Abstract
All of the currently available antiviral agents used to treat double-stranded (ds) DNA viruses inhibit the same target, the viral DNA polymerase, with the exception of interferon-α. With increasing reports of the development of resistance of herpes simplex virus, cytomegalovirus, and hepatitis B virus to some of these drugs, new antiviral agents are needed for these infections. Additionally, no drugs are approved to treat several DNA virus infections including those caused by adenovirus, smallpox, molluscum contagiosum, and BK virus. We report on the status of 10 new antiviral drugs for the treatment of dsDNA viruses. CMX-001 has broad activity against dsDNA viruses; 3 helicase-primase inhibitors, marabavir, and FV-100 have activity against certain herpesviruses; ST-246 inhibits poxviruses; GS-9191 inhibits papillomaviruses; and clevudine and emtricitabine are active against hepatitis B virus. Most of these drugs have completed at least phase I trials in humans and several are in additional clinical trials.
Keywords: antivirals, DNA viruses, herpesvirus, hepatitis B virus, adenovirus, poxvirus, human papillomavirus, CMX-001, BAY 57-1293, BILS 179 BS, ASP2151, FV-100, maribivar, ST-246, GS-9191, clevudine, emtricitabine
Introduction
The double-stranded (ds) DNA viruses include herpesviruses, polyomaviruses, papillomaviruses, hepadnaviruses (e.g. hepatitis B virus [HBV]), adenoviruses, and poxviruses. With the exception of the poxviruses, these viruses often establish persistent or latent infections and can reactivate in healthy or immunosuppressed persons. In the latter, these viruses can cause severe and sometimes fatal disease. All of the licensed drugs used for the systemic treatment of herpesviruses and for HBV inhibit the viral DNA polymerase with the exception of interferon-alpha that is used to treat HBV infection (Table 1). Approved therapies for papillomavirus include topical imiquimod and intralesional interferon-alpha.
Table 1.
Currently approved systemic antivirals for double-stranded DNA viruses
| Drug | HSV | VZV | CMV | EBV | Pox | Adeno | BK | HPV | HBV | Mechanism |
|---|---|---|---|---|---|---|---|---|---|---|
| Acyclovir | + | + | − | − | − | − | − | − | − | DNA polymerase |
| Famciclovir | + | + | − | − | − | − | − | − | − | DNA polymerase |
| Valacyclovir | + | + | − | − | − | − | − | − | − | DNA polymerase |
| Ganciclovir | − | − | + | − | − | − | − | − | − | DNA polymerase |
| Valganciclovir | − | − | + | − | − | − | − | − | − | DNA polymerase |
| Foscarnet | * | * | + | − | − | − | − | − | − | DNA polymerase |
| Cidofovir | * | * | + | − | # | # | # | # | − | DNA polymerase |
| Lamivudine | − | − | − | − | − | − | − | − | + | DNA polymerase |
| Adefovir | − | − | − | − | − | − | − | − | + | DNA polymerase |
| Entecavir | − | − | − | − | − | − | − | − | + | DNA polymerase |
| Telbivudine | − | − | − | − | − | − | − | − | + | DNA polymerase |
| Tenofovir | − | − | − | − | − | − | − | − | + | DNA polymerase |
| IFN-α | − | − | − | − | − | − | − | − | + | Multiple |
Not approved for use by FDA for this indication, but has activity in vitro and has been used to treat resistant virus
Not approved for use by FDA for this indication, but has activity in vitro and has been used for treatment for severe disease
HSV, herpes simplex virus; VZV, varicella-zoster virus, CMV, cytomegalovirus, EBV, Epstein-Barr virus; Pox, poxvirus; Adeno, adenovirus; BK, BK polyomavirus; HPV, human papillomavirus; HBV, hepatitis B virus.
While a large number of new drugs have been developed for HIV, a clear need exists for new drugs to treat dsDNA virus infections, including some viruses for which no drugs are approved (e.g. adenovirus, polyomavirus) (Table 2). In addition, with many licensed drugs acting on the same viral protein and the emergence of drug resistance, new antivirals directed against other viral targets are important. Finally, the toxicity associated with some antivirals limits their use and less toxic and more effective drugs are needed. This review will focus on several promising new drugs for the treatment of DNA virus infections.
Table 2.
Rationale for the development of new antivirals for the treatment of double-stranded DNA virus infections
|
CMX-001
CMX001 (phosphonic acid, [[(S)-2-(4-aminio-2-oxo-1(2H)-pyrimidinyl)-1-(hydroxymethyl)ethoxy]methyl]mono[3-(hexadecyloxy)propyl] ester; hexadecyloxypropyl cidofovir) (Figure 1A) is an orally-administered, bioavailable lipid conjugate of the nucleotide analog cidofovir, first described by Hostetler and colleagues (1). Addition of the lipid moiety to cidofovir improves the oral bioavailability compared to its parent compound, cidofovir, which has an oral bioavailability of < 5% and must be administered intravenously for systemic therapy. CMX001 was developed as an antiviral because of its bioavailability and minimal toxicity in animal studies compared with intravenous cidofovir. CMX001 has potent antiviral activity in cell culture against members of each of the double-stranded DNA virus families that are pathogenic to humans, including orthopoxviruses, herpesviruses, polyomaviruses, papillomaviruses, and adenoviruses. The mechanism for increased antiviral activity of CMX001 compared with cidofovir (Table 3) is likely dependent on the greater cell uptake of CMX001 with subsequent enhanced conversion of cidofovir to the active diphosphate compound. CMX001 is absorbed in the small intestine and then delivered to target organs throughout the body where its conjugated lysophospholipid crosses cell membranes by passive and facilitated diffusion. Once inside the cell, the lipid phosphate ester linkage of CMX001 is cleaved by intracellular phospholipases to release cidofovir. The free cidofovir is converted to cidofovir diphosphate by cellular kinases. Thus, viral thymidine kinase is not needed for activation of this compound. Cidofovir diphosphate is a potent alternative substrate inhibitor of DNA synthesis catalyzed by viral DNA polymerases. Cidofovir diphosphate is efficiently incorporated into the nascent viral DNA chain by these polymerases, resulting in a reduction in the overall rate of viral DNA synthesis. While polyoma and papilloma viruses do not encode a DNA polymerase, CMX001 is active in vitro against representative members of both families of viruses. The mechanism of action is unknown.
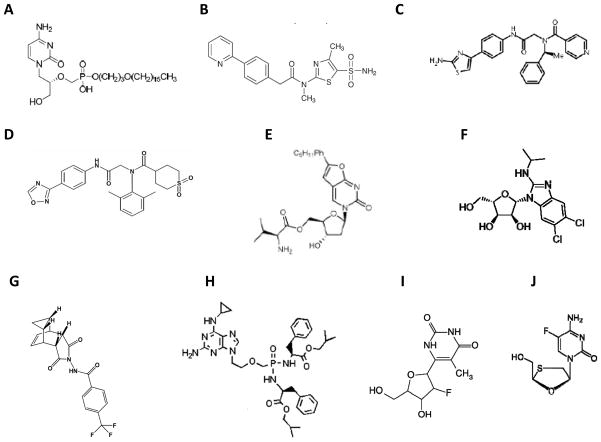
Figure 1.
Structures of CMX-001 (A), BAY 57-1293 (B), BILS 179 BS (C), ASP2151 (D), FV-100 (E), Maribivar (F), ST-246 (G), GS-9191 (H), Clevudine (I), Emtricitabine (J).
Table 3.
In vitro activity of new antivirals for double-stranded DNA viruses
| Drug | HSV | VZV | CMV | EBV | Pox | Adeno | BK | HPV | HBV | Mechanism |
|---|---|---|---|---|---|---|---|---|---|---|
| CMX-001 | + | + | + | + | + | + | + | + | ND | DNA polymerase |
| BAY 57-1293 | + | − | − | ND | ND | ND | ND | ND | ND | Helicase-primase |
| BILS 179 | + | − | − | ND | ND | ND | ND | ND | ND | Helicase-primase |
| ASP2151 | + | + | ND | ND | ND | ND | ND | ND | ND | Helicase-primase |
| FV-100 | − | + | − | ND | ND | ND | ND | ND | ND | DNA polymerase |
| Maribavir | − | − | + | + | ND | ND | ND | ND | ND | UL97 kinase |
| ST-246 | ND | ND | ND | ND | + | ND | ND | ND | ND | V061 envelope protein |
| GS-9191 | ND | ND | ND | ND | ND | ND | ND | + | ND | DNA polymerase |
| Clevudine | ND | ND | ND | ND | ND | ND | ND | ND | + | DNA polymerase |
| Emtricitabine | ND | ND | ND | ND | ND | ND | ND | ND | + | DNA polymerase |
HSV, herpes simplex virus; VZV, varicella-zoster virus, CMV, cytomegalovirus, EBV, Epstein-Barr virus; Pox, poxvirus; Adeno, adenovirus; BK, BK polyomavirus; HPV, human papillomavirus; HBV, hepatitis B virus; ND, not described.
The effective concentration of CMX001 required to inhibit replication of the orthopoxviruses, variola major and vaccinia virus, by 50% (EC50), is about 270 and 60-fold lower, respectively, than the EC50 obtained with cidofovir (Table 4). The activity of CMX001 against herpes simplex virus (HSV)-1 and cytomegalovirus (CMV) is enhanced about 300 to 400-fold compared to cidofovir. CMX001 also exhibits potent antiviral activity against ganciclovir-, foscarnet-, and cidofovir-resistant CMV mutants. The replication of other herpesviruses, such as varicella-zoster virus (VZV), Epstein-Barr virus (EBV), human herpesvirus (HHV)-6, and HHV-8, is markedly inhibited by CMX001. The EC50 values of CMX001 for inhibiting VZV and EBV replication are at least 1,000-fold lower than the EC50 values obtained with cidofovir. The EC50 values for inhibiting HHV-6 and HHV-8 replication are 100 to 900 fold lower for CMX001 than cidofovir. Thus, CMX001 has potent activity against each of the human herpesviruses.
Table 4.
Antiviral activity of CMX001 compared to parent compound, cidofovir
| Virus | Cell Line | Cidofovir EC50 (μM)) | CMX001 EC50 (μM) | Enhanced Activity | Reference |
|---|---|---|---|---|---|
| Variola major | NR | 27.3 | 0.10 | 273 | 2 |
| Vaccinia | HFF | 46.2 | 0.8 | 58 | 3 |
| HSV-1 | HFF | 22.5 | 0.08 | 280 | 1 |
| HCMV (AD169) | HFF | 0.38 | 0.0009 | 422 | 1 |
| HHV-6A | HSB-2 | 2.7 | 0.003 | 900 | 4 |
| HHV-6B | Molt-3 | 5.4 | 0.007 | 770 | 4 |
| HHV-8 | BCBL-1 | 2.6 | 0.02 | 130 | 4 |
| VZV | HFF | 0.5 | 0.0004 | 1250 | 4 |
| EBV | Daudi | 65.6 | 0.03 | 2186 | 4 |
| BK virus | WI-38 | 115.1 | 0.13 | 885 | 5 |
| Adenovirus 3 | HFF | 2.0 | 0.01 | 200 | 6 |
| Adenovirus 7 | HFF | 1.3 | 0.02 | 65 | 6 |
| Adenovirus 31 | HFF | 1.4 | 0.28 | 5 | 6 |
| HPV 18 | HeLa | 516 | 0.42 | 1228 | 7 |
| Resistant CMV | HFF | 2.3 | 0.003 | 760 | 1 |
NR, not reported; HFF, human foreskin fibroblasts; HSB-2, T cell leukemia cell line; Molt-3, human T-lymphoblastic cell line; BCBL-1, HHV-8-infected peripheral effusion lymphoma cell line; Daudi, human Burkitt’s lymphoma cell line; WI-38, human diploid lung cell line; HeLa, human epithelial cervical cancer cell line.
The EC50 determined for inhibiting BK virus replication in vitro is about 900-fold lower for CMX001 than cidofovir. CMX001 inhibited cell proliferation in human papillomavirus (HPV)-transformed HeLa cells 1,200-fold more effectively than cidofovir. The EC50 values of CMX001 for different serotypes of adenovirus were 5 to 200-fold lower than those obtained with cidofovir.
Animal studies: CMX001
CMX001 has been shown to be protective against disease in animal models of orthopoxvirus, CMV, and adenovirus infection. CMX001 was initially developed for the prevention and treatment of smallpox virus. The compound was effective in lethal models of cowpox and vaccinia virus infection in mice. CMX001 reduced the mortality of intranasally infected mice when it was administered prior to or 1, 2, or 3 days after infection (8). In a lethal aerosol challenge mouse model of ectromelia (mousepox) virus infection, CMX001 given orally prevented mortality from a high dose challenge and virus titers in the liver and spleen were reduced below the limit of detection (9). Oral CMX001 (5 mg/kg twice daily) administered for 5 days, beginning 1 day before infection with rabbitpox virus, completely protected rabbits from death (10).
Since human CMV does not replicate in animals, mice with severe combined immune deficiency (SCID) received human retinal or human thymus/liver tissue implants and then were infected with HCMV (11). Daily oral administration of CMX001 (5 or 10 mg/kg) was as effective in inhibiting CMV replication in human retinal tissue implants as daily dosing with 20 mg/kg of intraperitoneal cidofovir. Daily oral administration of CMX001 (5 to 10 mg/kg) in SCID mice with CMV-infected human thymus/liver tissue implants reduced virus replication below detectable limits, which represented a 4- to 5-log reduction in CMV replication compared with vehicle-treated controls.
Toth et al. developed a model for adenovirus infection in immunosuppressed Syrian hamsters, which resembles the severe infections seen in immuncompromised patients (12). CMX001 administered orally before or up to 2 days after intravenous infection with adenovirus serotype 5 significantly reduced morbidity and mortality compared to untreated animals. CMX001 decreased viral replication in the liver, pancreas, and salivary gland of the animals.
Safety studies in mice, rats, and monkeys showed dose-dependent enteritis that was reversible when the drug was discontinued. Unlike cidofovir, dose-dependent renal insufficiency or bone marrow toxicity was not observed with CMX001.
Clinical Studies: CMX001
The first human study with CMX001 was a dose-escalation, placebo-controlled, safety and pharmacokinetic study in healthy adults with 9 single dose cohorts (0.025 to 2 mg/kg) and 5 multi-dose cohorts (0.1 to 1 mg/kg) (13). CMX001 was well tolerated without any dose-limiting adverse events; no gastrointestinal, renal or hematologic toxicity was attributed to CMX001. Pharmacokinetic analyses showed that CMX001 was well absorbed and plasma concentrations achieved were predicted to be therapeutic against dsDNA viruses.
Oral CMX001 was used in combination with ST-246 (see below) for the treatment of progressive vaccinia in a patient who began cytotoxic chemotherapy for acute leukemia shortly after receiving the smallpox vaccine (14). The patient recovered; however, the patient’s improvement may have been due to vaccinia immune globulin, ST-246, CMX-001, recovery of his lymphocyte count, or a combination of these interventions.
A phase I/II multicenter, randomized, double-blind, placebo-controlled, multiple dose study to evaluate the safety, tolerability, and pharmacokinetics of CMX001 in renal transplant and hematopoietic stem cell transplant (HSCT) recipients with BK virus viruria is ongoing (www.clinicaltrials.gov). A secondary objective of this study is to evaluate the effect of CMX001 on the BK virus load in the urine and plasma. A second study, a phase II multicenter, randomized, double-blind, placebo-controlled, dose-escalation study of the safety, tolerability, and ability of CMX001 to prevent or control CMV infection in high risk HSCT patients is also in progress.
BAY 57-1293, BILS 179 BS, and ASP2151: HELICASE-PRIMASE INHIBITORS
BAY 57-1293 (Figure 1B) and BILS 179 BS (Figure 1C) were identified by high throughput screening of chemical libraries. Initially, compounds were found that inhibited HSV targets and these were subsequently modified to have more favorable pharmacologic activities (15, 16). BAY 57-1293, BILS 179 BS, and ASP2151 (17; Figure 1D) inhibit the helicase-primasecomplex of HSV, which is required for unwinding double-stranded viral DNA so that new DNA synthesis can occur; this is essential for virus replication.
The concentration of drug required to inhibit virus replication by 50% (IC50) for BAY 57-1293 is 0.02 uM for HSV-1, HSV-2, and acyclovir-resistant HSV-1 (16). HSV-1 resistant to BAY 57-1293 has mutations in the UL5 or UL52 genes of HSV that encode the helicase-primase complex. These drug-resistant viruses are still sensitive to acyclovir. The EC50 of BILS 179 BS for HSV-1 is 0.08–0.10 uM, for HSV-2 is 0.010–0.011 uM, for acyclovir-resistant HSV-1 0.13 uM, and for acyclovir-resistant HSV-2 0.09 uM. BAY 57-1293 and BILS 179 BS have little or no activity against VZV or CMV.
The EC50s of ASP2151 for HSV-1 are 0.016–0.042 uM, for HSV-2 are 0.032–0.12 uM, and for VZV are 0.038–0.10, which are lower than those for acyclovir (17). ASP2151 has no activity against CMV. A VZV mutant obtained after serial passage with the antiviral drug was less sensitive to inhibition and had a mutation in the viral helicase (17).
Animal Studies: helicase-primase inhibitors
Oral BAY 57-1293 protected mice from a lethal intranasal dose of HSV-1 or HSV-2, and reduced recurrent skin lesions in mice infected with HSV-2 on scarified skin (16). BAY 57-1293 was more effective for both HSV-1 and HSV-2 than acyclovir, valacyclovir, famciclovir, or ganciclovir in mice (18). Animals treated with BAY 57-1293 had lower titers of virus in the lung, brain, and trigeminal ganglia during acute infection and much less latent virus in trigeminal ganglia. Unlike acyclovir-resistant HSV-1 which is often less pathogenic than wild-type virus, a BAY 57-1293-resistant HSV-1 was almost as pathogenic as wild-type virus in mice after intranasal inoculation (18). The observation that drug-resistant viruses are present at relatively high frequencies (up to 10−4) in vitro and that they retain full or nearly full pathogenicity in animal models raises some concerns about BAY 57-1293 (19). Topical BAY 57-1293 was more effective than acyclovir for treatment of herpetic skin lesions in mice after dermal inoculation with HSV-2 (18). Likewise, topical BAY 57-1293 was more effective than acyclovir in preventing ocular disease and encephalitis in mice after corneal scarification and infection with HSV-1.
Oral BAY 57-1293 reduced acute and recurrent genital HSV-2 disease in guinea pigs after intravaginal inoculation (16). The drug was given on days 4–14 days after infection for acute disease experiments, at a time when disease had already begun, and given on day 0–4 in a recurrent disease model. BAY 57-1293 was more effective than valacyclovir in guinea pigs. BAY 57-1293 also reduced the amount of viral DNA in the dorsal root ganglia (20). Oral BAY 57-1293 reduced HSV-1 reactivation from the eye of rabbits after heat stress and reduced virus DNA in the trigeminal ganglia (21).
Oral BILS 179 BS reduced recurrent skin lesions in mice infected with HSV-1 on scarified skin (15). The drug also reduced acute HSV-2 genital disease, mortality, and shedding in a mouse model when animals were inoculated intravaginally (15); the drug was more effective than acyclovir in these studies. Oral BILS 45 BS, a structural analog of BILS 179 BS, reduced lesion scores in athymic mice inoculated cutaneously with acyclovir-resistant HSV-1 (22). Oral ASP2151 reduced disease in mice subcutaneously injected with HSV-1 more effectively than oral valacylovir (23).
Clinical Studies: helicase-primase inhibitors
Two clinical trials of ASP2151 have been completed (www.clinicaltrials.gov); however, results have not yet been reported. A randomized, placebo-controlled, dose-finding study with ASP2151 was performed in subjects with recurrent episodes of genital herpes. The primary endpoint was to compare the efficacy and safety of ASP2151 with valacyclovir and placebo in the acute treatment of recurrent genital HSV. The second study was a randomized, double-blind, dose-finding study of ASP2151 versus valacyclovir in persons with herpes zoster. The primary endpoint was to compare the efficacy and safety of ASP2151 with valacyclovir, while the secondary endpoint was to compare improvement of cutaneous symptoms and pain. A randomized, double-blind, multiple dose study comparing the safety of ASP2151 with valacylcovir and placebo in healthy volunteers was terminated because of treatment-emergent serious adverse events (www.clinicaltrials.gov).
FV-100
FV-100 (Figure 1E), an oral prodrug of CF1743, is a bicyclic nucleoside analog with potent activity against VZV (24). The original drug, Cf1743, was active in vitro, but very lipophilic. FV-100, is the valine ester of Cf1743, and is >500-fold more water soluble than Cf1743. Cf1743 is phosphorylated by the VZV thymidine kinase (but not by the other human herpesvirus thymidine kinases) and may undergo additional modifications inside the cell. The drug inhibits the VZV DNA polymerase. Cf1743 is active against VZV, but not against other human herpesviruses. The EC50 for FV-100 against VZV is 0.0026 uM, which is about 1,000-fold lower than that for acyclovir (24). VZV strains resistant to acyclovir are also resistant to CF1743.
Animal Studies: FV-100
Cf1743 showed no toxicity in mice. Since there is no small animal model in which VZV causes disease, in vivo studies of FV-100 to protect against VZV disease have not been performed in animals.
Clinical Studies: FV-100
Phase I human trials showed no apparent toxicity of FV-100 and concluded that once daily dosing is likely to be sufficient (25). A randomized, double-blind, comparative study of FV-100 versus valacyclovir in patients with herpes zoster is currently in progress (www.clinicaltrials.gov). The primary outcome measurement is herpes zoster associated pain, as measured by the zoster brief pain inventory.
MARIBAVIR
Maribavir is 1-β-L-ribofuranosyl-2-isopropylamino-5,6-dichlorobenzimidazole (Figure 1F). It was synthesized as a benzimidazole with an L-sugar moiety because this improves the biostability of the drug (26). Maribavir has activity against CMV and EBV, but not against other human herpesviruses. The IC50 against CMV is 19.4 ± 18.6 μM and for EBV is 10 ± 8 μM (27). The IC50 values against 11 clinical CMV isolates ranged from 0.03 to 0.13 μM for maribavir, compared to 0.15 to 1.10 μM for ganciclovir (26). Maribavir’s mechanism of action is unique compared to the currently approved antivirals for CMV in that maribavir inhibits the viral UL97 kinase rather than the viral DNA polymerase (26). In addition, maribavir does need to be phosphorylated for its activity. The UL97 kinase is important for viral DNA elongation, DNA packaging, and nuclear egress of encapsidated viral DNA. While the UL97 kinase is important for phosphorylation and activation of ganciclovir, mutations that confer resistance to ganciclovir occur in a different location than those that result in resistance to maribavir. Accordingly, maribavir has activity against CMV isolates that are resistant to ganciclovir, foscarnet or cidofovir (26, 28). Cross-resistance between maribavir and other anti-CMV antivirals has not been reported. Mutations in UL97 and UL27 (which encodes glycoprotein B) that confer resistance to maribavir have been identified in vitro (29). To date, no maribavir-resistant CMV strains have been reported in patients treated with the drug. Maribavir inhibits the EBV DNA polymerase processivity factor (BMRF1), reduces the level of certain EBV glycoproteins, and inhibits viral transcription (30).
Animal studies: maribavir
Pharmacokinetic studies in rats and monkeys showed that the oral bioavailability of maribavir was up to 92% in rats and up to 58% in monkeys (31). The primary pathway of clearance involves the enterohepatic circulation with biliary excretion.
Maribavir was evaluated in two SCID mouse models; human fetal retina was implanted into the anterior chamber of the eye and human thymus/liver tissue was implanted under the kidney capsule (32). The implants were inoculated with CMV and maribavir therapy resulted in a 4-fold reduction in virus replication at 21 days in the retina and a 30 to 3000-fold reduction at 28 days in the thymus/liver tissue compared with a vehicle control.
Clinical Studies: maribavir
Two phase 1 single dose-escalation trials with maribavir were conducted in healthy volunteers and in HIV-infected men. No major safety concerns, including renal toxicity or myelosuppression, were observed. The most frequently reported adverse events were headache (53%) and taste disturbance (80%) (33, 34). A phase 1, randomized, dose-escalation study was conducted with HIV-1-infected men who had asymptomatic CMV shedding. Maribavir was active at all of the dose regimens tested, and the mean reduction in semen CMV titers ranged from 2.9 to 3.7 log 10 PFU/ml on day 28 of treatment compared to placebo (33).
A phase 2, multicenter, randomized, double-blind, placebo-controlled, dose-ranging study was performed over a 12 week period in allogeneic stem cell transplant recipients for the prevention of CMV infection (35). The incidence of CMV infection, based on detection of CMV DNA in plasma, was significantly lower in each of the 3 maribavir dose groups (100 mg bid, 400 mg qd, or 400 mg bid) than with placebo. In an intent-to-treat analysis during the first 100 days after transplant, the number of subjects who required pre-emptive anti-CMV therapy was significantly reduced with maribavir compared to placebo. In addition, 3 cases of CMV disease were diagnosed in patients receiving placebo, while none occurred in patients receiving maribavir. The most common adverse events were taste disturbance, nausea, and vomiting. Unlike ganciclovir, no reductions in neutrophil or platelet counts were noted.
A phase 3 trial was performed in North America and Europe to evaluate the prophylactic use of maribavir (100 mg bid) for prevention of CMV disease in allogeneic stem cell transplant recipients. In February 2009, Viropharma announced that the Phase III study failed to achieve the primary endpoint, a statistically significant reduction in CMV disease in the maribavir versus placebo group (http://www.fiercebiotech.com/press-releases/viropharma-incorporated-vphm-reports-results-phase-3-clinical-trial-maribavir-bone-ma).
In 2007, a phase 3 study evaluating maribavir (100 mg orally twice daily) as prophylaxis against CMV disease in liver transplant recipients was initiated. Two years later, after the results of the phase 3 study in stem cell transplant recipients were released, the liver transplant recipient study was discontinued after the rate of viremia in the maribavir and oral ganciclovir treatment arms was reviewed by the data safety monitoring committee (http://www.drugs.com/news/viropharma-announces-discontinuation-maribavir-phase-3-study-liver-transplant-patients-16168.html). The future state of the development of maribavir is currently unknown.
ST-246
ST-246, 4-trifluoromethyl-N-(3,3a,4,4a,5,5a,6,6a-octahydro-1,3-dioxo-4,6-ethenocycloprop[f]isoindol-2(1H)-yl)-benzamide (Figure 1G), was identified by a high throughput screening assay to find compounds that inhibit the cytopathic effects of poxviruses (Fig 1) (36). ST-246 inhibits the replication of orthopoxviruses, including smallpox, vaccinia, and monkeypox viruses with EC50 values of 0.01–0.02 uM. ST-246 has no significant activity against herpesviruses (36). ST-246 targets the V061 gene of cowpox virus (36), which is the homolog of vaccinia virus F13L. This gene is conserved among the orthopoxviruses and encodes an envelope protein that is necessary for formation of extracellular virions. Cowpox virus resistant to ST-246 can be isolated in vitro.
Animal studies: ST-246
Oral ST-246 protected healthy mice from a lethal intranasal challenge with vaccinia virus (36). The drug was started the day of the virus challenge. ST-246 reduced spread of virus to the lungs, blood, spleen, liver, and brain of mice inoculated intranasally (37). While ST-246 protected all mice from death when given 3 days after intranasal inoculation with a lethal dose of vaccinia virus, most of the animals died when the drug was begun 4 days after virus inoculation. ST-246 was synergistic with CMX-001 in enhancing survival in a mouse model of cowpox virus; while mice treated 6 days after infection with either ST-246 or CMX-001 all died, mice treated with the combination of drugs had improved survival (38). ST-246 also protected healthy mice from lethal challenge with ectromelia virus (36). Nude mice and SCID mice given oral ST-246 at the time of infection had prolonged survival (but all mice subsequently died of infection) after lethal intranasal challenge with vaccinia virus (39).
Rabbits receiving daily oral ST-246 one hour after a lethal dose of aerosolized rabbitpox virus, all survived infection; when the treatment was begun 1, 2, 3 or 4 days after the virus, the survival rates were 88%, 100%, 67%, and 33% respectively (40). Ground squirrels that received a lethal dose of monkeypox virus followed by oral ST-246 on days 0 to 3 after infection all survived, while only 67% of those treated on day 4 survived (41).
ST-246 protected cynomolgus monkeys from death when begun on the day of, or the day after, a lethal intravenous challenge with smallpox virus and resulted in lower levels of virus in the blood compared with untreated animals (42). Cynomolgus monkeys that received ST-246 1 or 3 days after inoculation with a lethal intravenous dose of monkeypox virus also survived infection and had lower viral loads than untreated animals (42).
Clinical Studies: ST-246
A phase I, double-blind, randomized placebo-controlled trial of single oral dosing of ST-246 in healthy adults showed no drug-related adverse events (43). ST-246 reached plasma levels that were comparable to those achieved in monkeys protected from poxvirus challenges. The results of a phase 1, multiple-dose, safety, tolerability, and pharmacokinetics 21 day trial in healthy volunteers showed that ST-246 was well tolerated with no serious adverse events (44). The results of a larger phase II study evaluating the safety and pharmacokinetics of 2 different doses of ST-246 compared to placebo are pending (www.clinicaltrials.gov).
Two patients who received ST-246 for compassionate use to treat complications after smallpox vaccination have been reported. A 28 month-old child developed severe eczema vaccinatum after contact with a vaccinee and received vaccinia immune globulin, cidfovir, and ST-246 initiated at 5mg/kg by nasogastric tube for 2 weeks (45). The patient had a number of complications, but ultimately survived and developed antibody to vaccinia. It is not known which treatment or combination of treatments contributed to the good outcome or if the development of antibody to vaccinia was responsible alone. A 20 year-old man with progressive vaccinia after receiving smallpox vaccine was treated with vaccinia immune globulin, oral ST-246, topical (1%) ST-246, and CMX-001 and survived (14).
GS-9191
GS-9191 (L-phenylalanine,N,N′-[[[2-[2-amino-6-(cyclopropylamino)-9H-purin-9-yl] ethoxy]methyl]phosphinylidene]bis-, bis(2-methylpropyl) ester)(Figure 1H)is the prodrug of 9-(2-phosphonylmethoxyethyl)guanine(PMEG) (46). GS-9191 permeates skin and results in accumulation of PMEG-diphosphate (the active metabolite of PMEG) in cells. GS-9191 has an EC50 of 0.03 nM to 1.8 nM for its antiproliferative effects on HPV-transformed cervical carcinoma cell lines; in contrast, cidofovir has EC50s of ≥3,100 nM for these cells. GS-9191 has an EC50 of 5.0 to 15 nM for HPV-negative carcinoma cell lines, and an EC50 of 0.98 to 7.44 nM for primary human cells (46).
PMEG is metabolized to PMEG-diphosphate which inhibits DNA polymerases alpha, beta, delta, and epsilon and reduces growth of transformed cells. PMEG-diphosphate results in chain termination of the cellular polymerase (47), inhibition of cellular DNA synthesis, and apoptosis (46).
Animal Studies: GS9191
Topical application of GS-9191 (0.1%) for 48 weeks to rabbits with papillomas due to cottontail rabbit papillomavirus reduced the size of the papillomas by >70%; in contrast, topical cidofovir (0.5%) reduced the size by 34% (46). Four of 5 animals treated with 0.1% GS-9191 had complete resolution of visible papillomas and none of the 4 had recurrences 1 month after treatment was stopped. Topical GS-9191 (0.1%) resulted in irritation at the application site in some rabbits; this apparently resolved when the drug was held for a few days. No systemic signs of toxicity were observed in rabbits.
Clinical Studies: GS-9191
A phase 1, randomized, double-blind, placebo-controlled study assessing the tolerability and activity of topical GS-9191 (in doses ranging up to 1%) for treatment of external genital and perianal warts was recently completed (www.clinicaltrials.gov); no information is available on the results.
CLEVUDINE
Clevudine, 1-[2-deoxy-2-fluoro-B-L-arabinofuranosyl]-5-methyluracil (Figure 1I), is a thymidine nucleoside analog with an unnatural L-configuration that exhibits lower toxicity (less myelopsuppression and neurotoxicity) compared to its D-isomer counterpart. Clevudine has potent activity against HBV and EBV in vitro and in vivo (48). The EC50 of clevudine was 0.1 μM for HBV in a human hepatoma cell line transfected with the HBV genome and 5 μM for EBV in an EBV-positive Burkett lymphoma cell line. In cells transiently transfected with HBV DNA, clevudine is 4 to 10 fold more active than emtricitabine, lamivudine, and adefovir; entecavir is the most active. The EC50 for clevudine is 0.053 μM, for emtricitabine 0.24 μM, for lamivudine 0.56 μM, for adefovir 0.58 μM, and for entecavir 0.0004 μM (49). Clevudine is not active against most strains of lamivudine-resistant HBV and has no activity against HSV (48). Clevudine is phosphorylated by a cellular protein kinase to clevudine 5′-triphosphate which inhibits the HBV DNA polymerase.
Animal studies: clevudine
In vivo efficacy studies have been conducted in woodchuck and duck hepatitis virus models. A 28 day dose escalation study in woodchucks infected with woodchuck hepatitis virus, showed an 8 log10 fold reduction in viral DNA levels by 28 days in woodchucks receiving the highest dose of clevudine (10 mg/kg/day) (50). A dose-dependent decrease in woodchuck hepatitis virus replicative intermediates was noted. In addition, an average 10-fold decrease in the levels of covalently closed circular DNA (cccDNA) was observed. The sustained antiviral effects after withdrawal of clevudine correlated with the reduction in cccDNA (51). Duck hepatitis virus-infected animals had rebound viremia after short courses (4 days) of clevudine therapy, but no rebound during the 2 week post-treatment course after 8 days of drug therapy (52).
Clinical Studies: clevudine
Multiple phase II and phase III studies conducted in Asia, Europe, and the United States have shown that clevudine has potent activity against HBV, resulting in significant reduction of the HBV DNA load (about a 3 to 4 log10 decrease) and improvement in ALT in chronically infected patients (53). Clevudine is unlike the other nucleoside analogs already approved for treatment of chronic HBV infection in that it produces a sustained antiviral effect and biochemical improvement up to at least 6 months after discontinuation (53, 54). This sustained antiviral effect is hypothesized to arise because of the ability of clevudine to reduce cccDNA levels, the source of viral replication in the liver.
The QUASH studies were multicenter, randomized, double-blind, active control clinical trials evaluating the long-term safety and efficacy of clevudine compared with adefovir in nucleoside treatment-naïve patients with chronic HBV infection (www.clinicaltrials.gov). These studies were voluntarily terminated by the sponsor when it became aware of cases of severe myopathy occurring in patients on long term-therapy with clevudine. In recent reports of long-term therapy with clevudine, patients have presented with severe skeletal myopathy with muscle biopsies showing severe myonecrosis and evidence of mitochondrial DNA depletion (55, 56). Accumulation of intracellular clevudine-triphosphate after prolonged administration of the drug may explain the late onset of this toxicity and the lag in viral rebound after treatment is stopped. The further development of clevudine for regulatory approval for the treatment of HBV has been halted in the United States, because of concerns regarding myopathy.
EMTRICITABINE
Emtricitabine, 2′, 3′-dideoxy-5-fluro-3′-thiacytidine (Figure 1J), is an analog of cytidine that is structurally similar to lamivudine and differs only by the presence of fluorine at position 5 of the pyrimidine ring. It is FDA-approved for the treatment of HIV infection in combination with other antiretroviral agents.
Emtricitabine has activity against both HIV and HBV. Because of similarity in structure to lamivudine, both compounds have similar resistance profiles. With the exception of a longer half-life, emtricitabine does not confer significant advantages over lamivudine. Like other nucleoside analogs, emtricitabine is a prodrug that is phosphorylated by cellular kinases to its active triphosphate, which inhibits the HBV RNA-dependent DNA polymerase. Emtricitabine effectively inhibits the replication of wild-type HBV in HBV DNA transfected cells with an EC50 of 0.24 μM and is twice as potent in this assay as lamivudine (EC50 of 0.56 μM) (49). Emtricitadine was effective only against one of four lamivudine-resistant HBV mutants tested (49).
Animal studies
In a placebo-controlled study of woodchucks chronically infected with woodchuck hepatitis virus, emtricitabine significantly reduced viremia (at least a 3 log10 decrease at higher doses) and intrahepatic virus replication in a dose-dependent manner (57). No drug-related toxicity was observed. In a recent study evaluating the antiviral efficacy of various combinations of nucleoside/nucleotide analogs, emtricitabine and tenofovir was one of the most effective combinations and suppressed woodchuck hepatitis virus replication in the blood by 6.1 log10 genome equivalents/ml in chronically infected animals (58).
Clinical Studies
Clinical trials of nucleoside analogs for the treatment of chronic HBV infection have demonstrated that suppression of HBV DNA is associated with improvement in disease (59). Gish et al. conducted a phase II, randomized, double-blind study to evaluate the safety and efficacy of different doses of emtricitabine given once daily to patients with chronic HBV infection (60). After 48 weeks of treatment, 53% of patients had a serum HBV DNA load ≤ 3.7 log10 copies/ml compared to a median baseline of 7.6 log10 copies/ml. After therapy, 85% of patients had a normal ALT and, of those patients who were HBeAg positive, 33% seroconverted to anti-HBe. A second placebo-controlled study evaluating the antiviral potency of emtricitabine in patients chronically infected with HBV revealed that 48 weeks of emtricitabine treatment resulted in significant histologic, virologic, and biochemical improvement (61). Emtricitabine was well-tolerated in both studies.
Resistance to emtricitabine developed in 13 to 18% of patients in these studies. Emtricitabine selects for mutations in the HBV polymerase, similar to those seen with lamivudine. A major goal of new approaches for the treatment of chronic HBV infection is to prevent the development of resistance. For example, an ongoing phase II study of tenofovir alone versus tenofovir with emtricitabine will assess the relative efficacy and safety of combination versus monotherapy in chronic HBeAg positive and negative patients (www.clinicaltrials.gov).
BROAD SPECTRUM ANTIVIRAL COMPOUNDS
Two recent reports describe compounds that have broad anti-viral activities. Phosphatidylserine translocates from the inner leaflet of the plasma membrane to the outer surface of the plasma membrane during apoptosis or cell activation, which occurs during many virus infections. A mouse monoclonal antibody, bavituximab, crosslinks phosphatidylserine-binding plasma protein (beta-2 glycoprotein I) bound to phosphatidylserine on cell membranes (62). Bavituximab bound to cells infected with arenavirus (Pichinde virus which is a model for Lassa fever virus) and to the arenavirus itself. Bavituximab improved survival of guinea pigs infected with a lethal dose of Pichinde virus and already showing evidence of disease. Bavituximab induced antibody-dependent cellular cytotoxicity of virus-infected cells and opsonization and clearance of virus from the blood. Bavituximab bound to cells infected with influenza, vaccinia virus, vesicular stomatitis virus, and murine cytomegalovirus, and protected mice from fatal infection with murine cytomegalovirus. Bavituximab has been tested in clinical trials for chronic hepatitis C.
LJ001 is an aryl methyldiene rhodanine derivative identified by high throughput screening for inhibitors of Nipah virus (63). LJ001 intercalates into the virus membrane, and inactivates the virus, preventing it from entering cells. The drug inhibited fusion of virions with the cell, but not cell-to-cell fusion. LJ001 inhibits the replication of enveloped viruses (e.g. Nipah, Ebola, Marburg, influenza, parinfluenza, HIV, hepatitis C, and vaccinia virus), but not nonenveloped viruses (e.g. adenovirus, coxsackievirus). Pre-treatment of Ebola and Rift Valley fever with LJ001 inactivated the viruses so that they prevented or reduced fatal disease in mice. Once daily injections of LJ001 did not protect animals from a lethal challenge with Ebola virus and changes will be needed to improve the pharmacokinetics of the drug.
CONCLUSION
Promising new drugs for the treatment of a variety of dsDNA virus infections are on the horizon. Many of these drugs have targets other than the viral DNA polymerase and have been tested or are being tested in phase II clinical trials. Their contribution to the armamentarium of antivirals should provide new treatment options for a variety of dsDNA viral infections for which no effective therapy is available.
Footnotes
CONFLICTS OF INTEREST
J.I.C. has a collaborative research agreement with Chimerix which provides CMX001 for in vitro testing.
References
- 1.Beadle JR, et al. Alkoxyalkyl esters of cidofovir and cyclic cidofovir exhibit multiple log enhancement of antiviral activity against cytomegalovirus and herpes virus replication in vitro. Antimicrob Agents Chemother. 2002;46:2381–2386. doi: 10.1128/AAC.46.8.2381-2386.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Huggins JW, Baker RO, Beadle JR, Hostetler KY. Orally active ether lipid prodrugs of cidofovir for the treatment of smallpox. Antiviral Res. 2002;53 (A66):104. [Google Scholar]
- 3.Kern ER, et al. Enhanced inhibition of orthopoxvirus replication in vitro by alkoxyalkyl esters of cidofovir and cyclic cidofovir. Antimicrob Agents Chemother. 2002;46:991–995. doi: 10.1128/AAC.46.4.991-995.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Williams-Aziz SL, et al. Comparative activities of lipid esters of cidofovir anc cyclic cidofovir against replication of herpesviruses in vitro. Antimicrob Agents Chemother. 2005;49:3724–3733. doi: 10.1128/AAC.49.9.3724-3733.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Randhawa P, Farasati NA, Shapiro R, Hostetler KY. Ether lipid ester derivatives of cidofovir inhibit polyomavirus BK replication in vitro. Antimicrob Agents Chem. 2006;50:1564–1566. doi: 10.1128/AAC.50.4.1564-1566.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hartline CB, et al. Ether lipid-ester prodrugs of acyclic nucleoside phosphonates: activity against adenovirus replication in vitro. J Infect Dis. 2005;191:396–399. doi: 10.1086/426831. [DOI] [PubMed] [Google Scholar]
- 7.Hostetler KY, Rought S, Aldern KA, Trahan J, Beadle JR, Corbeil J. Enhanced antiproliferative effects of alkoxyalkyl esters of cidofovir in human cervical cancer cells in vitro. Mol Cancer Ther. 2006;5:156–159. doi: 10.1158/1535-7163.MCT-05-0200. [DOI] [PubMed] [Google Scholar]
- 8.Quenelle DC, Collins DJ, Hostetler KY, Beadle JR, Wan WB, Kern ER. Oral treatment of cowpox and vaccinia infections in mice with ether lipid esters of cidofovir. Antimicrob Agents Chemother. 2004;48:404–412. doi: 10.1128/AAC.48.2.404-412.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Buller RM, Owens G, Schriewer J, Melman L, Beadle JR, Hostetler KY. Efficacy oral active ether lipid analogs of cidofovir in lethal mousepox model. Virology. 2004;318:474–481. doi: 10.1016/j.virol.2003.11.015. [DOI] [PubMed] [Google Scholar]
- 10.Adams MM, Rice AD, Moyer RW. Rabbitpox virus and vaccinia virus infection of rabbits as a model for human smallpox. J Virol. 2007;81:11084–11095. doi: 10.1128/JVI.00423-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bidanset DJ, Beadle JR, Wan WB, Hostetler KY, Kern ER. Oral activity of ether lipid prodrugs of cidofovir against experimental human cytomegalovirus infection. J Infect Dis. 2004;190:499–503. doi: 10.1086/421912. [DOI] [PubMed] [Google Scholar]
- 12.Toth K, et al. Hexadecyloxypropyl-cidofovir, CMX001, prevents adenovirus-induced mortality in a permissive, immunosuppressed animal model. PNAS. 105:7293–7297. doi: 10.1073/pnas.0800200105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Robertson A, et al. Safety and pharmacokinetic analysis of CMX001; results from a FTIH dose escalation study (CMX001-102). IDSA Annual Meeting; October 2009. [Google Scholar]
- 14.Centers for Disease Control and Prevention. Progressive vaccinia in a military smallpox vaccinee–United States, 2009. Morb Mortal Wkly Rep. 2009;58:532–536. [PubMed] [Google Scholar]
- 15.Crute JJ, et al. Herpes simplex virus helicase-primase inhibitors are active in animal models of human disease. Nat Med. 2002;8:386–391. doi: 10.1038/nm0402-386. [DOI] [PubMed] [Google Scholar]
- 16.Kleymann G, et al. New helicase-primase inhibitors as drug candidates for the treatment of herpes simplex disease. Nat Med. 2002;8:392–398. doi: 10.1038/nm0402-392. [DOI] [PubMed] [Google Scholar]
- 17.Chono K, et al. ASP2151, a novel helicase-primase inhibitor, possesses antiviral activity against varicella-zoster virus and herpes simplex virus types 1 and 2. Journal Antimicrobial Chemotherapy. 2010 doi: 10.1093/jac/dkq198. in press. [DOI] [PubMed] [Google Scholar]
- 18.Betz UA, Fischer R, Kleymann G, Hendrix M, Rübsamen-Waigmann H. Potent in vivo antiviral activity of the herpes simplex virus primase-helicase inhibitor BAY 57-1293. Antimicrob Agents Chemother. 2002;46:1766–1772. doi: 10.1128/AAC.46.6.1766-1772.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Biswas S, Swift M, Field HJ. High frequency of spontaneous helicase-primase inhibitor (BAY 57-1293) drug-resistant variants in certain laboratory isolates of HSV-1. Antivir Chem Chemother. 2007;18:13–23. doi: 10.1177/095632020701800102. [DOI] [PubMed] [Google Scholar]
- 20.Baumeister J, Fischer R, Eckenberg P, Henninger K, Ruebsamen-Waigmann H, Kleymann G. Superior efficacy of helicase-primase inhibitor BAY 57-1293 for herpes infection and latency in the guinea pig model of human genital herpes disease. Antivir Chem Chemother. 2007;18:35–48. doi: 10.1177/095632020701800104. [DOI] [PubMed] [Google Scholar]
- 21.Kaufman HE, et al. Efficacy of a helicase-primase inhibitor in animal models of ocular herpes simplex virus type 1 infection. J Ocul Pharmacol Ther. 2008;24:34–42. doi: 10.1089/jop.2007.0084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Duan J, et al. Oral bioavailability and in vivo efficacy of the helicase-primase inhibitor BILS 45 BS against acyclovir-resistant herpes simplex virus type 1. Antimicrob Agents Chemother. 2003;47:1798–1804. doi: 10.1128/AAC.47.6.1798-1804.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Katsumata K, Chono K, Kontani T, Sudo K, Shimizu Y, Suzuki H. Effect of acute oral treatment with ASP2151 or valacyclovir (VACV) against cutaneous infection with herpes simplex virus (HSV) type 1 in mice. 49th Interscience Conference on Antimicrobial Agents and Chemotherapy; San Francisco, CA. Sept 12–15, 2009; p. Abstract V-1742. [Google Scholar]
- 24.McGuigan C, et al. Preclinical development of bicyclic nucleoside analogues as potent and selective inhibitors of varicella zoster virus. J Antimicrob Chemother. 2007;60:1316–1330. doi: 10.1093/jac/dkm376. [DOI] [PubMed] [Google Scholar]
- 25.Matson M, Pentikis H, Boehlecke B, Wenzel E, Henson G, Morris A. A study of the safety and pharmacokinetics of multiple ascending Doses of FV-100 in healthy subjects (abstract) Antiviral Research. 2009;82:A49. [Google Scholar]
- 26.Biron KK, et al. Potent and selective inhibition of human cytomegalovirus replication by 1263W94, a benzimidazole L-riboside with a unique mode of action. Antimicrob Agents Chemother. 2002;46:2365–2372. doi: 10.1128/AAC.46.8.2365-2372.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Williams SL, et al. In vitro activities of benzimidazole D- and L-ribonucleosides against herpesviruses. Antimicrob Agents Chemother. 2003;47:2186–2192. doi: 10.1128/AAC.47.7.2186-2192.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Drew WL, et al. Maribavir sensitivity of cytomegalovirus isolates resistant to ganciclovir, cidofovir or foscarnet. J Clin Virol. 2006;37:124–127. doi: 10.1016/j.jcv.2006.07.010. [DOI] [PubMed] [Google Scholar]
- 29.Chou S, et al. Mutations in the human cytomegalovirus UL27 gene that confer resistance to maribavir. J Virol. 2004;78:7124–7130. doi: 10.1128/JVI.78.13.7124-7130.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Wang F-Z, et al. Maribavir Inhibits Epstein-Barr Virus Transcription in Addition to Viral DNA Replication. J Virol. 2009;83:12108–12117. doi: 10.1128/JVI.01575-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Koszalka GW, et al. Preclinical and toxicology studies of 1263W94, a potent and selective inhibitor of human cytomegalovirus replication. Antimicrob Agents Chemother. 2002;46:2373–2380. doi: 10.1128/AAC.46.8.2373-2380.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kern ER, et al. Activities of benzimidazole D- and L-ribonucleosides in animal models of cytomegalovirus infections. Antimicrob Agents Chemother. 2004;48:1749–1755. doi: 10.1128/AAC.48.5.1749-1755.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Lalezari JP, et al. Phase 1 dose escalation trial evaluating the pharmacokinetics, anti-human cytomegalovirus (HCMV) activity, and safety of 1263W94 in human immunodeficiency virus-infected men with asymptomatic HCMV shedding. Antimicrob Agents Chemother. 2002;46:2969–2976. doi: 10.1128/AAC.46.9.2969-2976.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Wang LH, et al. Phase I safety and pharmacokinetics trial of 1263W94, a novel oral anti-human cytomegalovirus agent, in healthy and human immunodeficiency virus-infected subjects. Antimicrob Agents Chemother. 2003;47:1334–1342. doi: 10.1128/AAC.47.4.1334-1342.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Winston DJ, et al. Maribavir prophylaxis for prevention of cytogemalovirus infection in allogeneic stem cell transplant recipients: a multicenter, randomized, double-blind, placebo-controlled, dose-ranging study. Blood. 2008;111:5403–5410. doi: 10.1182/blood-2007-11-121558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Yang G, et al. An orally bioavailable antipoxvirus compound (ST-246) inhibits extracellular virus formation and protects mice from lethal orthopoxvirus challenge. J Virol. 2005;79:13139–13149. doi: 10.1128/JVI.79.20.13139-13149.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Berhanu A, et al. ST-246 inhibits in vivo poxvirus dissemination, virus shedding, and systemic disease manifestation. Antimicrob, Agents Chemother. 2009;53:4999–5009. doi: 10.1128/AAC.00678-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Quenelle DC, et al. Synergistic efficacy of the combination of ST-246 with CMX001 against orthopoxviruses. Antimicrob Agents Chemother. 2007;51:4118–4124. doi: 10.1128/AAC.00762-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Grosenbach DW, et al. Efficacy of ST-246 versus lethal poxvirus challenge in immunodeficient mice. Proc Natl Acad Sci U S A. 2010;107:838–843. doi: 10.1073/pnas.0912134107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Nalca A, et al. Evaluation of orally delivered ST-246 as postexposure prophylactic and antiviral therapeutic in an aerosolized rabbitpox rabbit model. Antiviral Res. 2008;79:121–127. doi: 10.1016/j.antiviral.2008.03.005. [DOI] [PubMed] [Google Scholar]
- 41.Sbrana E, et al. Efficacy of the antipoxvirus compound ST-246 for treatment of severe orthopoxvirus infection. Am J Trop Med Hyg. 2007;76:768–773. [PubMed] [Google Scholar]
- 42.Huggins J, et al. Nonhuman primates are protected from smallpox virus or monkeypox virus challenges by the antiviral drug ST-246. Antimicrob Agents Chemother. 2009;53:2620–2625. doi: 10.1128/AAC.00021-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Jordan R, et al. Single-dose safety and pharmacokinetics of ST-246, a novel orthopoxvirus egress inhibitor. Antimicrob Agents Chemother. 2008;52:1721–1727. doi: 10.1128/AAC.01303-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Jordan R, et al. Safety and pharmacokinetics of the antiorthopoxvirus compound ST-246 following repeat oral dosing in healthy adult subjects. Antimicrob Agents Chemother. 2010;54:2560–2566. doi: 10.1128/AAC.01689-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Vora S, et al. Severe eczema vaccinatum in a household contact of a smallpox vaccinee. Clin Infect Dis. 2008;46:1555–1561. doi: 10.1086/587668. [DOI] [PubMed] [Google Scholar]
- 46.Wolfgang GH, et al. GS-9191 is a novel topical prodrug of the nucleotide analog 9-(2-phosphonylmethoxyethyl)guanine with antiproliferative activity and possible utility in the treatment of human papillomavirus lesions. Antimicrob Agents Chemother. 2009;53:2777–2784. doi: 10.1128/AAC.00103-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Holý A, et al. Acyclic nucleotide analogues: synthesis, antiviral activity and inhibitory effects on some cellular and virus-encoded enzymes in vitro. Antiviral Res. 1990;13:295–311. doi: 10.1016/0166-3542(90)90014-x. [DOI] [PubMed] [Google Scholar]
- 48.Chu CK, et al. Use of 2-fluoro-5-methyl-β-L-arabinofuranosyluracil as a novel antiviral agent for hepatitis B virus and Epstein-Barr virus. Antimicrob Agents Chemother. 1995;39:979–981. doi: 10.1128/aac.39.4.979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Ono SK, et al. The polymerase L528M mutation cooperates with nucleotide binding-site mutations, increasing hepatitis B virus replication and drug resistance. J Clin Invest. 2001;107:449–455. doi: 10.1172/JCI11100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Chu CK, et al. Preclinical investigation of L-FMAU as an anti-hepatitis B agent. Antivir Ther. 1998;3(suppl 3):113–121. [PubMed] [Google Scholar]
- 51.Peek SF, et al. Antiviral activity of clevudine [L-FMAU, (1-(2-fluoro-5-methyl-beta, L-arabinofuranosyl) uracil)] against woodchuck hepatitis virus replication and gene expression in chronically infected woodchucks (Marmota monax) Hepatology. 2001;33:254–266. doi: 10.1053/jhep.2001.20899. [DOI] [PubMed] [Google Scholar]
- 52.Aguesse-Germon S, et al. Inhibitory effect of 2′-fluoro-5-methyl-beta-L-arabinofuranosyl-uracil on duck hepatitis B virus replication. Antimicrob Agents Chemother. 1998;42:369–376. doi: 10.1128/aac.42.2.369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Korba BE, Furman PA, Otto MJ. Clevudine: a potent inhibitor of hepatitis B virus in vitro and in vivo. Expert Rev Anti Infect Ther. 2006;4:549–561. doi: 10.1586/14787210.4.4.549. [DOI] [PubMed] [Google Scholar]
- 54.Marcellin P, et al. A phase II dose-escalating trial of clevudine in patients with chronic hepatitis B. Hepatology. 2004;40:140–148. doi: 10.1002/hep.20257. [DOI] [PubMed] [Google Scholar]
- 55.Fleischer RD, Lok ASF. Myopathy and neuropathy associated with nucleos(ti)de analog therapy for hepatitis B. J Hepatology. 2009;51:787–791. doi: 10.1016/j.jhep.2009.06.011. [DOI] [PubMed] [Google Scholar]
- 56.Seok JI, et al. Long-term therapy with clevudine for chronic hepatitis B can be associated with myopathy characterized by depletion of mitochondrial DNA. Hepatology. 2009;49:2080–2086. doi: 10.1002/hep.22959. [DOI] [PubMed] [Google Scholar]
- 57.Korba BE, Schinazi RF, Cote P, Tennant BC, Gerin JL. Effect of oral administration of emtricitabine on woodchuck hepatitis virus replication in chronically infected woodchucks. Antimicrob Agents Chemother. 2000;44:1757–1760. doi: 10.1128/aac.44.6.1757-1760.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Menne S, et al. Antiviral effects of lamivudine, emtricitabine, adefovir dipivoxil, and tenofovir disoproxil fumarate administered orally alone and in combination to woodchucks with chronic woodchuck hepatitis virus infection. Antimicrob Agents Chemother. 2008;52:3617–3632. doi: 10.1128/AAC.00654-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Dienstag JL, et al. Hepatitis B virus infection. N Engl J Med. 2008;359:1486–1500. doi: 10.1056/NEJMra0801644. [DOI] [PubMed] [Google Scholar]
- 60.Gish RG, et al. Safety and antiviral activity of emtricitabine (FTC) for the treatment of chronic hepatitis B infection: a two-year study. J Hepatol. 2005;43:60–66. doi: 10.1016/j.jhep.2005.02.017. [DOI] [PubMed] [Google Scholar]
- 61.Lim SG, et al. A double-blind placebo-controlled study of emtricitabine in chronic hepatitis B. Arch Intern Med. 2006;166:49–56. doi: 10.1001/archinte.166.1.49. [DOI] [PubMed] [Google Scholar]
- 62.Soares MM, King SW, Thorpe PE. Targeting inside-out phosphatidylserine as a therapeutic strategy for viral diseases. Nat Med. 2008;14:1357–1362. doi: 10.1038/nm.1885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Wolf MC, et al. A broad-spectrum antiviral targeting entry of enveloped viruses. Proc Natl Acad Sci U S A. 2010;107:3157–3162. doi: 10.1073/pnas.0909587107. [DOI] [PMC free article] [PubMed] [Google Scholar]