Abstract
Accumulating evidence suggests that increased visit-to-visit variability (VVV) of blood pressure is associated with stroke. No study has examined the association between VVV of blood pressure and stroke in postmenopausal women, and scarce data exists as to whether this relation is independent of the temporal trend of blood pressure. We examined the association of VVV of blood pressure with stroke in 58,228 postmenopausal women enrolled in the Women's Health Initiative. Duplicate blood pressure readings, which were averaged, were taken at baseline and at each annual visit. VVV was defined as the standard deviation about the participant's mean systolic blood pressure (SBP) across visits (SD), and about the participant's regression line with SBP regressed across visits (SDreg). Over a median follow-up of 5.4 years, 997 strokes occurred. In an adjusted model including mean SBP over time, the hazard ratios (95% CI) of stroke for higher quartiles of SD of SBP compared to the lowest quartile (referent) were 1.39 (1.03-1.89) for quartile 2, 1.52 (1.13-2.03) for quartile 3, and 1.72 (1.28-2.32) for quartile 4 (P trend<0.001). The relation was similar for SDreg of SBP quartiles in a model that additionally adjusted for the temporal trend in SBP (P trend<0.001). The associations did not differ by stroke type (ischemic vs. hemorrhagic). There was a significant interaction between mean SBP and SDreg on stroke with the strongest association seen below 120 mmHg. In postmenopausal women, greater VVV of SBP was associated with increased risk of stroke, particularly in the lowest range of mean SBP.
Keywords: hypertension, blood pressure, stroke, postmenopause, women
Introduction
In the United States, stroke is the fourth leading cause of death1 and the leading cause of disability.2 Women have lower age-adjusted stroke incidence than men.2 However, because of the longer life expectancy in women, the lifetime risk of stroke is greater in women compared with men. Women also account for a large proportion of stroke deaths and disability after stroke.2 A better understanding of the determinants of stroke in women has substantial implications in both the clinical and public health context.
Elevated blood pressure is a risk factor for stroke.3 The prognostic value of blood pressure is based on the traditional method of obtaining auscultatory measurements in a clinic setting, typically averaged over several visits.4 It is generally believed that readings obtained in this manner are limited by variability observed from one visit to the next.5 However, there is accumulating evidence that increased visit-to-visit variability (VVV) of blood pressure is associated with a higher risk of stroke,6 coronary heart disease (CHD),7 and all-cause mortality,8, 9 associations that are independent of average blood pressure over time and other possible explanatory factors.
Studies reporting on VVV of blood pressure and prognosis have been relatively small8, 9 and included select patients who were already at high cardiovascular disease (CVD) risk.6 Only one published study has specifically reported on stroke as an outcome.6 This latter study included patients with prior transient ischemic attack, stroke, or multiple CVD risk factors.6 Further, although individuals who have an increasing blood pressure over time may have a higher risk of stroke, scarce data exist as to whether the relation of VVV of blood pressure and stroke is independent of blood pressure increases over time.6 Finally, no study has previously examined these relations in postmenopausal women, who are at increased risk for stroke.
We determined whether VVV of blood pressure is associated with stroke, and whether this relation is independent of the mean and temporal change in blood pressure over time, in a large well-characterized cohort of postmenopausal women with a wide range of CVD risk enrolled in the Women's Health Initiative (WHI).
Methods
Sample Population
WHI is a multi-center study of 161,808 postmenopausal women aged 50 to 79 years consisting of overlapping clinical trials (CTs) and an observational study (OS).10 This analysis restricts the population to women enrolled in the CT components (N=68,132), and excludes women who did not have blood pressure assessed at the baseline visit and at least two follow-up visits up to the Year 3 visit, had experienced an incident stroke and/or mortality event prior to their Year 3 visit, or did not have a Year 3 visit or any subsequent follow-up, leaving a final sample size of 58,228. The online Data Supplement (please see http://hyper.ahajournals.org) provides further details on the design of WHI and how the sample for the current analyses was selected. The protocol was approved by institutional review boards of the participating institutions; all trial participants provided written informed consent.
Blood pressure and Heart Rate Measurement
Blood pressure and heart rate were measured at baseline and each annual study visit by certified staff with the use of standardized procedures and instruments. Appropriate cuff bladder size was determined at each visit based on arm circumference. Blood pressure was measured in the right arm with a mercury sphygmomanometer after the participant was seated and had rested for 5 minutes; 2 measures, taken 30 seconds apart, were recorded. The blood pressure at each visit was defined as the average of the 2 readings. Heart rate was measured manually once at each visit.
Outcome Ascertainment
Detailed definitions and methods for ascertaining and classifying outcomes have been published.11 Briefly, fatal and non-fatal strokes were verified by review of medical records by centrally trained physician adjudicators at each center. Stroke cases were centrally adjudicated at the WHI Clinical Coordinating Center. Stroke was defined as the rapid onset of a neurologic deficit lasting more than 24 hours, unless death supervened or a lesion compatible with acute stroke was evident on computed tomography or magnetic resonance imaging scan. For this analysis, the primary outcome was defined as the occurrence of a fatal or non-fatal ischemic or hemorrhagic stroke. Ischemic stroke was defined as the occlusion of cerebral or pericerebral arteries with infarction not resulting from a procedure (cerebral thrombosis, cerebral embolism, lacunar infarction). Hemorrhagic stroke was defined as subarachnoid hemorrhage, intracerebral hemorrhage, or other/unspecified intra-cranial hemorrhage not resulting from a procedure (nontraumatic epidural hemorrhage or subdural hemorrhage).
Statistical Analyses
VVV of blood pressure, the primary exposure, was defined as the standard deviation (SD) about the participant's mean systolic blood pressure (SBP) across visits.6, 8, 9 VVV of blood pressure was also defined as the standard deviation about the participant's regression line (SDreg) with SBP regressed across visits. The estimation of SD assumes that a participant's blood pressure is constant over follow-up, and the estimation of SDreg assumes a linear temporal trend. The online Data Supplement provides further details on the definitions of SD and SDreg. Other measures of VVV, such as coefficient of variation and variation independent of the mean,6, 8, 9 were not pursued because these measures were highly correlated with SD (r=0.97 for the correlation between SD and coefficient of variation, and r=0.90 for the correlation between SD and variation independent of the mean), and therefore, likely represent the same underlying domain of blood pressure variability.
Baseline characteristics of participants were examined by SD of SBP quartiles. Tests for linear trend across quartiles were adjusted for age, race/ethnicity, and randomization assignment in the hormone therapy trial. Primary analyses used time-to-event methods based on the Cox regression model with time defined as the number of days from the third annual visit to the first postrandomization diagnosis of stroke. Stroke events were included through the protocol-specified termination date of March 31, 2005. The online Data Supplement provides details on how covariates were ascertained and defined. An initial model (Model 1) provided hazard ratios for stroke associated with SD of SBP quartiles, with the lowest quartile serving as the referent, adjusting for age, race/ethnicity and allowing the hazard function to vary by 5-year age groups. Model 2 included covariates in Model 1 plus the baseline status of diabetes, high cholesterol, smoking status, education level, prior hormone therapy use, physical activity level, body mass index, history of CHD, history of atrial fibrillation, left ventricular hypertrophy on 12-lead electrocardiogram, and additional stratification on history of stroke and hormone therapy trial assignment; mean SBP across visits (time-dependent variable); mean heart rate across visits (time-dependent variable), and antihypertensive medication use across visits (time-dependent variable). Antihypertensive medication use across visits was defined as never used (no antihypertensive medication use at baseline and all available follow-up visits, used at all visits (on antihypertensive medications at baseline and all available follow-up visits), newly started during follow-up (on no antihypertensive medications at baseline, and on antihypertensive medications at one of the follow-up exams), and other (not in one of the above categories). To account for systematic changes in blood pressure, the final model (Model 3) used SDreg of SBP as the exposure variable, and included the covariates in Model 2 plus a participant's linear change in SBP. All time-dependent variables including SD and SDreg were based on measures through Year 3, and later updated at each subsequent visit while a participant remained at risk. Models 1 to 3 were also fit with the corresponding exposure variable, SD or SDreg, modeled as a continuous variable.
Subgroup analyses tested interactions between SDreg of SBP and several baseline characteristics within the final Cox regression model. An additional analysis was performed in which mean diastolic blood pressure (DBP) across visits was added to Model 3. The relations across quartiles of SDreg of SBP remained unchanged. Similar findings were observed when SD of DBP was added to the multivariable model. Lastly, results did not change when mean pulse pressure across visits was added to Model 3 instead of mean DBP across visits. We do not report further on these analyses, as the results do not alter the primary findings of the study.
All statistical tests were two sided and P values <0.05 were considered to be statistically significant. Analyses were performed by SAS statistical software version 9.2 (SAS Inc, Cary, NC) and figures were constructed with R version 2.11.12
Results
Characteristics and Correlates of VVV of SBP
The means (SD) of the SD of SBP and of SBP across visits were 10.9 (4.5) mm Hg and 125.8 (12.9) mm Hg respectively. Higher quartiles of SD of SBP were associated with older age; higher body mass index; higher mean SBP, DBP and pulse pressure; a small decrease in mean heart rate; randomization to the hormone therapy component; Black/African American race; not having successfully obtained a college degree or higher; antihypertensive medication use across visits; history of hypertension; statin, aspirin and anticoagulation use; history of diabetes and high cholesterol; smoking status; the presence of left ventricular hypertrophy; history of CHD; history of stroke; history of atrial fibrillation; and lower physical activity (Table S1 in the online Data Supplement).
Relation Between VVV of SBP and Stroke
The mean (SD) number of visits that were used to estimate SD of SBP was 7.9 (1.8). Over a median (IQR) follow-up of 5.4 (1.7) years, a total (annualized rate) of 997 (0.32%) strokes occurred during 315,789 person years of observation. Of the primary stroke events, 81.3% were ischemic and 18.7% were hemorrhagic. In an age-stratified model adjusted for age and race/ethnicity (Model 1, top panel, Table 1), higher quartiles of the SD of SBP were significantly associated with an increasing risk of stroke. After further adjustment for CVD risk factors, prevalent CVD, mean SBP, mean heart rate, and antihypertensive medication use (Model 2, top panel, Table 1), the relation between SD of SBP and stroke was attenuated, but the trend across quartiles remained significant. In a fully adjusted model that also accounted for linear change of SBP (Model 3, top panel, Table 1), increasing quartiles of SDreg of SBP were significantly related to higher stroke risks. In this latter model, a steeper slope of SBP across visits was also associated with a higher risk of stroke (P <0.05). A similar pattern of results was observed when SD (Models 1 and 2) or SDreg (Model 3) of SBP was expressed as a continuous variable (bottom panel, Table 1). The hazard ratios (95% CI) for each 5 mmHg increase in SD of SBP did not differ by stroke type in Model 2: 1.15 (95% CI 1.07 - 1.25) for ischemic stroke and 1.18 (95% CI 1.00 - 1.40) for hemorrhagic stroke (heterogeneity P = 0.78). The hazard ratios (95% CI) for each 5 mmHg increase in SDreg of SBP also did not differ by stroke type in Model 3: 1.12 (95% CI 1.04 - 1.21) for ischemic stroke and 1.14 (95% CI 0.97 - 1.34) for hemorrhagic stroke (heterogeneity P = 0.86).
Table 1. Hazard Ratios for Stroke by Quartiles of Visit-to-Visit Variability* of Systolic Blood Pressure (top panel) and Per Each 5 mm Hg Increase in Visit-to-Visit Variability* of Systolic Blood Pressure (bottom panel).
| Visit-to-Visit Variability of Systolic Blood Pressure Modeled as Quartiles | |||||
|---|---|---|---|---|---|
|
| |||||
| Characteristics | Q1 | Q2 | Q3 | Q4 | P trend |
| SD of Systolic Blood Pressure | <6 mm Hg | 6-8.9 mm Hg | 9-12.9 mm Hg | ≥13 mm Hg | - |
| Cases of stroke | 150 | 212 | 260 | 375 | - |
| Annualized % | 0.20% | 0.26% | 0.32% | 0.49% | - |
| Model | Hazard Ratio (95% CI) | ||||
| Model 1† | 1.00 (ref) | 1.50 (1.11 - 2.03) | 1.95 (1.46 - 2.60) | 2.91 (2.19 - 3.86) | <0.001 |
| Model 2‡ | 1.00 (ref) | 1.39 (1.03 - 1.89) | 1.52 (1.13 - 2.03) | 1.72 (1.28 - 2.32) | <0.001 |
| Model 3§ | 1.00 (ref) | 1.08 (0.84 - 1.39) | 1.26 (0.99 - 1.59) | 1.46 (1.15 - 1.85) | <0.001 |
|
| |||||
| Visit-to-Visit Variability of Systolic Blood Pressure Modeled as a Continuous Variable (Per Each 5 mm Hg Increase) | |||||
|
| |||||
| Model | Hazard Ratio (95% CI) | P value | |||
|
| |||||
| Model 1† | 1.40 (1.32 - 1.49) | <0.001 | |||
| Model 2‡ | 1.16 (1.08 - 1.24) | <0.001 | |||
| Model 3§ | 1.12 (1.05 - 1.19) | <0.001 | |||
Represents the standard deviation (SD) from the mean in Models 1 and 2, and the standard deviation (SDreg) from the least squares regression line in Model 3.
Model 1 includes adjustment for age at baseline and race/ethnicity and stratified by 5-year age groups.
Model 2 includes adjustment for variables in Model 1 + baseline variables including diabetes, high cholesterol, smoking, education level, prior hormone therapy use, physical activity, body mass index, history of CHD, history of atrial fibrillation, left ventricular hypertrophy on 12-lead ECG, and additional stratification on history of stroke and hormone therapy trial assignment; mean systolic blood pressure (time-dependent variable); mean heart rate (time-dependent variable); and the use of antihypertensive medications (time-dependent variable).
Model 3 includes adjustment for variables in Model 2 and additionally the temporal trend (estimated slope from least squares regression line) of systolic blood pressure (time-dependent).
Subgroup Analyses
As Table S2 shows (see online Data Supplement), there was a significant interaction (interaction P = 0.005) between mean SBP across visits and SDreg of SBP on stroke. The relation between SDreg of SBP and stroke became stronger with decreasing levels of mean SBP below 140 mm Hg, particularly among individuals with mean SBP <120 mm Hg. In participants with mean SBP <120 mm Hg, the prevalence of episodic systolic hypertension (i.e. having at least one visit with SBP >140 mm Hg) by quartiles of SDreg of SBP (<6 mm Hg, 6-8.9 mm Hg, 9-12.9 mm Hg, and ≥13 mm Hg) was 0.1%, 0.7%, 6.2%, and 39.6% respectively. Participants with mean SBP <120 mm Hg and who were in the highest quartile of SDreg of SBP (≥13 mm Hg) had less than a third of their visits with SBP >140 mm Hg.
The hazard ratio for stroke was greater in younger than in older women (Table S2), although the interaction was borderline significant (interaction P = 0.05). There was also a significant interaction of the number of visits used to estimate SDreg of SBP on the relationship between SDreg of SBP and stroke (Table S3 in the online Data Supplement).
Discussion
This study adds important information to the literature on VVV of blood pressure and stroke. Higher annual VVV of SBP was associated with an increased risk of stroke, independent of several possible explanatory factors including age, race/ethnicity, CVD risk factors, prevalent CVD, randomization to hormone therapy, antihypertensive medication use, and mean SBP over time.
Rothwell et al.6 showed that higher VVV of SBP was associated with stroke in four cohorts that included more than 7,000 patients who were already at high risk for stroke including those with previous transient ischemic attack or minor stroke. Higher VVV of SBP was also associated with stroke in treated hypertensive patients who had at least three other CVD risk factors or prevalent CVD enrolled in the Anglo-Scandinavian Cardiac Outcomes Trial Blood Pressure Lowering Arm (ASCOT-BPLA).6 Our study extends these findings by demonstrating that higher levels of annual VVV of SBP are independently associated with an increased risk of stroke in postmenopausal women representing a broad range of CVD risk.
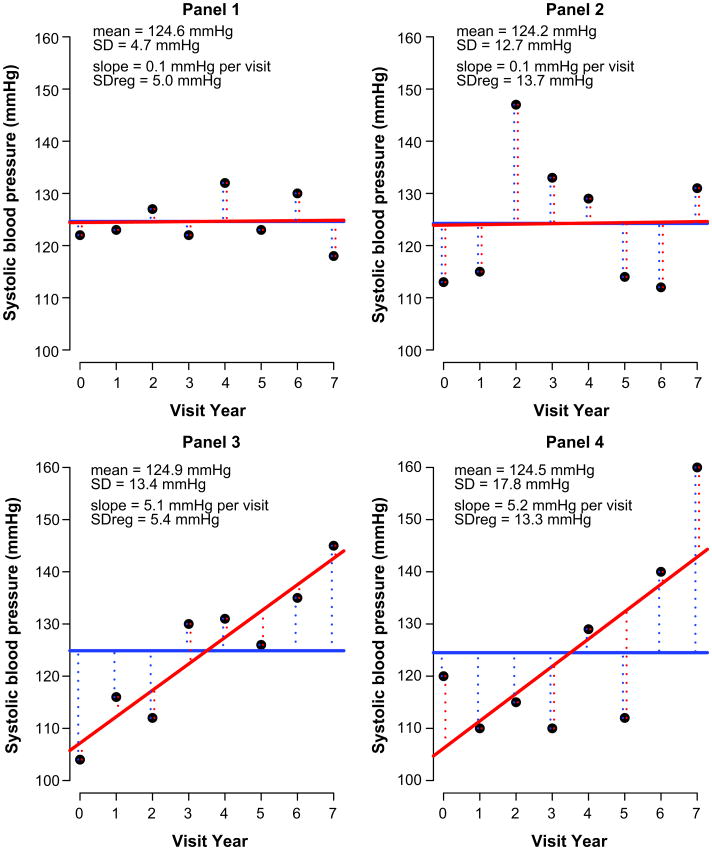
VVV of blood pressure is commonly defined as SD of SBP.6, 8, 9 Since SD of SBP represents the deviation of SBP from the mean, which is assumed to be static over time, then it is generally true that SD of SBP is higher with a greater linear increase in SBP over time compared with SBP that remains constant over time. Therefore, it is possible that the association between VVV of blood pressure and stroke may be explained by increasing blood pressure over time. However, in our study, SDreg of SBP and an increased temporal trend in SBP were independently associated with stroke, indicating that not only is an increase in blood pressure over time associated with stroke, but also VVV of blood pressure contributes to stroke in a manner that is independent of blood pressure trends. Rothwell et al.6 similarly reported that the relation between VVV of SBP and stroke was independent of the temporal trend in SBP. Figure 1 shows VVV and slopes of SBP in four representative individuals in our study who have approximately the same mean SBP. These examples are illustrative of how SD of SBP from the mean is partially determined by the temporal trend of SBP, and that the SDreg of SBP from the regression line represents variability that is independent of the temporal trend of SBP. Although other studies have demonstrated a relation of VVV of blood pressure with total mortality,8, 9 cardiovascular mortality,9 increased white matter hyperintensity volume in the brain,13 and carotid intima-media thickness,14 these studies did not examine whether the relations between VVV of blood pressure and these outcomes were independent of a temporal trend in blood pressure.
Figure 1. Representative Patterns of Visit-to-Visit Blood Pressure Variability.
Plots illustrate systolic blood pressure (SBP) measures over follow-up of four different individuals (Panels 1-4) with approximately the same mean SBP across visits. Standard deviations from the mean and least squares regression line are labeled “SD” and “SDreg”, respectively. Slope of the regression line is labeled “slope.” SBP at each visit is represented by black dots. SD is a measure of the VVV of SBP about the individual's mean (solid blue line), where the mean is assumed to be static. SDreg is a measure of the VVV of SBP about the individual's regression line (solid red line), where the mean (i.e., regression line) is assumed to be a linear function of time. Conceptually, SD is the ‘average’ of the deviations (lengths of dotted blue lines) about the mean (solid blue line), and SDreg is the ‘average’ of the deviations (lengths of dotted red lines) about the regression line (solid red line). The 2 individuals in Panels 3 and 4 (bottom left and right panels) have a larger temporal change in SBP across visits than the 2 individuals in Panels 1 and 2 (upper left and right panels). The individual in Panel 3 has a higher SD from the mean but a similar SDreg from the regression line, compared to the individual in Panel 1. A similar pattern is seen with the 2 individuals in Panels 4 and 2. Further, despite having similar mean SBP across visits, the individuals in Panels 1 and 2, and separately the individuals in Panels 3 and 4, have different SD from the mean and also different SDreg from the regression line.
The relation between VVV of SBP and stroke was stronger in postmenopausal women with SBP in the lowest range (mean <120 mm Hg). SBP was greater than 140 mm Hg in minority of visits in these participants. The VVV of SBP-stroke association was also possibly modified by younger age – the risk of stroke was stronger in the 50-59 year age category. Similar findings were reported in the study by Rothwell et al.6 in which the relation between VVV of SBP and stroke was stronger in participants who had mean SBP less than the median (∼143 mm Hg) and in those in the youngest tertile of age (<56 years). Therefore, VVV of blood pressure may be an important determinant of stroke, particularly in individuals who otherwise would be considered to be low risk based on their SBP and age.
As demonstrated by others,6 the risk for stroke increased with the number of visits used to estimate VVV. The reproducibility of VVV of blood pressure may also increase with more measurements.15, 16 Therefore, for evaluating an individual's risk associated with VVV of blood pressure, clinicians should be wary in using only a few visits to estimate VVV. Future studies are needed to determine the minimum number of visits required to obtain reproducible and valid estimates of VVV. Additionally, the optimal interval between visits (i.e. days, months, years) should also be determined.
The putative factors that explain the link between VVV of SBP and stroke are unclear. Arterial stiffness may play a role.14 Subclinical atherosclerosis, increased wall stress, baroreceptor dysfunction, and endothelial dysfunction are other possible mechanisms.6, 8, 17, 18 However, it is unclear if these factors are causes or consequences of VVV of SBP. Finally, the mechanisms into why lower SBP and younger age modified the relation between VVV of SBP and stroke in postmenopausal women needs to be clarified in future studies.
Finally, our study found that the relationship between VVV of SBP and stroke did not differ by stroke type (i.e. ischemic vs. hemorrhagic). In contrast, Rothwell et al.6 found that VVV of SBP was more predictive of ischemic than hemorrhagic strokes in treated hypertensive participants enrolled in ASCOT-BPLA. The reasons for these divergent results are unclear. The different populations examined as well as the substantially smaller percentage of hemorrhagic vs. ischemic strokes in either sample may be possible explanatory factors.
The sample comprised only women, whose age was restricted to 50 to 79 years. Thus, whether our results can be extended to men, elderly women, or younger premenopausal remains to be determined. Further, our analyses did not consider the various classes of antihypertensive medications that women may have been taking. Certain antihypertensive medication classes may have differential effects on VVV of SBP.19, 20 However, the relation of VVV of SBP with outcomes is also independent of antihypertensive medication class.6, 8 Lastly, it is possible that blood pressure readings were affected by measurement error in our study. However, since the presence of measurement error would have biased our results toward the null, it is likely that the association between VVV of SBP and stroke would be even stronger if measurement error were eliminated.
Major strengths of the study are the very large sample size, well-characterized cohort, and the large number of strokes that were available for analysis. This allowed for the consideration of several possible confounders in the relation between VVV of SBP and stroke, and also the examination of this relation across various subgroups. An additional strength of the study was the careful and standardized assessment of blood pressure and cardiovascular risk factors in WHI, and the central adjudication of all reported stroke events by study neurologists. Further, the participants in WHI represent a broad ethnic, geographic, and socioeconomic sample of women in the United States. Finally, this is one of the few studies to examine whether the relation of VVV of blood pressure and stroke is independent of blood pressure increases over time.
Perspectives
The results from this large study of generally healthy postmenopausal women suggest that higher levels of annual VVV of SBP are independently associated with an increased risk of stroke. The increase in stroke risk is not explained by important factors such as age, race/ethnicity, CVD risk factors, prevalent CVD, use of antihypertensive medications or hormone therapy, mean SBP over time, and the temporal trend of SBP. Notably, the association between VVV of SBP and stroke is stronger among women whose mean SBP is in the lowest range, which suggests a possible role for measures of VVV of blood pressure in refining office-based risk assessment. Future studies should identify the causal pathways that underlie the relation between VVV of SBP and stroke, and investigate the mechanisms as to why the association between VVV and stroke is stronger in postmenopausal women with the lowest SBP.
Supplementary Material
Novelty and Significance.
1. What is new?
This study examines whether annual VVV of blood pressure is associated with stroke in postmenopausal women who have a wide range of CVD risk, and whether this relation is independent of the temporal trend of blood pressure, which is a factor that contributes to VVV of blood pressure.
The large sample size facilitates the examination of this relation across several subgroups.
2. What is Relevant?
The study examines whether VVV of blood pressure is independently associated with stroke, an important hypertension-related outcome.
3. Summary
In postmenopausal women, greater VVV of SBP was independently associated with increased risk of stroke. A stronger association was observed in those with mean SBP in the lowest range.
Acknowledgments
None.
Sources of Funding: The WHI program is funded by the National Heart, Lung, and Blood Institute, National Institutes of Health, U.S. Department of Health and Human Services through contracts N01WH22110, 24152, 32100-2, 32105-6, 32108- 9, 32111-13, 32115, 32118-32119, 32122, 42107-26, 42129-32, and 44221. The online Data Supplement contains additional WHI administrative information.
Footnotes
Anthony Bavry is a consultant for the American College of Cardiology's Cardiosource, and has received research funding from Novartis. There are no other potential conflicts of interest.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Kochanek MA, Xu J, Murphy SL, Minino AM, Kung HC. Deaths: Preliminary data for 2009. Natl Vital Stat Rep. 2011;49:1–51. [PubMed] [Google Scholar]
- 2.Roger VL, Go AS, Lloyd-Jones DM, Adams RJ, Berry JD, Brown TM, Carnethon MR, Dai S, de Simone G, Ford ES, Fox CS, Fullerton HJ, Gillespie C, Greenlund KJ, Hailpern SM, Heit JA, Ho PM, Howard VJ, Kissela BM, Kittner SJ, Lackland DT, Lichtman JH, Lisabeth LD, Makuc DM, Marcus GM, Marelli A, Matchar DB, McDermott MM, Meigs JB, Moy CS, Mozaffarian D, Mussolino ME, Nichol G, Paynter NP, Rosamond WD, Sorlie PD, Stafford RS, Turan TN, Turner MB, Wong ND, Wylie-Rosett J, Roger VL, Turner MB, Wong ND, Wylie-Rosett J. Heart disease and stroke statistics--2011 update: A report from the american heart association. Circulation. 2011;123:e18–e209. doi: 10.1161/CIR.0b013e3182009701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lewington S, Clarke R, Qizilbash N, Peto R, Collins R. Age-specific relevance of usual blood pressure to vascular mortality: A meta-analysis of individual data for one million adults in 61 prospective studies. The Lancet. 2002;360:1903–1913. doi: 10.1016/s0140-6736(02)11911-8. [DOI] [PubMed] [Google Scholar]
- 4.Pickering TG, Hall JE, Appel LJ, Falkner BE, Graves J, Hill MN, Jones DW, Kurtz T, Sheps SG, Roccella EJ. Recommendations for blood pressure measurement in humans and experimental animals: Part 1: Blood pressure measurement in humans: A statement for professionals from the subcommittee of professional and public education of the american heart association council on high blood pressure research. Hypertension. 2005;45:142–161. doi: 10.1161/01.HYP.0000150859.47929.8e. [DOI] [PubMed] [Google Scholar]
- 5.Clarke R, Shipley M, Lewington S, Youngman L, Collins R, Marmot M, Peto R. Underestimation of risk associations due to regression dilution in long-term follow-up of prospective studies. American journal of epidemiology. 1999;150:341–353. doi: 10.1093/oxfordjournals.aje.a010013. [DOI] [PubMed] [Google Scholar]
- 6.Rothwell PM, Howard SC, Dolan E, O'Brien E, Dobson JE, Dahlöf B, Sever PS, Poulter NR. Prognostic significance of visit-to-visit variability, maximum systolic blood pressure, and episodic hypertension. The Lancet. 2010;375:895–905. doi: 10.1016/S0140-6736(10)60308-X. [DOI] [PubMed] [Google Scholar]
- 7.Grove JS, Reed DM, Yano K, Hwang LJ. Variability in systolic blood pressure--a risk factor for coronary heart disease? American journal of epidemiology. 1997;145:771–776. doi: 10.1093/oxfordjournals.aje.a009169. [DOI] [PubMed] [Google Scholar]
- 8.Muntner P, Shimbo D, Tonelli M, Reynolds K, Arnett DK, Oparil S. The relationship between visit-to-visit variability in systolic blood pressure and all-cause mortality in the general population: Findings from nhanes iii, 1988 to 1994. Hypertension. 2011;57:160–166. doi: 10.1161/HYPERTENSIONAHA.110.162255. [DOI] [PubMed] [Google Scholar]
- 9.Hsieh YT, Tu ST, Cho TJ, Chang SJ, Chen JF, Hsieh MC. Visit-to-visit variability in blood pressure strongly predicts all-cause mortality in patients with type 2 diabetes: A 5.5-year prospective analysis. European journal of clinical investigation. 2012;42:245–253. doi: 10.1111/j.1365-2362.2011.02574.x. [DOI] [PubMed] [Google Scholar]
- 10.Design of the women's health initiative clinical trial and observational study. The women's health initiative study group. Control Clin Trials. 1998;19:61–109. doi: 10.1016/s0197-2456(97)00078-0. [DOI] [PubMed] [Google Scholar]
- 11.Curb JD, McTiernan A, Heckbert SR, Kooperberg C, Stanford J, Nevitt M, Johnson KC, Proulx-Burns L, Pastore L, Criqui M, Daugherty S Committee WMaM. Outcomes ascertainment and adjudication methods in the women's health initiative. Annals of epidemiology. 2003;13:S122–128. doi: 10.1016/s1047-2797(03)00048-6. [DOI] [PubMed] [Google Scholar]
- 12.Team DC. R foundation for statistical computing. Vienna, Austria: 2010. R: A language and environment for statistical computing. [Google Scholar]
- 13.Brickman AM, Reitz C, Luchsinger JA, Manly JJ, Schupf N, Muraskin J, DeCarli C, Brown TR, Mayeux R. Long-term blood pressure fluctuation and cerebrovascular disease in an elderly cohort. Arch Neurol. 2010;67:564–569. doi: 10.1001/archneurol.2010.70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Nagai M, Hoshide S, Ishikawa J, Shimada K, Kario K. Visit-to-visit blood pressure variations: New independent determinants for carotid artery measures in the elderly at high risk of cardiovascular disease. J Am Soc Hypertens. 2011;5:184–192. doi: 10.1016/j.jash.2011.03.001. [DOI] [PubMed] [Google Scholar]
- 15.Howard SC, Rothwell PM. Reproducibility of measures of visit-to-visit variability in blood pressure after transient ischaemic attack or minor stroke. Cerebrovasc Dis. 2009;28:331–340. doi: 10.1159/000229551. [DOI] [PubMed] [Google Scholar]
- 16.Muntner P, Joyce C, Levitan EB, Holt E, Shimbo D, Webber LS, Oparil S, Re R, Krousel-Wood M. Reproducibility of visit-to-visit variability of blood pressure measured as part of routine clinical care. Journal of hypertension. 2011;29:2332–2338. doi: 10.1097/HJH.0b013e32834cf213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Diaz KM, Veerabhadrappa P, Kashem MA, Feairheller DL, Sturgeon KM, Williamson ST, Crabbe DL, Brown MD. Relationship of visit-to-visit and ambulatory blood pressure variability to vascular function in african americans. Hypertension research. 2012;35:55–61. doi: 10.1038/hr.2011.135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Rothwell PM. Limitations of the usual blood-pressure hypothesis and importance of variability, instability, and episodic hypertension. The Lancet. 2010;375:938–948. doi: 10.1016/S0140-6736(10)60309-1. [DOI] [PubMed] [Google Scholar]
- 19.Rothwell PM, Howard SC, Dolan E, O'Brien E, Dobson JE, Dahlof B, Poulter NR, Sever PS. Effects of beta blockers and calcium-channel blockers on within-individual variability in blood pressure and risk of stroke. Lancet Neurol. 2010;9:469–480. doi: 10.1016/S1474-4422(10)70066-1. [DOI] [PubMed] [Google Scholar]
- 20.Webb AJ, Fischer U, Mehta Z, Rothwell PM. Effects of antihypertensive-drug class on interindividual variation in blood pressure and risk of stroke: A systematic review and meta-analysis. The Lancet. 2010;375:906–915. doi: 10.1016/S0140-6736(10)60235-8. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.