Abstract
Background
Spiritual well-being (Sp-WB) is a resource that supports adaptation and resilience, strengthening quality of life (QOL) in patients with cancer or other chronic illnesses. However, the relationship between Sp-WB and QOL in patients with chronic GVHD (cGVHD) remains unexamined.
Methods
52 participants completed the Functional Assessment of Chronic Illness Therapy – Spiritual Well-Being (FACIT-Sp) questionnaire as part of a multidisciplinary study of cGVHD.
Results
Sp-WB was generally high (Mean 37.06, SD 9.5). Those with the lowest Sp-WB had significantly longer time since diagnosis of cGVHD (p=0.05) than those with higher Sp-WB. There were no associations between Sp-WB and demographics, cGVHD severity, or intensity of immunosuppression. Participants with the lowest Sp-WB (N=11) reported inferior physical (p = .0009), emotional (p = .003), social (p = .027), and functional well-being (p = < 0.0001) as well as lower overall QOL (p = <0.0001) compared to those with higher Sp-WB. They also had inferior QOL (M 54.88, S.E. 4.19) relative to population norms (M=80.1, S.E. 0.55). Differences between those with the lowest and those with better Sp-WB consistently exceeded the minimal clinically significant difference for all subscales and for overall QOL. Controlling for physical, emotional and social well-being, Sp-WB was a significant independent predictor of contentment with QOL.
Conclusions
Our results suggest that Sp-WB is an important factor contributing to the QOL of patients with cGVHD. Research is needed to identify factors that diminish Sp-WB and to test interventions designed to strengthen this coping resource in patients experiencing the late-effects of treatment.
Introduction
Hematopoietic stem cell transplantation (HSCT) is routinely used to treat patients with cancers and other disorders of the blood and immune systems.1,2 Although HSCT offers a chance at remission of the primary disease, patients are at risk for developing Graft-Versus-Host Disease (GVHD).3–5 Approximately 30–70% of individuals undergoing allogeneic HSCT for hematologic malignancies can anticipate experiencing cGVHD, which is the leading cause of non-relapse mortality in HSCT survivors.3–5 Chronic GVHD is a multi-system complication that results from recognition of the transplant recipient’s tissues as foreign, due to an autoimmune response that proceeds without modulation by thymic or peripheral mechanisms of tolerance.6 Chronic GVHD can affect multiple organ systems including the skin, mouth, eyes, lungs, gastrointestinal tract, musculoskeletal system, and the immune system. As a result, remission of the primary disease can be followed by months to years of additional therapy that are required to manage treatment for cGVHD. After suffering through the primary illness, patients may not be prepared for the difficult course of a second chronic illness. Transplantation related morbidity is evident throughout the course of HSCT, beginning with pre-transplantation conditioning and extending well into the post-transplantation recovery phase.1,7 Although cGVHD is associated with a potential graft versus malignancy effective, cGVHD and the therapies used to manage the disease can also result in symptom distress, functional loss, and disability. 3–5 The extended period of time that is generally spent recovering, as well as coping with these new issues, can have a profound impact on a patient’s QOL and well-being.8 With life threatening and chronic illnesses, clinicians must balance measures to control disease with concerns about optimizing patient QOL. 9
Spirituality is currently defined as a distinct entity, possessing a more basic etiology than religion.10 Spirituality can be expressed as being a subjective experience that exists both within and outside of traditional religious systems and can be characterized as the way in which people understand their lives in view of their ultimate meaning and value.11–14
Although there is no common definition of Sp-WB, according to various authors, Sp-WB may include such attributes as inner peacefulness, meaning and purpose in life9,15–17 connectedness with self, others and a higher power18,19 comfort in faith or beliefs,20 a sense of coherence,21 and feelings of confidence about the future. Additionally, Sp-WB can be viewed as a multi-dimensional construct which incorporates both existential and religious dimensions related to QOL.9,22,23 Existential well-being is defined as a sense of satisfaction with one’s purpose in life and identity, a belief that life is meaningful and positive, and optimism about one’s future. Religious well-being is described as a feeling of comfort that is derived from a connection to a higher power that is sacred and transcendent.23 Although clinical investigators have traditionally measured QOL using physical, emotional, social/family, and functional subscales, we view Sp-WB as a unique construct that would provide valuable insight into the patient that the other subscales fail to completely capture.
Research examining the role of Sp-WB in QOL has demonstrated the utility of this construct in contributing to maintenance and improvement in QOL both in cancer and non-cancer patient populations.24–26 The literature indicates that many cancer survivors experience improved Sp-WB; however, survivors of HSCT who are coping with cGVHD may represent a survivor group at risk for poorer Sp-WB because they are coping with symptoms and functional losses at a time when they may have expected to be resuming normal life roles and activities. Sp-WB in patients with cGVHD has not been well studied.4,23 Knowledge of the factors that promote Sp-WB in this population would enhance our understanding of the human experience of cGVHD and might reveal intervention approaches to strengthen this important coping resource. Therefore, the aims of this study are to describe the Sp-WB of individuals with cGVHD after allogeneic HSCT, to explore the clinical and demographic factors associated with Sp-WB, and to examine the association of Sp-WB with other dimensions of QOL in this population.
Materials and Methods
Setting and Sample
The data for this analysis were drawn from a prospective cross-sectional observational study of patients diagnosed with cGVHD after allogeneic HSCT 27 (ClinicalTrials.gov Identifier: NCT00331968.) Participants had been referred to this study from transplant centers across the country. Fifty-two participants were studied to explore the characteristics and correlates of Sp-WB and QOL.
Measures
Sp-WB was measured using the FACIT-Sp, a 12 item scale measuring meaning and purpose, harmony and peace and closeness to God or a higher power. The FACIT-Sp asks respondents to indicate the extent to which they experienced aspects of Sp-WB in the past week, ranging from not at all to very much.
Health-related quality of life (QOL) was measured using the FACT-G. The Functional Assessment of Cancer Therapy – General version 4 (FACT-G) The FACT-G is a 27 item questionnaire that addresses four domains of well-being: physical (7 items), social/family (7 items), emotional wellbeing (6 items) and functional wellbeing (7 items). The measures use a five point Likert scale ranging from 0 (not at all) to 4 (very much so). The time frame on which responses are based is “during the past seven days”. The FACT-G is scored by summing the items which provides an overall QOL score and a score for each subscale. The total score can range from 0–108. A higher score indicates a better QOL.28
There is evidence that the FACT-G has acceptable psychometric properties, with an internal consistency reliability of α= 0.89 and test=retest reliability of α = 0.92 in various cancer populations. The FACT-G has also demonstrated construct validity in hematopoietic stem cell transplant recipients.29 Chronic GVHD severity was assessed based on the exams performed by clinicians organ specialists and using a 0–3 severity scoring scale and a total score (CAS) based on the assessments of nine organs: skin, eyes, mouth, gastrointestinal, liver, lungs, musculoskeletal, hematologic and female genital.
Procedure
After obtaining informed consent, self–report measures and clinical and demographic data were collected during the course of a comprehensive multidisciplinary evaluation of cGVHD. Permission for the study was granted by the IRB of the National Cancer Institute, Intramural Research Program.
Statistical Analysis
Comparisons of the spirituality score for the patients at NCI and those of other published studies were performed using a Wilcoxon signed rank test. Continuous parameters such as the actual spirituality score were compared between two groups using a Wilcoxon rank sum test while comparisons among subjects in three or more unordered categories were performed using a Kruskal-Wallis test. Spirituality scores were compared across ordered categories using a Jonckheere-Terpstra test for trend.30 Comparisons between the spirituality score classified into a four group ordered categorical variable and dichotomous parameters were performed using an exact Cochran-Armitage test.31 Comparisons between the categorized spirituality parameter and non-ordered categorical parameters were made using a Kruskal-Wallis test for ordered columns.
Correlations between two continuous parameters were made using Spearman rank correlation. The correlation coefficient, r, would be interpreted as follows: |r| >0.70 would be a strong correlation; 0.5< |r| <0.7 would be a moderately strong correlation; 0.3< |r| <0.5 would indicate a weak to moderately strong correlation, and |r| <0.3 would be a weak correlation. Since the p-value associated with a correlation coefficient is for a test of whether r = 0, this would be of lower importance than the magnitude of the correlation coefficient itself.
Logistic regression analysis was used to determine whether factors of interest along with spirituality would be jointly associated with the results from the question: “I am content with the quality of my life right now,” number twenty-seven from the FACT-G questionnaire. This question was regrouped to be a three level question (0–1, 2, 3–4) because of the sparseness of the results at the extremes, in order to permit a more satisfactory modeling to be performed.
All p-values are two-tailed and are being reported without adjustment for multiple comparisons.
Results
Complete data were available on 51 of the 52 subjects in the study. The median age of the participants was 47.7 years with a range of 20 to 62 years, the sample was equally comprised of males and females, and 67% percent of the sample were married. Clinician rated GVHD severity scores ranged from 2–15, with a mean of 8 indicating moderately severe clinical manifestations of cGVHD. A median of 5 (range 2–9) organ systems were involved with cGVHD. We performed tests to evaluate whether there were any associations between clinical and demographic factors (Table 1) and Sp-WB. Those with the lowest Sp-WB had been living with cGVHD significantly longer (p=0.05) than those with higher levels of Sp-WB. There were no associations between Sp-WB and demographic variables, cGVHD severity or intensity of immunosuppression (data not shown; all p-values were between 0.10 and 0.88). Thus, these patient traits were not associated with the level of Sp-WB.
Table 1.
Clinical and Demographic Characteristics
| N (%) | |
|---|---|
| Donor Source | |
| Related | 41 (79%) |
| Unrelated | 11 (21%) |
| Source of Stem Cells | |
| Peripheral Blood | 47 (90%) |
| Bone Marrow | 5 (10%) |
| Chronic GVHD Onset | |
| De Novo | 20 (38%) |
| Quiescent | 6 (12%) |
| Progressive | 26 (50%) |
| Prior Acute GVHD | |
| Yes | 33 (63%) |
| No | 19 (37%) |
| Seattle Classification | |
| Limited | 1 (2%) |
| Extensive | 51 (98%) |
| NIH Staging Criteria | |
| Mild | 2 (4%) |
| Moderate | 34 (65%) |
| Severe | 16 (31%) |
| Mean Total Score (SD) | 8 |
| Range | 2 – 15 |
| Number of Organs Involved | |
| Median | 5 |
| Range | 2 – 9 |
| CAS Score | |
| Mean (SD) | 7.90 (2.62) |
| Range | 2 – 15 |
| KPS Score | |
| < = 60 | 4 (8%) |
| 70 | 11 (21%) |
| 80 | 19 (36%) |
| 90 | 18 (35%) |
| Diagnosis | |
| CML | 8 (15%) |
| CLL | 3 (6%) |
| AML | 12 (23%) |
| ALL | 3 (6%) |
| MM | 6 (12%) |
| Non-Hodgkin’s Lymphoma | 7 (13%) |
| Hodgkin’s Lymphoma | 3 (6%) |
| Other | 10 (19%) |
| Disease Status at the Time of Evaluation of Sp-WB | |
| Remission | 49 (93%) |
| Recurrent | 3 (7%) |
| Immunosuppression | |
| Yes | 37 (77%) |
| No | 15 (23%) |
| Median Time from Transplant to Enrollment (Days) | 810 |
| Range | 137 – 6021 |
| Median Time from cGVHD Diagnosis (Days) | 165 |
| Range | 42 – 5692 |
| Median Number of Prior Treatments | 3 |
| Range | 0 – 6 |
| Myeloblative | 29 (56%) |
| Non-Myeloblative | 23 (44%) |
| TBI Conditioning | 21 (40%) |
| Non-TBI Conditioning | 31 (60%) |
| Marital Status | |
| Married | 35 (67%) |
| Single | 11 (21%) |
| Divorced | 5 (10%) |
| Widowed | 1 (2%) |
| Religious Affiliation | |
| Catholic | 18 (35%) |
| Jewish | 3 (5%) |
| Protestant | 15 (29%) |
| Other | 16 (31%) |
| Gender | |
| Male | 29 (56%) |
| Female | 23 (44%) |
| Race | |
| White | 47 (90%) |
| African-American | 4 (8%) |
| South-Asian | 1 (2%) |
| Age | |
| Median | 47.7 |
| Range | 20 – 62 |
Table 2 presents a description of the Quality of Life Subscale scores for all patients in this study. Sp-WB was generally high (Mean 37.06, SD 9.5) and comparable to that reported by another investigator in a mixed sample of autologous and allogeneic HSCT survivors (Mean 35.9, SD 8.6, p=0.25).1 The study population was divided into two groups based on whether their FACIT-sp score was low (0–30) or high (31–48) in order to examine the relationship between Sp-WB and each of these subscale scores.
Table 2.
FACT-G Total and Subscale Scores
| Variable | Mean (SD) | Median | Range |
|---|---|---|---|
| Spiritual Well-being (SP-WB) | 37.06 (9.5) | 41 | 11 – 48 |
| Physical Well-being (PWB) | 18.4 (6.4) | 20 | 6 – 27 |
| Functional Well-Being (FWB) | 17.3 (6.6) | 18 | 3 – 28 |
| Social Well-Being (SWB) | 19.1 (8.0) | 22 | 1.71 – 28 |
| Emotional Well-Being (EWB) | 18.1 (4.4) | 19 | 2 – 24 |
| FACT-G Total | 75.1 (18.9) | 74.33 | 17 – 105 |
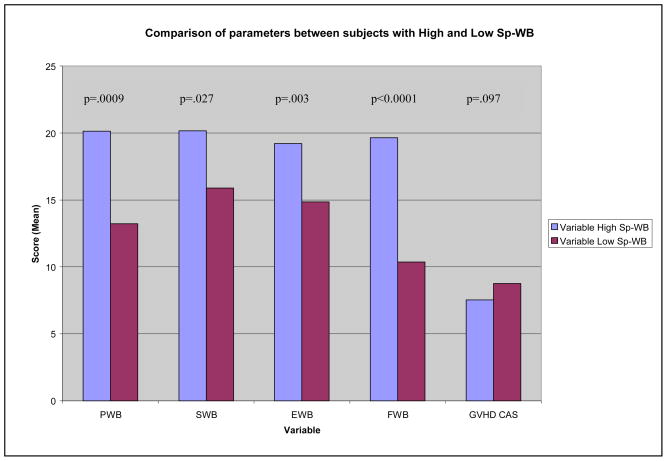
As shown in Figure 1, individuals scoring in the higher category on the Sp-WB scale also scored significantly higher on each of the FACT-G subscales and reported a higher total QOL score. Participants with the lowest Sp-WB (N=11) reported inferior physical (p = .0009), emotional (p = .003), social (p = .027), and functional well-being (p = < 0.0001) as well as lower overall QOL (p = <0.0001) compared to those with higher Sp-WB. They also had inferior QOL (M 54.88, S.E. 4.19) relative to population norms (M=80.1, S.E. 0.55).32 Differences between those with the lowest and those with better Sp-WB consistently exceeded the minimal clinically significant difference for all subscales and for overall QOL. Therefore, patients with a higher Sp-WB also experienced a better QOL overall. On the other hand, patient’s CAS score, an indicator of the severity of GVHD, was not shown to be significantly different according to level of Sp-WB.
Figure 1.
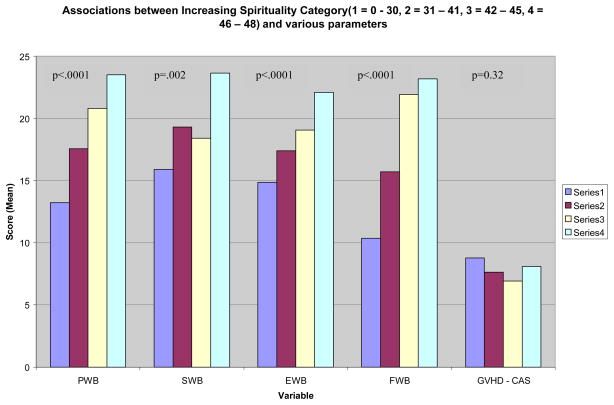
Further examination of the Sp-WB groups into four ordered categorical groups of similar size (Figure 2) demonstrated a significant trend in increasing value of each parameter investigated with increasing values in Sp-WB, except for GVHD CAS score.
Figure 2.
It was also of interest to determine if the current perception of QOL would be related to Sp-WB as well as the other components of the FACT-G. In order to examine a participant’s current QOL, we evaluated their score on question 27 of the FACT-G (0–4 likert scale), “I am content with the quality of my life right now,” as compared with their scores on the other scales including Sp-WB. The functional well-being scale was excluded from this analysis because it contains question 27. We found that patients who rated their current QOL higher also tended to score higher on the Sp-WB, social well-being, physical well-being, and emotional well-being scales with all p-values <0.02 for trends demonstrating associations between these subscales and increasing levels of current contentment with their QOL (data not shown).
Finally, in order to determine if the level of contentment with QOL may be associated with a set of components of the FACT-G, a logistic regression was performed. As shown in Table 5, the level of current QOL is significantly associated in a positive manner to EWB and level of Sp-WB, while other factors (PWB and SWB) were not important when these other factors were taken into consideration. Controlling for physical, emotional and social well-being, Sp-WB was a significant independent predictor of contentment with QOL. Table 6 summarizes patient’s Sp-WB scores for our study compared with other studies with similar populations. The mean Sp-WB score for the current study is 37.06 (9.5) with a range of 11 to 48. We found that our cGVHD population exhibited comparable values to those of the majority of existing research investigating QOL in cancer and transplant populations, but our results were significantly higher than those of studies reported by Cotton et al10(p < 0.0001) and Robb et al33 (p = .0059), that both were limited to breast cancer patients.
Table 5.
Results of Logistic Regression analysis relating contentment of quality of life and FACT-G subscales
| Parameter | Estimate | p-value | odds ratio | 95% CI for odds ratio |
|---|---|---|---|---|
| EWB | 0.20 | 0.032 | 1.22 | 1.02 – 1.46 |
| SP-WB | 0.15 | 0.0011 | 1.16 | 1.06 – 1.27 |
Table 6.
Spiritual Well-Being Scores in Other Cancer Populations
| Mean (S.D.) SP-WB | Sample Size | p-value comparing present study to all others | Population Description | |
|---|---|---|---|---|
| Harris et al | 37.06 (9.5) | 52 | cGVHD after HSCT | |
| Andrykowski et al | 35.9 (8.6) | 662 | 0.25 | HSCT survivors |
| Robb et al | 33.46 (6.11) | 127 | 0.0059 | Breast cancer survivors |
| Tate et al | 38.5 (7.8) | 208 | 0.76 | Breast Cancer (terminal patients excluded) |
| Cotton et al | 28.34 (9.24) | 142 | <0.0001 | Breast Cancer-diagnosed within the last 18 months |
| Peterman et al | 38.5 (8.1) | 1617 | 0.76 | Cancer - All types |
| Daugherty et al | 40.7 (7.2) | 162 | 0.09 | Advanced Cancer and participating in Phase I Trials |
Discussion
We set out to describe the extent to which Sp-WB influenced QOL in the current cGVHD population. Additionally, we sought to examine demographic and clinical predictors of QOL that would predispose an individual to rely more or less on spirituality as a coping mechanism. Furthermore, it was of interest to investigate the subset of the current population who reported extremely low Sp-WB and to observe any significant differences between this group and those individuals who reported higher Sp-WB.
We found that Sp-WB scores for patients in our population were comparable to similar cancer and transplant populations studied previously with the exception of two studies investigating breast cancer. The majority of the current population presents with multi-system organ involvement as well as suffers from severe physical and functional limitations; yet, it is remarkable to note that these individuals exhibited one of the highest averages for Sp-WB. This observation could be due to several possibilities including an increased connection with spiritual resources or from patient habituation to coping with a chronic, life threatening illness that has allowed them to accommodate better to their condition. Our second question inquired as to whether there were any demographic or clinical features that would be predictive of a higher or lower Sp-WB score. The statistical analysis demonstrated that no relationship existed between demographic or clinical variables. While this result does not confirm the findings of previous studies performed in other patient populations, 12, 34 it may suggest that HSCT survivor’s QOL is dictated by the course of the disease rather than by any demographic or clinical features of the individual. It may also be a reflection of the intrinsic inability of the current cGVHD severity assessment scales to separate signs of active disease from the inactive end-stage organ manifestations.
Next, we compared the Sp-WB scores to the core subscales of the FACT-G. Interestingly, we found that patients in the higher range of Sp-WB were associated with higher scores in each of the four traditional subscales as well as the total QOL score. Therefore, patients with higher Sp-WB scores also experience a higher QOL in general. Although the majority of the patient’s Sp-WB scores trended toward the upper end of the range, it was interesting to document a subset of the population that demonstrated extremely low satisfaction with their Sp-WB. These individuals also expressed significantly lower scores in each of the core subscales when compared with the participants that exhibited higher Sp-WB. Yet, there was no significant difference observed in GVHD CAS scores, which indicates the extent of involvement of GVHD, between the groups. Therefore, the severity of the disease does not appear to provide an explanation for the relatively preserved QOL observed.
There were several limitations to the current study that are worth noting. First, we were limited to a small population size of fifty-two patients. In addition, our population was not completely representative of all ethnic or religious factors that may have accounted for Sp-WB. Consequently, the current research has revealed several lines of inquiry that should be explored in future studies. Future research may wish to investigate other clinical and demographic parameters to evaluate the significance of and to identify additional predictors. The development of an alternate hypothesis that can account for the discrepancy between individuals with high and low Sp-WB should become a priority for future investigation. Furthermore, projects seeking to evaluate Sp-WB in patients with chronic, life threatening illness may wish to expand upon the current study by investigating a longitudinal sample with an increase in the number of participants.
Due to the emergence of spirituality as a coping mechanism and its subsequent efficacy in improving QOL, interventions designed to enhance Sp-WB must be identified. Several recent reports have described interventions intended to strengthen Sp-WB including a mindfulness-based stressed reduction and healing arts35 prayer, spiritual healing and meditation36 and meaning making interventions37,38 The development of protocols designed to promote Sp-WB will encourage patients to confront their spiritual questions and may give them new perspective on the value and meaning of their life. Hopefully, this newfound outlook on life will translate to improved QOL.
Sp-WB has been increasingly noted as a major coping resource for patients with cancer and other chronic life, threatening illnesses; therefore, more research must be completed to elucidate the value of including the construct into future QOL studies. The current study demonstrates the importance of educating clinicians who are treating patients with chronic, life threatening illness on the benefit that cultivation of Sp-WB can have on QOL. Accordingly, clinicians must recognize the value of encouraging their patients to explore and confront the many existential and spiritual issues that are raised by dealing with their illness. As shown by the current study, patient optimization of their Sp-WB could contribute to improving overall QOL. With further investigation into the impact that Sp-WB can have to enhance patient QOL, the medical community can develop interventional programs aimed at identifying and supporting a patient’s spiritual needs.
Acknowledgments
This work was supported in part by the National Cancer Institute’s intramural program – Center for Cancer Research.
Footnotes
Disclaimer: The statements presented in this article are of the authors and do not represent the opinion of the NIH, NCI or the US government.
References
- 1.Andrykowski M, Bishop M, Hahn E, et al. Long-Term Health-Related Quality of Life, Growth, and Spiritual Well-being After Hematopoietic Stem Cell Transplantation. Journal of Clinical Oncology. 2005;23(3):599–608. doi: 10.1200/JCO.2005.03.189. [DOI] [PubMed] [Google Scholar]
- 2.Bishop M, Beaumont J, Hahn E, et al. Late Effects of Cancer and Hematopoietic Stem-Cell Transplantation on Spouses or Partners Compared With Survivors and Survivors-Matched Controls. Journal of Clinical Oncology. 2007;25:1403–1411. doi: 10.1200/JCO.2006.07.5705. [DOI] [PubMed] [Google Scholar]
- 3.Fraser C, Bhatia S, et al. Impact of chronic graft-versus-host disease of the health status of hematopoietic cell transplantation survivors: a report from the Bone Marrow Transplant Survivor Study. Blood. 2006;108(8):2867–2873. doi: 10.1182/blood-2006-02-003954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lee SJ, Kim HT, Ho VT, et al. Quality of life associated with acute and chronic graft-versus-host disease. Bone Marrow Transplantation. 2006:1–6. doi: 10.1038/sj.bmt.1705434. [DOI] [PubMed] [Google Scholar]
- 5.Lee SJ, Klein JP, Barrett J, et al. Severity of chronic graft versus host disease: association with treatment-related mortality and relapse. Blood. 2002;100:406–414. doi: 10.1182/blood.v100.2.406. [DOI] [PubMed] [Google Scholar]
- 6.Shlomchik WD, Lee SJ, Couriel D, Pavletic SZ. Transplantation’s greatest challenges: advances in chronic graft-versus-host disease. Biology of Blood and Bone Marrow Transplantation. 2007;13(1 Suppl 1):2–10. doi: 10.1016/j.bbmt.2006.10.020. [DOI] [PubMed] [Google Scholar]
- 7.Lowe T, Bhatia S, Somlo G. Second malignancies after allogeneic hematopoietic cell transplantation. Biology of Blood and Bone Marrow Transplantation. 2007;13(10):1121–1134. doi: 10.1016/j.bbmt.2007.07.002. [DOI] [PubMed] [Google Scholar]
- 8.Hills JJ, Paice A, et al. Spirituality and distress in palliative care consultation. Journal of Palliative Medicine. 2005;8(4):782–8. doi: 10.1089/jpm.2005.8.782. [DOI] [PubMed] [Google Scholar]
- 9.Lin HR, Bauer-Wu SM. Psycho-spiritual well-being in patients with advanced cancer: an integrative review of the literature. Journal of Advanced Nursing. 2003;44(1):69–80. doi: 10.1046/j.1365-2648.2003.02768.x. [DOI] [PubMed] [Google Scholar]
- 10.Cotton S, Levine E, Fitzpatrick C, Dold K, Targ E. Exploring the Relationships Among Spiritual Well-Being, Quality of Life, and Psychological Adjustment in Women With Breast Cancer. Psycho-Oncology. 1999;8:429–438. doi: 10.1002/(sici)1099-1611(199909/10)8:5<429::aid-pon420>3.0.co;2-p. [DOI] [PubMed] [Google Scholar]
- 11.Brady M, Peterman A, Fitchett G, Mo M, Cella D. A Case for Including Spirituality in Quality of Life Measurements in Oncology. Psycho-Oncology. 1999;8:417–428. doi: 10.1002/(sici)1099-1611(199909/10)8:5<417::aid-pon398>3.0.co;2-4. [DOI] [PubMed] [Google Scholar]
- 12.Mystakidou K, Tsilika E, Parpa, et al. Assessing Spirituality and Religiousness in Advanced Cancer Patients. American Journal of Hospice and Palliative Medicine. 2007;23(6):457–463. doi: 10.1177/1049909106294880. [DOI] [PubMed] [Google Scholar]
- 13.Nelson CJ, Rosenfeld B, et al. Spirituality, religion, and depression in the terminally ill. Psychosomatics. 2002;43(3):213–20. doi: 10.1176/appi.psy.43.3.213. [DOI] [PubMed] [Google Scholar]
- 14.Peterman A, Fitchett G, Brady M, Hernandez L, Cella D. Measuring Spiritual Well-Being in People With Cancer: The Functional Assessment of Chronic Illness Therapy- Spiritual Well-Being Scale (FACIT-Sp) Annals of Behavioral Medicine. 2002;24(1):49–58. doi: 10.1207/S15324796ABM2401_06. [DOI] [PubMed] [Google Scholar]
- 15.Delgado C. Sense of Coherence, Spirituality, Stress and Quality of Life in Chronic Illness. Journal of Nursing Scholarship. 2007;39 (3):229–234. doi: 10.1111/j.1547-5069.2007.00173.x. [DOI] [PubMed] [Google Scholar]
- 16.Clarke J. A discussion paper about ‘meaning’ in the nursing literature on spirituality: an interpretation of meaning as “ultimate concern” using the work of Paul Tillich. International Journal of Nursing Studies. 2006;44(4):645–646. doi: 10.1016/j.ijnurstu.2006.05.005. [DOI] [PubMed] [Google Scholar]
- 17.McGrath P. Positive outcomes for survivors of haematological malignancies from a spiritual perspective. International Journal of Nurse. 2004;10(6):280–291. doi: 10.1111/j.1440-172x.2004.00490.x. [DOI] [PubMed] [Google Scholar]
- 18.Mahoney MJ, Graci GM. The meanings and correlates of spirituality: suggestions from an exploratory survey of experts. Death Studies. 1999;23(6):521–528. doi: 10.1080/074811899200867. [DOI] [PubMed] [Google Scholar]
- 19.Levine EG, Yoo G, Aviv C, Ewing C, Au A. Ethnicity and spirituality in breast cancer survivors. Journal of Cancer Survivorship. 2007;1(3):212–225. doi: 10.1007/s11764-007-0024-z. [DOI] [PubMed] [Google Scholar]
- 20.Mount BM, Boston PH, Cohen SR. Healing connections: on moving from suffering to a sense of well-being. Journal of Pain Symptom Management. 2007;33(4):372–388. doi: 10.1016/j.jpainsymman.2006.09.014. [DOI] [PubMed] [Google Scholar]
- 21.George LK, Larson DB, Koenig HG, McCullough ME. Spirituality and health: What we know, what we need to know. Journal of Social and Clinical Psychology. 2000;19(102):102–116. [Google Scholar]
- 22.Breitbart W. Spirituality and meaning in supportive care: spirituality- and meaning-centered group psychotherapy interventions in advanced cancer. Support Care Cancer. 2002;10(4):272–80. doi: 10.1007/s005200100289. [DOI] [PubMed] [Google Scholar]
- 23.Edmonson D, Park C, Blank T, Fenster J, Mills M. Deconstructing spiritual well-being: existential well-being and HRQOL in cancer survivors. Psycho-Oncology. 2008;17(2):161–169. doi: 10.1002/pon.1197. [DOI] [PubMed] [Google Scholar]
- 24.Bekelman D, Dy S, Becker D, et al. Spiritual Well-Being and Depression in Patients with Heart Failure. Journal of General Internal Medicine. 2007;22:470–477. doi: 10.1007/s11606-006-0044-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Sherman DW, Ye XY, et al. Spiritual well-being as a dimension of quality of life for patients with advanced cancer and AIDS and their family caregivers: results of a longitudinal study. American Journal of Hospice and Palliative Care. 2005;22(5):349–62. doi: 10.1177/104990910502200508. [DOI] [PubMed] [Google Scholar]
- 26.Tsevat J. Spirituality/Religion and Quality of Life in Patients with HIV/AIDS. Journal of General Internal Medicine. 2006;21:S1–S2. [Google Scholar]
- 27.Martin PJ, Weisdorf D, Przepiorka D, et al. National Institutes of Health Consensus Development Project on Criteria for Clinical Trials in Chronic Graft-versus-Host Disease: VI. Design of Clinical Trials Working Group report. Biology of Blood and Bone Marrow Transplantation. 2006;12(5):491–505. doi: 10.1016/j.bbmt.2006.03.004. [DOI] [PubMed] [Google Scholar]
- 28.Webster K, Cella D, Yost K. The Functional Assessment of Chornic Illness Therapy (FACIT) Measurement System: properties, applications, and interpretation. Health and Quality of Life Outcomes. 2003;1(79):1–7. doi: 10.1186/1477-7525-1-79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Lee SJ, Cook EF, Soiffer R, Antin JH. Development and validation of a scale to measure symptoms of chronic graft-versus-host disease. Biology of Blood and Bone Marrow Transplantation. 2002;8(8):444–452. doi: 10.1053/bbmt.2002.v8.pm12234170. [DOI] [PubMed] [Google Scholar]
- 30.Hollander M, Wolfe DA. Nonparametric Statistical Methods, Second Edition. New York: John Wiley and Sons, Inc; 1999. pp. 189–269. [Google Scholar]
- 31.Agresti A. Categorical Data Analysis. New York: John Wiley and Sons, Inc; 1990. pp. 79–129. [Google Scholar]
- 32.Brucker PS, Yost K, Cashy J, Webster K, Cella D. General Population and Cancer Patient Norms for the Functional Assessment of Cancer Therapy–General (FACT-G) Evaluation and the Health Professions. 2005;28(2):192–211. doi: 10.1177/0163278705275341. [DOI] [PubMed] [Google Scholar]
- 33.Robb C, Haley W, Balducci L, et al. Impact of breast cancer survivorship on quality of life in older women. Critical Reviews in Oncology and Hematology. 2006;62(1):84–91. doi: 10.1016/j.critrevonc.2006.11.003. [DOI] [PubMed] [Google Scholar]
- 34.Wan G, Counte M, Cella D, et al. An Analysis of the Impact of Demographic, Clinical, and Social Factors on Health-Related Quality of Life. Value in Health. 1999;2(4):308–318. doi: 10.1046/j.1524-4733.1999.24006.x. [DOI] [PubMed] [Google Scholar]
- 35.Garland SN, Carlson LE, Cook S, Lansdell L, Speca M. A non-randomized comparison of mindfulness-based stress reduction and healing arts programs for facilitating post-traumatic growth and spirituality in cancer outpatients. Supportive Care Cancer. 2007;15(8):949–961. doi: 10.1007/s00520-007-0280-5. [DOI] [PubMed] [Google Scholar]
- 36.Taylor EJ. Spiritual complementary therapies in cancer care. Seminars in Oncology Nursing. 2005;21(3):159–63. doi: 10.1016/j.soncn.2005.04.003. [DOI] [PubMed] [Google Scholar]
- 37.Lee V. The existential plight of cancer: meaning making as a concrete approach to the intangible search for meaning. Supportive Care Cancer. 2008 doi: 10.1007/s00520-007-0396-7. [E-pub Ahead of Print] [DOI] [PubMed] [Google Scholar]
- 38.Chochinov HM, Hack T, Hassard T, et al. Dignity therapy: a novel psychotherapeutic intervention for patients near the end of life. Journal of Clinical Oncology. 2005;23(24):5427–5428. doi: 10.1200/JCO.2005.08.391. [DOI] [PubMed] [Google Scholar]
- 39.Tate DG, Forchheimer M. Quality of Life, Life Satisfaction, and Spirituality. American Journal of Physical Medicine and Rehabilitation. 2002;81(6):400–410. doi: 10.1097/00002060-200206000-00002. [DOI] [PubMed] [Google Scholar]
- 40.Daugherty C, Fitchett G, et al. Trusting God and Medicine: Spirituality in advanced cancer patients volunteering for clinical trials of experimental agents. Psycho-oncology. 2004;14:135–146. doi: 10.1002/pon.829. [DOI] [PubMed] [Google Scholar]