Abstract
Context
The current state of palliative care in cancer centers is not known.
Objective
We conducted a survey to determine the availability and degree of integration of palliative care services, and to compare between National Cancer Institute (NCI) and non-NCI cancer centers in the United States.
Design, Setting, and Participants
Between June and October 2009, we surveyed both executives and palliative care clinical program leaders, where applicable, of 71 NCI cancer centers and a random sample of 71 non-NCI centers regarding their palliative care services. Executives were also asked about their attitudes toward palliative care.
Main Outcome Measure
Availability of palliative care services in the cancer center, defined as the presence of at least one palliative care physician.
Results
We sent 142 and 120 surveys to executives and program leaders, with response rates of 71% and 82%, respectively. NCI cancer centers were significantly more likely to have a palliative care program (50/51 (98%) vs. 39/50 (78%), P=0.002), at least one palliative care physician (46/51 (90%) vs. 28/50 (56%), P=0.04), an inpatient palliative care consultation team (47/51 (92%) vs. 28/50 (56%), P<0.001), and an outpatient palliative care clinic (30/51 (59%) vs. 11/50 (22%), P<0.001). Few centers had dedicated palliative care beds (23/101 (23%)) or an institution-operated hospice (37/101 (36%)). The median reported durations from referral to death were 7 (Q1–Q3 4–16), 7 (Q1–Q3 5–10), and 90 (Q1–Q3 30–120) days for inpatient consultation teams, inpatient units, and outpatient clinics, respectively. Research programs, palliative care fellowships, and mandatory rotations for oncology fellows were uncommon. Executives were supportive of stronger integration and increasing palliative care resources.
Conclusion
Most cancer centers reported a palliative care program, although the scope of services and the degree of integration varied widely. Further efforts to consolidate existing infrastructure and to integrate palliative care in cancer centers are warranted.
INTRODUCTION
While significant progress has been made in cancer treatment, approximately half of all cancer patients eventually die of their disease, and one third of cancer deaths happen within 6 months of diagnosis.1 Palliative care outpatient clinics, inpatient consultation teams, palliative care units (PCUs) and hospices all play an integral role providing symptom control, psychosocial support and transition of care for cancer patients and their families along the cancer care continuum. Based on this understanding, multiple national and international organizations support early incorporation of palliative care into oncology practice.2–5 Most recently, the American Society of Clinical Oncology (ASCO) has taken a step further to support full integration of palliative care as a routine part of comprehensive cancer care in the United States (US) by 2020.6
The understanding that palliative care is most effective when incorporated early in oncology care led to the development of the comprehensive cancer care model, which integrates palliative care along with anticancer therapy from the time of diagnosis.7, 8 The current state of palliative care availability and degree of integration of palliative care services into oncology practice at various cancer centers in the US is unknown. Many cancer centers claim that they provide palliative care, although the structures, processes, and outcomes for their programs remain unclear. A more thorough picture of the level of palliative care that currently exists in these cancer centers would allow us to identify deficiencies and barriers to comprehensive cancer care, and to develop specific strategies to improve care delivery. In this survey study, we aimed to determine the availability and degree of integration of palliative care services in US cancer centers, as well as their executives’ attitudes toward palliative care. We also compared palliative care services of National Cancer Institute (NCI)-designated cancer centers with those of non-NCI cancer centers.
PATIENTS AND METHODS
Survey Development
The Institutional Review Board at The University of Texas M. D. Anderson Cancer Center approved this study and waived the requirement for review and informed consent. Survey questions were generated after a comprehensive literature search, review of guidelines from the National Quality Forum,9, 10 and discussions among seven physicians (four medical oncologists, three palliative care specialists) with research interest in palliative oncology. Survey questions were generated based on the Donabedian tripartite division of structure, processes, and outcomes to evaluate the administrative, clinical, education, and research aspects of palliative care in cancer centers (eTable 1),11 and subsequently reviewed for readability and face validity. The surveys were further revised by our institutional Patient-Reported Outcomes, Survey and Population Research (PROSPR) Shared Resource. Three physicians (DH, MDLC, DSZ) tested the final version of the surveys, and assessed the time required for completion.
Table 1.
Attitudes of Cancer Center Executives towards Palliative Care
| Program Effectiveness 5 Years Ago |
Program Effectiveness Now |
P- valueb |
|||||
|---|---|---|---|---|---|---|---|
| N | % | 95% CI (%) | N | % | 95% CI (%) | ||
| NCI Cancer Centers | |||||||
| Pain management services | N=51a | N=51a | |||||
| Good or Excellent (7–10) | 25 | 49 | 35–63 | 45 | 88 | 78–97 | |
| Neutral (4–6) | 20 | 39 | 26–54 | 5 | 10 | 3–22 | <0.001 |
| Poor (0–3) | 6 | 12 | 4–24 | 1 | 2 | 0–11 | |
| Unknown or not answered | 0 | 0 | |||||
| Palliative care services | |||||||
| Good or Excellent (7–10) | 15 | 30 | 18–45 | 40 | 80 | 68–91 | |
| Neutral (4–6) | 13 | 26 | 15–40 | 10 | 20 | 10–34 | <0.001 |
| Poor (0–3) | 22 | 44 | 30–59 | 0 | 0 | - | |
| Unknown or not answered | 1 | 1 | |||||
| Non-NCI Cancer Centers | |||||||
| Pain management services | N=50a | N=50a | |||||
| Good or Excellent (7–10) | 18 | 39 | 25–54 | 37 | 77 | 63–88 | |
| Neutral (4–6) | 24 | 52 | 36–66 | 11 | 23 | 12–37 | <0.001 |
| Poor (0–3) | 4 | 9 | 2–20 | 0 | 0 | - | |
| Unknown or not answered | 4 | 2 | |||||
| Palliative care services | |||||||
| Good or Excellent (7–10) | 9 | 20 | 10–35 | 27 | 57 | 42–72 | |
| Neutral (4–6) | 20 | 46 | 30–60 | 16 | 34 | 21–49 | <0.001 |
| Poor (0–3) | 15 | 34 | 20–49 | 4 | 9 | 2–20 | |
| Unknown or not answered | 6 | 3 | |||||
|
NCI Cancer Centers N=51a |
Non-NCI Cancer Centers N=50a |
||||||
|
A stronger integration of palliative care services into oncology practice will benefit patients at my institution |
N | % | 95% CI (%) | N | % | 95% CI (%) | |
| Agree or strongly agree (7–10) | 46 | 90 | 79–97 | 44 | 92 | 80–98 | |
| Neutral (4–6) | 4 | 8 | 2–19 | 4 | 8 | 2–20 | <0.99 |
| Disagree or strongly disagree (0–3) | 1 | 2 | 0–10 | 0 | 0 | - | |
| Unknown or not answered | 0 | 2 | |||||
|
More research funding should be directed towards palliative care services |
|||||||
| Agree or strongly agree (7–10) | 43 | 84 | 71–93 | 39 | 81 | 67–91 | |
| Neutral (4–6) | 6 | 12 | 4–24 | 9 | 19 | 9–33 | 0.28 |
| Disagree or strongly disagree (0–3) | 2 | 4 | 0–13 | 0 | 0 | - | |
| Unknown or not answered | 0 | 2 | |||||
|
My institution will be increasing the number of palliative care physicians over the next 5 years |
|||||||
| Agree or strongly agree (7–10) | 28 | 56 | 41–70 | 12 | 25 | 14–40 | |
| Neutral (4–6) | 20 | 40 | 26–55 | 28 | 60 | 44–74 | 0.005 |
| Disagree or strongly disagree (0–3) | 2 | 4 | 0–14 | 7 | 15 | 6–28 | |
| Unknown or not answered | 1 | 3 | |||||
|
My institution will be increasing the number of palliative care mid- level providers over the next 5 years |
|||||||
| Agree or strongly agree (7–10) | 30 | 59 | 44–72 | 15 | 33 | 20–48 | |
| Neutral (4–6) | 18 | 35 | 22–50 | 28 | 61 | 45–75 | 0.03 |
| Disagree or strongly disagree (0–3) | 3 | 6 | 1–16 | 3 | 7 | 1–18 | |
| Unknown or not answered | 0 | 4 | |||||
|
My institution will be increasing the number of palliative care staff nurses over the next 5 years |
|||||||
| Agree or strongly agree (7–10) | 26 | 52 | 37–66 | 13 | 27 | 15–42 | |
| Neutral (4–6) | 21 | 42 | 28–57 | 31 | 65 | 49–78 | 0.04 |
| Disagree or strongly disagree (0–3) | 3 | 6 | 1–17 | 4 | 8 | 2–20 | |
| Unknown or not answered | 1 | 2 | |||||
|
My institution will be increasing the number of palliative care acute beds over the next 5 years |
|||||||
| Agree or strongly agree (7–10) | 16 | 33 | 20–48 | 8 | 17 | 7–30 | |
| Neutral (4–6) | 20 | 41 | 27–56 | 28 | 58 | 43–72 | 0.14 |
| Disagree or strongly disagree (0–3) | 13 | 27 | 15–41 | 12 | 25 | 14–40 | |
| Unknown or not answered | 2 | 2 | |||||
|
My institution will be increasing the funding for palliative care over the next 5 years |
|||||||
| Agree or strongly agree (7–10) | 22 | 44 | 30–59 | 11 | 23 | 12–37 | |
| Neutral (4–6) | 26 | 52 | 37–66 | 29 | 60 | 45–74 | 0.03 |
| Disagree or strongly disagree (0–3) | 2 | 4 | 0–14 | 8 | 17 | 7–30 | |
| Unknown or not answered | 1 | 2 | |||||
Abbreviations: CI, confidence interval; NCI, National Cancer Institute
Total number of respondents
Comparisons were made between NCI and non-NCI cancer centers using the Fisher’s exact test. Confidence intervals were computed using the exact binominal test. Missing values were not included in the analyses.
Two surveys were utilized in this study. The first survey consisted of 22 questions and was directed to cancer center executives (eSurvey 1). This survey provided information regarding access to and attitudes toward palliative care. The second 74-question survey was sent only to cancer centers with palliative care programs (eSurvey 2). This survey asked palliative care program leaders details about their programs, including personnel, inpatient PCUs, consultation teams, outpatient clinics, hospice, and educational and research activities.
Cancer Centers
Cancer centers in the US were identified by using the Commission of Cancer (CoC) database. The CoC accredits hospitals as cancer centers based on 36 standards that encompass a range of clinical, research, and quality improvement aspects of cancer care.12 We obtained a list of 1482 CoC-accredited cancer centers, which represent approximately 30% of all American hospitals and provide services to approximately 70% of patients with new cancer diagnoses.13 Among these institutions, 71 were NCI-designated centers (40 NCI-designated comprehensive cancer centers, 15 NCI clinical cancer centers, and 16 NCI community cancer centers). The NCI designation is based on scientific excellence related to cancer prevention, diagnosis and treatment, and does not bear any specific reference to the quality of patient care or palliative care research. NCI-designated cancer centers are widely recognized as leading institutions in the US, and represent a well-defined cohort in previous studies.14 We surveyed all 71 NCI-designated cancer centers and a sample of 71 of 1411 non-NCI cancer centers using a simple randomization scheme.
Survey Process
We determined the names and contact information of cancer center executives through the CoC and NCI website, with independent verification through telephone contact. Information on palliative care program leaders was identified by calling the palliative care department directly. All respondents received an initial invitation with a mail survey, along with a $10 gift certificate. They or their delegates were asked to complete the survey anonymously and to return it by mail, fax or electronically through a secured website. A reminder letter was sent to non-respondents at 2 weeks and 4 weeks, followed by a phone or e-mail reminder at 8 weeks. Data collection was performed between June and October 2009.
Response Rate Calculation
Response rates were determined following the metrics of the American Association for Public Opinion Research.15 The formula for calculation is shown here:
Response rate = (complete responses + partial responses)/(complete responses + partial responses + non-response + explicit refusals + implicit refusals)
In this study, a complete response was defined as >80% of questions answered, a partial response as <80% of questions answered and completion of the key question in the corresponding survey regarding the availability of palliative care (Question IIB for the executive survey and Question IB for the palliative care program leader survey), and non-response as not answering the key question. Three of 120 palliative care program leader surveys sent were later found to be ineligible due to absence of palliative care programs in those centers, and were not included in the analysis.
Statistical Analysis
Our primary outcome was the availability of palliative care services in the cancer center, defined as the presence of at least one physician with dedicated time to the provision of palliative care (with or without board certification). We compared the proportions of NCI and non-NCI cancer centers that met this criterion using a binomial test. Given that we surveyed 71 NCI cancer centers and 71 non-NCI cancer centers with an anticipated response rate of 65% (therefore 46 evaluable NCI centers and 46 evaluable non-NCI cancer centers), we were able to declare as statistically significant a difference of 28% between groups, assuming a two-sided significance level of 0.05 and 80% power.
We summarized the availability of various types of palliative care services at different cancer centers using standard descriptive statistics, including medians, interquartile ranges, proportions, and frequencies, together with 95% confidence intervals where appropriate. Differences in services provided between NCI-designated cancer centers and non-NCI centers were computed using Fisher’s exact tests for categorical variables. The Mann-Whitney test was used for nonparametric continuous variables. A P-value of <0.05 was considered to be statistically significant.
The Statistical Package for the Social Sciences (SPSS version 16.0, SPSS Inc., Chicago, Illinois) software and STATA (version 10.0, College Station, Texas) were used for statistical analysis.
RESULTS
Response Rates
Among the 140 executive surveys sent, we had 89 (63%) complete responses, 12 (8%) partial responses, 40 (28%) implicit refusals and 1 (1%) explicit refusal. The response rate was 101/140 (72%), and did not differ by cancer center type (NCI vs. non-NCI) nor whether the center had a palliative care program based on independent phone verification.
Among the 120 palliative care program leader surveys sent, the number of complete responses, partial responses, implicit refusals, explicit refusals and ineligible cases were 86 (72%), 10 (8%), 21 (15%), 0 (0%) and 3 (2%), respectively. The response rate was 96/117 (82%). Palliative care program leaders from NCI cancer centers were more likely than those from non-NCI centers to respond (61/67 (91%) vs. 35/50 (70%), p=0.007).
We did not detect any differences in CoC center type between the non-NCI cancer centers that were surveyed and those not surveyed (p=0.98).
Perceived Barriers and Attitudes towards Palliative Care
The barriers to delivery of palliative care identified by cancer center executives are shown in Figure 1. Poor reimbursement and limited institutional resources were the most commonly cited reasons. A small number of executives were concerned that the presence of palliative care could negatively affect their hospital mortality rate and national rating.
Figure 1. Perceived Barriers to Palliative Care Access According to Cancer Center Executives.
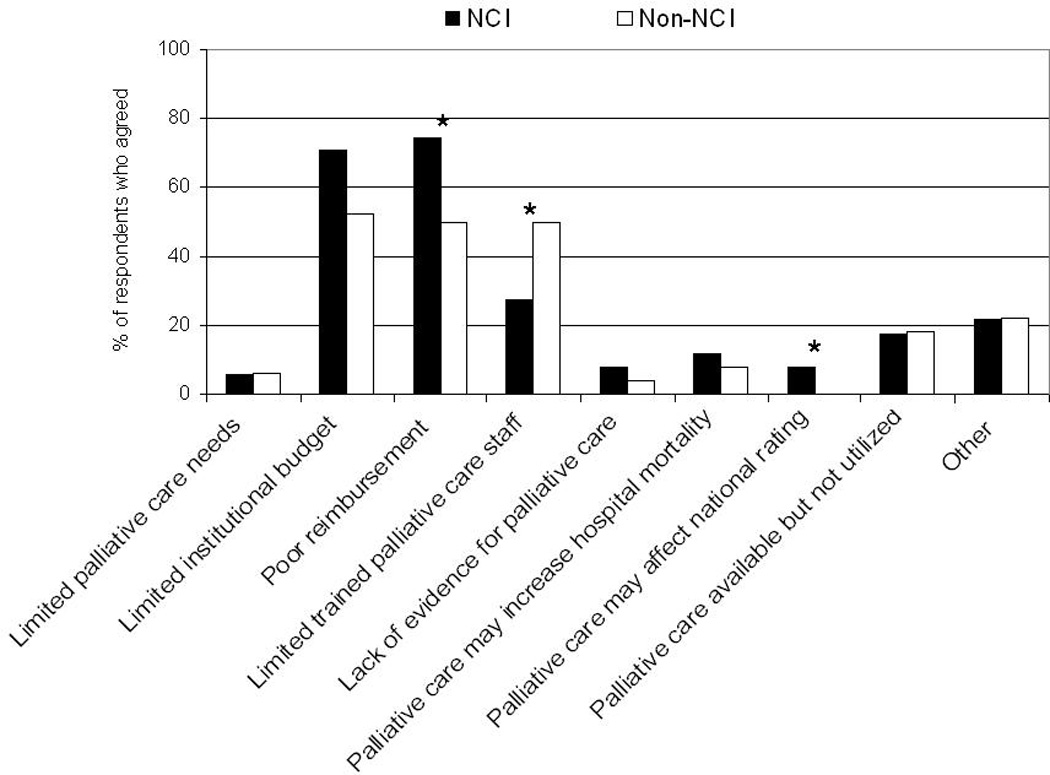
Perceived barriers to palliative care access based on the question “Irrespective of whether palliative care is offered at your institution, what in your opinion, are some of the potential barriers to palliative care access for your institution? (check all that apply)”. All 51 NCI and all 50 non-NCI executives who responded to the survey completed this question. *P<0.05
Cancer center executives rated their current pain and palliative care services favorably, and reported a significant improvement compared to 5 years ago (Table 1). Importantly, they strongly agreed that further integration of palliative care services into oncology practice will benefit patients, and that more funding should be directed toward palliative care research (Table 1). NCI cancer center executives were significantly more likely than their non-NCI cancer center counterparts to agree with an increase in palliative care resources at their institutions over the next 5 years.
Availability of Palliative Care Programs
A majority of responding cancer center executives reported an active palliative care program (Table 2). Compared to non-NCI cancer centers, NCI-designated cancer centers were significantly more likely to provide palliative care services, to have at least one palliative care physician, an inpatient consultation team and an outpatient clinic. Fewer centers had dedicated acute palliative care beds or an institution-operated hospice.
Table 2.
Availability of Palliative Care Programs According to Cancer Center Executives
| NCI Cancer Centers (N=51)a |
Non-NCI Cancer Centers (N=50)a |
P-valueb | |||||||
|---|---|---|---|---|---|---|---|---|---|
|
Cancer Center Characteristics |
N | % | 95% CI (%)c | N | % | 95% CI (%)c | |||
| Type of Cancer Center | |||||||||
| NCI-designated Comprehensive Cancer Center | 31 | 61 | 46–74 | 0 | 0 | - | |||
| NCI-designated Clinical Cancer Center | 11 | 21 | 11–35 | 0 | 0 | - | - | ||
| NCI-designated Community Cancer Center | 9 | 18 | 8–31 | 0 | 0 | - | |||
| Non NCI-designated Cancer Center | 0 | 0 | - | 50 | 100 | 93–100 | |||
| Unknown or not answered | 0 | 0 | |||||||
| Number of outpatients in 2008 (Q1–Q3) |
10000 | (2500–55000) | 3002 | (800–8400) | 0.01 | ||||
| Unknown or not answered | 12 | 16 | |||||||
| Inpatient beds available | 41 | 87 | 74–95 | 30 | 67 | 51–80 | 0.02 | ||
| Unknown or not answered | 4 | 5 | |||||||
| Number of inpatient beds (Q1–Q3)d |
80 | (44–400) | 52 | (20–300) | 0.22 | ||||
| Unknown or not answered | 13 | 23 | |||||||
| Palliative Care Program | |||||||||
| Available anytime over the last 10 years |
50 | 98 | 90–100 | 39 | 78 | 64–88 | 0.002 | ||
| Unknown or not answered | 0 | 0 | |||||||
| Currently active | 50 | 98 | 90–100 | 39 | 78 | 64–88 | 0.002 | ||
| Unknown or not answered | 0 | 0 | |||||||
| Palliative care physician present |
46 | 92 | 79–97 | 28 | 74 | 57–87 | 0.04 | ||
| Unknown or not answered | 1 | 12 | |||||||
| Palliative Care Infrastructure | |||||||||
| Inpatient consultation team | 47 | 92 | 81–98 | 28 | 56 | 41–70 | <0.001 | ||
| Unknown or not answered | 0 | 0 | |||||||
| Outpatient clinic | 30 | 59 | 44–72 | 11 | 22 | 12–36 | <0.001 | ||
| Unknown or not answered | 0 | 0 | |||||||
| Dedicated palliative care acute care beds |
13 | 26 | 14–40 | 10 | 20 | 10–34 | 0.64 | ||
| Unknown or not answered | 0 | 0 | |||||||
| Institution-operated hospice |
16 | 31 | 19–46 | 21 | 42 | 28–57 | 0.31 | ||
| Unknown or not answered | 0 | 0 | |||||||
Abbreviations: CI, confidence interval; NCI, National Cancer Institute; Q1–Q3, interquartile range
Total number of respondents
Comparisons were made between NCI and non-NCI cancer centers using the Fisher’s exact test for categorical variables, and the Mann-Whitney test for continuous variables. Confidence intervals were computed using the exact binominal test. Missing values were not included in the analyses.
Unless stated otherwise
Among centers with inpatient units only
Palliative Care Clinical Services
Table 3 provides an overview of existing palliative care programs based on information provided by palliative care program leaders, including the range of services and personnel. Palliative care services have been in place at NCI cancer centers longer than at non-NCI cancer centers. Importantly, a majority of programs reported a short patient follow-up duration of less than 1 month.
Table 3.
Palliative Care Program Characteristics According to Palliative Care Program Leaders
| NCI Cancer Centers (N=61)a |
Non-NCI Cancer Centers (N=35)a |
P- valueb |
|||||
|---|---|---|---|---|---|---|---|
| N | % | 95% CI (%)c | N | % | 95% CI (%)c |
||
|
Time from Palliative Care Program Activation |
|||||||
| >5 years | 30 | 51 | 37–64 | 9 | 27 | 13–46 | 0.03 |
| Unknown or not answered | 2 | 2 | |||||
| Estimated Patient Follow-up Time | |||||||
| 1–7 days | 20 | 34 | 22–47 | 14 | 43 | 25–61 | |
| >1–4 weeks | 17 | 28 | 17–41 | 8 | 24 | 11–42 | |
| >1–12 months | 17 | 28 | 17–41 | 9 | 27 | 13–46 | 0.85 |
| >1 year | 6 | 10 | 4–21 | 2 | 6 | 1–20 | |
| Unknown or not answered | 1 | 2 | |||||
|
Professional Background of Palliative Care Leaderd |
|||||||
| Medical Oncology | 10 | 17 | 8–29 | 6 | 18 | 7–35 | >0.99 |
| Palliative Medicine | 32 | 53 | 40–66 | 6 | 18 | 7–35 | 0.001 |
| Nursing | 5 | 8 | 3–18 | 10 | 30 | 16–49 | 0.009 |
| Unknown or not answered | 1 | 2 | |||||
| Palliative Care Physician | |||||||
| Number of full-time equivalent positions, median (Q1–Q3) |
1 | (1–2) | 1 | (0–2) | 0.07 | ||
| Unknown or not answered | 4 | 3 | |||||
| Number of physicians with at least 20% of protected time, median (Q1–Q3) |
0 | (0–1.5) | 0 | 0 | 0.047 | ||
| Unknown or not answered | 1 | 2 | |||||
| Professional Requirement | |||||||
| Board certification for physicianse | 34 | 57 | 43–69 | 15 | 45 | 28–64 | 0.39 |
| Unknown or not answered | 1 | 2 | |||||
| Board certification for nursesf | 19 | 32 | 20–45 | 8 | 24 | 11–42 | 0.49 |
| Unknown or not answered | 1 | 2 | |||||
| Palliative Care Servicesd | |||||||
| Assessment and management of psychiatric disorders |
29 | 48 | 35–62 | 11 | 33 | 18–52 | 0.193 |
| Unknown or not answered | 1 | 2 | |||||
| Obtaining advanced directives/DNR orders |
54 | 90 | 79–96 | 29 | 88 | 72–97 | 0.817 |
| Unknown or not answered | 1 | 2 | |||||
| Ethical issues | 44 | 73 | 60–84 | 29 | 88 | 72–97 | 0.121 |
| Unknown or not answered | 1 | 2 | |||||
| Referrals to hospice, home care and other placements |
55 | 92 | 82–97 | 30 | 91 | 76–98 | >0.99 |
| Unknown or not answered | 1 | 2 | |||||
| Comprehensive care plan | 53 | 88 | 77–95 | 27 | 82 | 65–93 | 0.53 |
| Unknown or not answered | 1 | 2 | |||||
| Pain consultation | 57 | 95 | 86–99 | 61 | 94 | 80–99 | >0.99 |
| Unknown or not answered | 1 | 2 | |||||
| Psychosocial support | 54 | 90 | 79–96 | 25 | 76 | 58–89 | 0.08 |
| Unknown or not answered | 1 | 2 | |||||
| Symptom management | 57 | 95 | 86–99 | 33 | 100 | 89–100 | 0.55 |
| Unknown or not answered | 1 | 2 | |||||
Abbreviations: CI, confidence interval; DNR, Do-not-resuscitate; NCI, National Cancer Institute; Q1–Q3, interquartile range
Total number of respondents
Comparisons were made between NCI and non-NCI cancer centers using the Fisher’s exact test for categorical variables, and the Mann-Whitney test for continuous variables. Confidence intervals were computed using the exact binominal test. Missing values were not included in the analyses
Unless stated otherwise
More than one option may apply
Based on the question “Does your palliative care program require physicians to be certified by the American Board of Hospice and Palliative Medicine or American Board of Medical Specialties?”
Based on the question “Does your palliative care program require nurses to be certified by the National Board for Certification of Hospice and Palliative Nurses?”
While most palliative care teams had physicians (80%, 95% confidence interval (CI) 71–88%), mid-level providers (71%, 95% CI 62–80%), social workers (55%, 95% CI 45–65 %) and nurses (47%, 95% CI 37–58%), other healthcare professions were present in fewer than half of the cancer centers surveyed. Only one-third of palliative care program leaders identified their professional background as palliative care (Table 3). Board certification was not a requirement for physicians or nurses in a majority of programs (Table 3).
Table 4 provides further information about the structures and processes for the four main branches of palliative care services, including inpatient consultation teams, outpatient clinics, PCUs and institution-operated hospices. Inpatient consultation teams were not only the most common service, but also served a larger proportion of patients than PCUs and outpatient clinics. Importantly, the median duration from referral to death was 7 days (N=49, interquartile range 4–16 days) for inpatient consultation teams, 7 days (N=8, interquartile range 5–10 days) for palliative care units, and 90 days (N=11, interquartile range 30–120 days) for outpatient clinics. Notably, a large minority of programs with an outpatient clinic reported that they see patients in oncology clinics.
Table 4.
Structure and Processes of Palliative Care Clinical Services, Education and Research in Cancer Centers According to Palliative Care Program Leaders
| NCI Cancer Centers (N=61)a |
Non-NCI Cancer Centers (N=35)a |
P- valueb |
|||||
|---|---|---|---|---|---|---|---|
| N | % | 95% CI (%)c | N | % | 95% CI (%)c |
||
| Consultation Service (N=83)d | 54 | 89 | 78–95 | 29 | 83 | 66–93 | 0.54 |
| Availability | |||||||
| 24 hours/7 days per week | 23 | 45 | 31–60 | 11 | 38 | 21–58 | |
| 24 hours/weekdays only | 4 | 8 | 2–19 | 3 | 10 | 2–27 | 0.68 |
| Business hours/weekdays only | 23 | 45 | 31–60 | 13 | 45 | 26–64 | |
| Other | 1 | 2 | 0–10 | 2 | 7 | 1–23 | |
| Unknown or not answered | 3 | 0 | |||||
| Number of referrals/month, median (Q1–Q3) |
47.5 | (30–75) | 30 | (19–50) | 0.03 | ||
| Unknown or not answered | 2 | 0 | |||||
| Number of days from referral to death, median (Q1–Q3) |
6 | (4–16.25) | 7 | (4–10) | 0.76 | ||
| Unknown or not answered | 26 | 8 | |||||
| Palliative Care Units/Beds (N=27)d | 16 | 26 | 16–39 | 11 | 31 | 17–49 | 0.64 |
| Physical unit present | 9 | 69 | 39–91 | 4 | 40 | 12–74 | |
| Unknown or not answered | 3 | 1 | |||||
| Duration ≥3 years | 11 | 92 | 62–100 | 7 | 70 | 35–93 | - |
| Unknown or not answered | 4 | 1 | |||||
| Number of beds, median (Q1–Q3) | 10.5 | (4–12) | 4 | (4–6) | - | ||
| Unknown or not answered | 4 | 6 | |||||
| Number of discharges/month, median (Q1–Q3) |
45 | (30–50) | 15 | (11.5–26.5) | - | ||
| Unknown or not answered | 7 | 3 | |||||
| Median days from admission to death, median (Q1–Q3) | 6 | (3–21) | 7 | (6.3–7) | |||
| Unknown or not answered | 13 | 6 | |||||
| Mortality rate, median (Q1–Q3) | 40 | (28–65) | 43 | (25–70) | |||
| Unknown or not answered | 5 | 2 | |||||
| Outpatient Clinic (N=50)d | 40 | 66 | 52–77 | 10 | 29 | 15–46 | 0.001 |
| Dedicated palliative care outpatient clinic |
33 | 54 | 41–67 | 7 | 20 | 8–37 | 0.001 |
| Unknown or not answered | 0 | 0 | |||||
| Patients seen in oncology clinics | 14 | 23 | 13–35 | 4 | 11 | 3–27 | 0.19 |
| Unknown or not answered | 0 | 0 | |||||
| Number of clinic days/week, median (Q1–Q3) |
2 | (1–4.5) | 1 | (.5–3.5) | 0.46 | ||
| Unknown or not answered | 2 | 1 | |||||
| Number of referrals/month, median (Q1–Q3) |
14 | (6–22.5) | 7.5 | (2–18) | 0.08 | ||
| Unknown or not answered | 4 | 0 | |||||
| Number of days from referral to death, median (Q1–Q3) |
90 | (84–120) | 41 | (28–54) | - | ||
| Unknown or not answered | 31 | 8 | |||||
| Hospice (N=43)d | 19 | 31 | 20–44 | 24 | 69 | 51–83 | 0.001 |
| Daily census, median (interquartile range) |
20 | (7–50) | 85 | (19.5–268) | 0.03 | ||
| Unknown or not answered | 5 | 4 | |||||
| Palliative Care Education | |||||||
| Palliative care fellowship program | 23 | 38 | 26–51 | 6 | 17 | 7–34 | 0.04 |
| Unknown or not answered | 0 | 0 | |||||
| Fellows ≥5 in the program | 4 | 18 | 5–40 | 1 | 17 | 0–64 | >0.99 |
| Unknown or not answered | 1 | 0 | |||||
| Training for mid-level providers | 23 | 43 | 30–58 | 11 | 42 | 23–63 | >0.99 |
| Unknown or not answered | 8 | 9 | |||||
| Mandatory rotation for medical oncology |
14 | 27 | 16–42 | 4 | 22 | 6–48 | 0.76 |
| Unknown or not answered | 10 | 17 | |||||
| Mandatory rotation for radiation oncology |
1 | 2 | 0–10 | 0 | 0 | - | >0.99 |
| Unknown or not answered | 10 | 19 | |||||
| Mandatory rotation for pediatric oncology |
3 | 6 | 1–17 | 0 | 0 | - | 0.57 |
| Unknown or not answered | 12 | 19 | |||||
| Mandatory rotation for medical students |
6 | 12 | 4–23 | 2 | 13 | 2–38 | >0.99 |
| Unknown or not answered | 9 | 19 | |||||
| Palliative Care Research | |||||||
| Research programs | 28 | 46 | 33–59 | 6 | 17 | 7–34 | 0.007 |
| Unknown or not answered | 0 | 0 | |||||
| Receives research funding | 19 | 70 | 50–86 | 4 | 80 | 28–99 | >0.99 |
| Unknown or not answered | 1 | 1 | |||||
| Peer reviewed grants | 13 | 68 | 43–87 | 3 | 75 | 19–99 | >0.99 |
| Unknown or not answered | 0 | 0 | |||||
| Private foundations/philanthropy |
12 | 63 | 38–84 | 3 | 75 | 19–99 | >0.99 |
| Unknown or not answered | 0 | 0 | |||||
| Funding source private industry |
9 | 47 | 24–71 | 2 | 50 | 7–93 | >0.99 |
| Unknown or not answered | 0 | 0 | |||||
| Funding source institutional sources |
8 | 42 | 20–67 | 3 | 75 | 19–99 | 0.32 |
| Unknown or not answered | 0 | 0 | |||||
Abbreviations: CI, confidence interval; NCI, National Cancer Institute; Q1–Q3, interquartile range
Total number of respondents
Comparisons were made between NCI and non-NCI cancer centers using the Fisher’s exact test for categorical variables, and the Mann-Whitney test for continuous variables. Confidence intervals were computed using the exact binominal test. Missing values were not included in the analyses.
Unless stated otherwise
The inpatient consultation teams, outpatient clinics and PCUs were generally larger and served more patients at NCI cancer centers than at non-NCI cancer centers (Table 4). In contrast, NCI cancer centers were less likely to report an institution-operated hospice than non-NCI cancer centers, and had a smaller median daily hospice census.
Palliative Care Education
NCI cancer centers were more likely than non-NCI cancer centers to offer a palliative care fellowship program (Table 4). The fellowship programs were generally small, with few having five or more clinical fellows, and even fewer with research fellowships. Almost half of the responding programs provided training for mid-level providers. In NCI cancer centers, palliative care was a mandatory rotation for oncology fellows in a minority of programs (Table 4).
Palliative Care Research
Table 4 provides information regarding the availability of palliative care research programs and funding sources. Less than half of the respondents had research programs in place, even for NCI cancer centers.
DISCUSSION
Our survey provides up-to-date information on the availability and degree of integration of palliative care services in US cancer centers. Despite significant growth in the number of palliative care programs over the past decade,16–19 there remains much heterogeneity in the infrastructure and delivery of care in US cancer centers. Fewer than half of the palliative care programs were equipped with an outpatient clinic, PCU or hospice, and even fewer had fellowship and research programs in place. NCI cancer centers were more likely to offer palliative care services, particularly inpatient consultation teams and outpatient clinics, than non-NCI cancer centers. Cancer patients were referred to palliative care late in the disease trajectory. Further efforts to consolidate existing infrastructure and to integrate palliative care in cancer centers are warranted.
Availability of Palliative Care
While a great majority of cancer centers reported the presence of a palliative care program, many of these programs were limited to providing inpatient consultation services, and only few centers had a PCU. While palliative care for many inpatients can be managed effectively through the consultation service, those with severe distress requiring intensive palliative care are best managed in a PCU under the care of an interprofessional team.20–22
Fewer than half of the cancer centers offered palliative care outpatient services, although NCI cancer centers reported having more clinics in place. Given that oncology care is provided predominantly on an outpatient basis, the relative lack of palliative care outpatient clinics is an important finding. Palliative care clinics have the potential not only to significantly increase the number of referrals, but also to promote early access to integrated care. A novel outpatient model of integration involves palliative care personnel seeing patients at oncology clinics, which can potentially increase referral and enhance coordination and communication between oncology and palliative care teams.23 Thirty percent of centers reported that they have combined oncology-palliative care clinics. The exact nature and outcomes of these clinics need to be further delineated.
Integration of Palliative Care
Almost all cancer center executives, who play a critical role in defining the future of cancer care, agreed that a stronger integration between palliative and oncology care is necessary. Early incorporation of principles of palliative medicine in cancer care has been shown to be associated with improved symptom control, quality of life, and transition to hospice care.24–26 Conversely, delayed referral significantly limits the effectiveness of palliation.27–29 Our survey revealed that palliative care patients were referred too late in the disease trajectory, a marker of limited access and integration.
How can we facilitate this important process of integration? First, healthcare professionals, patients and their families need to be educated on the benefits of palliative care and the concept of simultaneous care.30 This can be accomplished through longitudinal discussions, mass media and integration of relevant materials into heath professionals’ educational curricula, scientific meeting programs and certification/recertification requirements.6 Second, increased availability of palliative care outpatient clinics can facilitate early referral. Third, oncologists should be encouraged to make early palliative care referrals and to participate regularly in family conferences and palliative care educational rounds, whereas palliative care specialists should start attending interdisciplinary cancer treatment rounds. Fourth, enhanced training of oncologists in core competencies related to palliative care can increase the overall quality of care and prompt more timely referrals to palliative care.6 Fifth, NCI should dedicate more resources toward research on integration models, with particular attention paid to the documentation of clinically important outcomes.31 The Institute of Medicine also recommended that “NCI should add the requirement of research in palliative care and symptom control for recognition as a Comprehensive Cancer Center.” 4 Finally, as highlighted in the executive survey, financial constraints remain the major obstacle to effective delivery of palliative care. It is prudent to advocate for increased resources and health policy changes through political engagement at the state and national levels.
Palliative Care Research and Education
The future of palliative care depends on research and education. Our study revealed the troublesome finding that few cancer centers have research programs available, and less than half offer palliative care fellowship programs and mandatory palliative care rotations for medical oncology fellows. Given the self-perceived lack of palliative care training among oncologists,32, 33 standardization and consolidation of palliative care in oncology fellowships is essential. To meet the anticipated growth in palliative care, the infrastructures for both research and education need to be developed further.
Limitations
This study has several limitations. First, we sampled only a small number of cancer centers, with some missing values. Second, responses from our survey could be biased, as they were based on recalled information and approximated data. Third, we surveyed only cancer centers approved by the CoC, and did not include any non-accredited hospitals. This may result in an overestimation of palliative care services in non-NCI cancer centers.12 Fourth, there remains no gold standard for what constitutes a palliative care program, which could have affected how our respondents interpreted questions in the surveys. An operational definition of palliative care related to program infrastructure and/or staff qualifications would be helpful. Finally, although we addressed the surveys to the cancer center executives and palliative care program leaders, their delegates might have filled out the surveys instead. Nevertheless, in delegating this task, we believe that the executives/program leaders identified the most appropriate representatives for completing the surveys.
Conclusions
While most cancer centers now have a palliative care program, there remain significant gaps and delays in the delivery of care. To fulfill ASCO’s vision of full integration of palliative care as a routine part of comprehensive cancer care by 2020,6 we urgently need to consolidate infrastructure such as outpatient clinics and PCUs, increase training of palliative care professionals and oncologists, conduct research on novel integration models and quality-improvement measures, educate patients and their families, and advocate for public health policy changes. Oncologists, palliative care specialists, executives and political leaders need to work closely together to ensure access to high-quality palliative care for all cancer patients in the US.
Acknowledgment
Author contributions: Dr. Hui had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Study concept and design: Elsayem, Hui, Bruera, De La Cruz, Berger, Zhukovsky, Fadul, Palmer
Acquisition of data: Hui, De La Cruz, Evans, Elsayem, Berger, Zhukovsky, Fadul Analysis and interpretation of data: Hui, Palla, Bruera
Drafting of the manuscript: Hui, Bruera
Critical revision of the manuscript for important intellectual content: Hui, Bruera, Elsayem, Zhukovsky, Palla, Palmer, De La Cruz, Berger, Evans,, Fadul
Statistical analysis: Hui, Palla, Palmer
Obtained funding: Bruera
Administrative, technical, or material support: Hui, Elsayem, De La Cruz, Berger, Zhukovsky, Evans, Fadul, Palla, Palmer, Bruera
Study supervision: Bruera
Funding/Support: Supported in part by National Institutes of Health grants RO1NR010162-01A1, RO1CA122292-01, and RO1CA124481-01 (EB); National Cancer Institute grant NCI #CA16672 (PROSPR Shared Resources); the Clinician Investigator Program, Royal College of Physicians and Surgeons of Canada (DH)
Role of Sponsor: The funding organizations had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; and preparation, review, or approval of the manuscript.
Footnotes
Financial Disclosures: The authors reported no financial disclosures.
Additional Contributions: We would like to thank the Patient-reported Outcomes, Survey and Population Research core facility (NCI CA16672) at M.D. Anderson Cancer Center for assistance with conduction of this survey. We would like to thank Ms. Kathryn Hale, MS, MLIS (Department of Scientific Publications, M.D. Anderson Cancer Center) for review of manuscript. We are also grateful to all respondents for completing the surveys.
REFERENCES
- 1.Ingham J. The epidemiology of cancer at the end of life. In: Berger A, Portenoy RK, Weissman DE, editors. Principles and Practice of Supportive Oncology. Philadelphia, PA: Lippincott-Raven; 1998. pp. 749–765. [Google Scholar]
- 2.Cancer care during the last phase of life. J Clin Oncol. 1998;16(5):1986–1996. doi: 10.1200/JCO.1998.16.5.1986. [DOI] [PubMed] [Google Scholar]
- 3.Levy MH, Back A, Benedetti C, et al. NCCN clinical practice guidelines in oncology. palliative care. 2008. Available at: http://www.nccn.org/professionals/physician_gls/f_guidelines.asp. [DOI] [PubMed] [Google Scholar]
- 4.IOM National Cancer Policy Board. Improving Palliative Care for Cancer. 1st ed. Washington, DC: Institute of Medicine; 2001. [Google Scholar]
- 5.National Cancer Control Programmes: Policies and Managerial Guidelines. 2nd ed. Geneva: World Health Organization; 2002. Pain relief and palliative care; pp. 83–91. [Google Scholar]
- 6.Ferris FD, Bruera E, Cherny N, et al. Palliative cancer care a decade later: Accomplishments, the need, next steps -- from the American Society of Clinical Oncology. J Clin Oncol. 2009;27(18):3052–3058. doi: 10.1200/JCO.2008.20.1558. [DOI] [PubMed] [Google Scholar]
- 7.Lagman R, Walsh D. Integration of palliative medicine into comprehensive cancer care. Semin Oncol. 2005;32(2):134–138. doi: 10.1053/j.seminoncol.2004.11.015. [DOI] [PubMed] [Google Scholar]
- 8.Byock I. Completing the continuum of cancer care: Integrating life-prolongation and palliation. CA Cancer J Clin. 2000;50(2):123–132. doi: 10.3322/canjclin.50.2.123. [DOI] [PubMed] [Google Scholar]
- 9.Ferrell B, Paice J, Koczywas M. New standards and implications for improving the quality of supportive oncology practice. J Clin Oncol. 2008;26(23):3824–3831. doi: 10.1200/JCO.2007.15.7552. [DOI] [PubMed] [Google Scholar]
- 10.A National Framework and Preferred Practices for Palliative and Hospice Care Quality. Washington, USA: National Quality Forum; 2006. [Google Scholar]
- 11.Donabedian A. Evaluating the quality of medical care. Milbank Mem Fund Q. 1966;44(3) Suppl:166–206. [PubMed] [Google Scholar]
- 12.Bilimoria KY, Bentrem DJ, Stewart AK, Winchester DP, Ko CY. Comparison of commission on cancer-approved and -nonapproved hospitals in the united states: Implications for studies that use the national cancer data base. J Clin Oncol. 2009;27(25):4177–4181. doi: 10.1200/JCO.2008.21.7018. [DOI] [PubMed] [Google Scholar]
- 13.Bilimoria KY, Stewart AK, Winchester DP, Ko CY. The national cancer data base: A powerful initiative to improve cancer care in the united states. Ann Surg Oncol. 2008;15(3):683–690. doi: 10.1245/s10434-007-9747-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Coluzzi PH, Grant M, Doroshow JH, Rhiner M, Ferrell B, Rivera L. Survey of the provision of supportive care services at national cancer institute-designated cancer centers. J Clin Oncol. 1995;13(3):756–764. doi: 10.1200/JCO.1995.13.3.756. [DOI] [PubMed] [Google Scholar]
- 15.Lenexa KS. Standard definitions: Final dispositions of case codes and outcome rates for surveys. 6th ed. [Accessed February 1, 2010]. Available at: http://www.aapor.org/Standard_Definitions/1481.htm. [Google Scholar]
- 16.Billings JA, Pantilat S. Survey of palliative care programs in united states teaching hospitals. J Palliat Med. 2001;4(3):309–314. doi: 10.1089/109662101753123913. [DOI] [PubMed] [Google Scholar]
- 17.Pan CX, Morrison RS, Meier DE, et al. How prevalent are hospital-based palliative care programs? status report and future directions. J Palliat Med. 2001;4(3):315–324. doi: 10.1089/109662101753123922. [DOI] [PubMed] [Google Scholar]
- 18.Goldsmith B, Dietrich J, Du Q, Morrison RS. Variability in access to hospital palliative care in the United States. J Palliat Med. 2008;11(8):1094–1102. doi: 10.1089/jpm.2008.0053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Morrison RS, Maroney-Galin C, Kralovec PD, Meier DE. The growth of palliative care programs in united states hospitals. J Palliat Med. 2005;8(6):1127–1134. doi: 10.1089/jpm.2005.8.1127. [DOI] [PubMed] [Google Scholar]
- 20.Elsayem A, Swint K, Fisch MJ, et al. Palliative care inpatient service in a comprehensive cancer center: Clinical and financial outcomes. J Clin Oncol. 2004;22(10):2008–2014. doi: 10.1200/JCO.2004.11.003. [DOI] [PubMed] [Google Scholar]
- 21.Baker JN, Hinds PS, Spunt SL, et al. Integration of palliative care practices into the ongoing care of children with cancer: Individualized care planning and coordination. Pediatr Clin North Am. 2008;55(1):223–250. doi: 10.1016/j.pcl.2007.10.011. xii. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hui D, Elsayem A, Palla S, et al. Discharge outcomes and survival of patients with advanced cancer admitted to an acute palliative care unit at a comprehensive cancer center. J Palliat Med. 2010;13(1):49–57. doi: 10.1089/jpm.2009.0166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Temel JS, Jackson VA, Billings JA, et al. Phase II study: Integrated palliative care in newly diagnosed advanced non-small-cell lung cancer patients. J Clin Oncol. 2007;25(17):2377–2382. doi: 10.1200/JCO.2006.09.2627. [DOI] [PubMed] [Google Scholar]
- 24.Meyers FJ, Linder J, Beckett L, Christensen S, Blais J, Gandara DR. Simultaneous care: A model approach to the perceived conflict between investigational therapy and palliative care. J Pain Symptom Manage. 2004;28(6):548–556. doi: 10.1016/j.jpainsymman.2004.03.002. [DOI] [PubMed] [Google Scholar]
- 25.Wright AA, Zhang B, Ray A, et al. Associations between end-of-life discussions, patient mental health, medical care near death, and caregiver bereavement adjustment. JAMA. 2008;300(14):1665–1673. doi: 10.1001/jama.300.14.1665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Higginson IJ, Finlay IG, Goodwin DM, et al. Is there evidence that palliative care teams alter end-of-life experiences of patients and their caregivers? J Pain Symptom Manage. 2003;25(2):150–168. doi: 10.1016/s0885-3924(02)00599-7. [DOI] [PubMed] [Google Scholar]
- 27.Osta BE, Palmer JL, Paraskevopoulos T, et al. Interval between first palliative care consult and death in patients diagnosed with advanced cancer at a comprehensive cancer center. J Palliat Med. 2008;11(1):51–57. doi: 10.1089/jpm.2007.0103. [DOI] [PubMed] [Google Scholar]
- 28.Cheng WW, Willey J, Palmer JL, Zhang T, Bruera E. Interval between palliative care referral and death among patients treated at a comprehensive cancer center. J Palliat Med. 2005;8(5):1025–1032. doi: 10.1089/jpm.2005.8.1025. [DOI] [PubMed] [Google Scholar]
- 29.Morita T, Akechi T, Ikenaga M, et al. Late referrals to specialized palliative care service in japan. J Clin Oncol. 2005;23(12):2637–2644. doi: 10.1200/JCO.2005.12.107. [DOI] [PubMed] [Google Scholar]
- 30.Meyers FJ, Linder J. Simultaneous care: Disease treatment and palliative care throughout illness. J Clin Oncol. 2003;21(7):1412–1415. doi: 10.1200/JCO.2003.01.104. [DOI] [PubMed] [Google Scholar]
- 31.Earle CC, Landrum MB, Souza JM, Neville BA, Weeks JC, Ayanian JZ. Aggressiveness of cancer care near the end of life: Is it a quality-of-care issue? J Clin Oncol. 2008;26(23):3860–3866. doi: 10.1200/JCO.2007.15.8253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Cherny NI, Catane R European Society of Medical Oncology Taskforce on Palliative and Supportive Care. Attitudes of medical oncologists toward palliative care for patients with advanced and incurable cancer: Report on a survery by the european society of medical oncology taskforce on palliative and supportive care. Cancer. 2003;98(11):2502–2510. doi: 10.1002/cncr.11815. [DOI] [PubMed] [Google Scholar]
- 33.Johnson CE, Girgis A, Paul CL, Currow DC. Cancer specialists' palliative care referral practices and perceptions: Results of a national survey. Palliat Med. 2008;22(1):51–57. doi: 10.1177/0269216307085181. [DOI] [PubMed] [Google Scholar]


