Abstract
Purpose
To compare and analyse the relationship between horizontal tear and root ligament tear of the posterior horn of the medial meniscus (PHMM) and the degree of varus in the axis of lower limb and body weight.
Methods
One hundred and nineteen patients underwent surgical treatment as they were diagnosed with medial meniscus tear in our hospital from May 2006 to December 2009. Of these, 19 cases (group 1), underwent partial meniscectomy as they were confirmed to solely have horizontal tear of the PHMM on arthroscopic examination and 27 cases (group 2), underwent subtotal meniscectomy as they were confirmed to solely have root ligament tear of the PHMM on arthroscopic examination, were chosen for retrospective study. Standing radiographs were taken of every case prior to arthroscopic surgery to measure varus angle. Also, we checked body mass index (BMI) of two groups. The difference of varus angle and BMI between two groups were statistically verified using the Levene’s test, paired t-test.
Results
Group 1 showed mean value of varus angle of 2.30 ± 0.54, and BMI of 25.32 ± 3.23. Group 2 showed mean value of varus angle of 5.64 ± 0.54, and BMI of 25.67 ± 3.12. The degree of varus of group 2 was statistically significantly higher than group 1 (p = 0.002). Comparison between the BMI of two groups showed no statistical significance (p = 0.053).
Conclusion
Through a comparative study of sole horizontal tear and root ligament tear of the PHMM, the authors have found that sole root ligament tear of the PHMM is more relative to the genu varum than sole horizontal tear of the PHMM. However, body weight was statistically irrelevant to the incidence of the two lesions.
Introduction
The degenerative horizontal tear of the posterior horn of the medial meniscus (PHMM) in late middle age is the most common type of injury of the meniscus [1, 2]. In a large-scale study targeting the middle aged or the elderly, a maximum of 35 % showed meniscus injury, and the prevalence increased with age [2]. On the other hand, in Asian countries certain postures, such as crossed-legged or crouching, are frequent in daily life, and could easily lead to the root ligament tear of the PHMM, the part where the PHMM is attached on the anterior tibia to the posterior cruciate ligament [3]. However, basic studies of the root ligament tear of the PHMM are rare.
The alignment of lower limb is one of the factors related with the meniscal tear. In many studies, including that by Bolano and Grana [4], the increased degree of varus of lower limb is reported to be related to the progression of osteoarthritis due to medial meniscus injury and articular cartilage injury [1, 2, 5, 6]. Also, many reports have proven the biomechanical relationship between body mass index (BMI) and medial meniscus tear [5], showing that high BMI brings about abnormalities of lower limb (genu varum), which accounts for the relationship of the progression of the degenerative osteoarthritis of the knee [7–13]. However, there have been no reports considering the relationship of the root ligament tear of the PHMM and the degree of genu varum and BMI.
The authors have noticed the horizontal tear of the PHMM and root ligament tear of the PHMM in the middle aged or the elderly that were unrelated to trauma. Even though these two types of lesion are anatomically very close together, the lesions vary by patients as degenerative horizontal tear or root ligament tear of the PHMM.
The authors postulated that body weight was more closely related to the sole horizontal tear of the PHMM than root ligament tear of PHMM for the initial development of tear of the PHMM area. Furthermore, the authors postulated that sole root ligament tear of the PHMM was more closely related to the innate varus deformity of the knee than the sole horizontal tear of the PHMM because they considered that the initial varus deformed knee would stress the root the ligament of the PHMM more significantly than the posterior body of medial meniscus biomechanically. The authors then compared and performed an analysis of the relationship between the two types of lesion and the degree of varus of the axis of lower limb and the body weight, targeting the middle aged or the elderly who underwent partial meniscectomy due to early degenerative horizontal tear of the PHMM and those who underwent subtotal meniscectomy due to complete tear of the root ligament of the PHMM.
Methods
Materials and duration
One hundred and nineteen patients underwent surgical treatment for the diagnosis of medial meniscus tear in our hospital from May 2006 to December 2009. Of these, 19 cases (group 1) underwent partial meniscectomy as they were confirmed to solely have horizontal tear of the PHMM on arthroscopic examination, and 27 cases (group 2) underwent subtotal meniscectomy as they were confirmed to solely have the root ligament tear of the PHMM on arthroscopic examination. These patients were chosen for retrospective study of the relationship between these two types of lesion and the patients’ lower limb alignment and body weight. Among the patients with no history of trauma, the inclusion criteria were cases with confirmed sole degenerative horizontal tear or complete root ligament tear of the PHMM on preoperative MRI, early degenerative arthritic findings of grade 0, 1 of Kellgren-Lawrence classification [14] on plain radiograph, or mild cartilage injury of grade 0, 1, 2 of Outerbridge classification [15] on arthroscopic surgery. In both groups, cases with any other ligament injury, arthritic finding of grade 2 or more of Kellgren-Lawrence classification, cartilage injury of grade 3 or more of Outerbridge classification, lateral meniscal tear, or meniscal complex tear with accompanied longitudinal, radial or flap tear were excluded.
Of the 19 cases of group 1, the mean age was 46.47 ± 2.63 years; 13 male and six female patients; 14 cases of grade 0 and five cases of grade 1 on radiological Kellgren-Lawrence classification; 12 cases of grade 1 and 7 cases of grade 2 on Outerbridge classification of arthroscopic findings. Of the 27 cases of group 2, the mean age was 57.5 ± 8.32 years; eight male and 19 female patients; 19 cases of grade 0 and eight cases of grade 1 on radiological Kellgren-Lawrence classification; 11 cases of grade 1 and 16 cases of grade 2 on Outerbridge classification of arthroscopic findings.
Measurement of mechanical axis and varus angle
Standing radiographs were taken of every case prior to arthroscopic surgery. We checked the “varus angle”. The varus angle is defined as the angle between the line of mechanical axis of the femur and the line of the tibial anatomical axis. The mechanical axis of the femur is the line connecting the centre of the femoral head and that of the articular side of the proximal tibia. The tibial anatomical axis is the line connecting the centre of the talus upper articular side and the centre of the articular side of the proximal tibia (Figs. 1 and 2). All radiological measurements were done manually twice by two different observers on PACS (Picture Archiving and Communication System, Loral, USA). For the evaluation between the observers, within the observers, Kappa value was used, and by the method of Fleiss JL, we judged that 0.75 or above was “excellent agreement”, below 0.75 was “fair to good agreement”, and below 0.4 was “poor agreement” [16].
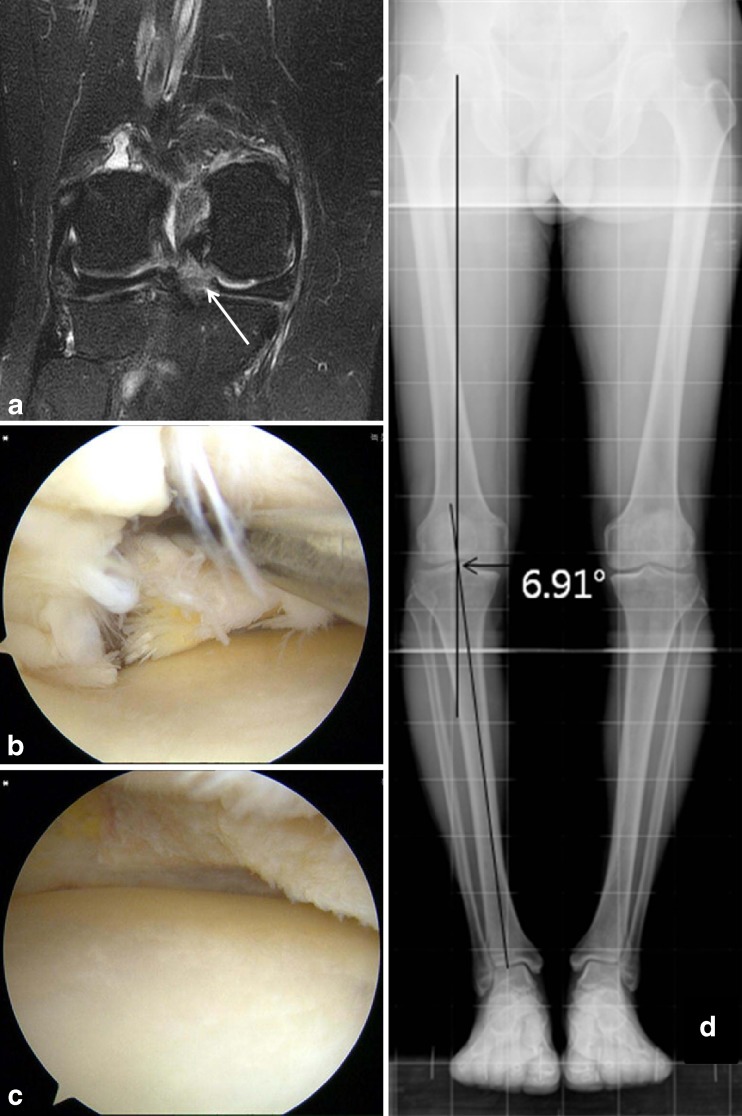
Fig. 1.
a MRI image of tear of the PHMM. b Arthroscopic finding was a horizontal tear of the PHMM on the left knee in a 46 year old man. c Partial meniscectomy was done. d The varus angle between the mechanical axis and the line connecting the centre of the talus upper articular side and the centre of the articular side of proximal tibia was measured
Fig. 2.
a MRI image of the root ligament tear of the PHMM. b Arthroscopic finding was degenerative root ligament tear of the PHMM (white arrow) right knee in a 79 year old woman. b Subtotal meniscectomy was done. c The varus angle between the mechanical axis and the line connecting the centre of talus upper articular side and the centre of articular side of the proximal tibia was measured
Understanding the relationship of body weight
For the evaluation of the relationship between the difference of body weight of the group with sole horizontal tear of the PHMM (group 1) and the group with sole complete root ligament tear of the PHMM(group 2), BMI [17], was used.
Statistical analysis
Before the study, a sample size analysis was performed. The sample size was chosen on the basis of the value of varus angle and BMI. We assumed an alpha error of 0.05 and applied an allocation ratio of 1. A sample size of 46 participants was calculated to provide 80 % power. The difference of the varus angle between the two groups was statistically verified using the Levene’s test and paired t-test, and was statistically significant since the p-value was below 0.05. When comparing the BMI of the two groups, paired t-test was used for the statistical verification, and considered statistically significant when the p-value was below 0.05.
Results
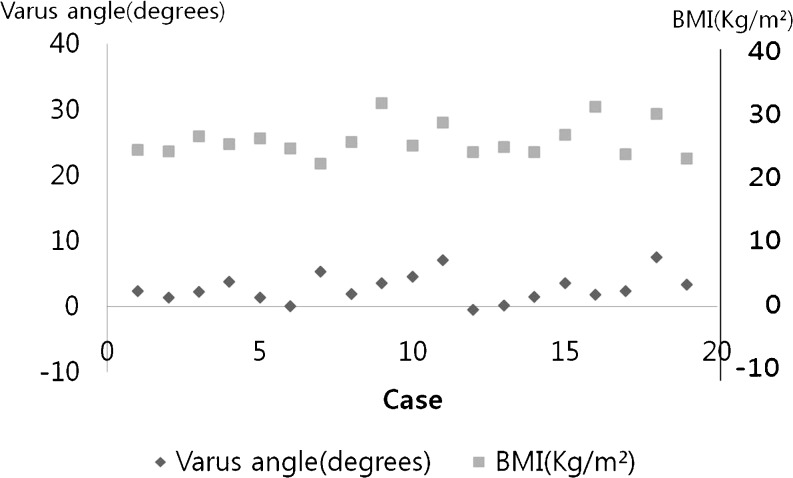
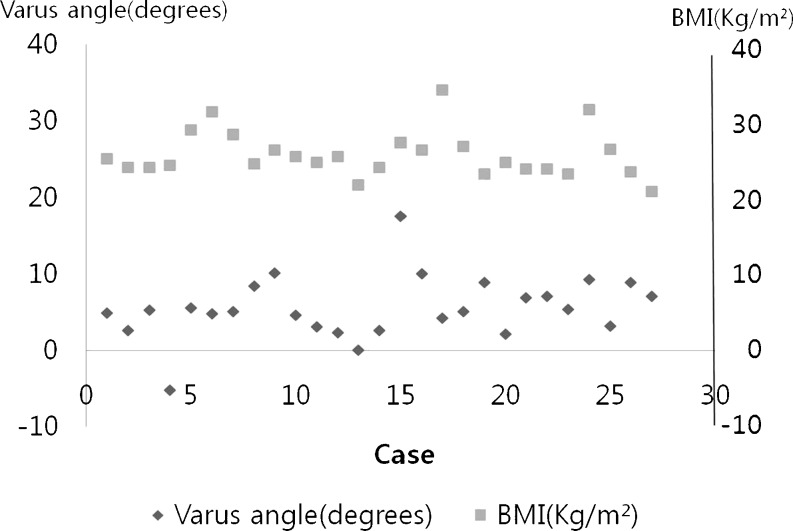
Group 1 showed mean value of varus angle of 2.30 ± 0.54, and BMI of 25.32 ± 3.23 (Table 1, Fig 3). Group 2 showed mean value of varus angle of 5.64 ± 0.54, and BMI of 25.67 ± 3.12 (Table 2, Fig 4). The degree of varus of group 1 was statistically significantly higher than group 2 (p = 0.002). Comparison between the BMI of two groups showed no statistical significance (p = 0.053). The mean age of group 1 was 46.47 years, in which age group the normal BMI value is ranged from 20 to 25 for males, and ranged from 22 to 27 for females, which means that the BMI of group 1 was within normal range. The mean age of group 2 was 57.5 years, in which age group the normal BMI value is ranged from 20 to 25 for males, and ranged from 23 to 28 for females, which means that the BMI of group 2 was also within normal range. Kappa value was 0.73 ± 0.023, which means “fair to good agreement”.
Table 1.
19 cases of group 1, who underwent partial meniscectomy as they were confirmed to have horizontal tear of the PHMM on arthroscopic examination, were measured for varus angle, weight, height and body mass index (BMI), and checked Kellgen-Lawrence grade and Outerbridge grade
| Case | Varus angle (degrees) | Weight (kg) | Height (cm) | BMIa | KLb | OBc |
|---|---|---|---|---|---|---|
| 1 | 2.35 | 73 | 175 | 23.83 | 0 | 1 |
| 2 | 1.39 | 73.2 | 176 | 23.63 | 0 | 2 |
| 3 | 2.26 | 75 | 170 | 25.95 | 1 | 2 |
| 4 | 3.7 | 73 | 172 | 24.67 | 0 | 1 |
| 5 | 1.37 | 69 | 164 | 25.65 | 0 | 1 |
| 6 | 0 | 67 | 167 | 24.02 | 1 | 2 |
| 7 | 5.24 | 63 | 170 | 21.79 | 0 | 1 |
| 8 | 1.93 | 65 | 161 | 25.07 | 1 | 2 |
| 9 | 3.52 | 87.6 | 168 | 31.03 | 1 | 2 |
| 10 | 4.53 | 58.2 | 154.3 | 24.45 | 0 | 1 |
| 11 | 7.06 | 83.4 | 172.6 | 27.99 | 0 | 2 |
| 12 | -0.5 | 72 | 175 | 23.51 | 0 | 1 |
| 13 | 0.16 | 63 | 161 | 24.3 | 1 | 2 |
| 14 | 1.4 | 61 | 161 | 23.53 | 0 | 1 |
| 15 | 3.52 | 80 | 175 | 26.12 | 0 | 1 |
| 16 | 1.82 | 85 | 167 | 30.47 | 0 | 1 |
| 17 | 2.28 | 63 | 165 | 23.14 | 0 | 1 |
| 18 | 7.5 | 66 | 150 | 29.33 | 0 | 1 |
| 19 | 3.27 | 64.5 | 169 | 22.58 | 0 | 1 |
| Mean | 2.3 | 70.62 | 169.99 | 25.32 |
aBody mass index
bKellgen-Lawrence grade
cOuterbridge grade
Fig. 3.
The relationship between varus angle and body mass index (BMI) of group 1 is drawn in graphs.* Body mass index
Table 2.
27 cases of group 2, who underwent subtotal meniscectomy as they were confirmed to have medial root ligament of the PHMM on arthroscopic examination, are measured varus angle, weight, height and body mass index (BMI), and checked Kellgen-Lawrence grade and Outerbridge grade
| Case | Varus angle (degrees) | Weight (kg) | Height (cm) | BMIa | KLb | OBc |
|---|---|---|---|---|---|---|
| 1 | 4.89 | 68.6 | 165.1 | 25.16 | 0 | 2 |
| 2 | 2.65 | 57 | 154 | 24.03 | 0 | 2 |
| 3 | 5.29 | 57 | 154 | 24.03 | 0 | 2 |
| 4 | 57.21 | 60.3 | 157.6 | 24.27 | 0 | 1 |
| 5 | 5.56 | 73.4 | 159.5 | 28.85 | 1 | 1 |
| 6 | 4.85 | 79 | 159 | 31.24 | 0 | 2 |
| 7 | 5.08 | 72 | 159.5 | 28.3 | 0 | 1 |
| 8 | 8.42 | 61.5 | 158.6 | 24.44 | 0 | 2 |
| 9 | 10.17 | 60 | 151 | 26.31 | 1 | 2 |
| 10 | 4.6 | 54 | 142 | 25.45 | 1 | 2 |
| 11 | 3.1 | 57 | 152 | 24.67 | 1 | 2 |
| 12 | 2.3 | 63.3 | 157.7 | 25.45 | 1 | 2 |
| 13 | 0 | 59 | 165 | 21.67 | 1 | 2 |
| 14 | 2.61 | 61.4 | 160 | 23.98 | 1 | 1 |
| 15 | 17.57 | 71.3 | 161.7 | 27.26 | 0 | 1 |
| 16 | 10.07 | 60 | 151 | 26.31 | 0 | 1 |
| 17 | 4.2 | 81 | 154 | 34.15 | 0 | 1 |
| 18 | 5.08 | 53.9 | 141.9 | 26.76 | 1 | 2 |
| 19 | 8.9 | 62.3 | 164 | 23.16 | 0 | 1 |
| 20 | 2.12 | 57 | 152 | 24.67 | 0 | 2 |
| 21 | 6.91 | 67.4 | 168.3 | 23.79 | 0 | 1 |
| 22 | 7.1 | 67.4 | 168.3 | 23.79 | 0 | 1 |
| 23 | 5.4 | 55.16 | 154.3 | 23.16 | 0 | 2 |
| 24 | 9.3 | 65.5 | 144.1 | 31.54 | 0 | 2 |
| 25 | 3.2 | 66.4 | 158.6 | 26.39 | 0 | 2 |
| 26 | 8.9 | 63 | 164 | 23.42 | 0 | 1 |
| 27 | 7.1 | 58.3 | 167.4 | 20.8 | 0 | 2 |
| Mean | 5.64 | 63.41 | 157.2 | 25.67 |
aBody mass index
bKellgen-Lawrence grade
cOuterbridge grade
Fig. 4.
The relationship between varus angle and body mass index (BMI) of group 2 is drawn in graphs. * Body mass index
Discussion
The meniscus has a important role of reinforcing and stabilising the incongruity of the femur and tibia, and knee meniscus is responsible for 40 ∼ 60 % of stress to the knee when standing, and 85 % when at 90 degrees flexion [1, 13]. Medial meniscus tears are more frequently reported since the medial structures are more firmly attached to the tibia, compared to the lateral meniscus which has relatively free range of motion [18]. Many studies have reported that varus deformity appeared to be closely related to the presence of medial meniscus tear conclusively [4, 6, 19–21]. But these results do not mean that varus deformity causes the medial meniscus tear, although varus deformity is a common conclusive finding of medial meniscus tear. There are no systematic reports about the factors that bring about the root ligament tear of the PHMM, although frequent cross-legged posture or crouching during daily life are the suspected reasons for such [3]. Traditionally, medial meniscus root tear has been treated by meniscectomy. However, a recent biomechanical study showed that a root ligament tear caused a 25 % increase in the peak contact pressure, whereas repair restored the peak contact pressure to normal [22]. Root ligament repair has gained interest since West et al. [23] described pullout repair of a lateral root ligament tear. Currently, that repair of the root ligament tear is accepted as standard management.
The authors have experienced not only sole horizontal tear of the PHMM without trauma in the middle aged, but also numerous cases of complete root ligament tear of the PHMM. Even though these two types of lesion are anatomically close together, the lesions vary by patients as degenerative horizontal tear or root ligament tear of the PHMM. The authors assumed this difference was caused mainly by the axis of the alignment of the lower limb and body weight, and conducted a retrospective study of the effects caused by them. We postulated that body weight was more closely related to the sole horizontal tear of the PHMM than root ligament tear of PHMM for the initial development of tear of the PHMM area. We also postulated that sole root ligament tear of the PHMM was more closely related to the innate varus deformity of the knee than the sole horizontal tear of the PHMM because we considered that initial varus deformed knee would stress the root the ligament of the PHMM more significantly than the posterior body of medial meniscus biomechanically. In our restrospective study, we confirmed that sole complete tear of the root ligament of the PHMM (group 2) had a more severe degree of varus of the axis of the lower limb alignment compared to the group with sole horizontal tear of the PHMM (group 1), and body weight (BMI) showed no correlation between the two groups in patients with relatively mild findings of degenerative osteoarthritis of knee on radiology, and with mild articular cartilage injury on arthroscopy.
Obesity brings about degenerative change to the joints with body stress. According to the study by Kelley et al. [24], Glyn et al. [25], and Kellgren and Lawrence [26], numerous cases of obesity have varus deformity of the knee, which is due to alteration of the centre of the gravity to the feet since the distance between both femurs is increased due to excessive fat, resulting in the injury of the meniscus, eventually leading to degenerative osteoarthritis of the knee. In other words, though the relationship between obesity and the tear of the medial meniscus related to degenerative arthritis of the knee is known, there is no reference to the relationship between sole horizontal tear of the PHMM and obesity, and sole root ligament tear of the PHMM and obesity. The reason why there was little difference in the relationship with obesity, the inducing factor of the degenerative change, between the two groups was that only cases with mild degenerative change were chosen and the BMI of both groups was in the normal range according to their age group. Additionally, already known, since increase in body weight is a significant factor for degenerative change, this study of cases of mild degenerative change has no significance.
The limitations of our study are that only a few cases and that only cases who underwent surgical treatment were chosen. Thus, further study is needed. In addition, using prospective biomechanical or cadaveric study, discovery of the independent cause of the root ligament tear of the PHMM from the cause of the horizontal tear is required.
Conclusion
The authors have found, through a comparative study of sole horizontal tear of the PHMM and sole complete root ligament tear of the PHMM, that the latter is more related to the genu varum than the former. However, body weight was statistically insignificant to the incidence of the two lesions.
Footnotes
Author contributions
Young-Mo Kim, M.D.,Ph.D. : literature search, study design, data analysis, data interpretation, writing.
Yong-Bum Joo, M.D. : literature search, data collection, data analysis, data interpretation, writing
Soo-Min Cha, M.D. : literature search, data collection, data analysis, data interpretation, writing, figures
Jung-Mo Hwang, M.D. : literature search, data collection, data analysis, data interpretation, writing, figures
References
- 1.Smillie IS (1978) Injuries of the knee joint. 5th ed. Curchill Livingston, Edinburgh 114-118
- 2.Englund M. Meniscal tear – a feature of osteoarthritis. Acta Orthop Scand Suppl. 2004;75:1–45. doi: 10.1080/03008820410002057. [DOI] [PubMed] [Google Scholar]
- 3.Nishimura A, Hasegawa M, Kato K, Yamada T, Uchida A, Sudo A. Risk factors for the incidence and progression of radiographic osteoarthritis of the knee among Japanese. Int Orthop. 2011;35:839–843. doi: 10.1007/s00264-010-1073-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bolano LE, Grana WA. Isolated arthroscopic partial meniscectomy. Functional radiographic evaluation at 5years. Am J Sports Med. 1993;21:432–437. doi: 10.1177/036354659302100318. [DOI] [PubMed] [Google Scholar]
- 5.Wendelboe AM, Hegmann KT, Biggs JJ, Cox CM, Portmann AJ, Gildea JH, Gren LH, Lyon JL. Relationships between body mass indices and surgical replacements of knee and hip joints. Am J Prev Med. 2003;25:290–295. doi: 10.1016/S0749-3797(03)00218-6. [DOI] [PubMed] [Google Scholar]
- 6.Jeong HJ, Park SJ, Shin HK, Kim EG, Choi JY, Lee JM. Analysis of the mechanical axis of the lower limb in patients with isolated meniscal tear. J Korea Knee Soc. 2009;21:286–291. [Google Scholar]
- 7.Boytim MJ, Smith JP, Fischer DA, Quick DC. Arthroscopic posteromedial visualization of the knee. Clin Orthop Relat Res. 1995;310:82–86. [PubMed] [Google Scholar]
- 8.Burks RT, Metcalf MH, Metcalf RW. Fifteen-year follow-up of arthroscopic partial meniscectomy. Arthroscopy. 1997;13:673–679. doi: 10.1016/S0749-8063(97)90000-1. [DOI] [PubMed] [Google Scholar]
- 9.Cooper C, McAlindon T, Snow S, Vines K, Young P, Kirwan J, Dieppe P. Mechanical and constitutional risk factors for symptomatic knee osteoarthritis: differences between medial tibiofemoral and patellofemoral disease. J Rheumatol. 1994;21:307–313. [PubMed] [Google Scholar]
- 10.Felson DT, Anderson JJ, Naimakr A, Walker AM, Meenan RF. Obesity and knee osteoarthritis. The Framingham study. Ann Intern Med. 1998;109:18–24. doi: 10.7326/0003-4819-109-1-18. [DOI] [PubMed] [Google Scholar]
- 11.Felson DT. The epidemiology of knee osteoarthritis: result from the framingham osteoarthritis study. Semin Arthritis Rheum. 1990;20:42–50. doi: 10.1016/0049-0172(90)90046-I. [DOI] [PubMed] [Google Scholar]
- 12.Hart DJ, Spector TD. The relationship of obesity, fat distribution and osteoarthritis in women in the general population: the chingford study. J Rheumatol. 1993;20:331–335. [PubMed] [Google Scholar]
- 13.Leach RE, Baumgard S, Broom J. Obesity: its relationship to osteoarthritis of the knee. Clin Orthop Relat Res. 1973;93:271–273. doi: 10.1097/00003086-197306000-00030. [DOI] [PubMed] [Google Scholar]
- 14.Kellgren JH, Lawrence JS. Radiological assessment of osteoarthrosis. Ann Rheum Dis. 1957;16:494–502. doi: 10.1136/ard.16.4.494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Outerbridge RE. The etiology of chondromalacia patellae. J Bone Joint Surg Br. 1961;43-B:752–757. doi: 10.1302/0301-620X.43B4.752. [DOI] [PubMed] [Google Scholar]
- 16.Fleiss JL, Cohen J. The equivalence of weighted kappa and the intraclass correlation coefficient as measures of reliability. Educ Psychol Meas. 1973;33:613–619. doi: 10.1177/001316447303300309. [DOI] [Google Scholar]
- 17.Bray GA. Overweight is risking fate. Definition, classification, prevalence, and risks. Ann N Y Acad Sci. 1987;31:14–28. doi: 10.1111/j.1749-6632.1987.tb36194.x. [DOI] [PubMed] [Google Scholar]
- 18.Lim HC, Lee SH, Shon WY, Lee DW. A clinical study of meniscus injury. J Korean Orthop Assoc. 1989;24:27–33. [Google Scholar]
- 19.McBride GG, Constine RM, Hofmann AA, Carson RW. Arthroscopic partial medial menisectomy in older patient. J Bone Joint Surg Am. 1984;66:547–551. [PubMed] [Google Scholar]
- 20.Habata T, Ishimura M, Ohgushi H, Tamai S, Fujisawa Y. Axial alignment of the lower limb in patients with isolated meniscal tear. J Orthop Sci. 1998;3:85–89. doi: 10.1007/s007760050026. [DOI] [PubMed] [Google Scholar]
- 21.Niinimäki TT, Eskelinen A, Ohtonen P, Junnila M, Leppilahti J (2012) Incidence of osteotomies around the knee for the treatment of knee osteoarthritis: A 22-year population-based study. Int Orthop. [Epub ahead of print] doi:10.1007/s00264-012-1508-7 [DOI] [PMC free article] [PubMed]
- 22.Allaire R, Muriuki M, Gilbertson L, Harner CD. Biomechanical consequences of a tear of the posterior root of the medial meniscus. Similar to total meniscectomy. J Bone Joint Surg Am. 2008;90:1922–1931. doi: 10.2106/JBJS.G.00748. [DOI] [PubMed] [Google Scholar]
- 23.West RV, Kim JG, Armfield D, Harner CD. Lateral meniscal root tears associated with anterior cruciate ligament injury: classification and management. ANNA. 2004;20:e32–e33. [Google Scholar]
- 24.Kelley WN, Harris EDJR, Ruddy S, Sledge CB. Textbook of Rheumatology. Philadelphia: Saunders; 1981. [Google Scholar]
- 25.Glyn JH, Sutherland I, Walker GF, Young AC. Low Incidence of osteoarthritis in hip and after ant polio. A late review. Br Med J. 1996;2:739–742. doi: 10.1136/bmj.2.5516.739. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kellgren JH, Lawrence JS. Osteoarthrosis and disc degeneration in an urban population. Ann Rheum Dis. 1958;17:388–397. doi: 10.1136/ard.17.4.388. [DOI] [PMC free article] [PubMed] [Google Scholar]