Abstract
Purpose
The study aim was to describe what kind of operative technique performs best with respect to initial strength after the surgical repair of acute Achilles tendon ruptures.
Methods
We performed a systematic search of the keywords “Achilles tendon AND (suture strength OR biomechanics) AND (cadaver NOT animal)” in the online databases PubMed, EMBASE, CINAHL, and the Cochrane Library. We included studies that employed open, mini-open, or percutaneous Achilles tendon repair in human cadavers, and assessed some measure of tensile strength as a primary outcome.
Results
Our search produced 11 relevant papers reporting results for Kessler, Bunnell, and Krackow sutures in open repair, as well as the Achillon device, the Ma-Griffith repair technique, the triple bundle technique and the “giftbox” technique. The weighted tensile strengths ranged from 81 to 453 N (mean 222.7 N) with the Triple Bundle technique in combination with # 2 Ethibond performing best with a mean of 453 N.
Conclusions
Due to the small sample sizes, different study designs, and heterogeneity of strength measurement techniques, definite recommendations on surgical technique cannot be made but presented information might help in the decision making process for foot and ankle surgeons.
Introduction
Approximately six out of 100,000 people, with middle-aged athletes as the most commonly affected, suffer from a rupture of their Achilles tendon per year [1, 2]. This leads to further socioeconomic problems in our present day population as we face increasing sporting demands in the elderly [1–4]. Every other distance runner suffers from an Achilles tendinopathy, and one in three sports-related injuries affect the Achilles tendon [5].
The treatment regimen of acute Achilles tendon ruptures has been intensively discussed with respect to conservative versus operative interventions [1, 6–9]. There is consensus that conservative treatment requires a prolonged episode of immobilization and is characterized by slow healing and a risk of re-tears as late as six months [10]. With respect to the high demands of the elderly and, since conservative treatment is long, arduous, and associated with re-rupture rates as high as 50–80 %, currently, Achilles tendon ruptures are dealt with surgical intervention in the active population [11]. The primary goal of surgical reconstruction and the crucial determinant of surgical success remains the initial strength and optimum length of the Achilles tendon repair.
Over 60 different surgical techniques with various suture combinations have been described so far [12], but surgeons still lack consensus on what technique and material performs best with respect to different initial pull-out strength.
Whilst limited in vivo data exists, various human cadaver studies have been performed to address this topic, and therefore the objective of this study was to systematically review, collect and compile data for human cadaver trials on the initial strength of Achilles tendon repair and perform a meta-analysis to address two questions: (1) Which kind of operative technique and (2) which kind of suture material and suture-knot combination provides evidence of best performance with respect to initial strength after surgical repair of acute Achilles tendon ruptures?
Methods
We performed a systematic search of the keywords “Achilles tendon AND (suture strength OR biomechanics) AND (cadaver NOT animal)” in the online databases PubMed, EMBASE, CINAHL, and the Cochrane Library repeatedly up to August 1, 2011 according to the PRISMA and QUOROM statement [13, 14]. All publication dates and languages were included.
We included studies that employed open, mini-open, or percutaneous Achilles tendon repair in human cadavers and assessed tensile strength as a primary outcome. Studies in animals, using experimental procedures, or assessing other outcomes than tensile strength were not eligible for inclusion.
All results from the online search were reviewed in duplicate and independently for eligibility. Extracted data from the included studies included sample size, biomechanical outcome and demographic data. For statistical analysis, biomechanical outcomes were synthesized as weighted mean tensile strength. Inverse variance was used as weight and 95 % confidence intervals were calculated for weighted mean tensile strength. Since all included data came from cadaver studies, difference in biological healing response based on age or gender can be ruled out as covariables. However, we included suture types as co-variates and formed subgroups accordingly.
All calculations were performed using intercooled STATA 12 (Stata Corp LP, College Station, TX).
Results
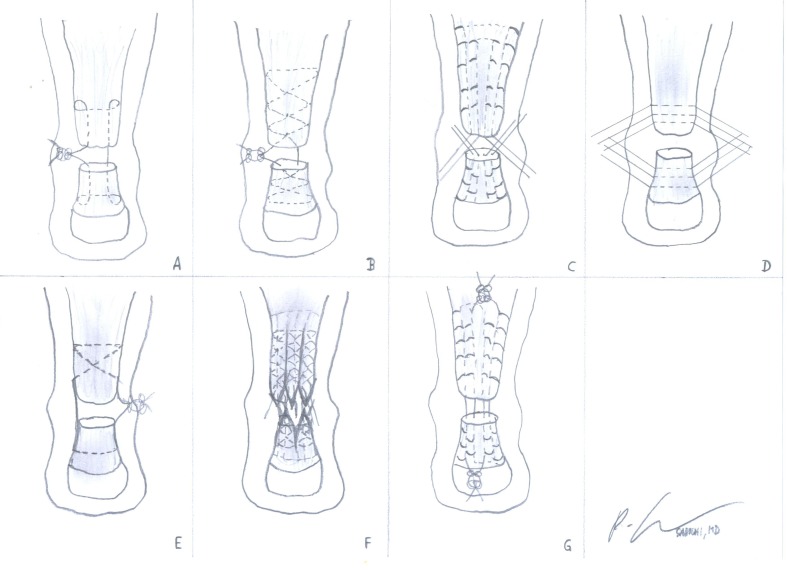
Our search produced 11 papers, published in English and German between 2000 and 2010 [15–25], that provided data for 23 treatment groups of 196 repairs in total. These studies report results for Kessler, Bunnell, and Krackow sutures in open repair, as well as the Achillon device, the Ma-Griffith repair technique, the triple bundle technique and the “giftbox” technique. These techniques are illustrated in Fig. 1.
Fig. 1.
Achilles tendon repair according to the open Kessler (a), the open Bunnell (b), the open Krackow (c), the percutaneous Achillon device (d), the percutaneous Ma-Griffith repair (e), the open triple bundle (f), and the open “giftbox” (g) technique are hereby illustrated
The mean study size was eight + three tendons per group, the mean age of the used cadavers was 65.2 years (range 15–95) with 61 % male and 39 % female. The mean weighted tensile strength of the different techniques ranged from 81 to 453 N (mean 222.7) with the Triple Bundle technique in combination with # 2 Ethibond revealing the highest value. Tables 1 and 2 summarize tensile strengths of seven different techniques using up to five different suture materials each.
Table 1.
Initial tensile strength after different suture techniques for Achilles tendon repair
| Type | Sample size | Strength (N) | 95 % confidence interval (CI) | |
|---|---|---|---|---|
| Lower | Upper | |||
| Bunnell | 37 | 217.2 | 214.3 | 220.1 |
| Kessler | 40 | 167.7 | 164.0 | 171.3 |
| Krackow | 67 | 172.7 | 171.0 | 174.4 |
| Achillon | 10 | 342.0 | 331.4 | 352.6 |
| Ma-Griffith | 13 | 149.5 | 145.3 | 153.8 |
| Giftbox | 13 | 168.0 | 160.1 | 175.9 |
| Triple Bundle | 8 | 453.0 | 445.8 | 460.2 |
Table 2.
Initial tensile strength after Achilles tendon repair with different techniques and suture materials
| Type | Suture | Sample size | Strength (N) | 95 % confidence interval (CI) | |
|---|---|---|---|---|---|
| Lower | Upper | ||||
| Bunnell | PDS-cord 0.7 | 22 | 264.8 | 260.5 | 269.0 |
| #1 PDS | 15 | 168.7 | 164.1 | 173.3 | |
| #2 Mersilene | 8 | 196.2 | 188.4 | 204.0 | |
| Kessler | PDS-cord 0.7 | 22 | 186.0 | 180.8 | 191.1 |
| #1 PDS | 10 | 137.0 | 130.3 | 143.7 | |
| #2 Mersilene | 8 | 166.9 | 158.6 | 175.2 | |
| Krackow | #1 Ethibond | 10 | 276.0 | 265.7 | 286.3 |
| #2 Ethibond | 30 | 181.0 | 179.0 | 183.1 | |
| #2 Hi Fi | 13 | 81.0 | 76.7 | 85.3 | |
| Fiberloop 2-0 | 6 | 282.0 | 272.5 | 291.5 | |
| #2 Mersilene | 8 | 199.0 | 193.8 | 204.2 | |
| Achillon | #1 Ethibond | 10 | 342.0 | 331.4 | 352.6 |
| Ma-Griffith | #2 Vicryl | 13 | 149.5 | 145.3 | 153.8 |
| Giftbox | #2 Hi Fi | 13 | 168.0 | 160.1 | 175.9 |
| Triple bundle | #2 Ethibond | 8 | 453.0 | 445.8 | 460.2 |
Cook et al. [15] presented a cadaveric study in 2010 on the strength of braided polyblend polyethylene sutures versus braided polyester sutures in Achilles tendon repair using a modified Krackow suture technique. Twelve Achilles tendon specimens were mounted to a materials testing machine and loaded to failure in anatomical direction. They found the smaller-caliber 2–0 FiberLoop significantly stronger than #2 Ethibond and concluded that there was no advantage on using traditional larger suture material for Achilles tendon repair.
Cretnik et al. [16] tested 36 cadaveric Achilles tendons using the Ma-Griffith technique and a new modified approach in a testing machine until failure. They found the new modified repair technique almost double the strength in comparison with the Ma-Griffith method and concluded that these results may be clinically relevant in terms of choice of percutaneous methods for Achilles tendon repair.
Gebauer et al. [17] tested the Bunnell and Kessler technique using different suture materials (PDS-thread or PDS-cord) or an additional plantaris tendon augmentation until failure. They found Bunell's technique to have a stronger primary suture stability compared to Kessler's technique and higher values using a PDC-cord. They concluded that Achilles tendon suture with a PDS-cord according to Bunnell's technique augmented with a plantaris longus tendon adds to an already mechanically strong method.
Herbort et al. [18] also tested the Bunnell and Kessler technique on fresh human cadaveric tendons using cyclic loading. They found no significant differences except at maximum loads but conclude that the typical failure mode of the Bunnell technique shows potential to optimize biomechanical behaviour when using stronger suture materials.
Huffard et al. [19] performed their testing on ten paired cadaveric Achilles tendon specimens using the Krackow technique on one specimen and a repair with the Achillon Suture System on the contralateral specimen with identical suture material. They found significantly higher values for the Achillon suture and concluded that Achillon repair is stronger in a cadaveric biomechanical study than the Krackow repair using identical sutures.
Jaakkola et al. [20] compared the Krakow locking loop technique with the triple bundle technique on eight pairs of fresh frozen cadaveric Achilles tendons. They used a servohydraulic testing machine until failure at a displacement of 2.54/sec. They found significant superiority of 2.8 to 1 in favour of the triple bundle technique for their conclusion.
Labib et al. [21] compared the conventional Krackow locking loop technique with the Giftbox technique where the knots of the suture are tied away from the rupture site on 13 pairs of fresh frozen cadaveric Achilles tendons until failure. They found the Giftbox technique twice as strong as those repaired using the traditional Krackow technique.
Lee et al. [22] transected 18 fresh-frozen cadaveric Achilles tendons and repaired them with a 4-strand Krackow core stitch, performed suture augmentation with three figure-of-eight stitches in six specimens and a running cross-stitch weave in six specimens. They found force to failure, stiffness and gapping resistance increased by suture augmentation and concluded that cross-stich augmentation of Achilles tendon repair yields a stronger and stiffer repair with greater resistance to gapping.
McCoy and Haddad [23] used 24 fresh-frozen human cadaver Achilles tendons to test maximum strength of the double Bunnell, double Kessler, and double Krackow technique using No. 2 polyester (Mersilene, Ethicon, Sommerville, NJ) nonabsorbable sutures in all repairs. They found no statistically significant difference between all three techniques and concluded that in a laboratory setting there actually was no significant difference in strength between the three suture techniques, when each was performed with a double suture weave.
Shepard et al. [24] tested five matched pairs of fresh frozen human Achilles tendons with and without the addition of an epitenon suture to the core repair suture using a No. 2 Ethibond Krakow locking loop core suture and a MTS testing machine (MTS Systems Corp., Eden Prairie, MN), which was loaded to failure in all cases. They found that an addition of epitenon sutures significantly increased the force necessary to produce a 2-mm gap as compared to core sutures alone.
Zandenbergen et al. [25] repaired artificially-created ruptures in 24 human cadaveric Achilles tendons using an open Bunnell repair, a percutaneous calcaneal tunnel or a percutaneous bone-anchor repair and tested using a machine until failure. They found suture breakage in non-anchor repairs, and anchor pullout in anchor repairs as common modes of failure, and that the average strength of the repairs varied from 166 N (SD 60) to 211 N (SD 30), with no differences between the techniques (p = 0.5). They concluded that taking costs into account, the percutaneous calcaneal tunnel technique and the open technique are the methods of choice.
Discussion
The objective of this study was to systematically review, collect and compile data for human cadaver trials on initial strength of Achilles tendon repair and to perform a meta-analysis to assess which knot and suture technique results in the strongest time zero repair. Additionally we wanted to include different types of sutures as covariates into our assessment. In this comparison and description of the strength of different sutures, we focussed on clinically meaningful outcomes, such as actual repair strength, rather than on statistical inference. Thus results are presented as confidence intervals, which reflect the range of potential outcomes, rather than as p-values from t-tests or ANOVA.
One of the most striking findings was that despite the considerable amount of Achilles tendon research, there is only very little specific data on the very basic determinant of repair effectiveness: knot and suture strength. Moreover, there are no systematic comparisons of the major techniques. Therefore, it was not possible to determine which technique performed “best” due to the heterogeneity of testing setups.
However, we found a wide range of weighted tensile strengths of the different techniques and systems from 81 to 453 N (mean 222.7 N) with the Triple Bundle technique in combination with # 2 Ethibond achieving the highest value of 453 N. For direct end-to-end repair we saw the highest tensile strength for the Bunnell technique, and somewhat lower values for Krackow and Kessler techniques, although the latter two produced widely equivalent results. The fairly high sample sizes for these three groups suggest robust data, but we still assessed subgroups by suture type. This subgroup analysis corroborated the earlier shown results, for example, for PDS which produced an almost 50 % stronger repair with Bunnell sutures. Interestingly, there were fewer differences with Mersilene. While we can only speculate on reasons for this difference and cannot deduce a “best suture”, our data do offer evidence for an interaction between type of suture and technique in Achilles tendon repair.
Limitations
There are potential shortcomings in our study. First, like any systematic review, our study’s validity depends on the quality of the primary studies that were included. For this particular study, the quality of the primary studies was in the mid to low range, but this finding is not unusual for surgical and musculoskeletal research.
Another shortcoming is heterogeneity among the primary studies, i.e. mathematical and methodological differences among the primary studies. The methodological differences, such as animal models, or the type and suture technique used were described in the text to allow readers to make their own judgment.
In addition, transection mechanisms of Achilles tendon injuries were performed in the animal models, which do not correspond to the appearance of a typical “horse tail” as it is present in real-life conditions. Therefore, the failure rate of sutures in the experimental setting is expected to be lower than in real life. Concerning the mathematical side of heterogeneity, which jeopardizes the validity the results of a meta-analysis, we used standardized mean differences to combine results. As mentioned above, this method uses mean differences divided by SDs, i.e. all results are given as “how many times SD” the result is away from no effect. This measure is also known as effect size.
Conclusion
Due to the small sample sizes, different study designs and heterogeneity of strength measurement techniques, a definite recommendation on an optimal surgical technique cannot be made. However, the authors present an overview of techniques and suture materials with respect to tensile strength, which might help in the decision-making process for foot and ankle surgeons.
References
- 1.Maffulli N. Rupture of the Achilles tendon. J Bone Joint Surg Am. 1999;81:1019–1036. doi: 10.2106/00004623-199907000-00017. [DOI] [PubMed] [Google Scholar]
- 2.Mafulli N, Waterson SW, Squair J, Reaper J, Douglas AS. Changing incidence of Achilles tendon rupture in Scotland: a 15-year study. Clin J Sport Med. 1999;9(3):157–160. doi: 10.1097/00042752-199907000-00007. [DOI] [PubMed] [Google Scholar]
- 3.Bhattacharyya M, Gerber B. Mini-invasive surgical repair of the Achilles tendon-does it reduce post-operative morbidity? Int Orthop. 2009;33(1):151–156. doi: 10.1007/s00264-008-0564-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Chiara Vuliani M, Guzzini M, Ferreti A. Operative treatment of chronic Achilles tendinopathy. Int Orthop. 2003;27(5):307–310. doi: 10.1007/s00264-003-0472-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Maffulli N. Rupture of the Achilles tendon. J. Bone Joint Surg Am. 1999;817:1019–1036. doi: 10.2106/00004623-199907000-00017. [DOI] [PubMed] [Google Scholar]
- 6.Assal M, Jung M, Stern R, et al. Limited open repair of Achilles tendon ruptures: a technique with a new instrument and findings of a prospective multicenter study. J Bone Joint Surg Am. 2002;84:161–170. [PubMed] [Google Scholar]
- 7.Buchgraber A, Pässler HH. Percutaneus repair of Achilles tendon rupture: immobilization versus functional postoperative treatment. Clin Orthop. 1997;341:113–122. [PubMed] [Google Scholar]
- 8.Cetti R, Christensen SE, Ejsted R, et al. Operative versus nonoperative treatment of Achilles tendon rupture. A prospective randomized study and review of the literature. Am J Sports Med. 1993;21:791–799. doi: 10.1177/036354659302100606. [DOI] [PubMed] [Google Scholar]
- 9.Möller M, Movin T, Granhed H, et al. Acute rupture of tendo Achillis. A prospective, randomized study of comparison between surgical and non-surgical treatment. J Bone Joint Surg Br. 2001;83:843–848. doi: 10.1302/0301-620X.83B6.11676. [DOI] [PubMed] [Google Scholar]
- 10.Kocher MS, Bishop J, Marshall R, Briggs KK, Hawkins RJ. Operative versus nonoperative management of acute Achilles tendon rupture: expected-value decision analysis. Am J Sports Med. 2002;306:783–790. doi: 10.1177/03635465020300060501. [DOI] [PubMed] [Google Scholar]
- 11.Wills C, Washburn S, Caiozzo V, Prietto CA. Achilles tendon rupture: a review of the literature comparing surgical versus nonsurgical treatment. Clin Orthop Relat Res. 1986;207:156–163. [PubMed] [Google Scholar]
- 12.Crolla RMPH, Leeuwen DM, Ramshorst B, et al. Acute rupture of the tendo calcaneus. Surgical repair with functional after treatment. Acta Orthop Belg. 1987;53:492–494. [PubMed] [Google Scholar]
- 13.Moher D, Liberati A, Tetzlaff J, Altman DG, Group P. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ. 2009;339:b2535. doi: 10.1136/bmj.b2535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Moher D, Cook DJ, Eastwood S, Olkin I, Rennie D, Stroup DF. Improving the quality of reports of meta-analyses of randomised controlled trials: the QUOROM statement. Quality of reporting of meta-analyses. Lancet. 1999; 354(9193):1896–900. doi: 10.1016/S0140-6736(99)04149-5. [DOI] [PubMed] [Google Scholar]
- 15.Cook KD, Clark G, Lui E, et al. Strength of braided polyblend polyethylene sutures versus braided polyester sutures in Achilles tendon repair: a cadaveric study. J Am Podiatr Med Assoc. 2010;100:185–188. doi: 10.7547/1000185. [DOI] [PubMed] [Google Scholar]
- 16.Cretnik A, Zlajpah L, Smrkolj V, Kosanovic M. The strength of percutaneous methods of repair of the Achilles tendon: a biomechanical study. Med Sci Sports Exerc. 2000;32:16–20. doi: 10.1097/00005768-200001000-00004. [DOI] [PubMed] [Google Scholar]
- 17.Gebauer M, Beil FT, Beckmann J, et al. Mechanical evaluation of different techniques for Achilles tendon repair. Arch Orthop Trauma Surg. 2007;127:795–799. doi: 10.1007/s00402-007-0325-8. [DOI] [PubMed] [Google Scholar]
- 18.Herbort M, Haber A, Zantop T, et al. Biomechanical comparison of the primary stability of suturing Achilles tendon rupture: a cadaver study of Bunnell and Kessler techniques under cyclic loading conditions. Arch Orthop Trauma Surg. 2008;128:1273–1277. doi: 10.1007/s00402-008-0602-1. [DOI] [PubMed] [Google Scholar]
- 19.Huffard B, O'Loughlin PF, Wright T, et al. Achilles tendon repair: Achillon system vs. Krackow suture: an anatomic in vitro biomechanical study. Clin Biomech (Bristol, Avon) 2008;23:1158–1164. doi: 10.1016/j.clinbiomech.2008.05.007. [DOI] [PubMed] [Google Scholar]
- 20.Jaakkola JI, Hutton WC, Beskin JL, Lee GP. Achilles tendon rupture repair: biomechanical comparison of the triple bundle technique versus the Krakow locking loop technique. Foot Ankle Int. 2000;21:14–17. doi: 10.1177/107110070002100103. [DOI] [PubMed] [Google Scholar]
- 21.Labib SA, Rolf R, Dacus R, Hutton WC. The "Giftbox" repair of the Achilles tendon: a modification of the Krackow technique. Foot Ankle Int. 2009;30:410–414. doi: 10.3113/FAI.2009.0410. [DOI] [PubMed] [Google Scholar]
- 22.Lee SJ, Goldsmith S, Nicholas SJ, et al. Optimizing Achilles tendon repair: effect of epitendinous suture augmentation on the strength of achilles tendon repairs. Foot Ankle Int. 2008;29:427–432. doi: 10.3113/FAI.2008.0427. [DOI] [PubMed] [Google Scholar]
- 23.McCoy BW, Haddad SL. The strength of Achilles tendon repair: a comparison of three suture techniques in human cadaver tendons. Foot Ankle Int. 2010;31:701–705. doi: 10.3113/FAI.2010.0701. [DOI] [PubMed] [Google Scholar]
- 24.Shepard ME, Lindsey DP, Chou LB. Biomechanical testing of epitenon suture strength in Achilles tendon repairs. Foot Ankle Int. 2007;28:1074–1077. doi: 10.3113/FAI.2007.1074. [DOI] [PubMed] [Google Scholar]
- 25.Zandbergen RA, Boer SF, Swierstra BA, et al. Surgical treatment of achilles tendon rupture: examination of strength of 3 types of suture techniques in a cadaver model. Acta Orthop. 2005;76:408–411. [PubMed] [Google Scholar]