Abstract
Purpose
The surgical technique, medial patellar retinaculum plasty, can almost restore both static and dynamic stability and verge on anatomical repair for the treatment of habitual patellar dislocation in adolescents.
Methods
In accordance with the injury patterns of the medial patellar retinaculum through knee MRI, we repaired different injury sites with this surgical procedure. We reviewed this technique in 16 patients with an average age of 15 years. Retrospective review of charts and radiographs immediately after the surgery up to the latest follow-up (range 12–36 months) was undertaken.
Results
All patients were evaluated clinically and radiologically over an average of 20.7 months. The recovery of knee mobility results were good. No recurrence of patellar instability has been found.
Conclusion
We think this could be a valid technique to treat habitual patellar dislocation in adolescents.
Introduction
Potential anatomical abnormalities are one of the major reasons for adolescents to develop habitual patella dislocation, such as the femoral trochlear dysplasia, Q angle increase, tibial tubercle–trochlear groove distance (TTTG distance) increase, lateral soft tissue contracture and medial soft tissue relaxation [1, 2]. In addition, poor healing of the patellar retinaculum after traumatic dislocation is also a major risk factor [3, 4]. Most experts advocate surgical treatment. Traditionally, reefing of medial capsule was performed, but it had a high recurrence rate, and the postoperative results were not satisfactory [2, 5]. Later surgeons tried to transfer the tendons for reconstruction. Ostermeier et al. described their technique of transferring the semitendinosus tendon to complete MPFL reconstruction [6]. Steensen et al. [7] described a simple technique for MPFL reconstruction by transferring gracilis tendons, but those operations could not restore the static stability and the dynamic stability of the knee, moreover, they were not anatomical reconstructions. Studies confirmed that the MPFL contributes about 53–60 % of the total medial restraining force as a distinct restraining structure in the second layer of the medial soft tissues [8–10]. Wang et al. [11] found that fibres of the MPFL form two relatively concentrated fibre bundles: the superior-oblique bundle and the inferior-straight bundle. Many clinical findings have shown that acute patellar dislocation is associated with a high rate of MPFL injuries [12–14]; thus, based on the latest anatomical research [11], double bundle anatomical reconstruction of the MPFL is more popular, as this method can restore the MPFL structure, and thus recover both the static stability and the dynamic stability of the knee. However, it involves drilling a tunnel in the femur to fix the graft [15]. Therefore in adolescents with open growth plates, this surgical technique can damage the growth plate if used inappropriately. In view of this, we proposed a new surgical technique called the medial patella retinaculum plasty. In recent years, different patterns of MPFL injury have been reported, so that, in accordance with the injury patterns of the medial patellar retinaculum, we will describe different injury sites to complete the medial patellar retinaculum plasty.
Materials and methods
Patients
From June 2005 to January 2009, 17 patients with recurrent patellar dislocation were operated upon in our hospital. We defined recurrent patella dislocation as more than one traumatic episode, in which disruption of the normal position of the patella within the femoral groove occurred. Of the 17 patients, seven were boys and ten were girls, with a mean age of 15 years (range 12–18 years). From MRI of knee joint [16], eight patients had only injured the medial patellar retinaculum near the patella, one patient had only a femoral attachment injury and the others had injury to both femoral attachment and patella attachment of the medial patellar retinaculum. All those patients were treated by the same experienced senior orthopaedic surgeons using the same technique. A single independent observer evaluated the results of all patients.
Surgical technique
For injury of the medial patella retinaculum near the patella alone, the surgical procedure was as follows (Figs. 1, 2 and 3):
A physical examination was performed to assess patellar tracking under anaesthesia. Routine diagnostic arthroscopy was performed to observe the intra-articular tracking of patellar through the standard inferolateral and inferomedial portals, and at the same time, to release the lateral patellar retinaculum. The lateral patellar retinaculum release is still a widely used standard surgical technique and is the primary surgical intervention for patellar dislocation when combined with medial patellar retinaculum plication [17].
A 5-cm longitudinal skin incision was made centred on the anterior region of knee. We held the incision open by two retractors and split the superficial fascia; then deepened the dissection up to the medial retinaculum then the medial patellar soft tissue (vastus medialis obliquus muscle fibres, medial patella retinaculum, the joint capsule) was elevated off the medial patella without violation of the anatomical layer.
A longitudinal incision was made along the medial border of the patella and a transverse incision was made at the junction of the vastus medialis obliquus and the medial patellar retinaculum, then the two parts were clamped separately with haemostats (Fig. 4).
We then centred the patella in the trochlear groove. At 30 degrees of knee flexion, the far end was pulled approximately to the lateral proximal border of the patellar border, and was sutured temporarily onto the surface of the patella with a no. 2 nonabsorbable whipstitch; then the vastus medialis oblique muscle fibres were pulled to the lateral distal end border of the patella approximately, and overlapped on the far end, sutured temporarily to the surface of patella with a no. 2 nonabsorbable whipstitch (Fig. 5).
We observed the patellofemoral joint relationship by arthroscopy, and particular attention was paid to see whether the patellar tracking was normal through the range of motion of the knee, and then an assistant manually adjusted the tension and position of the two ends using the temporary sutures. The suturing needs to be done under tension. Insufficient tension would result in a lack of correction of the lateral instability, whereas excessive tension would cause increased pressure on the medial patellofemoral joint and might restrict knee range of motion. Then we sutured the far end with PDS-I whipstitch, and sutured the vastus medialis oblique muscle fibres to the far end on the surface of patella, and sutured the inter connecting area with PDS-I whipstitch. Finally, the incision was irrigated and closed in layers.
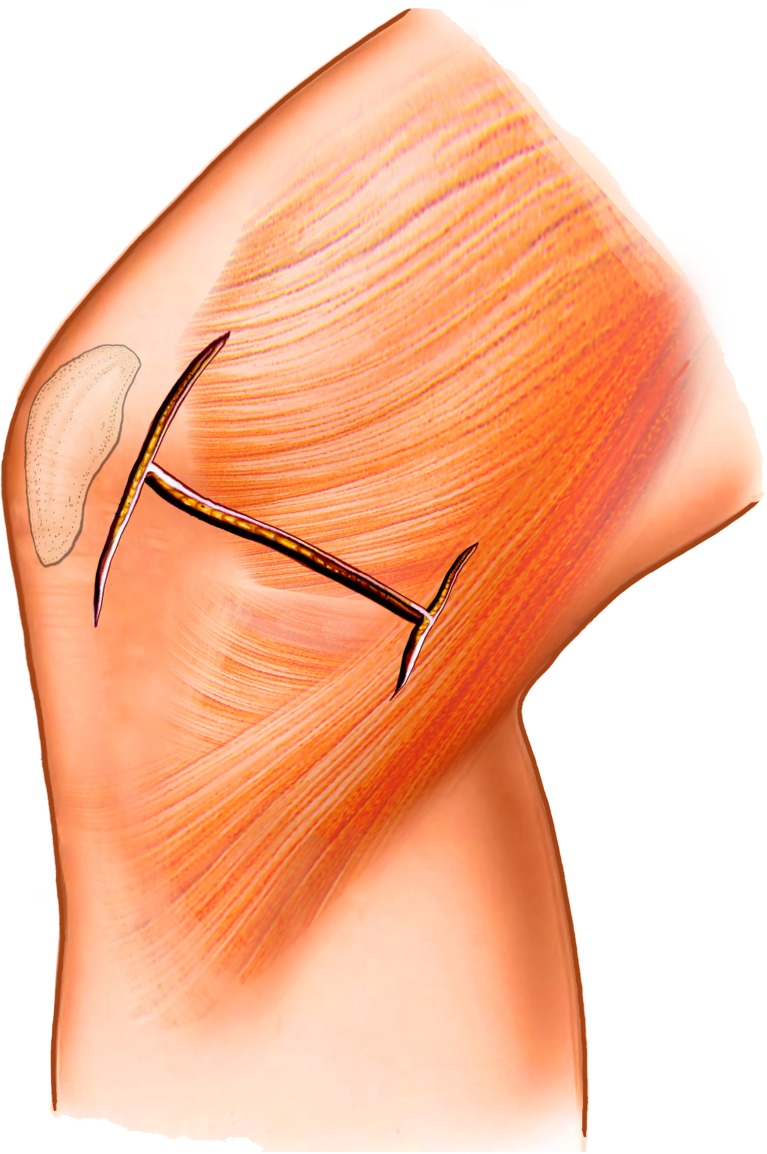
Fig. 1.
A longitudinal incision is made along the medial border of the patellar, then a transverse incision was made at the junction of the vastus medialis obliquus and the medial patellar retinaculum and a transverse incision was made at the inferior border of medial patellar retinaculum
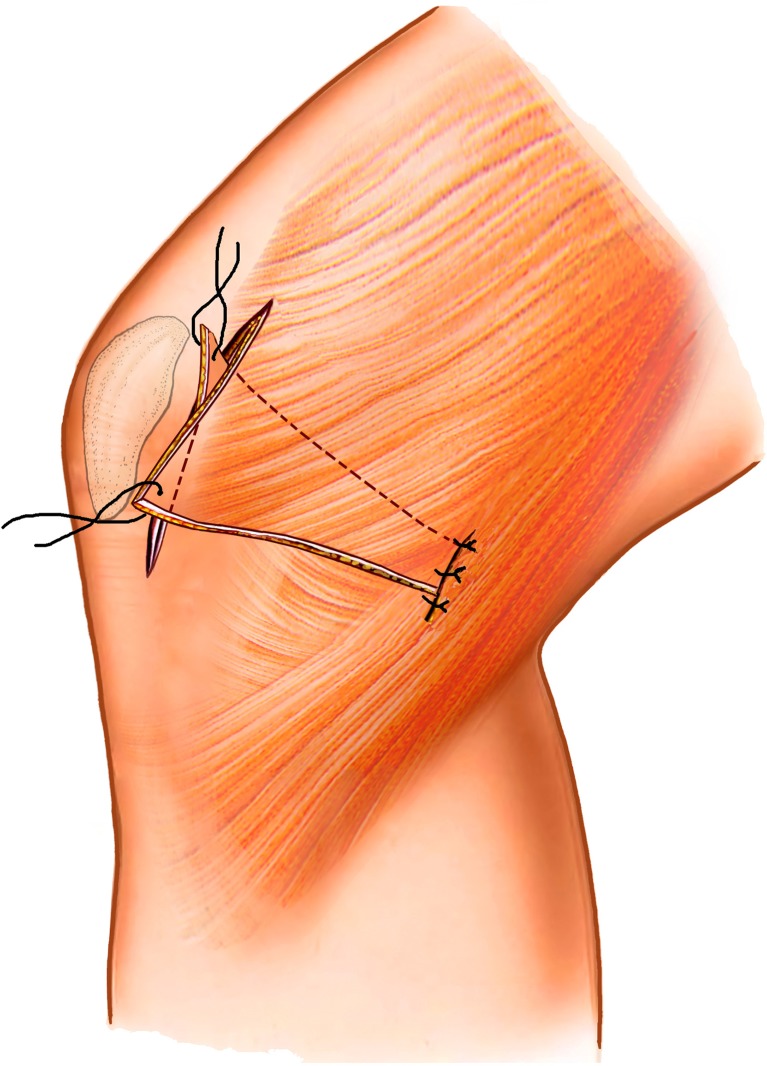
Fig. 2.
We made overlapped sutures at the inferior border of medial patellar retinaculum, and then, at 30 degrees of knee flexion, the medial patellar retinaculum end was pulled approximately to the lateral proximal border of the patellar, and the vastus medialis oblique muscle fibres were pulled approximately to the lateral distal end border of the patella
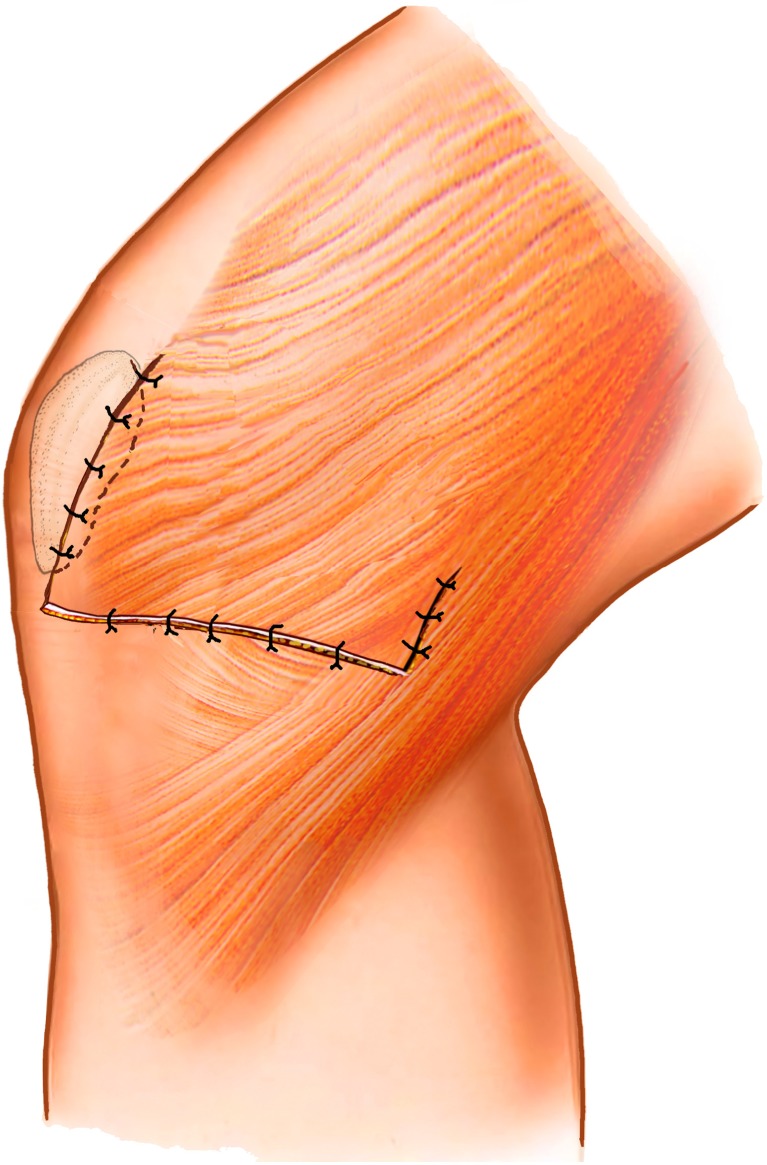
Fig. 3.
We sutured the vastus medialis oblique muscle fibres to the medial patellar retinaculum end on the surface of patella
Fig. 4.
The transverse incision which was made at the junction of the vastus medialis obliquus and the medial patellar retinaculum. VMO vastus medialis obliquus
Fig. 5.
The vastus medialis obliquus and the medial patellar retinaculum were overlapped. VMO vastus medialis obliquus
In some patients avulsion of the medial patellar retinaculum affected both femoral attachment and patella attachment and the procedure was then as follows:
Before repairing the injury to medial patella retinaculum, we made a 3-cm longitudinal skin incision between the adductor tubercle and condylus medialis. Then we split the superficial fascia, deepened the dissection and exposed the stub which was removed with scissors. Next, a transverse incision was made at the injured inferior border of medial patellar retinaculum and the two parts were clamped separately with haemostats (Fig. 6). The far end was pulled to the proximal border of the adductor tubercle while the proximal end was pulled approximately to the distal border of the adductor tubercle (Fig. 7). Lastly, we sutured the two parts with PDS-I. After the repairing the injury of the medial patellar retinaculum, the incision was irrigated and incision closed in layers.
Postoperatively, the knee was immobilised in full extension and immediate quadriceps strengthening was initiated. After two days, all the patients started knee flexion exercises, and within four weeks flexion gradually increased to 90°. Patients could walk on crutches after two days and after four weeks full weight bearing was resumed. After two months they could return to normal work and at four months could resume normal sports.
Fig. 6.
A transverse incision was made at the injured inferior border of medial patellar retinaculum, then the two parts were clamped separately with hemostats
Fig. 7.
The far end was pulled to the proximal border of the adductor tubercle while the proximal end was pulled approximately to the distal end border of the adductor tubercle
Assessment
The mean follow-up was 20.7 months (range 12–36 months). All patients completed a preoperation and postoperation Kujala knee questionnaire and Lysholm knee questionnaire. In addition, we also evaluated patients with the statement that best described the results of the surgical procedure, outlined by Drez et al. [18] as follows: (1) The knee has markedly improved, and I have returned to all activities; (2) The knee has improved, but there is still occasional discomfort or problems in sports activities; (3) The knee has improved, but I am still unable to return to sports activities; or (4) The knee is not better or is worse than before surgery. The patient response to this question yielded the subjective evaluation of excellent, good, fair, or poor, respectively. Finally, an inquiry was made into any dislocations or subluxations since the operation.
A thorough knee examination was performed on both knees of each patient. The examination included evaluation of quadriceps angles, medial or lateral facet tenderness, lateral or medial mobility, lateral retinacular tenderness, apprehension to lateral displacement, lateral patellar tilt, presence of pain with patellar compression against the trochlear grove and range of motion and persistent quadriceps atrophy.
Radiographic evaluation included the patellar tilt and the lateral shift ratio. The same measurements were then made on the preoperative radiographs, and the two were compared. Data obtained from the radiographs were compared by Student's paired t test, and significance was set at P = 0.05.
Results
To date, of the 17 patients with habitual patella dislocation who have been treated by this technique, no recurrence of patellar instability has been found. One patient was lost to follow-up. The mean Kujala score at follow-up was 93.4 (range 88–100). The mean Lysholm score was 92.3 (range 87–99). Based on this score, 11 knees (69 %) had excellent results, three (19 %) had good results, and two (12 %) had fair results. The average postoperative quadriceps angle was 12.8° (range 10–20°). One patient had some mild medial facet tenderness, and no patient exhibited mild medial patellar hypermobility. Three patients lost some flexion but no flexion loss exceeded 10°. No loss of extension existed in any patient. There was some degree of quadriceps atrophy in eight patients. Four patients had less than two centimetres of atrophy, while three patients had two to three centimetres of atrophy. No patient had lateral retinacular tenderness, apprehension to lateral displacement of the patella or pain on patellar compression against the trochlear groove. Radiographically, the patellar tilt showed improvement from 12.2° (range 9–16°) preoperatively to 6.8° (range 5–9°) postoperatively (P = 0.000). The lateral shift ratio improved from 18.8 (range 9–16) preoperatively to 8.9 (range 6–13) at latest follow-up (P = 0.000). Results of the physical examination, questionnaire, knee score results, and radiographic examination are summarised in Tables 1 and 2.
Table 1.
Physical examination results
| Patient | Medial facet tenderness | Lateral retinacular tenderness | Patellar hypermobility | Flexion loss | Quadriceps atrophy |
|---|---|---|---|---|---|
| 1 | Mild | —— | —— | —— | 2 cm |
| 2 | —— | —— | —— | 8° | 1.5 cm |
| 3 | —— | —— | —— | —— | —— |
| 4 | —— | —— | —— | —— | —— |
| 5 | —— | —— | —— | 5° | 2.5 cm |
| 6 | —— | —— | —— | —— | —— |
| 7 | —— | —— | —— | —— | 1 cm |
| 8 | —— | —— | —— | —— | —— |
| 9 | —— | —— | —— | —— | —— |
| 10 | —— | —— | —— | —— | 2.5 cm |
| 11 | —— | —— | —— | —— | —— |
| 12 | —— | —— | —— | 10° | 3 cm |
| 13 | —— | —— | —— | —— | 1 cm |
| 14 | —— | —— | —— | —— | —— |
| 15 | —— | —— | —— | —— | —— |
| 16 | —— | —— | —— | —— | —— |
Table 2.
Radiographic examination results
| Patient | Kujala score | Lysholm score | Patellar tilt | Lateral shift ratio | ||||
|---|---|---|---|---|---|---|---|---|
| Preop | Postop | Preop | Postop | Preop | Postop | Preop | Postop | |
| 1 | 50 | 88 | 60 | 90 | 15° | 8° | 15 | 8 |
| 2 | 55 | 90 | 58 | 87 | 10° | 6° | 17 | 7 |
| 3 | 60 | 98 | 58 | 95 | 12° | 7° | 20 | 12 |
| 4 | 68 | 100 | 55 | 90 | 11° | 6° | 24 | 13 |
| 5 | 58 | 90 | 65 | 98 | 10° | 5° | 22 | 10 |
| 6 | 54 | 89 | 62 | 94 | 15° | 9° | 15 | 7 |
| 7 | 59 | 92 | 66 | 99 | 14° | 9° | 17 | 9 |
| 8 | 61 | 95 | 64 | 89 | 12° | 6° | 19 | 8 |
| 9 | 55 | 94 | 57 | 96 | 14° | 8° | 15 | 7 |
| 10 | 59 | 98 | 60 | 98 | 13° | 7° | 23 | 12 |
| 11 | 53 | 88 | 50 | 89 | 10° | 5° | 20 | 10 |
| 12 | 62 | 96 | 59 | 93 | 9° | 5° | 24 | 10 |
| 13 | 56 | 96 | 58 | 94 | 16° | 9° | 19 | 8 |
| 14 | 60 | 98 | 63 | 98 | 11° | 6° | 17 | 9 |
| 15 | 65 | 89 | 60 | 95 | 10° | 7° | 18 | 6 |
| 16 | 55 | 94 | 53 | 88 | 14° | 6° | 16 | 7 |
Discussion
Non-surgical treatment is unsatisfactory because the normal anatomy is not restored [19, 20]. Thus, surgical treatment is more appropriate for recurrent dislocation of the patella. Many studies have confirmed that MPFL is the primary soft tissue restraint for lateral patella dislocation, and there is always MPFL injury associated with the patellar dislocation. When conservative management fails, if the injured MPFL was not repaired there is a risk of recurrent patella dislocation [1]. The reefing of the medial capsule has been popular in the past, but fails to restore the anatomical structure of MPFL [21]. Others have tried to perform a tendon transposition surgery, using the semitendinosus tendon [12], gracilis tendons [13], and so on. Though they reported no recurrent short-term patellar dislocation and statistically significant short-term improvement on the Kujala score for all patients, there was little information about the long-term outcomes. Furthermore these techniques are no substitute for MPFL due to the nonanatomical reconstruction. Recently, with in-depth research on the anatomy of MPFL, Wang et al. [14] found that from approximately the femoral origin, fibres of the MPFL form two relatively concentrated fibre bundles: the superior-oblique bundle and the inferior-straight bundle. The inferior-straight bundle is the main static soft tissue restraint whereas the superior-oblique bundle associated with vastus medialis obliquus (VMO) serves as the main dynamic and static union stability structure. Based on this theory, the double-bundle anatomical medial patellofemoral ligament reconstruction was proven to be more effective.
Though medial patellofemoral ligament reconstruction surgery can restore the local anatomical structure, in adolescents, bony procedures are not recommended due to the potential damage to the growth plate. Thus treatment of habitual patella dislocation in adolescents is still a clinical challenge.
Under these circumstances, we have introduced the medial patella retinaculum plasty to solve this problem. In this operation, the vastus medialis oblique head, fascia and joint capsule are used to constitute the new medial stable complex which enhances the tension of the medial patellar retinaculum, restores the anatomical structure of the MPFL, and strengthens the synergistic effect of the MPFL and the VMO. The far end is pulled to the lateral proximal border of the patella, shortening the medial patella retinaculum, so that it has a strong transverse tension in quiescent conditions. The vastus medialis oblique head pulled to the lateral distal end of the patella, which enhances the tensile force of the vastus medialis. Furthermore, the vastus medialis oblique head, fascia and joint capsule are used to constitute the new medial stable complex which enhances the strength of the medial patellar retinaculum, forming a vector structure of a triangle and almost restoring the local anatomical structure.
However, in the clinical context, different patterns of MPFL injury have been reported; in addition, Elias et al. [22] reported more than one site of injury to the medial stabilisers. To date, most authors have proposed that injury to the MPFL is almost always close to or at the femoral attachment site. Balcarek et al. [23] considered that an isolated injury to the MPFL at or close to the femoral origin was found in only 50.0 % of their cases, and injury to the patellar attachment, to the midsubstance site, or to more than one site of injury was found in 13.9 %, 13.9 %, and 22.2 % respectively. Our researches revealed that there were three patterns injury of the MPFL: isolated region injury, combined region injury and combined injury. Combined region injury is defined as an injury from that point to the medial patellar margin, to the femoral origin is called the isolated region injury and the combined injury is the coexistence of the combined region and isolated region injury. For femoral attachment injury only, we also repaired the patellar attachment to enhance the strength of the medial patellar retinaculum. Once there are injuries to both femoral attachment and patella attachment, our technique is very practical. Because both the repair to the femoral attachment and patella attachment can maintain the integrity of the medial patella retinaculum, recover its anatomical structure and balance its tension.
Conclusion
For adolescents, patellar instability is a clinical disease caused by multiple factors, and any single operation is not ideal. With further studies on the MPFL anatomy, restoration of the static and dynamic stability is extremely important. Our surgical application can enhance the strength of the vastus medialis and the tension of the medial patella retinaculum. Moreover, the new retinaculum can restore the anatomical function of MPFL almost to its full capacity, and restore the static and dynamic stability of patellar.
Footnotes
Drs Ji, Wang, Zhang, Chen, Ma and Dong have no relevant financial relationships to disclose.
References
- 1.Sallay PI, Poggi J, Speer KP, et al. Acute dislocation of the patella. A correlative pathoanatomic study. Am J Sports Med. 1996;24(1):52–60. doi: 10.1177/036354659602400110. [DOI] [PubMed] [Google Scholar]
- 2.Senacongse W, Amis AA. The effects of articular, or muscular deficiencies on patellofemoral joint stability. J Bone Joint Surg Br. 2005;87(4):577–582. doi: 10.1302/0301-620X.87B4.14768. [DOI] [PubMed] [Google Scholar]
- 3.Herrington L, Nester C. Q-angle undervalued? The relationship between Q-angle and medio-lateral position of the patella. Clin Biomech (Bristol, Avon) 2004;19(10):1070–1073. doi: 10.1016/j.clinbiomech.2004.07.010. [DOI] [PubMed] [Google Scholar]
- 4.Andrikoula S, Tokis A, Vasuliadis HS, et al. The extensor mechanism of the knee joint: an anatomical study. Knee Surg Sports Traumatol Arthrosc. 2006;14(3):214–220. doi: 10.1007/s00167-005-0680-3. [DOI] [PubMed] [Google Scholar]
- 5.Panagopoulos A, Niekerk L, Triantafillopoulos IK. MPFL reconstruction for recurrent patella dislocation: a new surgical technique and review of the literature. Int J Sports Med. 2008;29:359–365. doi: 10.1055/s-2007-965360. [DOI] [PubMed] [Google Scholar]
- 6.Ostermeier S, Holst M, Bohnsack M, et al. In vitro measurement of patellar kinematics following reconstruction of the medial patellofemoral ligament. Knee Surg Sports Traumatol Arthrosc. 2007;15(3):276–285. doi: 10.1007/s00167-006-0200-0. [DOI] [PubMed] [Google Scholar]
- 7.Steensen RN, Dopirak RM, Maurus PB. A simple technique for reconstruction of the medial patellofemoral ligament using a quadriceps tendon graft. Arthroscopy. 2005;21(3):365–370. doi: 10.1016/j.arthro.2004.10.007. [DOI] [PubMed] [Google Scholar]
- 8.Davis DK, Fithian DC. Techniques of medial retinacular repair and reconstruction. Clin Orthop Relat Res. 2002;402:38–52. doi: 10.1097/00003086-200209000-00005. [DOI] [PubMed] [Google Scholar]
- 9.Warren LF, Marshall JL. The supporting structures and layers on medial side of the knee: an anatomical analysis. J Bone Joint Surg. 1979;61A:56–62. [PubMed] [Google Scholar]
- 10.Desio SM, Burks RT, Bachus KN. Soft tissue restraints to lateral patellar translation in the human knee. Am J Sports Med. 1998;26(1):59–65. doi: 10.1177/03635465980260012701. [DOI] [PubMed] [Google Scholar]
- 11.Kang HJ, Wang F, Chen BC, et al. Functional bundles of the medial patellofemoral ligament. Knee Surg Sports Traumatol Arthrosc. 2010;18:1511–1516. doi: 10.1007/s00167-010-1090-8. [DOI] [PubMed] [Google Scholar]
- 12.Nomura E, Horiuchi Y, Kihara M. Medial patellofemoral ligament restraint in lateral patellar translation and reconstruction. Knee. 2000;7:121–127. doi: 10.1016/S0968-0160(00)00038-7. [DOI] [PubMed] [Google Scholar]
- 13.Amis AA, Firer P, Mountney J, et al. Anatomy and biomechanics of the medial patellofemoral ligament. Knee. 2003;10:215–220. doi: 10.1016/S0968-0160(03)00006-1. [DOI] [PubMed] [Google Scholar]
- 14.Nomura E, Inoue M. Injured medial patellofemoral ligament in acute patellar dislocation. J Knee Surg. 2004;17:1–7. doi: 10.1055/s-0030-1247148. [DOI] [PubMed] [Google Scholar]
- 15.Wang F, Kang HJ, Chen BC, et al. Combination of medial patellofemoral ligament reconstruction with vastus medialis advancement for chronic patellar dislocation. Chin Med J. 2010;123(21):3024–3029. [PubMed] [Google Scholar]
- 16.Nomura E. Classification of lesions of the medial patello-femoral ligament in patellar dislocation. Int Orthop. 1999;23(5):260–263. doi: 10.1007/s002640050366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Haspl M, Cicak N, Klobucar H, Pecina M. Fully arthroscopic stabilization of the patella. Arthroscopy. 2002;18(1):E2. doi: 10.1053/jars.2002.29868. [DOI] [PubMed] [Google Scholar]
- 18.Drez D, Edwards T, Williams C. Results of medial patellofemoral ligament reconstruction in the treatment of patellar dislocation. Arthroscopy. 2001;17:298–306. doi: 10.1053/jars.2001.21490. [DOI] [PubMed] [Google Scholar]
- 19.Buchner M, Baudendistel B, Sabo D, et al. Acute traumatic primarypatellar dislocation: long-term results comparing conservative and surgical treatment. Clin J Sport Med. 2005;15:62–66. doi: 10.1097/01.jsm.0000157315.10756.14. [DOI] [PubMed] [Google Scholar]
- 20.Apostolovic M, Vukomanovic B, Slavkovic N, et al. Acute patellar dislocation in adolescents: operative versus nonoperative treatment. Int Orthop. 2011;35(10):1483–1487. doi: 10.1007/s00264-011-1265-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ahmad CS, Stein BE, Matuz D, Henry JH. Immediate surgical repair of the medial patellar stabilizers for acute patellar dislocation. Am J Sports Med. 2000;28:804–810. doi: 10.1177/03635465000280060701. [DOI] [PubMed] [Google Scholar]
- 22.Elias DA, White LM, Fithian DC. Acute lateral patellar dislocation at MR imaging: Injury patterns of medial patellar soft-tissue restraints and osteochondral injuries of the inferomedial patella. Radiology. 2002;225:736–743. doi: 10.1148/radiol.2253011578. [DOI] [PubMed] [Google Scholar]
- 23.Balcarek P, Ammon J, Frosch S, et al. Magnetic resonance imaging characteristics of the medial patellofemoral ligament lesion in acute lateral patellar dislocations considering trochlear dysplasia, patella alta, and tibial tuberosity–trochlear groove distance. Arthroscopy. 2010;26(7):926–935. doi: 10.1016/j.arthro.2009.11.004. [DOI] [PubMed] [Google Scholar]