Abstract
Synthetic oligonucleotides containing CpG motifs (CpG ODNs) have been shown to induce proliferation, differentiation and cytokine production in B cells, macrophages and DCs through a TLR9-dependent mechanism. A class (CpG-A) and B class (CpG-B) ODNs display distinct physical properties. CpG-A, but not CpG-B, can multimerize to form exceedingly large lattices. CpG-A cannot effectively activate B cells but does induce pDCs to produce high levels of IFNα, while CpG-B is a potent B cell mitogen. Here we report that CpG-A is internalized by B cells, and CpG-A and CpG-B accumulate to distinct intracellular compartments. When present in the form of an immune complex (CpG-A IC), CpG-A is taken up more efficiently by AM14 IgG2a-specific B cells, and elicits a robust TLR9-dependent B cell proliferative response. B cells proliferating comparably and in a TLR9-dependent fashion in response to CpG-A IC and CpG-B exhibited distinct cytokine profiles. CpG-A IC induced enhanced production of RANTES and markedly reduced levels of IL-6 when compared to CpG-B. We also found that engagement of the AM14 BCR by a protein IC, which cannot by itself induce proliferation, promoted TLR9-dependent but BCR-independent proliferation by bystander CpG-A or fragments of mammalian dsDNA. These data identify direct and indirect mechanisms by which BCR engagement facilitates access of exogenous ligands to TLR9-associated compartments and subsequent B cell activation.
Introduction
Synthetic oligonucleotides containing CpG motifs (CpG ODN) have been valuable tools for the study of TLR9 function in a diverse range of cell populations. There are two major categories of synthetic CpG ODN that elicit distinct functional outcomes as a result of TLR9 engagement, CpG class A (CpG-A) and CpG class B (CpG-B). CpG-A ODNs are generally 20–21 bases in length and incorporate a single CpG motif within a hairpin-forming palindrome phosphodiester region. CpG-A ODNs also routinely include phosphorothioate-stabilized G repeats at the 5’ and 3’ ends. In saline solutions these poly-G sequences participate in intermolecular salt bridges, leading to the formation of large molecular aggregates (1). By contrast, CpG-B ODNs incorporate one or more CpG motifs within a fully phosphorothioate backbone, and remain monomeric in saline solutions (1).
The two ODN classes have distinct functional properties. CpG-A ODNs induce IFNα production by pDCs, IFNγ production by NK cells and monocyte maturation into dendritic cells, but are poor inducers of B cell activation. CpG-B ODNs fail to induce pDC IFNα production but do trigger pDC expression of co-stimulatory molecules and TNFα production, B cell proliferation and IgM production, as well as upregulation of activation markers and IL-6 production by both B cells and monocytes (2–7).
In pDCs, CpG function has been shown to reflect differential subcellular localization. CpG-A routinely accumulates in early endosomes, while CpG-B accumulates in LAMP1+ endolysosomes. Importantly, experimental manipulation of CpG-A for delivery to lysosomal compartments leads to a CpG-B-like cytokine response (2, 3, 8). The discrete trafficking patterns of CpG-A and CpG-B ODN are at least partially due to differences in receptor-mediated uptake. Scavenger receptors, such as CXCL16 in pDCs (4) and SR-A (9, 10) in macrophages have been implicated in CpG-A ODN uptake and cytokine production. In contrast, the scavenger receptor MARCO has been shown responsible for CpG-B uptake and function in macrophages (11). Whether there is a direct association between specific scavenger receptors, subcellular localization of CpG ODN, and quality of TLR9-dependent responses in these and other cell types remains unclear.
In B cells, little is known about the entry mechanism employed by CpG ODNs. B cells do not express CXCL16, and lack of expression of this receptor has been correlated with unresponsiveness to CpG-A ODN (4). CpG-A is internalized by human CD19+ PBMC (7) and at high concentrations induces modest B cell responses (7, 12). Hence, the weak activity of CpG-A in B cells may be due to a relative inability of B cells to take up CpG-A or a failure of CpG-A to accumulate in a TLR9-containing compartment.
In resting B cells, TLR9 is mainly found in early endosomes, and remains in this compartment upon stimulation with CpG-B. However, when B cells are stimulated with anti-IgM F(ab’)2, TLR9 is recruited to autophagosome-like structures. In this compartment, TLR9 can “sample” the antigen bound to the BCR. This recruitment is MyD88-independent (13). Our previous observations with IgG2a reactive AM14 B cells are consistent with a model in which BCR engagement promotes TLR9-dependent responses. AM14 B cells respond robustly to immune complexes (ICs) containing endogenous DNA in a TLR9-dependent manner (14, 15). We therefore reasoned that delivery of CpG-A in the form of an IC would prove to be a potent TLR9 stimulus in these cells. Moreover, since BCR engagement induces relocalization of TLR9 (13), we hypothesized that BCR engagement by an irrelevant IC would promote B cell responses to uncomplexed CpG-A. Accordingly, we also explored the ability of mammalian DNA to promote TLR9-dependent B cell responses upon BCR engagement by antibody/protein ICs.
Materials and Methods
Mice
AM14 transgenic mice and AM14 TLR9−/− mice have been described (14, 16). AM14 KI mice were generated by insertion of the AM14 H chain into the endogenous H chain locus (Christensen and Shlomchik, manuscript in preparation) and were maintained at the Laboratory Animal Sciences Center at Boston University School of Medicine. All animal procedures were performed under the guidelines of the Association for Assessment and Accreditation of Laboratory Animal Care, and approved by Boston University School of Medicine Institutional Animal Care and Use Committee.
Reagents
Unlabelled ODN 2336 and 2216 (CpG class A), control ODN 2243 (GpC class A), ODN 1826 and 2006 (CpG class B) were from Coley Pharmaceuticals (Wellesley, MA). Biotin-and Alexa-488- modified ODN 2336, Alexa 647-modified ODN 2336, and Cy5-CpG-B ODN were purchased from Operon (Huntsville, AL). Biotin-1826 was purchased from TriLink (San Diego, CA). The anti-biotin IgG2a mAb 1D4 has been described (17). Ovalbumin was purchased from Sigma (St Louis, MI) and biotinylated by using Sulfo-NHS-LC-biotin from Pierce (Rockford, IL) following the manufacturer’s specifications. F (ab’)2 fragments of goat anti-mouse IgM were from Jackson Immunoresearch (West Grove, PA). Pam3CysSK4 was from EMC Microcollections (Tuebingen, Germany) and R848 was from Invitrogen (Carlsbad, CA). Clone 11 and CGneg fragments were described previously (15, 17), BLyS was kindly provided by Human Genome Sciences (Rockville, MD). Alexa 647 and FITC-labeled choleratoxin subunit B and Hochst dye were from Molecular Probes-Invitrogen (Carlsbad, CA).
B cell proliferation studies
Mouse splenic B cells were purified using B220+ magnetic beads (BD biosciences, San Jose, CA) following manufacturer’s specifications. Primary B cells were stimulated in RPMI supplemented with 10% (v/v) fetal bovine serum (Hyclone, Ogden, UT). B cells were stimulated with specified reagents for 24 h, and then pulsed with 5 mCi/mL of [3H] thymidine in RPMI complete for additional 6 h. Incorporated radioactivity was counted using a Microbeta Trilux counter (PerkinElmer, Waltham, MA). CpG-A, CpG-B and OVA immune complexes were preformed by combination of 1D4 and biotinylated reagents in RPMI and incubation for 15–30 min at 37°C.
Gel permeation chromatography
CpG ODN 2216 (A-class) or CpG ODN 2006 (B-class) was dissolved in PBS and run on a Superose 6 size exclusion column (GE Healthcare) that had previously been equilibrated with PBS. UV absorbance at 254 nm was recorded over time. Marker proteins dissolved in PBS with defined molecular weights (GE Healthcare) were separated in different runs and the absorbance was recorded as above. In addition, CpG ODN 2216 was dissolved in water and heat denatured before separation on a Superose 6 size exclusion column that had been equilibrated in water.
Cytokine production
Culture supernatants were collected from B cells after 24 hrs of stimulation. Cytokine concentrations were determined with the Milliplex Mouse Cytokine Assay (Millipore, Billerica, MA).
Confocal microscopy
Purified splenic B cells were stimulated with specified reagents for 30 min at 37°C, attached on poly-L-lysine coated glass-bottom 35 mm tissue culture dishes (MatTek Corporation, Ashland, MA), and visualized using a Leica SP2 AOBS laser scanning microscope. Live cells were imaged on a heated chamber at 37°C (Warner Instruments).
Results
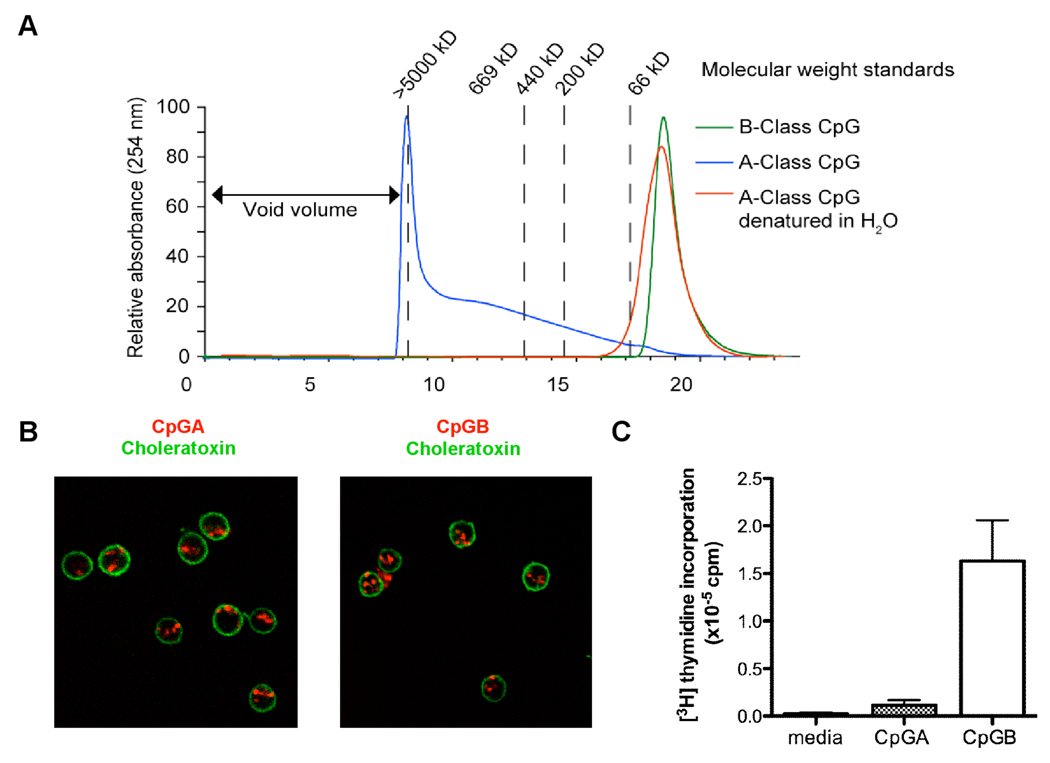
B cells take up large CpG-A ODN particles
The preponderance of CpG-A, but not CpG-B monomers to form macromolecular aggregates was demonstrated by gel filtration chromatography. The CpG-A ODN 2216 diluted in PBS, a condition that favors G-tetrad formation, was compared to 2216 dissolved in water and to the CpG-B ODN 2006 in PBS. CpG-A in PBS formed aggregates of 5000 kDa or larger, however in the absence of salt, CpG-A ODN exhibited a molecular weight lower than 66 kDa, comparable to CpG-B (Fig 1A).
Figure 1. CpG-A ODN forms large aggregates that are internalized by B cells but induce low proliferation.
(A) CpG-A in PBS (blue) or in water (red) was separated by gel permeation chromatography and compared to CpG-B in PBS (green). (B) B cells were incubated with Alexa 647-labeled CpG-A at 1 µM (red), and stained with FITC-choleratoxin to delimit the plasma membrane (green). Shown in a representative experiment of at least three additional experiments. Scale bar represents 5 µm. (C) AM14 B cells were incubated with 1 µM CpG-A or 0.1 µM CpG-B for comparison, and proliferation determined by [3H] thymidine incorporation after 24 h. Shown are mean+SEM, n=3.
To determine whether CpG-A ODN could be efficiently internalized by B cells, we assessed the uptake of increasing concentrations of Alexa 647-labeled CpG-A by confocal microscopy. To delimit the plasma membrane, we added fluorescently labeled cholera toxin subunit B, which binds to lipid rafts. We were only able to detect CpG-A internalization when it was used at a concentration of at least 1 µM (Fig 1B panel and data not shown). The same concentration of CpG-A induces very weak proliferation of AM14 B cells (Fig 1C), much lower than the proliferative response elicited by a 10-fold lower concentration (0.1 µM) of CpG-B.
CpG-A incorporation into immune complexes leads to enhanced uptake and TLR9-dependent B cell proliferation
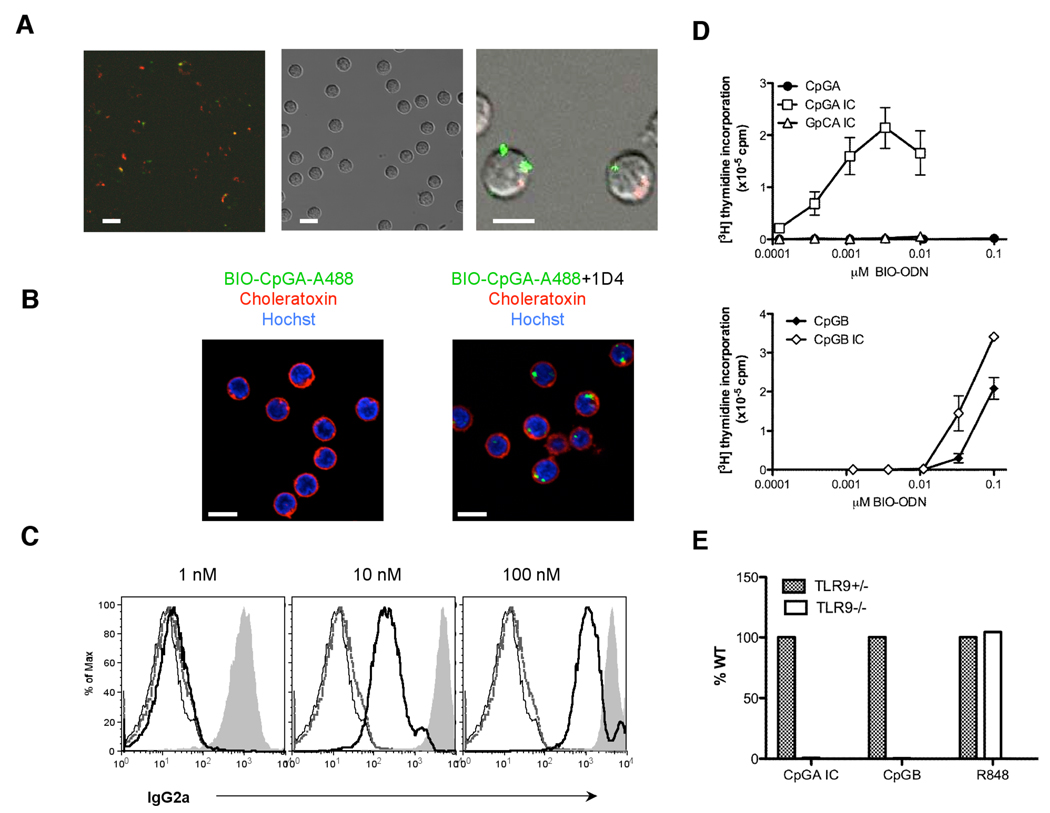
Since it appeared that lack of internalization alone could not account for the inability of CpG-A to activate B cells, we next asked whether CpG-A and CpG-B accumulated in distinct subcellular compartment. B cells were incubated with 1 µM concentrations of Alexa488-labeled CpG-A (green) and Cy5-labeled CpG-B (red). B cells take up CpG-B much more efficiently than CpG-A, as shown by the higher number of Cy5-labeled B cells that could be detected (Fig 2A left panel) compared to Alexa488-labeled B cells. In B cells that took up both classes of ODN, CpG-A and CpG-B did not appear to colocalize (Fig 2A, right panel). This staining pattern suggested that the inability of CpG-A to effectively activate B cells was not simply due to inefficient internalization.
Figure 2. CpG-A is internalized more efficiently when added as an IC, and mediates TLR9-dependent activation.
(A) Alexa 488-labeled CpG-A (green) and Cy5-labeled CpG-B (red) both at 1 µM were added to AM14 B cells and analyzed by confocal microscopy after 30 min. (B) AM14 B cells were incubated with 0.1 µM Alexa 488-labeled CpG-A (left panel) or 0.1 µM CpG-A IC (right panel) for 30 min. Plasma membrane was stained using fluorescently-labeled choleratoxin (red) and cell nucleus using Hochst dye (blue). Shown are representative experiments of at least three (A) and two (B) additional experiments. Scale bar represents 5 µm. (C) Immune complexes formed by combining 5 µg/ml 1D4 with CpG-A (grey solid curve) or CpG-B (bold black line) at 1, 10 and 100 nM concentration were added to AM14 B cells, and IC binding detected by flow cytometry using an anti-IgG2a antibody. No addition: thin black line, 1D4 alone: grey line. (D) AM14 B cells were incubated with increasing concentrations of CpG-A (closed circles), CpG-A + 3 µg/ml 1D4 (CpG-A IC, open squares) or GpC-A + 3 µg/ml 1D4 (GpC-A IC, open triangles) (top), or with increasing concentrations of CpG-B alone (closed diamonds) or CpG-B + 3µg/ml 1D4 (open diamonds) (bottom). (E) AM14 WT and AM14 TLR9−/− B cells were stimulated with CpG-A IC, CpG-B and R848. In (D) and (E), proliferation was determined by [3H] thymidine incorporation. In (E), data is represented as % proliferation of WT.
We have previously shown that IgG2a-specific AM14 B cells can be effectively activated by immune complexes (ICs) containing CpG-rich DNA through a mechanism dependent on BCR-mediated uptake and TLR9 (15, 17). To determine whether delivery of CpG-A to B cells as an IC could enhance CpG-A internalization, we used doubly-conjugated Alexa 488/biotin CpG-A (A488/Bio-CpG-A) in combination with the IgG2a anti-biotin mAb, 1D4. At a 0.1 µM concentration, we were unable to detect the uptake of uncomplexed CpG-A (Fig 2B, left panel), however when delivered as an IC, CpG-A was very efficiently internalized (Fig 2B, right panel). To determine how well CpG-A delivered as an IC could activate B cells, increasing concentrations of biotin-conjugated CpG-A or CpG-B were premixed with a fixed amount of 1D4. As anticipated, at any given concentration, Bio-CpG-A formed larger ICs than the ICs formed with Bio-CpG-B, as detected by binding to AM14 B cells at 4°C (Fig 2C). AM14 B cells bind IgG2a with low affinity and the increased avidity of larger ICs has a dramatic effect on BCR-dependent binding (17). Quite remarkably, CpG-A ICs induced a robust proliferative response, even at exceedingly low concentrations, under conditions where control GpC-A ICs (same sequence except for an inverted CG dinucleotide) completely lacked stimulatory activity (Fig 2D, top panel). By comparison, CpG-B ICs were only slightly more active than uncomplexed CpG-B (Fig 2D, bottom panel). The proliferative response by CpG-A IC was completely dependent on TLR9, as AM14 TLR9−/− B cells failed to respond to these complexes (Fig 2E). Therefore, CpG-A is perfectly capable of activating TLR9 in B cells when incorporated into an IC that can be bound and internalized by the BCR.
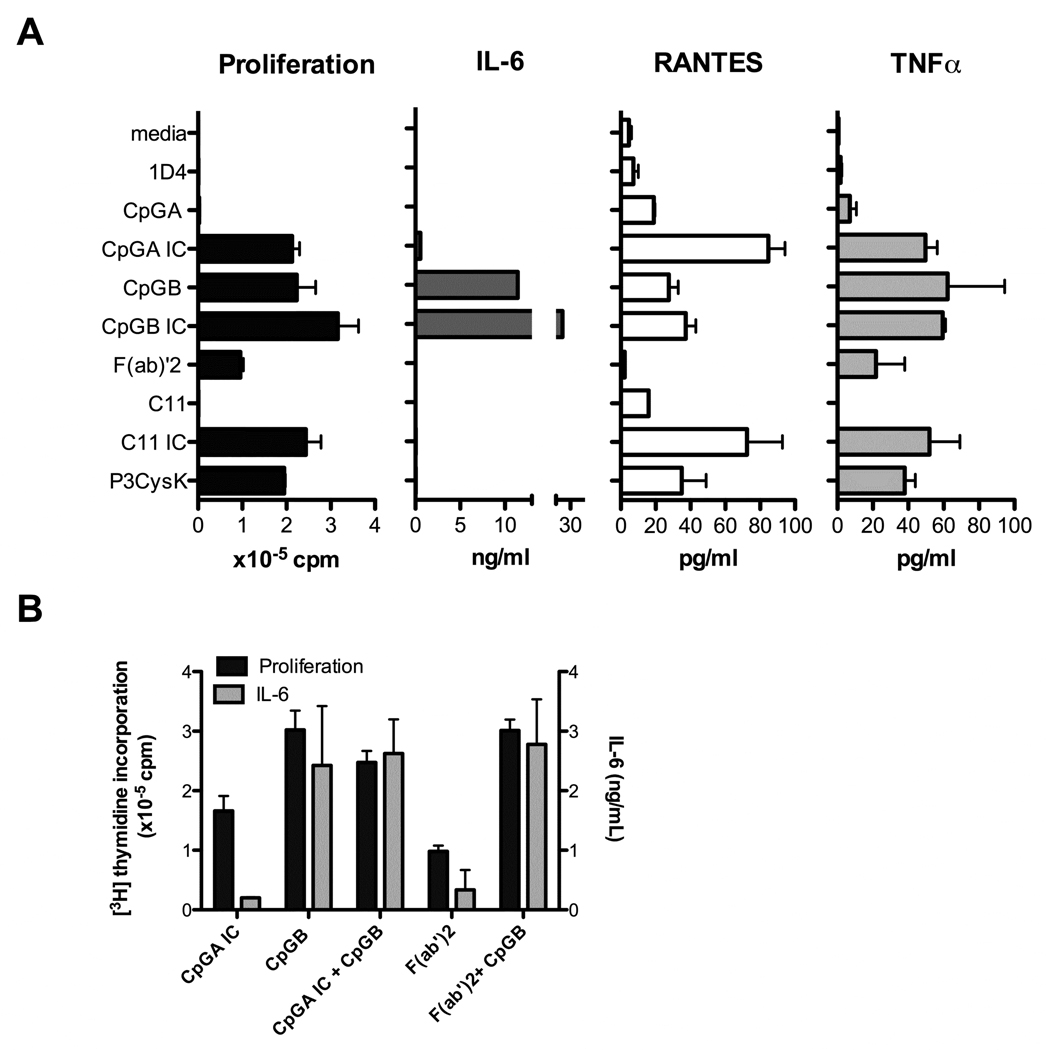
CpG-A IC and CpG-B elicit a distinct cytokine profile
It is well established that CpG-B induces B cells to both proliferate and produce a variety of cytokines, including high titers of IL-6 (7). To determine if CpG-A ICs elicited a comparable response, AM14 B cells were stimulated with CpG-A IC and CpG-B, using concentrations that induced similar levels of proliferation. Unexpectedly, B cells stimulated by CpG-A ICs produced at least 20-fold less IL-6 than B cells stimulated with CpG-B, even though they produced relatively similar amounts of TNFα (Fig 3A). These results were surprising, since the doses of CpG-A IC and CpG-B used for these experiments induced comparable and fully TLR9-dependent levels of proliferation. To determine whether BCR crosslinking simply suppressed the production of IL-6, AM14 B cells were stimulated simultaneously with either CpG-A IC and CpG-B, or anti-IgM F(ab’)2 and CpG-B. We found that the CpG-B induction of IL-6 was not inhibited by CpG-A IC or by anti-IgM F(ab’)2 (Fig 3B). Importantly, ICs composed of IgG2a bound to the mammalian CG-rich dsDNA fragment Clone 11 (Clone 11 ICs), which have been shown to promote TLR9-dependent B cell proliferative responses (17) also failed to induce IL-6 production. By contrast, ICs consisting of antibody-bound CpG-B (Fig 3A) produced even more IL-6 than CpG-B alone (Fig 3A). Overall, these results are consistent with the notion that high level IL-6 production correlates with engagement of intracellular TLR9 by relatively small ligands.
Figure 3. Stimulation of autoreactive B cells with CpG-A IC leads to enhanced RANTES and lower IL-6 production when compared to CpG-B alone.
(A) AM14 B cells were incubated with 3 µg/ml 1D4, 0.1 µM CpG-A, 0.2 µM CpG-B, CpG-A in complex with 3 µg/ml 1D4 (CpG-A IC), CpG-B in complex with 3 µg/ml 1D4 (CpG-B IC), 15 µg/ml F(ab’)2 anti-IgM, 300 ng/ml Clone 11 (C11), Clone 11 in complex with 3 µg/ml 1D4 (C11 IC) or control TLR2 ligand Pam3CysK4 at 1 µg/ml (P3CysK) for 24 hours, the supernatants harvested and IL-6, RANTES and TNFα production measured. Proliferation was determined by [3H] thymidine incorporation. (B) AM14 B cells were stimulated with CpG-A IC, CpG-B, CpG-A IC plus CpG-B, F(ab’)2 anti-IgM or F(ab’)2 plus CpG-B at the concentrations specified in (A). Proliferation and IL-6 production were determined as in (A).
Since CpG-A and CpG-B elicit distinct sets of cytokines in pDCs, it was important to determine whether CpG-A IC activated B cells to secrete cytokines other than IL-6. We found that CpG-A IC-activated cells secreted 3-fold more RANTES than CpG-B. High levels of RANTES were also secreted in response to Clone 11 ICs, but not in response to F(ab’)2 anti-IgM (Fig 3A). Thus large ICs incorporating TLR9 ligands appear functionally distinct from smaller TLR9 ligands such as CpG-B, as well as from ligands that only crosslink the BCR.
BCR stimulation induces TLR9-dependent B cell activation by uncomplexed CpG-A
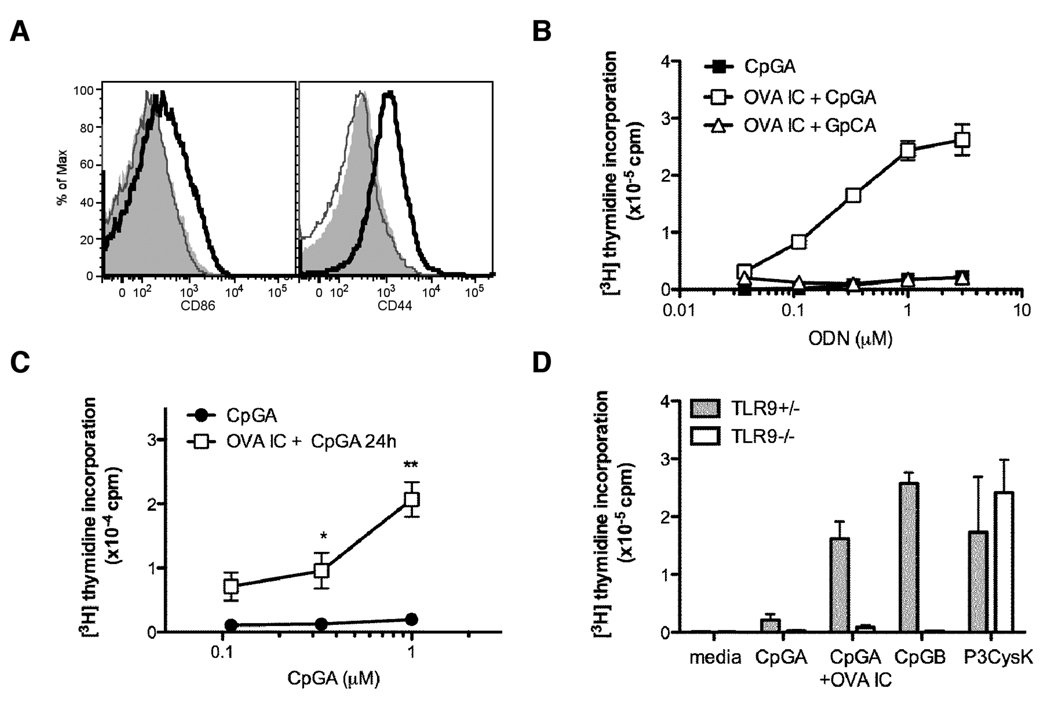
As shown above, BCR delivery of CpG-A to AM14 B cells results in the enhance uptake of this ODN when compared to non-BCR mediated entry. It has been further shown that BCR ligation by anti-IgM F(ab’)2 is sufficient to redirect the subcellular localization of TLR9 from endosomal to autophagosome-like compartments (13). These results suggest that BCR signaling cascades play a critical role in the intracellular trafficking events that follow BCR ligation. It follows that BCR engagement should facilitate the colocalization of uncomplexed CpG-A and TLR9. As shown previously with protein ICs, and above with GpC ICs, crosslinking the AM14 BCR with IgG2a-associated ICs that do not incorporate a TLR9 or (or TLR7 ligand) fails to elicit a proliferative response. Under the same conditions, B cells expressing a receptor with ~100 fold higher affinity for IgG2a can be activated by protein ICs (15). Protein IC consisting of 1D4 bound to biotinylated ovalbumin (OVA IC) do however induce upregulation of the costimulatory molecule CD86 and the activation marker CD44 in AM14 B cells (Fig 4A) in spite of promoting very little proliferation (<0.1×105 cpm), indicating that suboptimal activation of the BCR by OVA IC mediates certain aspects of B cell activation. To determine whether BCR engagement by OVA IC modified B cell responses to uncomplexed CpG-A, we stimulated AM14 B cells with OVA IC and increasing concentrations of CpG-A. The results showed that B cells incubated with OVA IC and CpG-A proliferated strongly in a CpG-A dose-dependent manner (Fig 4B). The control GpC-A added together with OVA IC, (as well as CpG-A alone) failed to induce B cell proliferation (Fig 4B). This CpG-A-dependent proliferative response required BCR crosslinking, as the addition of anti-biotin antibody alone did not have an effect (results not shown).
Figure 4. BCR stimulation with protein ICs induce TLR9-dependent responses to CpG-A.
(A) AM14 B cells were stimulated with medium alone (grey shaded curve), 3 µg/ml anti-biotin 1D4 (thin grey line) or 1 µg/ml Bio-ovalbumin in complex with 3µg/ml 1D4 (OVA IC, bold black line), and CD86 and CD44 were measured by flow cytometry. (B) AM14 B cells were stimulated with increasing concentrations of CpG-A alone (closed squares), CpG-A in the presence of OVA IC (open squares), or control GpC-A plus OVA IC (open triangles). (C) AM14 B cells were stimulated with OVA IC for 24 h in the presence of BLyS, washed twice to remove OVA IC, and then stimulated with increasing concentrations of CpG-A for additional 24 h. (D) AM14 TLR9+/− (grey bars) and TLR9−/− (open bars) B cells were stimulated with 1 µM CpG-A alone, CpG-A plus OVA IC, 0.2 µM CpG-B or the TLR2 ligand Pam3CysK4 at 1 µg/ml (P3CysK). Proliferation was determined by [3H] thymidine incorporation. (* p<0.05, **p<0.01, n=3).
To rule out the possibility that CpG-A was simply taken up non-specifically through the BCR-internalized endosomes, AM14 B cells were preincubated with OVA IC for 24 h, then washed to remove any remaining ICs. Increasing concentrations of CpG-A were then added for an additional 24 hr. Because AM14 B cells typically do not survive well for more than 24 h in culture, these experiments were conducted in the presence of the B cell growth factor BLyS. We found that AM14 B cells preincubated with OVA IC were still able to respond to CpG-A to a significantly greater extent than B cells not pre-incubated with OVA IC (Fig 4C). B cell activation by OVA IC in the presence of CpG-A was completely abolished in TLR9−/− B cells (Fig 4D). These results indicated that suboptimal BCR engagement can promote the co-localization of CpG-A and TLR9.
BCR stimulation enhances TLR9-dependent activation of B cells by mammalian DNA
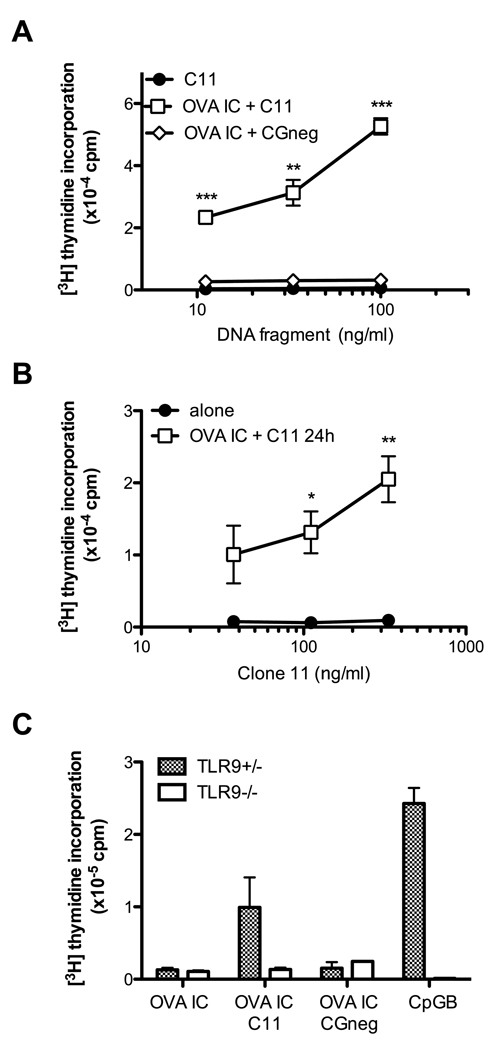
A mentioned above, AM14 B cells proliferate in response to Clone 11 ICs that incorporate ~600bp fragments of CG-rich mammalian DNA (17). Uncomplexed fragments did not elicit a response. The CpG-A IC data above suggested that suboptimal BCR engagement might also promote B cell responses to uncomplexed mammalian dsDNA fragments. To determine whether BCR crosslinking induced B cell responses to more physiologically relevant TLR9 ligands than CpG-A, we incubated AM14 B cells with OVA IC and added increasing concentrations of the immunostimulatory CpG island dsDNA fragment Clone 11 (17). Clone 11 induce a dose-dependent proliferative response only in the presence of OVA IC. A control DNA fragment devoid of CpG motifs, CGneg, was unable to stimulate B cell activation under similar conditions (Fig 5A). As in the case of CpG-A, AM14 B cells pre-incubated with OVA IC for 24 hr and then washed, could also respond to Clone 11, in contrast to B cells not primed with OVA IC (Fig 5B). This response was again TLR9-dependent (Fig 5C). Thus BCR crosslinking promotes the response of B cells to mammalian TLR9 ligands.
Figure 5. BCR stimulation leads to TLR9-dependent AM14 B cell proliferation in response to bystander mammalian DNA.
(A) AM14 B cells were stimulated with increasing concentrations of the CpG island Clone 11 alone (C11, closed circles), C11 in the presence of OVA IC (open squares) or CGneg in the presence of OVA IC (open diamonds). (B) AM14 B cells were stimulated with OVA IC for 24 h in the presence of the growth factor BLyS, washed twice, and incubated with increasing concentrations of Clone11 for additional 24 h. (C) AM14 TLR9+/− (checkered bars) or TLR9−/− (open bars) B cells were stimulated with Clone 11 (C11) plus OVA IC, CGneg plus OVA IC or CpG-B. Proliferation was determined by [3H] thymidine incorporation. * p<0.05, ** p<0.01 and *** p<0.001, n=3).
Discussion
It is well established that CpG-A and CpG-B ODNs accumulate in distinct intracellular compartments in pDCs. CpG-A localizes to early endosomes where it triggers the production of IFNα, and CpG-B localizes to a LAMP1+ compartment where it triggers the production of proinflammatory cytokines and pDC maturation. By altering the structure and delivery mechanism of these ODNs, it was possible to force CpG-A ODNs to induce CpG-B-like responses and vice-versa (2, 3). Moreover, when a third form of ODN, CpG-C, which normally traffics to both compartments and elicits both IFNα production and pDC maturation, was specifically directed to only the LAMP1+ compartment, pDC maturation was observed but IFNα production was eliminated (2). Together, these studies clearly demonstrate the importance of intracellular localization in TLR9-elicited pDC effector functions. We have now extended this compartment/function paradigm to B cells.
Prior to this report, CpG-A ODNs had been shown to have only minimal effects on B cells, while CpG-B ODNs were recognized as potent B cell mitogens. One possible explanation for the inability of CpG-A to activate B cells was the lack of expression of the scavenger receptor(s) shown to mediate CpG-A uptake in other cell types (4). Our data indicate that CpG-A is internalized by resting B cells but fails to traffic to a TLR9+ compartment in these cells. The uptake of CpG-A can be increased by incorporating the ODN into an IC recognized by the AM14 BCR. Under these conditions, CpG-A induces a remarkably robust proliferative response, comparable to that elicited by a 100-fold higher molar concentration of CpG-B. This CpG-A response most likely reflects both increased uptake of CpG-A through the BCR and relocalization of TLR9 as a result of BCR ligation (13).
BCR crosslinking by anti-IgM has also been reported to enhance the non-specific uptake of radiolabeled F(ab) (18). Thus BCR stimulation promotes the overall endocytic capacity of B cells, possibly to ensure more efficient responses to antigens present at high concentration in the local microenvironment during the course of an infection. Therefore the proliferative response of AM14 B cells elicited by uncomplexed CpG-A and clone 11 in the context of co-stimulation with protein ICs could also be due to the combined effects of increased CpG-A/clone 11 uptake and BCR-mediated TLR9 relocalization. This observation also has implications for B cell function in the context of autoimmune disease, where it is possible that B cells activated by BCR-recognition of a microbial antigen or autoantigen, can then more efficiently endocytose bystander self-antigens that are taken up nonspecifically and then engage a relocalized TLR. In accordance with this mechanism of activation, marginal zone (MZ) B cells isolated from lupus mice show enhanced responses to CpG-A when compared to MZ B cells from normal mice suggesting these cells may be in activated state in lupus-prone mice and more easily activated by bystander DNA (19, 20).
Our results also demonstrate that CpG-induced proliferation does not always correlate with a predicted profile of cytokine production. Both CpG-B and CpG-A ICs induce a robust proliferative response but they elicit very different cytokine profiles. While the two stimuli elicit comparable amounts of TNFα, CpG-B triggers the release of much higher levels of IL-6 and CpG-A ICs consistently induces twice as much RANTES. High levels of RANTES, a T cell and macrophage chemokine, have been detected in the serum and kidneys of patients with SLE (21, 22) and in murine models of autoimmune disease (23, 24). The cell type(s) responsible for elevated RANTES titers in these conditions remains to be determined, but autoreactive B cells responding to self-antigens may be an important component. Interestingly, CpG-A ICs failed to induce the expression of Type I IFNs in B cells (data not shown), despite the known role of CpG-A in the induction of IFNα production by pDCs. Thus, TLR9-dependent B cell responses to CpG-A ICs do not recapitulate the pDC response to CpG-A.
Notably, the functional outcome elicited by CpG-B ICs (Bio-CpG-B + anti-biotin 1D4) is remarkably similar to CpG-B response. Both the level of proliferation and the amount of IL-6 produced are slightly higher than the response to CpG-B alone. CpG-B ICs are much smaller than CpG-A ICs as they have only one biotinylated residue /molecule of CpG-B; and are not likely to aggregate to form macromolecular lattices like CpG-A, or CpG-A ICs. Therefore simply targeting CpG-B to the BCR and thereby facilitating uptake may modestly increase the level but not the quality of the response. Importantly, extensive crosslinking of the BCR by anti-IgM did not suppress CpG-B-elicited IL-6 production. Therefore, it is most likely that the size of the CpG-A ICs determines intracellular location and, as in the case of pDCs, that location determines functional outcome. This is consistent with the observation that stimulation with both defined CG-rich Clone 11 dsDNA ICs and spontaneous chromatin ICs (mAb PL2-3) results in a cytokine profile very similar to that of the CpG-A ICs (25); Clone 11 and PL2-3 ICs are likely to be much larger that CpG-B IC and the function elicited by the these ICs is probably the most relevant from a disease-perspective.
In summary, the BCR has a multifaceted role in the activation of autoreactive B cells. First, it can facilitate the uptake of autoantigens, and the subsequent delivery to TLR9+ compartments. Identification of the exact compartments targeted by this process will require further study, but it is highly likely that the final destination depends at least to some extent on the size of the ligand. Moreover, either the extent of TLR9 crosslinking, or differential activation of TLR9 signaling cascades due to compartment-specific co-receptors or downstream adaptor proteins, determines function. While both smaller and larger TLR9 agonists appear to induce clonal expansion, the specific set of cytokines produced by the B cell can be highly variable. Secondly, the data indicate that TLR9-dependent B cell responses to DNA-associated autoantigens are not only restricted to their direct delivery by the BCR. BCR ligation by an antigen incapable of engaging TLR9 may nevertheless promote the enhanced BCR-independent uptake of autoantigens and/or relocalization of TLR9 to the appropriate autoantigen-associated endocytic compartment. Such non-specific uptake associated with TLR ligation essentially extends the potential contribution of B cells to the further activation of macrophages and autoreactive T cells and may partially account for the therapeutic efficacy of targeting B cells in a remarkably wide range of autoimmune conditions (26).
Abbreviations used in this paper
- ODN
oligonucleotide
- SLE
Systemic Lupus Erythematosus
- LAMP
Lysosome Associated Membrane Protein
Footnotes
This work was supported by National Institutes of Health Grants AR050256 and AR35230 to A.M.R, and RO1 AI068056 to F.L.
References
- 1.Kerkmann M, Costa LT, Richter C, Rothenfusser S, Battiany J, Hornung V, Johnson J, Englert S, Ketterer T, Heckl W, Thalhammer S, Endres S, Hartmann G. Spontaneous formation of nucleic acid-based nanoparticles is responsible for high interferon-alpha induction by CpG-A in plasmacytoid dendritic cells. J Biol Chem. 2005;280:8086–8093. doi: 10.1074/jbc.M410868200. [DOI] [PubMed] [Google Scholar]
- 2.Guiducci C, Ott G, Chan JH, Damon E, Calacsan C, Matray T, Lee KD, Coffman RL, Barrat FJ. Properties regulating the nature of the plasmacytoid dendritic cell response to Toll-like receptor 9 activation. J Exp Med. 2006;203:1999–2008. doi: 10.1084/jem.20060401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Honda K, Ohba Y, Yanai H, Negishi H, Mizutani T, Takaoka A, Taya C, Taniguchi T. Spatiotemporal regulation of MyD88-IRF-7 signalling for robust type-I interferon induction. Nature. 2005;434:1035–1040. doi: 10.1038/nature03547. [DOI] [PubMed] [Google Scholar]
- 4.Gursel M, Gursel I, Mostowski HS, Klinman DM. CXCL16 influences the nature and specificity of CpG-induced immune activation. J Immunol. 2006;177:1575–1580. doi: 10.4049/jimmunol.177.3.1575. [DOI] [PubMed] [Google Scholar]
- 5.Krug A, Rothenfusser S, Hornung V, Jahrsdorfer B, Blackwell S, Ballas ZK, Endres S, Krieg AM, Hartmann G. Identification of CpG oligonucleotide sequences with high induction of IFN-alpha/beta in plasmacytoid dendritic cells. Eur J Immunol. 2001;31:2154–2163. doi: 10.1002/1521-4141(200107)31:7<2154::aid-immu2154>3.0.co;2-u. [DOI] [PubMed] [Google Scholar]
- 6.Verthelyi D, Ishii KJ, Gursel M, Takeshita F, Klinman DM. Human peripheral blood cells differentially recognize and respond to two distinct CPG motifs. J Immunol. 2001;166:2372–2377. doi: 10.4049/jimmunol.166.4.2372. [DOI] [PubMed] [Google Scholar]
- 7.Gursel M, Verthelyi D, Gursel I, Ishii KJ, Klinman DM. Differential and competitive activation of human immune cells by distinct classes of CpG oligodeoxynucleotide. J Leukoc Biol. 2002;71:813–820. [PubMed] [Google Scholar]
- 8.Latz E, Schoenemeyer A, Visintin A, Fitzgerald KA, Monks BG, Knetter CF, Lien E, Nilsen NJ, Espevik T, Golenbock DT. TLR9 signals after translocating from the ER to CpG DNA in the lysosome. Nat Immunol. 2004;5:190–198. doi: 10.1038/ni1028. [DOI] [PubMed] [Google Scholar]
- 9.Pearson AM, Rich A, Krieger M. Polynucleotide binding to macrophage scavenger receptors depends on the formation of base-quartet-stabilized four-stranded helices. J Biol Chem. 1993;268:3546–3554. [PubMed] [Google Scholar]
- 10.Suzuki K, Doi T, Imanishi T, Kodama T, Tanaka T. Oligonucleotide aggregates bind to the macrophage scavenger receptor. Eur J Biochem. 1999;260:855–860. doi: 10.1046/j.1432-1327.1999.00233.x. [DOI] [PubMed] [Google Scholar]
- 11.Jozefowski S, Sulahian TH, Arredouani M, Kobzik L. Role of scavenger receptor MARCO in macrophage responses to CpG oligodeoxynucleotides. J Leukoc Biol. 2006;80:870–879. doi: 10.1189/jlb.0705357. [DOI] [PubMed] [Google Scholar]
- 12.Ballas ZK, Krieg AM, Warren T, Rasmussen W, Davis HL, Waldschmidt M, Weiner GJ. Divergent therapeutic and immunologic effects of oligodeoxynucleotides with distinct CpG motifs. J Immunol. 2001;167:4878–4886. doi: 10.4049/jimmunol.167.9.4878. [DOI] [PubMed] [Google Scholar]
- 13.Chaturvedi A, Dorward D, Pierce SK. The B cell receptor governs the subcellular location of Toll-like receptor 9 leading to hyperresponses to DNA-containing antigens. Immunity. 2008;28:799–809. doi: 10.1016/j.immuni.2008.03.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Leadbetter EA, Rifkin IR, Hohlbaum AM, Beaudette BC, Shlomchik MJ, Marshak-Rothstein A. Chromatin-IgG complexes activate B cells by dual engagement of IgM and Toll-like receptors. Nature. 2002;416:603–607. doi: 10.1038/416603a. [DOI] [PubMed] [Google Scholar]
- 15.Viglianti GA, Lau CM, Hanley TM, Miko BA, Shlomchik MJ, Marshak-Rothstein A. Activation of autoreactive B cells by CpG dsDNA. Immunity. 2003;19:837–847. doi: 10.1016/s1074-7613(03)00323-6. [DOI] [PubMed] [Google Scholar]
- 16.Hannum LG, Ni D, Haberman AM, Weigert MG, Shlomchik MJ. A disease-related rheumatoid factor autoantibody is not tolerized in a normal mouse: implications for the origins of autoantibodies in autoimmune disease. J Exp Med. 1996;184:1269–1278. doi: 10.1084/jem.184.4.1269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Uccellini MB, Busconi L, Green NM, Busto P, Christensen SR, Shlomchik MJ, Marshak-Rothstein A, Viglianti GA. Autoreactive B cells discriminate CpG-rich and CpG-poor DNA and this response is modulated by IFN-alpha. J Immunol. 2008;181:5875–5884. doi: 10.4049/jimmunol.181.9.5875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Song W, Cho H, Cheng P, Pierce SK. Entry of B cell antigen receptor and antigen into class II peptide-loading compartment is independent of receptor crosslinking. J Immunol. 1995;155:4255–4263. [PubMed] [Google Scholar]
- 19.Brummel R, Lenert P. Activation of marginal zone B cells from lupus mice with type A(D) CpG-oligodeoxynucleotides. J Immunol. 2005;174:2429–2434. doi: 10.4049/jimmunol.174.4.2429. [DOI] [PubMed] [Google Scholar]
- 20.Brummel R, Roberts TL, Stacey KJ, Lenert P. Higher-order CpG-DNA stimulation reveals distinct activation requirements for marginal zone and follicular B cells in lupus mice. Eur J Immunol. 2006;36:1951–1962. doi: 10.1002/eji.200535734. [DOI] [PubMed] [Google Scholar]
- 21.Lit LC, Wong CK, Tam LS, Li EK, Lam CW. Raised plasma concentration and ex vivo production of inflammatory chemokines in patients with systemic lupus erythematosus. Ann Rheum Dis. 2006;65:209–215. doi: 10.1136/ard.2005.038315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Vila LM, Molina MJ, Mayor AM, Cruz JJ, Rios-Olivares E, Rios Z. Association of serum MIP-1alpha, MIP-1beta, and RANTES with clinical manifestations, disease activity, and damage accrual in systemic lupus erythematosus. Clin Rheumatol. 2007;26:718–722. doi: 10.1007/s10067-006-0387-y. [DOI] [PubMed] [Google Scholar]
- 23.Moore KJ, Wada T, Barbee SD, Kelley VR. Gene transfer of RANTES elicits autoimmune renal injury in MRL-Fas(1pr) mice. Kidney Int. 1998;53:1631–1641. doi: 10.1046/j.1523-1755.1998.00911.x. [DOI] [PubMed] [Google Scholar]
- 24.Tsukahara T, Makino Y, Fujii T, Ogawa M, Saisho H, Hamano Y, Ueda S, Akikusa B, Danoff TM. Role of RANTES in the development of autoimmune tissue injuries in MRL-Fas lpr mice. Clin Immunol. 2002;103:89–97. doi: 10.1006/clim.2001.5198. [DOI] [PubMed] [Google Scholar]
- 25.Busconi L, Bauer JW, Tumang JR, Laws A, Perkins-Mesires K, Tabor AS, Lau C, Corley RB, Rothstein TL, Lund FE, Behrens TW, Marshak-Rothstein A. Functional outcome of B cell activation by chromatin immune complex engagement of the B cell receptor and TLR9. J Immunol. 2007;179:7397–7405. doi: 10.4049/jimmunol.179.11.7397. [DOI] [PubMed] [Google Scholar]
- 26.Sfikakis PP, Boletis JN, Tsokos GC. Rituximab anti-B-cell therapy in systemic lupus erythematosus: pointing to the future. Curr Opin Rheumatol. 2005;17:550–557. doi: 10.1097/01.bor.0000172798.26249.fc. [DOI] [PubMed] [Google Scholar]