Abstract
Fibrosing mediastinitis is a rare, chronic inflammatory disease that has several implicated etiologies. We describe a case of a 41-year old woman who presented with the classic signs and symptoms of superior vena cava syndrome. Imaging revealed a diffuse infiltrative mediastinal process, which on biopsy was consistent with fibrosing mediastintis.
Key Words : Fibrosing mediastintis, superior vena cava (SVC) syndrome
Introduction
Fibrosing mediastintis, also known as sclerosing mediastinitis, is a rare disease characterized by diffuse fibrosis of the soft tissues of the mediastinum which can lead to significant morbidity secondary to obstruction of central structures. The pathogenesis is uncertain, but can be a consequence of granulomatous disease, most frequently histoplasmosis. Other contributing factors include tuberculosis, sarcoidosis, autoimmune and other fungal diseases.
Case report
A 41-year old diabetic, non-smoker presented with a 8 month history of progressive swelling of her face, neck and upper extremities. This was accompanied by headaches, distortion of vision, dizziness on bending over, facial flushing and occasional hemoptysis. Physical examination revealed the classic findings of superior vena cava obstruction with severe edema in the face and upper extremities, and obvious venous collateralization across the chest.
A chest computed tomography demonstrated a 5 cm × 5 cm × 6.5 cm diffuse infiltrative process within the anterior mediastinum, occluding the superior vena cava and extending into the right hilar and subcarinal region (Figure 1). This process engulfed the take-off of all the branch vessels of the aorta and truncus anterior. A Positron Emission Tomography (PET) did not demonstrate any abnormal hypermetabolism in the patient’s body.
Figure 1.
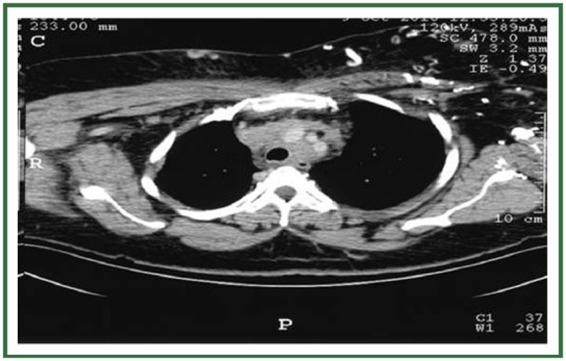
Diffuse infiltrative process (indicated by arrows) within the anterior mediastinum extending along the superior vena cava into the right hilar and subcarinal region with calcifications.
Laboratory tests including a panel of antibodies for autoimmune processes, immunohistochemistry analysis for lymphoma, fungal serology, sputum smears and cultures for acid fast bacilli were all negative. A mediastinoscopy was performed. Biopsy of the ‘rock hard’ mediastinal mass and paratracheal nodes was consistent with fragments of dense fibrous collagen and adipose tissue, with no evidence of malignancy. A pathology review at our institution was consistent with a diagnosis of fibrosing mediastintis.
A trial of itraconazole has been initiated and a superior vena cava stent has been placed via trans-jugular access (Figure 2). The patient’s severe edema and symptoms started to recede within a day of the interventional procedure.
Figure 2.

Trans-jugular passage of Kumpe catheter into the Superior Vena cava -- balloon angioplasty and placement of Viabahn covered stent.
Discussion
Fibrosing mediastintis, also known as sclerosing mediastinitis, is a rare disease characterized by accumulation and proliferation of dense acellular collagen and fibrous tissue. The process encases central structures in the mediastinum such as the superior vena cava, trachea, esophagus, pulmonary vasculature and nerves. Superior vena cava obstruction is the most frequent complication (1), but involvement of the pulmonary artery, phrenic nerve, recurrent laryngeal nerve, and pulmonary veins have also been reported (2). Involvement of the proximal coronary ostia with myocardial ischemia and infarction, has also been described (3). Cardiology consultation should be considered in patients with chest pain.
The pathogenesis of the disease still remains elusive. It has been seen in patients as young as 7 years of age (4). In patients with histoplasmosis, it has been postulated that prolonged seepage of some soluble antigen or other substance from the involved lymph nodes causes unchecked fibrosis (5).
CT and MR imaging techniques play a vital role in the diagnosis, work up and monitoring of the disease. They also play a vital role in guiding either surgical or percutaneous therapy by assessing the extent of mediastinal involvement (6). Biopsy samples obtained by percutaneous needle technique may be insufficient to rule out malignancy. Open biopsy with extensive sampling is frequently required to establish a definitive diagnosis and rule out other infiltrative lesions of the mediastinum, including lymphoma, carcinoma, and desmoid tumors (7,8).
Steroid therapy and use of antifungal agents are generally not useful in cases of extensive fibrosis (9). However, Inoue and colleagues suggest that the serum IgG4 level is a good selection indicator for steroid therapy in sclerosing mediastinitis (10). Most reports advocate minimal intervention unless symptoms become life- threatening (7).
The relief of superior vena cava syndrome is important in the palliative management of such a patient. Intravascular stents are a promising option for relief of non-neoplastic SVC obstruction (11). Restenosis of the stent is a frequent complication in patients with fibrosing mediastinitis. Short- and midterm success can be achieved, but progressive fibrosing mediastinitis remains a difficult clinical problem with repeat dilation of stents and/or additional stent placement necessary to maintain optimal stent patency and improvement in clinical symptomatology (12).
Acknowledgements
Disclosure: The authors declare no conflict of interest.
References
- 1.Mathisen DJ, Grillo HC. Clinical manifestation of mediastinal fibrosis and histoplasmosis. Ann Thorac Surg 1992;54:1053-7;discussion 1057-8 [DOI] [PubMed] [Google Scholar]
- 2.Fauci AS, Braunwald E, Fuselbacher KJ, et al. Harrison's principles of internal medicine 14th ed. 1998, 1476 McGraw Hill. San Francisco, CA. [Google Scholar]
- 3.Addatu DT, Jr, Tan HC. Fibrosingmediastinitis causing acute ostial left main myocardial infarction. J Invasive Cardiol 2010;22:456-60 [PubMed] [Google Scholar]
- 4.Shinkawa T, Nakajima M, Kishimoto T, et al. A case of idiopathic sclerosingmediastinitis in a 7-year-old Japanese boy. Eur J Pediatr 2005;164:302-5 [DOI] [PubMed] [Google Scholar]
- 5.Goodwin RA, Nickell JA, Des Prez RM. Mediastinal fibrosis complicating healed primary histoplasmosis and tuberculosis. Medicine (Baltimore) 1972;51:227-46 [DOI] [PubMed] [Google Scholar]
- 6.Rossi SE, McAdams HP, Rosado-de-Christenson ML, et al. Fibrosingmediastinitis. Radiographics 2001;21:737-57 [DOI] [PubMed] [Google Scholar]
- 7.Mole TM, Glover J, Sheppard MN. Sclerosingmediastinitis: a report on 18 cases. Thorax 1995;50:280-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Dunn EJ, Ulicny KS, Jr, Wright CB, et al. Surgical implications of sclerosingmediastinitis.A report of six cases and review of the literature. Chest 1990;97:338-46 [DOI] [PubMed] [Google Scholar]
- 9.Dines DE, Payne WS, Bernatz PE, et al. Mediastinal granuloma and fibrosingmediastinitis. Chest 1979;75:320-4 [DOI] [PubMed] [Google Scholar]
- 10.Inoue M, Nose N, Nishikawa H, et al. Successful treatment of sclerosingmediastinitis with a high serum IgG4 level. Gen ThoracCardiovascSurg 2007;55:431-3 [DOI] [PubMed] [Google Scholar]
- 11.Dodds GA, 3rd, Harrison JK, O'Laughlin MP, et al. Relief of superior vena cava syndrome due to fibrosingmediastinitis using the Palmaz stent. Chest 1994;106:315-8 [DOI] [PubMed] [Google Scholar]
- 12.Ferguson ME, Cabalka AK, Cetta F, et al. Results of intravascular stent placement for fibrosingmediastinitis. Congenit Heart Dis 2010;5:124-33 [DOI] [PubMed] [Google Scholar]


