not limited to, leadership/management skills, embodiment of the development of a practice philosophy focused on improving patient outcomes, role modeling as a practitioner, commitment to excellence in scholarly teaching, effective communication skills, and encouragement of self-directed learning.
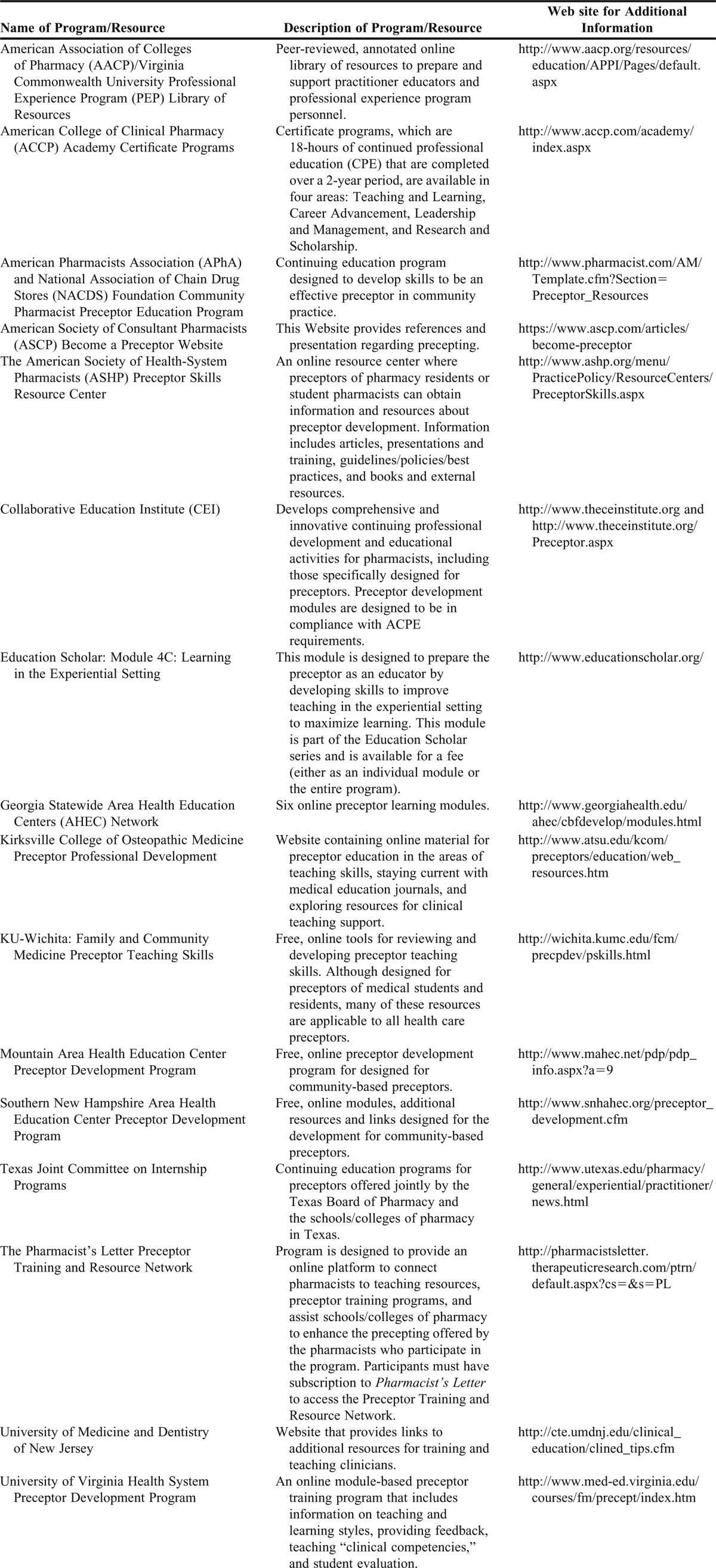
Recommendation 1. AACP will periodically update resources in the Academic-Practice Partnership Initiative (specifically the Professional Experience Program Library of Resources).
Recommendation 2. AACP will explore establishing and reaffirming formal relationships with nationally available pharmacy preceptor training development programs.
Recommendation 3. AACP supports the development of a national master preceptor recognition program.
Recommendation 4. AACP will develop a resource/communication vehicle to enable practitioners designated as a “master preceptor” to communicate best practices/development opportunities with one another and schools/colleges of pharmacy.
Suggestion 1. Schools and colleges of pharmacy should institute and continuously review a preceptor development program and ensure that they include the competencies of leadership/management skills, embodiment of practice philosophy, role modeling as a practitioner, commitment to excellence in scholarly teaching, effective communication skills, and encouragement of self-directed learning.
Suggestion 2. Schools and colleges of pharmacy should make preceptor development programs available via a variety of mechanisms to facilitate various learning styles.
Suggestion 3. Experiential Directors should consider collaborating with other schools/colleges of pharmacy in the local/regional area to develop common approaches to preceptor development, that allow for consistency in communicating performance expectations to preceptors and the potential for sharing resources and training opportunities.
Suggestion 4. AACP encourages schools and colleges of pharmacy to develop and maintain mechanisms for preceptor recognition.
Suggestion 5. Schools and colleges of pharmacy should develop or refine their current recognition system for preceptors based, in part, on objective criteria.
WHAT IS A “MASTER PRECEPTOR”?
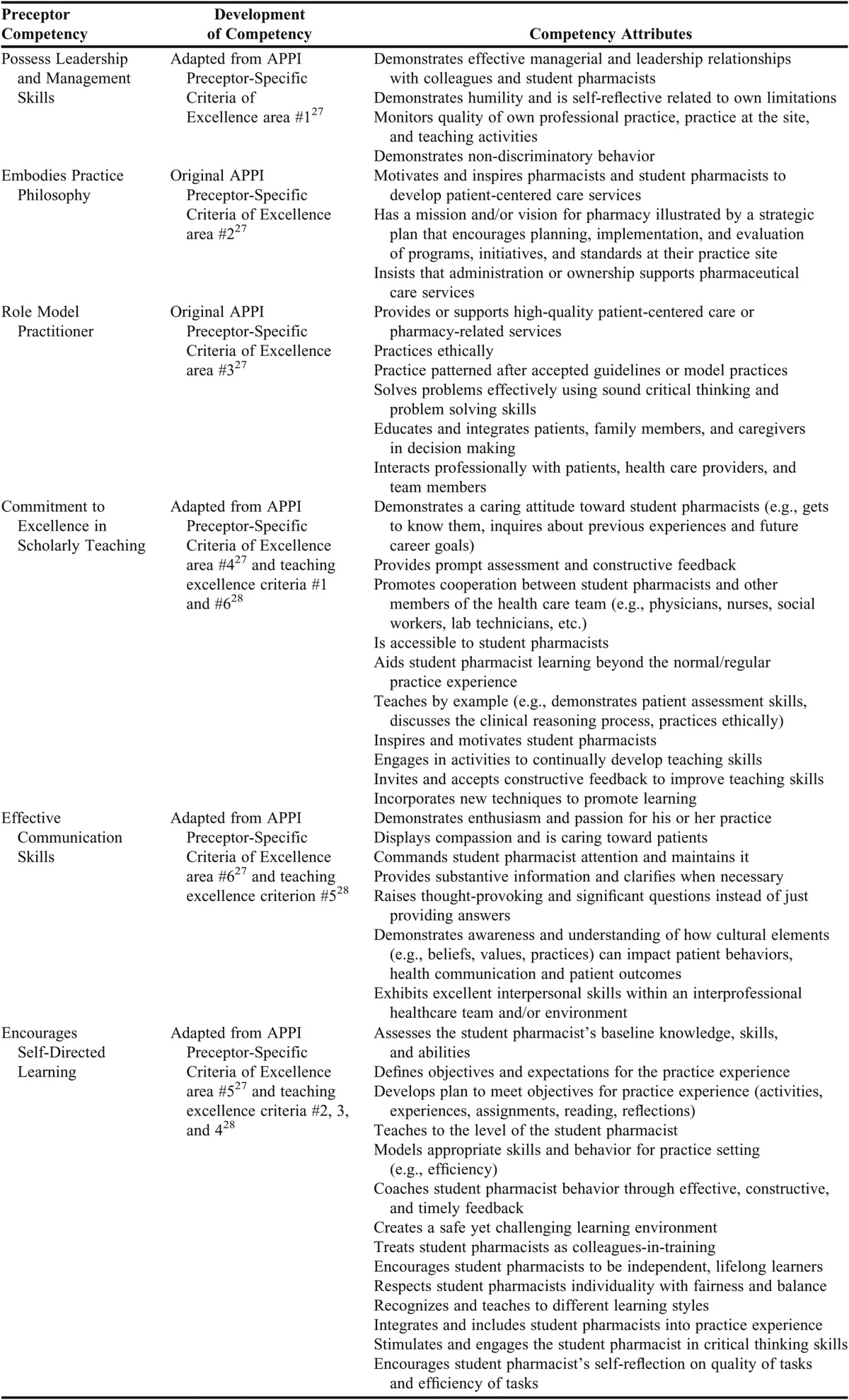
The PAC discussed the concept of a “Master Preceptor” at length and many aspects related to quality and effectiveness in teaching, practice, community service/involvement and professionalism were offered. Ultimately, it was decided that defining the competencies desired in all preceptors should be elucidated. ACPE provides guidance on preceptor training components (Table 1) and the behaviors expected by preceptors who are positive role models (Table 2).
Table 1.
Preceptor Training Program Components (Adapted from Appendix C in Reference 8)
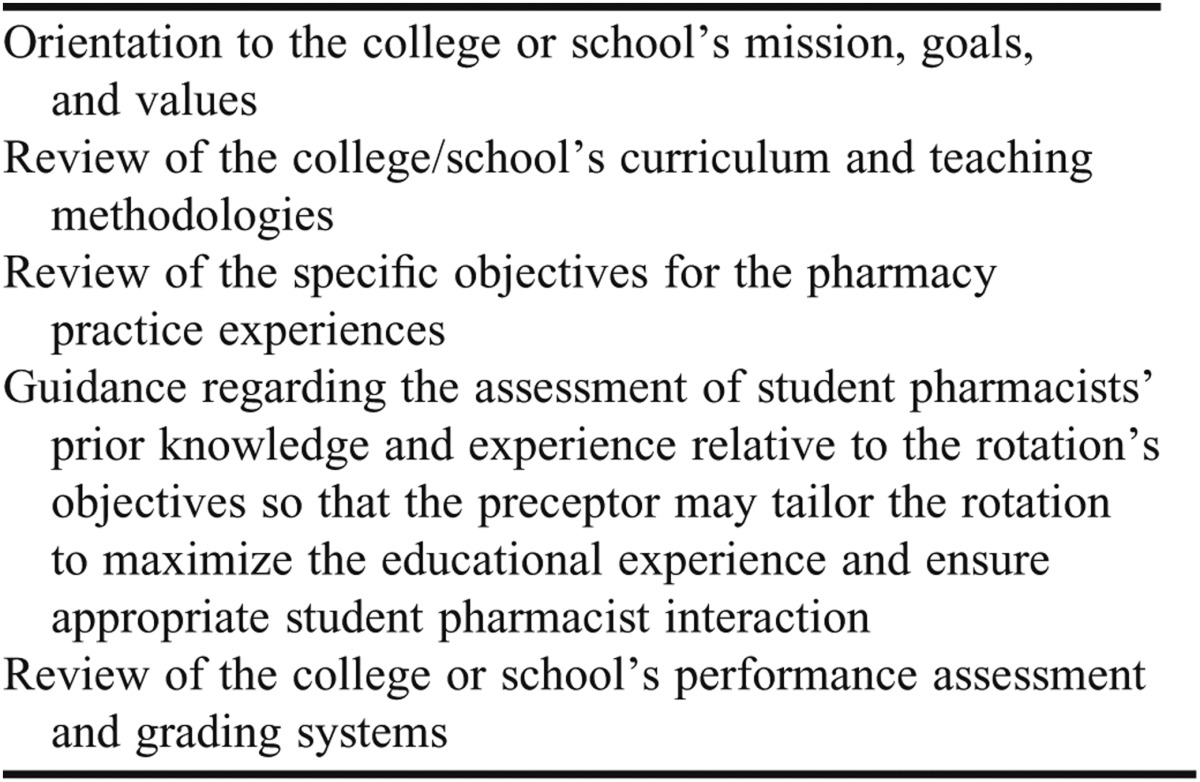
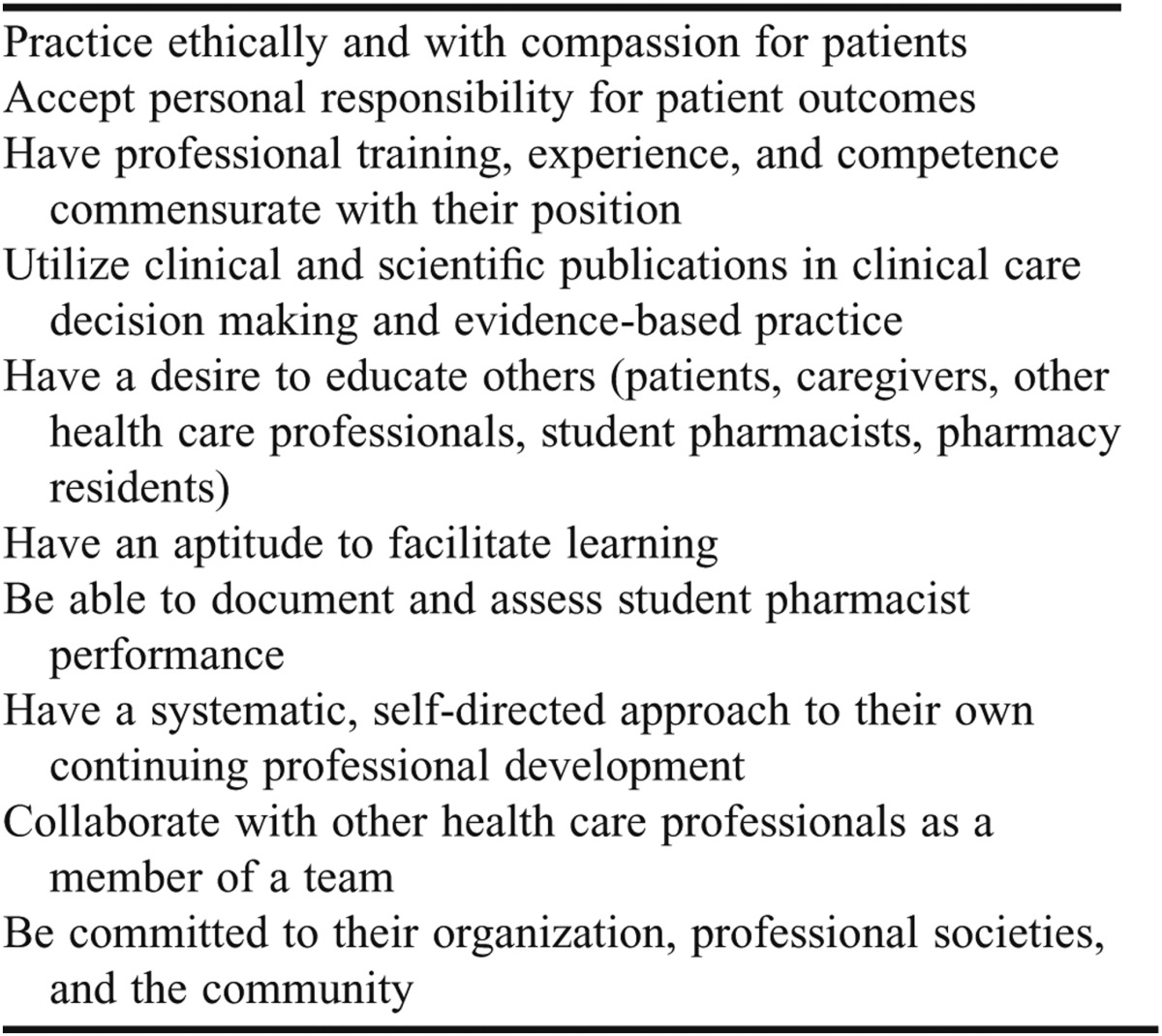
Table 2.
Preceptor Role Model Behaviors, Qualities, and Values (Adapted from Appendix C in Reference 8)
An outgrowth of the AACP Report of the 2004 Professional Affairs Committee was the Academic-Practice Partnership Initiative (APPI).21 APPI was created to identify strategies and develop resources to increase capacity and enhance quality, efficiency, and effectiveness of professional experience programs. It serves to improve pharmacy education and practice by enhancing opportunities for pharmacists to become partners of schools/colleges of pharmacy, enabling member institutions in their efforts to assist practitioners and organizations to advance patient care services, and to assist administrators at schools/colleges of pharmacy as well as in pharmacy organizations to enhance experiential education. The outgrowth of APPI included a 2005 Summit on Advancing Experiential Education in Pharmacy,22 a professional experience program (PEP) library of resources comprised of peer-reviewed resources to prepare and support practitioner educators and professional experience program personnel,23 an advanced practice experience site profiling system (APESPS) which is a toolkit designed to identify, document and profile models of exemplary experiential education practice sites exhibiting the APPI-developed quality criteria,24 and the Crystal Academic-Practice Partnerships for Learning Excellence (APPLE) Award.25 Contained within APESPS are experiential site-specific criteria for excellence and preceptor-specific criteria of excellence, which were developed based upon the 2001 Institute of Medicine report Crossing the Quality Chasm: A New Health System for the 21st Century and the AACP Center for the Advancement of Pharmaceutical Education (CAPE) Educational Outcomes.26 The APPI preceptor-specific criteria of excellence describes six areas necessary for a preceptor to be engaged in effective precepting: possess(es) leadership/management skills, embody(ies) a practice philosophy, demonstrates being a role model practitioner, is an effective, organized, and enthusiastic teacher, encourages self-directed learning with constructive feedback, and has well developed inter-personal communication skills.27
After examining the APPI preceptor-specific criteria of excellence,23 the PAC recognized the need for preceptors to place more emphasis on effective teaching. The 2008-2009 AACP Task Force for the Recognition of Teaching Excellence collected best teaching practices from schools/colleges of pharmacy, evaluated the literature to identify evidence-based criteria for excellent teaching, and provided recommendations on the acknowledgement and rewarding of teaching excellence.28 The characteristics of a good teacher, as defined by the task force, were distilled into six target areas for all preceptors. These include: (1) having positive student-faculty contact, (2) encouraging effective active learning, (3) setting achievable, yet high expectations, (4) respecting diverse talents and ways of learning, (5) demonstrating effective communication skills, and (6) having a commitment to teaching well.28
The PAC examined both the APPI preceptor-specific criteria of excellence and the recommendation by the Task Force on Teaching Excellence and combined them into six competencies that should be embodied with all pharmacy preceptors. These competency areas and elements that can be used to measure them are found in Table 3. It is recommended that these areas be included in all training programs for pharmacy preceptors.
Table 3.
Pharmacy Preceptor Competencies (adapted from References 27 and 28)
Just as schools/colleges of pharmacy are encouraged to provide developmental opportunities for its experiential education faculty and administrative staff members,29 there is a need for all schools/colleges of pharmacy to establish training programs for preceptors.30 Effective preceptor training programs should result in the development of, and improvement in, student pharmacist learning and satisfaction as well as contribute to providing exemplary patient care, enhancing current and developing new models of care as well as increasing preceptor satisfaction. Preceptor development in pharmacy residency training programs offers some valuable suggestions for creating an effective development plan. These include understanding accreditation standards, conducting a needs assessment, setting goals for the requirements, development and improvement of preceptor teaching skills, establishing how the preceptor training and development plan will be implemented and assessed, completing training for preceptors (as needed), evaluating the effectiveness of the training, assessing preceptors’ progress toward goals, and reviewing the entire procedure on an annual basis.31 Preceptor training programs should be delivered using a variety of approaches, including live, electronic, and paper formats, in order to accommodate preceptors. After completion of an initial preceptor training program, ongoing preceptor development should be required of preceptors every 1-2 years.
The report of the 2010 AACP Council of Sections Preceptor Development Task Force provides some valuable information regarding the types of preceptor development program components found at schools/colleges of pharmacy.32 There was a 73% response rate for the survey, which was administered to experiential education administrators at schools/colleges of pharmacy. Of these, 97% indicated they currently offer preceptor development programming. The reasons cited by respondents for not providing preceptor training included lack of time and financial resources. These responses are consistent with findings from the AACP Council of Deans Costs of Experiential Education Task Force, which reported that minimal experiential education costs were allocated toward preceptor development compared to other experiential education program costs, such as faculty salaries, administrative staff salaries, and preceptor stipends.33
Of those who offer preceptor development programming, 48% stated they required preceptor development. Most (71%) respondents indicated that their training programs for new and existing preceptors were the same. A variety of delivery methods were offered for preceptor training including live, web-based, and electronic programs as well as hard copy training materials. The task force recommended several topics for preceptor development training including how to give feedback, evaluating/grading student pharmacists, how to develop an Introductory Pharmacy Practice Experience (IPPE)/Advanced Pharmacy Practice Experience (APPE), how to manage conflict/dealing with difficult students, professional communication skills, cultural competence, incorporating student pharmacists into the practice setting, evaluating practice management, and ethics for preceptors.32 A variety of preceptor training programs were reported in the survey. These include live (92%) and web-based (52%) school-developed programs, Pharmacist’s Letter Preceptor Training and Resource Network34 (81%), the APhA/National Association of Chain Drug Stores (NACDS) Foundation Community Pharmacist Preceptor Education Program35 (64%), and the Collaborative Education Institute (CEI) preceptor program.36 While the APhA/NACDS Foundation Preceptor Program35 and the Collaborative Education Institute (CEI)36 have direct involvement with schools/colleges of pharmacy and its experiential education faculty, the Pharmacist’s Letter Preceptor Training and Resource Network34 was discussed in the task force report as having limited input from academic pharmacy. Given the large number of schools/colleges of pharmacy utilizing this training program, it may be beneficial for AACP to explore a formal relationship with The Pharmacist’s Letter for its preceptor training/development program.
There are many other examples of preceptor training/development programs provided by schools/colleges of pharmacy. Efforts such as an Academy of Preceptors,37 developing a center of teaching excellence,38 using a LearningBridge® tool,39 and other programs targeting specific practice settings40-43 are tools that schools/colleges can review and consider implementing to enhance and expand their level of preceptor training. Teaching certificate programs are also an example of training that can be extended to preceptors to advance their teaching skills.44,45 Many schools/colleges of pharmacy have developed consortiums to provide training and development for preceptors in specific regions and such approaches should be considered when possible to promote consistency and efficiency.46,47 Many schools/colleges of pharmacy have also developed an experiential education newsletter that address timely issues in experiential education and can also provide an avenue for preceptor recognition. A listing of preceptor training and development programs, including some outside of pharmacy, are found in Appendix I.
Preceptors, just as all other teachers and educators, should be assessed for their effectiveness in teaching. Schools/colleges should have a continuous quality improvement process in place to ensure preceptor development programs are achieving outcomes related to increasing preceptor effectiveness. Most schools/colleges of pharmacy do this through student pharmacist evaluations of the practice experience and practice site visits performed by experiential department personnel. Student pharmacist evaluations are sometimes criticized as being subjective and therefore having an evaluation instrument with specific questions designed to solicit factual-based responses is necessary.3 Additional assessments that may be used include preceptor self-assessment, monitoring of completion of preceptor development modules, and (re)appointment procedures for preceptors that collect information on training and development completed regarding education/precepting.
To go beyond regular preceptor development and assessment, each school/college of pharmacy should develop their own definition and criteria for preceptor excellence. A “master preceptor” should not only encompass the competencies described in Table 3, they should demonstrate the competencies over time by their education, practice, citizenship, and recognition by their peers, supervisor(s), and other organizations.
RECOGNITION OF PRECEPTOR TEACHING EXCELLENCE
Recognition of a job well done is valued by most people in a variety of situations, including academic pharmacy. Many schools/colleges of pharmacy offer tangible benefits for being a preceptor including books, clinical appointments, continuing education, tuition credits, stipend or salary compensation, and access to drug information, library resources, and reference materials.6 Many schools/colleges of pharmacy recognize faculty with awards and some include preceptor awards. Institutional teaching awards result in varying outcomes on faculty recruitment and retention.48-50
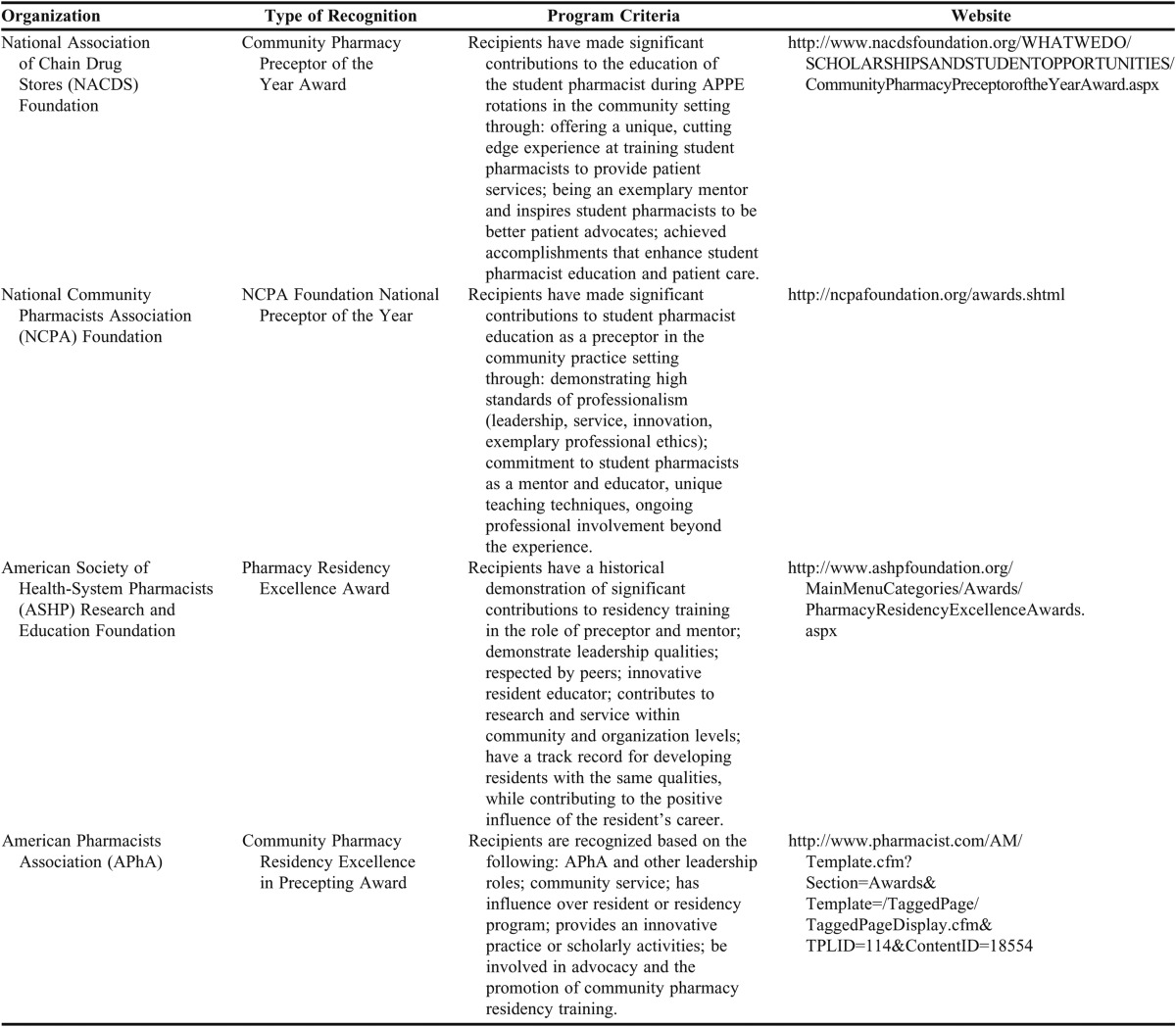
In order to attract and retain high quality preceptors, schools/colleges should ensure that preceptors are provided incentives and recognition for supporting the experiential component of their curriculum.30 In a survey of preceptor awards provided by schools/colleges, 79% of the respondents indicated providing recognition for preceptors/volunteer faculty members.48 Recognitions included a plaque or certificate, recognition at a ceremony/luncheon, monetary award, and/or travel funds for a professional conference.48 Other forms of preceptor recognition have included authorship in preceptor/experiential education newsletters and recognition in national communications.51 Various categories of preceptor recognition exist (eg, new preceptor of the year, IPPE preceptor of the year, APPE preceptor of the year) as well as differing mechanisms for selecting preceptor awards (i.e., student pharmacist vote, school/college committee vote following nominations, administrative decision, or course evaluation surveys).48 National pharmacy practice organizations also recognize the value of pharmacy preceptors and examples of such recognition programs are listed in Table 4.
Table 4.
National Pharmacy Associations' Preceptor Recognition Programs
The PAC believes that schools/colleges of pharmacy should develop preceptor recognition programs that distinguish and celebrate excellence in teaching and other essential elements in precepting. These preceptor recognition programs should be based, in part, on objective data, and should include some element of the three primary sources of evidence/data used to measure teaching excellence: (1) student pharmacists/learners and alumni; (2) peers, administrators, and/or instructional specialists; and (3) the teacher himself/herself in the form of self-assessment and reflection.28 Schools/colleges of pharmacy should create valid and reliable methods by which to judge and formally recognize preceptor teaching excellence.28
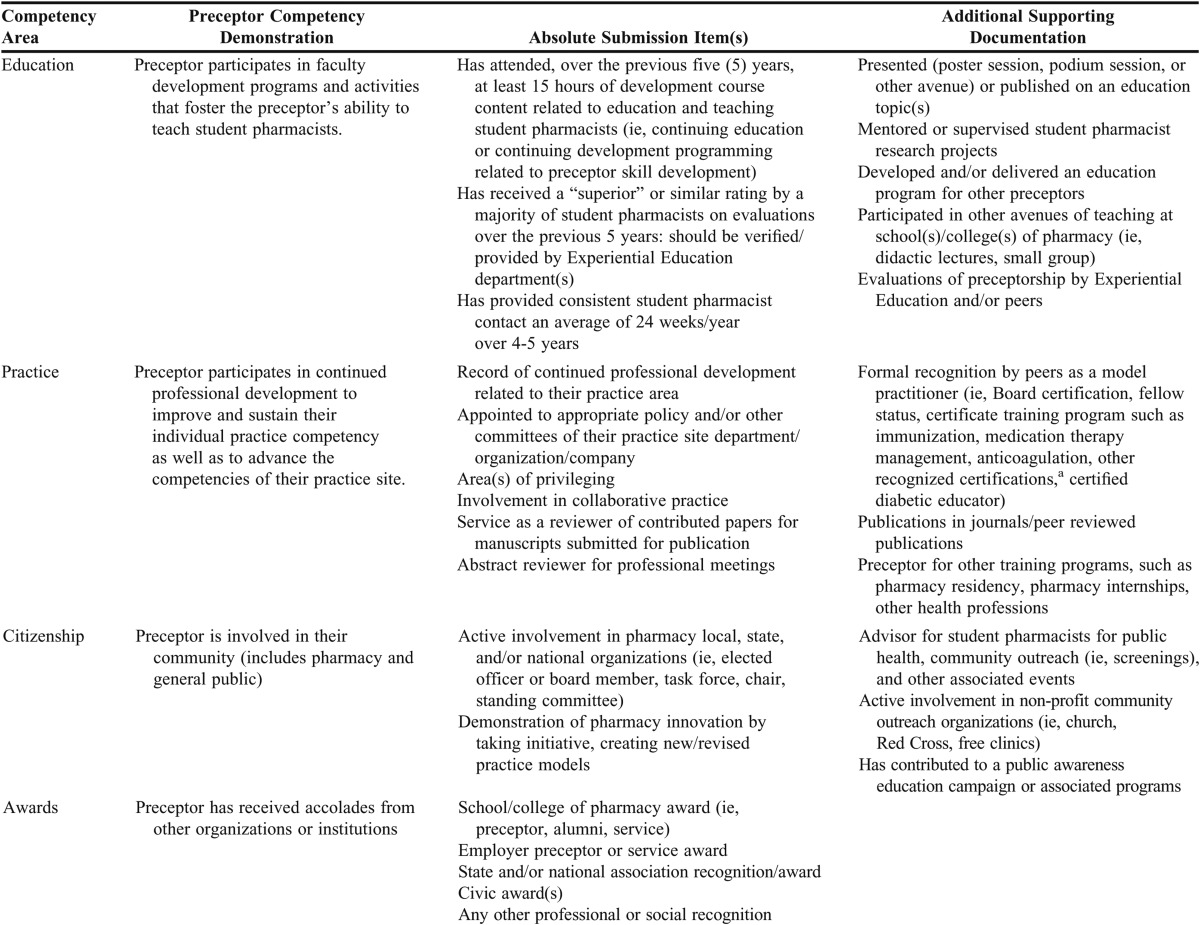
The PAC also believes that a national “master preceptor” recognition program should be created to reward and celebrate those preceptors who are exemplary in precepting and teaching. This program should be recognized by multiple pharmacy organizations, yet be administrated by AACP, as it is the national association representing pharmacy education. This AACP Master Preceptor Recognition Program would be based on criteria related to the preceptor’s training/education in teaching, practice competency, citizenship, and recognition by other persons and organizations.
The AACP Master Preceptor Recognition Program
The purpose of the AACP Master Preceptor Recognition Program is to recognize preceptors who do not directly report to a school/college of pharmacy for their professional practice position and who have demonstrated sustained commitment to excellence in experiential education. This program, to be made available annually at the beginning of each academic year (ie, August/September) would consist of a self-nomination process where preceptor applicants would complete and submit an application and a portfolio of supporting documentation.
Program Submission Materials (Content)
The program submission information should include an application that requests information from the previous five years. Exceptions to the five year period could be considered for extenuating circumstances (eg, extended leave of absence). All preceptors should be licensed pharmacists or recognized in their field of expertise by the appropriate licensure/registration and be in good standing.
The applicant must submit a personal statement/reflection statement on precepting. This statement should describe as specifically as possible their philosophy and achievements in the areas of education, professional practice, citizenship (service), and recognition, and how these demonstrate their pursuit of excellence in experiential education. The personal statement/reflection should be no more than 5 pages in length and have specifics on formatting (ie, font size) as well as detailed instructions/references on how to write a personal statement.
The applicant must also submit letters of recommendation attesting to the preceptor’s education and/or practice competency. Letters from the following individuals should be submitted with the application:
1. Dean or Experiential Education Director [or other designate] from the applicable school(s)/college(s) of pharmacy;
2. Previous IPPE or APPE students who have graduated from pharmacy school (total of 3 graduates); and
3. A direct supervisor, peer, or direct report of the preceptor.
Table 5 displays the suggested additional submission materials for the AACP Master Preceptor Recognition Program in the areas of education, practice, citizenship, and awards. The absolute submission column contains information of definitive requirements for master preceptor recognition that will be contained in the application. The additional supporting documentation column contains elements that can be demonstrated/illustrated in a portfolio or similar other system. Further development and refining of the program application content should be pursued by AACP and other interested stakeholders.
Table 5.
Submission Elements for the AACP Master Preceptor Recognition Program
Program Evaluation
Preceptor applicants will submit their materials to an evaluation committee. This committee will have the administrative assistance of an AACP staff member (who will not have a vote on the applicants) and be comprised of AACP Experiential Education Section member leadership (ie, president, president-elect, immediate past president) and representatives (preferably members involved in experiential education) of pharmacy practice organizations, such as ACCP, ASHP, APhA, the NACDS Foundation, and the National Community Pharmacists Association (NCPA). Other potential evaluation team members may include representatives from the AACP Pharmacy Practice Section and the AACP Social and Administrative Sciences Section. The evaluation committee should be comprised of no more than 15 members and may eventually include past master preceptor recipients. The evaluation team should be sent all submitted applications electronically for review and evaluation based on an assessment formulated from the recognition program attributes. Following the individual committee members review, the entire committee will meet virtually to determine master preceptor designees. There should be no set number of master preceptor awardees allocated per year as long as budgetary guidelines for the recognition program are satisfied.
Program Recognition
The recipients of the AACP Master Preceptor Recognition Program will receive a certificate of recognition that is valid for the five years following the award notification. The master preceptors can submit materials, to be determined and developed by the AACP Experiential Education Section, for reaffirmation/renewal of their master preceptor recognition status every five years. Master Preceptor Recognition recipients will receive a travel stipend to receive their award at their AACP/National Association of Boards of Pharmacy (NABP) regional meeting,52 which are generally held in late summer/early fall. In addition, recipients will have their name advertised via various communication vehicles of AACP and other pharmacy practice organizations and can be celebrated by the school(s)/college(s) of pharmacy of which they are a preceptor. They will also receive a free AACP membership for the length of their recognition period (5 years), which will provide the opportunity to further develop their skills through AACP programming and resources.
Program Outcomes
A variety of other potential valuable outcomes may result from the AACP Master Preceptor Recognition Program. Mechanisms such as an AACP special interest group [SIG], LinkedIn, or Facebook page could be developed for the AACP Master Preceptor recipients to communicate with one another and other stakeholders interested in precepting. Recipients could also be used for continuing education/continuing professional development programming for preceptors at schools/colleges of pharmacy as well as national, state, and regional pharmacy meetings. The formation of an Academy of Master Preceptors, comprised of current AACP Master Preceptor recipients, could serve as an advisory board to AACP and other interested stakeholders to develop standards and best practices for effective and exemplary precepting and preceptor development.
CONCLUSION
The application of knowledge in practice environments is an effective and accepted learning experience methodology used by many professions including pharmacy. Reliance on experiential educators has expanded in quantity and diversity of experience concurrently with the increased numbers of ACPE accredited schools/colleges of pharmacy across the United States. Consensus from practitioners, practice organizations, and academia on recognizing the merits of experiential educators and the need for consistent training and education of these practice educators has been proposed. Supporting the professional development of teaching practitioners and cultivating these practitioners to pursue teaching excellence to the benefit of student pharmacists would be most readily achieved by a cooperative effort by all interested professional stake holders. Though the ability and efforts put forth by experiential educators has been recognized by many schools and colleges of pharmacy, the need to step forward, share and recognize the leadership and commitment to excellence in teaching student pharmacists at a higher level is best directed by AACP, the national organization of pharmacy educators.
In response to the charge by AACP President Brian Crabtree, this committee examined preceptor recognition programs in pharmacy and other professions. The committee evaluated the potential benefits and challenges that would be required in defining a “Master Preceptor” that supported the schools and colleges of pharmacy programs already in place. Continuing to partner with members of the Academy and supporting the advancement of both our student pharmacists and our valuable preceptors led to the development of the proposed policy statements and recommendations related to preceptor development and recognition.
Appendix 1. Preceptor Development Programs/Resources
REFERENCES
- 1.Crabtree BL. Excellence and relevance. Am J Pharm Educ. 2011;75(9):Article 173. doi: 10.5688/ajpe767121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Harralson AF. Financial personnel, and curricular characteristics of advanced practice experience programs. Am J Pharm Educ. 2003;67(1):Article 17. [Google Scholar]
- 3.Littlefield LC, Haines ST, Harralson AF, et al. Academic pharmacy’s role in advancing practice and assuring quality in experiential education: Report of the 2003-2004 Professional Affairs Committee. Am J Pharm Educ. 2004;68(3):Article S8. [Google Scholar]
- 4.Plaza CM, Draugalis JR. Implications of advanced pharmacy practice experience placements: a 5-year update. Am J Pharm Educ. 2005;69(3):Article.45.. [Google Scholar]
- 5.Skrabal MZ, Kahaleh AA, Nemire RE, et al. Preceptors’ perspectives on benefits of precepting student pharmacists to students, preceptors, and the profession. J Am Pharm Assoc. 2006;46(5):605–612. doi: 10.1331/1544-3191.46.5.605.skrabal. [DOI] [PubMed] [Google Scholar]
- 6.Skrabal MZ, Jones RM, Nemire RE, et al. National survey of volunteer pharmacy preceptors. Am J Pharm Educ. 2008;72(5):Article 112. doi: 10.5688/aj7205112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. National Association of Boards of Pharmacy Survey of Pharmacy Law 2012, National Association of Boards of Pharmacy; CD Rom, 2011. [Google Scholar]
- 8.Accreditation Council for Pharmacy Education. Accreditation standards and guidelines for the professional program in pharmacy leading to the doctor of pharmacy degree: Guidelines Version 2.0. Chicago, IL: Accreditation Council for Pharmacy Education: 2011. https://www.acpe-accredit.org/pdf/FinalS2007Guidelines2.0.pdf. Accessed July 7, 2012.
- 9.AACP Institutional Research. http://www.aacp.org/RESOURCES/RESEARCH/INSTITUTIONALRESEARCH/Pages/default.aspx. Accessed July 7, 2012.
- 10.AACP Preceptor Survey Information and Summary Reports. http://www.aacp.org/resources/research/institutionalresearch/Pages/PreceptorSurveyInformationandSummaryReports.aspx. Accessed July 7, 2012.
- 11.American Society of Health-System Pharmacists. ASHP accreditation standard for postgraduate year one (PGY1) pharmacy residency programs. http://www.ashp.org/DocLibrary/Accreditation/ASD-PGY1-Standard.aspx. Accessed July 7, 2012.
- 12.American Society of Health-System Pharmacists. ASHP accreditation standard for postgraduate year two (PGY2) pharmacy residency programs. http://www.ashp.org/DocLibrary/Accreditation/ASD-PGY2-Standard.aspx. Accessed July 7, 2012.
- 13.American Society of Health-System Pharmacists. Commission on Credentialing meeting highlights. http://www.ashp.org/DocLibrary/Accreditation/Communiqu-Newsletter/Communique-Fall-2011.aspx. Accessed July 7, 2012.
- 14.Assemi M, Corelli RL, Ambrose PJ. Development needs of volunteer pharmacy practice preceptors. Am J Pharm Educ. 2011;75(1):Article 10. doi: 10.5688/ajpe75110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Payakachat N, Ounpraseuth S, Ragland D, et al. Job and career satisfaction among pharmacy preceptors. Am J Pharm Educ. 2011;75(8):Article 153. doi: 10.5688/ajpe758153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Baldor RA, Brooks WB, Warfield MD, et al. A survey of primary care physicians’ perceptions and needs regarding the precepting of medical students in their offices. Med Educ. 2001;35(8):739–795. doi: 10.1046/j.1365-2923.2001.00980.x. [DOI] [PubMed] [Google Scholar]
- 17.Kumar A, Loomba D, Rahangdale RY, et al. Rewards and incentives for nonsalaried clinical faculty who teach medical students. J Gen Intern Med. 1999;14(6):370–372. doi: 10.1046/j.1525-1497.1999.00341.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Chisholm MA, Hawkins DW, Taylor AT. Providing pharmaceutical care: are pharmacy students beneficial to patients? Hosp Pharm. 1997;32(3):370–375. [Google Scholar]
- 19.Briceland LL, Kane MP, Hamilton RA. Evaluation of patient-care interventions by PharmD clerkship students. Am J Hosp Pharm. 1992;49(5):1130–1132. [PubMed] [Google Scholar]
- 20.Haase KK, Smythe MA, Orlando PL, et al. ACCP White paper: quality experiential education. Pharmacotherapy. 2008;28(10):219e–227e. doi: 10.1592/phco.28.12.1548. [DOI] [PubMed] [Google Scholar]
- 21.American Association of Colleges of Pharmacy Academic-Practice Partnership Initiative. http://www.aacp.org/resources/education/APPI/Pages/default.aspx. Accessed July 7, 2012.
- 22.American Association of Colleges of Pharmacy Academic Practice Partnership Initiative Summit to Advance Experiential Education in Pharmacy: Final Report and Proceedings. http://www.aacp.org/resources/education/APPI/Documents/SummitFinalReport.pdf. Accessed July 7, 2012.
- 23.Professional Experience Program (PEP) Library of Resources. http://www.peplibrary.vcu.edu/index.html. Accessed July 7, 2012.
- 24.American Association of Colleges of Pharmacy. Development of a profile system to display exemplary pharmacy Practice experiential sites. http://www.aacp.org/resources/education/APPI/Documents/ExemplaryPPEs.pdf. Accessed July 7, 2012.
- 25.AACP Crystal APPLE Award. http://www.aacp.org/career/awards/Pages/crystalappleaward.aspx. Accessed July 7, 2012.
- 26.American Association of Colleges of Pharmacy Center for the Advancement of Pharmaceutical Education, Educational Outcomes 2004. http://www.aacp.org/resources/education/Documents/CAPE2004.pdf. Accessed July 7, 2012.
- 27.American Association of Colleges of Pharmacy Academic-Practice Partnership Initiative (APPI) Preceptor-Specific Criteria of Excellence. http://www.aacp.org/resources/education/APPI/Documents/Preceptor%20Criteria%20PPEs.pdf. accessed July 7, 2012.
- 28.Hammer D, Piascik P, Medina M, et al. Recognition of teaching excellence. Am J Pharm Educ. 2010;74(9):Article 164. doi: 10.5688/aj7409164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Reynolds JR, Briceland LL, Carter JT, et al. Experiential education delivery—ensuring success through support and development of the faculty and administrative team: Report of the 2004-2005 Professional Affairs Committee. 2005;26(5):Article S9. [Google Scholar]
- 30.Haase KK, Smythe MA, Orlando PL, et al. ACCP White paper: quality experiential education. Pharmacotherapy. 2008;28(10):219e–227e. doi: 10.1592/phco.28.12.1548. [DOI] [PubMed] [Google Scholar]
- 31.Ricchetti C, Jun A. Strategies and resources for successful preceptor development. Am J Health-Syst Pharm. 2011;68:1837–1842. doi: 10.2146/ajhp100654. [DOI] [PubMed] [Google Scholar]
- 32. 2010 AACP Council of Sections Preceptor Development Task Force. Report made available from Denise Soltis, Chair of the 2010 AACP Council of Sections Preceptor Development Task Force, July 15, 2011.
- 33.Final Report of the Council of Deans Costs of Experiential Education Task Force. http://www.aacp.org/governance/councildeans/Documents/FINAL%20REPORT%20-%20AACP%20Cost%20Exp%20Ed%20TF%20-%205-26-09.pdf. Accessed July 7, 2012.
- 34. The Pharmacist Letter Preceptor Training and Resource Network. http://pharmacistsletter.therapeuticresearch.com/ptrn/default.aspx?cs=&s=PL. Accessed July 7, 2012.
- 35.American Pharmacists Association (APhA) and National Association of Chain Drug Stores (NACDS) Foundation Community Pharmacist Preceptor Education Program. http:/www./pharmacists.com/AM/Template.cfm?Section=Preceptor_Resources. Accessed July 7, 2012.
- 36.Collaborative Education Institute Preceptor Program. http://www.theceinstitute.org/Preceptor.aspx. Accessed July 7, 2012.
- 37.Boyle CJ, Morgan JA, Layson-Wolf C, et al. Developing and implementing an academy of preceptors. Am J Pharm Educ. 2009;73(2):Article 34. doi: 10.5688/aj730234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Andurkar S, Fjortoft N, Sincak C, et al. Development of a center for teaching excellence. Am J Pharm Educ. 2010;74(7):Article 123. doi: 10.5688/aj7407123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Karimi R, Cawley P, Arendt CS. Learning bridge tool to improve student learning, preceptor training, and faculty teamwork. Am J Pharm Educ. 2011;73(3):Article 46. doi: 10.5688/ajpe75346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Cerulli J, Briceland LL. A streamline training program for community pharmacy advanced practice preceptors to enable optimal experiential learning opportunities. Am J Pharm Educ. 2004;68(1):Article 9. [Google Scholar]
- 41.Scott DM, Narducci WA, Jungnickel PW, et al. Pharmaceutical care preceptor training and assessment in community pharmacy clerkship sites. Am J Pharm Educ. 1999;63(3):265–271. [Google Scholar]
- 42.Rodis JL, Legg JE, Casper KA. Partner for promotion: An innovative advanced community pharmacy practice experience. Am J Pharm Educ. 2009;72(6):Article 134. doi: 10.5688/aj7206134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Bianco T, Haxby DG, Vanderveen RP, et al. Development of ambulatory clerkships in a managed care setting. Am J Pharm Educ. 1996;60(1):48–52. [Google Scholar]
- 44.Romanelli F, Smith KM, Brandt BF. Teaching residents how to teach: a scholarship of teaching and learning certificate program (STLC) for Pharmacy Residents. Am J Pharm Educ. 2005;69(2):Article 2. [Google Scholar]
- 45.Gettig JP, Sheehan AH. Perceived value of a pharmacy resident teaching certificate program. Am J Pharm Educ. 2008;72(5):Article 104.. doi: 10.5688/aj7205104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Duke LJ, Unterwagner WL, Byrd DC. Establishment of a multi-state experiential pharmacy program consortium. Am J Pharm Educ. 2008;72(3):Article 62. doi: 10.5688/aj720362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.McDuffie CH, Duke LJ, Stevenson TL. Consortium-based approach to an online preceptor development program. Am J Pharm Educ. 2011;75(7):Article 135. doi: 10.5688/ajpe757135. 10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Kalis MM, Kirschenbaum HL. Faculty awards at US colleges and schools of pharmacy. Am J Pharm Educ. 2008;72(4):Article 85. doi: 10.5688/aj720485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Chism NVN. Teaching awards: what do they award? J High Educ. 2006;77(4):589–617. [Google Scholar]
- 50.Batshaw ML, Plotnick LP, Petty BG, et al. Academic promotion at a medical school: experience at Johns Hopkins University School of Medicine. New Engl J Med. 1988;318(12):741–747. doi: 10.1056/NEJM198803243181204. [DOI] [PubMed] [Google Scholar]
- 51.20Ways. www.rxinsider.com/20Ways/. Accessed February 21, 2012.
- 52.NABP/ACCP District Meeting Dates and Locations. http://www.nabp.net/meetings/district-meetings. Accessed July 7, 2012.
- 53.Certification Programs for Pharmacists. Council on Credentialing in Pharmacy (CCP) website. http://pharmacycredentialing.org/ccp/Files/CertificationPrograms-comprehensivelist08-10Final.pdf. Accessed July 7, 2012.