Abstract
We report a 40 year old woman admitted with an acute abdomen. Investigations revealed pancreatitis, bilateral pleural effusion, renal failure, disseminated intravascular coagulation, and scrub IgM ELISA and dengue NS1 positivity. She improved with azithromycin and appropriate pain and fluid management. She also developed central venous catheter-related MRSA sepsis that was managed in the hospital.
Keywords: scrub typhus pancreatitis, dengue, gastrointestinal manifestations
Introduction
Tropical infections due to dengue, leptospira, salmonella and parasites causing acute pancreatitis have been reported [1]. Scrub typhus is a widespread zoonotic disease with a high prevalence in Southeast Asia [2]. In South India it is estimated that 40 to 50% of cases of undiagnosed acute febrile illness are attributable to scrub typhus [3]. We report a rare case of pancreatitis caused by co-infection of scrub typhus and dengue in a 40 year old farm labourer.
Case
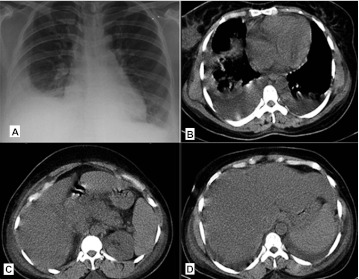
This woman presented with four days’ of epigastric abdominal pain and fever. At admission she was febrile (103F), tachycardic (105/min), tachypneic (25/min) and had pedal edema, right pleural effusion, distended abdomen, hepatosplenomegaly and absent bowel sounds. Fluid resuscitation after jugular central venous (CV) catheter placement and empirical cefoperazone-sulbactum was administered pending investigations. Her tests showed leucocytosis, thrombocytopenia (Table 1), interstitial pneumonitis with right sided pleural effusion on chest radiograph (Figure 1) and bilateral effusion with right-sided pneumonitis, hepatosplenomegaly and bulky pancreas on computed tomography (Figure 1B, 1C, 1D). Her scrub IgM Elisa, Weil-Felix test (OX:K titre 1:80) and dengue IgM were positive, while dengue IgG, leptospira IgM, malarial antigens and smear, HIV, HBsAg, AntiHCV, antinuclear antibody and ds-DNA were negative. She did not recall being bitten by mosquitoes or mites, but in view of the high local prevalence of scrub typhus and the results of suggestive investigations, injectable azithromycin was also administered (due to renal failure and nil per oral status, doxycyline was not given). Her pleural fluid analysis was transudative-protein 2.2 g/dL, lactate dehydrogenase (LDH) 527 U/L, serum LDH 1000 U/L, with lymphocytosis (92% of 450 cells). She was kept nil per orally for ~48 hours after which she was gradually introduced to food with no worsening of symptoms. On day 6 she developed fever, and methicillin-resistant Staphylococcus aureus was isolated from the CV line blood culture. This was treated with 10 days of clindamycin prior to discharge (13th day of illness). The patient did not return for further follow-up and hence convalescent samples could not be obtained to satisfy diagnostic criteria on a serological basis for either disorder.
Table 1.
Investigations from day 3 to day 12 of the illness.
| Investigation | Normal range | Day 3 | Day 4 | Day 6 | Day 12 |
|---|---|---|---|---|---|
| Hemoglobin | 12–14 g/dL | 9.2 | 11.3 | 9.3 | 8.8 |
| Hematocrit | 37–45% | 34.3 | 28.3 | 27 | |
| Platelets | 150–450×109/L | 34 | 51 | 130 | |
| TLC | 4.5–9.5×109/L | 8.1 | 11.3 | 19.7 | 14.3 |
| Bilirubin | 3.42–18.81 µmol/L | 106.02 | 90.63 | 102.6 | 51.3 |
| Direct fraction | 1.7–6.8 µmol/L | 88.92 | 82.08 | 94.05 | 34.2 |
| AST | 0.17–0.68 µkat/L | 3.47 | 2.94 | 1.53 | |
| ALT | 0.17–0.51 µkat/L | 1.29 | 0.92 | 0.64 | |
| ALP | 0.5–2.0 µkat/L | 12.5 | 10.26 | ||
| Amylase | <90 U/L | 728 | 59 | ||
| Lipase | < 38 U/L | 156 | 25 | ||
| Urea | 2.5–7 mmol/L | 14.6 | 24.2 | 10.7 | |
| Creatinine | 44.2–80 µmol/L | 88.4 | 88.4 | 53.04 |
TLC-total leukocyte count; ALP-alkaline phosphatase; AST-aspartate aminotransferase; ALT-alanine aminotransferase
Fig. 1.
A: Chest radiograph showing bilateral interstitial infiltrates and right-sided pleural effusion
B: CT chest showing bilateral pleural effusion and right-sided pneumonitis
C: CT abdomen showing reduced pancreatic attenuation, fat stranding around tail, and free fluid in abdomen
D: CT abdomen showing hepatosplenomegaly and free fluid abdomen
Discussion
Trombiculid mites transmit Orientia tsutsugumashi, the causative organism of scrub typhus, by biting hosts and producing the formation of an eschar. Common symptoms include fever, headache, myalgia, exanthematous rash, generalized lymphadenopathy and pneumonia. Gastrointestinal manifestations include acute abdominal pain, gastric ulcers, hepatitis, jaundice, hematemesis, melena and hepatosplenomegaly [2, 4]. Rare manifestations are meningoencephalitis, acute respiratory distress syndrome, acute renal failure, disseminated intravascular coagulation and myocarditis [2, 5–6]. Pancreatitis with scrub typhus has been described on two occasions: one caused by scrub typhus alone and later complicated by pancreatic abscess with multiorgan failure [7], and the second as a co-infection with leptospirosis [8]. The second patient also had acute acalculous cholecystitis. In both cases, patients were successfully treated with doxycycline and ceftriaxone. To our knowledge, this is the first report of pancreatitis due to both scrub typhus and dengue. The mechanism of pancreatic involvement is unclear.
Dengue hemorrhagic fever can also present as acute abdomen as in scrub typhus with acalculous cholecyctitis [9], splenic rupture [10] and pancreatitis. Generally, dengue patients present with preceding fever of 2 to 7 days’ duration. In the case of scrub-related acute abdomen, patients present on day 1 as in our case [7]. In our patient, leucocytosis, interstitial infiltrates, elevated alkaline phosphatase, acute abdomen at onset, lack of hemoconcentration or bleeding diathesis and supportive results in a patient who came from an endemic area would suggest scrub typhus as the main contributing factor. Thrombocytopenia, bilateral pleural effusion, AST>ALT (aspartate and alanine transaminase) pattern of elevated transaminases may favor coexisting dengue infection. AST>ALT pattern can also be seen in scrub typhus, but it is generally associated with alkaline phosphatase elevations. Thrombocytopenia and leucocytosis would favor scrub [2], while bicytopenia is more commonly seen in dengue.
In conclusion, we report pancreatitis arising from coexisting acute febrile illnesses that are common in the tropics and subtropics. Health practitioners in endemic areas should be aware of unusual medical causes of acute abdomen namely, scrub typhus and dengue. Also co-infections should be considered in cases of infectious pancreatitis when the results of investigations do not fully justify a single aetiology.
Conflict of interest
None
References
- 1.Parenti DM, Steinberg W, Kang P. Infectious causes of acute pancreatitis. Pancreas 1996; 13(4): 356–371 [DOI] [PubMed] [Google Scholar]
- 2.Vivekanandan M, Mani A, Priya YS, Singh AP, Jayakumar S, Purty S. Outbreak of scrub typhus in Pondicherry. J Assoc Physicians India 2010; 58: 24–28 [PubMed] [Google Scholar]
- 3.Isaac R, Varghese GM, Mathai EJM, Joseph I. Scrub typhus: prevalence and diagnostic issues in rural Southern India. Clin Infect Dis 2004; 39(9): 1395–1396 [DOI] [PubMed] [Google Scholar]
- 4.Aung T, Supanaranond W, Phumiratanaprapin W, Phonrat B, Chinprasatsak S, Ratanajaratroj N. Gastrointestinal manifestations of septic patients with scrub typhus in Maharat Nakhon Ratchasima Hospital. Southeast Asian J Trop Med Public Health 2004; 35: 845–851 [PubMed] [Google Scholar]
- 5.Sittiwangkul R, Pongprot Y, Silviliarat S, Oberdorfer P, Jittamala P, Sirisanthana V. Acute fulminant myocarditis in scrub typhus. Ann Trop Paediatr 2008; 28(2): 149–154 [DOI] [PubMed] [Google Scholar]
- 6.Rathi N, Rathi A. Rickettsial infections: Indian perspective. Indian Pediatr 2010; 47(2): 157–164 [DOI] [PubMed] [Google Scholar]
- 7.Yi SY, Tae JH. Pancreatic abscess following scrub typhus associated with multiorgan failure. World J Gastroenterol 2007; 13(25): 3523–3525 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wang NC, Ni YH, Peng MY, Chang FY. Acute acalculous cholecystitis and pancreatitis in a patient with concomitant leptospirosis and scrub typhus. J Microbiol Immunol Infect 2003; 36(4): 285–287 [PubMed] [Google Scholar]
- 9.Khor BS, Liu JW, Lee IK, Yang KD. Dengue hemorrhagic fever patients with acute abdomen: clinical experience of 14 cases. Am J Trop Med Hyg 2006; 74(5): 901–904 [PubMed] [Google Scholar]
- 10.Seravali MR, Santos AH, Costa CE, Rangel DT, Valentim LF, Gonçalves RM. Spontaneous splenic rupture due to dengue fever: report of two cases. Braz J Infect Dis 2008; 12(6): 538–540 [DOI] [PubMed] [Google Scholar]