Abstract
Purpose
The purpose of this study was to compare arthroscopic rotator cuff repair with single-row and double-row techniques because research has demonstrated the superiority of double-row repair from a biological and mechanical point of view but there is no evidence of clinical superiority.
Methods
A total of 160 patients with a full-thickness rotator cuff tear underwent arthroscopic repair with suture anchors. They were randomised into two groups of 80 patients according to the repair technique: single-row (group 1) and double-row (group 2). Results were evaluated by use of the University of California, Los Angeles (UCLA), American Shoulder and Elbow Surgeons (ASES) and Constant questionnaires, the Shoulder Strength Index (SSI) and range of motion. Follow-up time was two years. Magnetic resonance imaging (MRI) studies were performed on each shoulder preoperatively and two years after repair.
Results
One hundred per cent of the patients were followed up. All measurements showed significant improvement compared with the preoperative status. The UCLA score showed significant improvement in group 2. In over 30-mm tears UCLA and ASES showed significant differences. SSI showed significant improvement in group 2. Range of motion showed significant improvements in flexion and abduction in group 2. In under 30-mm tears group 2 showed also significant improvement in internal and external rotation. In MRI studies there were no significant differences.
Conclusions
At two years follow-up the double-row repair technique showed a significant difference in clinical outcome compared with single-row repair and this was even more significative in over 30-mm tears. No MRI differences were observed.
Introduction
Arthroscopic techniques and instrumentation are improving rapidly, and arthroscopic rotator cuff repair has gained popularity. Most studies have used a single row of anchors for attaching the rotator cuff tendon to bone when doing the repair with good results. However, the technique using a double row of anchors is reported to re-establish the normal rotator cuff footprint and increase the contact area for healing [8, 13, 23] making the anatomical and biomechanical outcomes are better than with the single-row technique [3, 6, 15, 18]. Although a few studies have compared single-row repair and double-row repair with regard to clinical aspects [5, 7, 17, 19, 21, 24], no articles have been published that support the superior clinical outcomes of double-row fixation over single-row fixation. This prospective randomised clinical trial was performed to address the question of whether a double-row rotator cuff anchor repair gives results superior to a single-row anchor repair in clinical outcome scores and in magnetic resonance imaging (MRI) evaluation.
Materials and methods
This study was approved by our Institutional Review Board, and all patients gave written informed consent to participate in the clinical trial.
Design and randomization
Patients were recruited among those referred by primary care doctors because of symptoms of rotator cuff tears and with an MR image of rotator cuff tear and were enrolled in the study by the three senior surgeons of the shoulder and elbow section at the University Hospital Miguel Servet in Zaragoza, Spain.
Recruitment started in September 2007 and was completed in September 2009. A total of 160 patients were eligible and randomised: 80 patients to single-row anchor repair and 80 patients to double-row anchor repair. All patients received the allocated treatment.
The 2-year results were available for all of them.
Patient selection
Inclusion criteria included the following: (1) rotator cuff tear, clinically confirmed, in a sane patient with complete passive range of motion (ROM) with inability to perform activities of daily living, (2) full-thickness tears bigger than ten millimetres with MRI evidence, (3) older than 18 and (4) informed consent.
Exclusion criteria included: (1) glenohumeral osteoarthritis, (2) ipsilateral shoulder pathology, (3) contralateral shoulder pathology, (4) rotator cuff tears bigger than 50 mm or retracted and insufficient mobile lesions to allow repair, (5) fatty degeneration grade 4 of Fuchs, (6) active use of steroids and (7) inability to complete questionnaires or the rehabilitation treatment.
Clinical evaluation
Evaluations were performed on all patients preoperatively and 2 years postoperatively. Data were collected to allow a determination of the University of California, Los Angeles (UCLA) score, Constant-Murley score and the shoulder index of the American Shoulder and Elbow Surgeons (ASES). ROM was evaluated in flexion, abduction, internal and external rotation. Muscle strength was tested using a spring-scale myometer (Manley 2012 spring scale, Manley Tool and Machine, Independence, MO, USA). We compared muscle strength using the Shoulder Strength Index (SSI). Instead of using the absolute value of the muscle strength, we used relative muscle strength of the affected shoulder compared with the muscle strength of the contralateral shoulder. To calculate the SSI, muscle strength of the affected shoulder is divided by the muscle strength of the contralateral shoulder.
Imaging
All scans were read by two specialists in musculoskeletal radiology. The size of the tear in the anteroposterior dimension and retraction of the tendon medially were recorded. Anteroposterior tear dimension was used to categorise tears into two groups: (1) ten to 30 mm and (2) 30–50 mm. Postoperative scans divided the rotator cuff into three groups: (1) full-thickness tear, (2) partial-thickness tear and (3) cuff integrity.
Randomization procedure
After a diagnostic arthroscopy to assess the status of the shoulder joint and the presence and size of the rotator cuff tear, we ascertained whether the tear was mobile evaluating the medial-to-lateral and anterior-to-posterior mobility of the tear margins with a soft tissue grasper. If this was verified, patients were randomised into one of two groups to receive either a single-row suture anchor repair technique (group 1) or a double-row suture anchor repair technique (group 2).
Randomization was performed with statistical software [Statistical Package for the Social Sciences (SPSS) version 11.0] through a random selection of 50 % of the cases. The randomisation list was kept by an independent researcher (not involved in the study), and the assignment code of each patient to one of the two groups was revealed to the surgeon at the time of surgery. All of the operations were performed in a standardised manner by three surgeons (I.C., A.M. and A.C.) using the same randomisation list.
In group 1 there were 35 men and 45 women. The mean age was 55.79 ± 6.3. The rotator cuff tear was small (ten to 30 mm) in 51 patients and large (30–50 mm) in 29 patients with a total mean size of 25.3 ± 8.3 mm. There were 46 crescent lesions, 15 L-shaped lesions, 11 inverted L-shaped lesions and 8 U-shaped lesions (Table 1).
Table 1.
Tear description
| Single row | Double row | P value | |
|---|---|---|---|
| Mean age (years) | 55.79 ± 6.3 | 55.21 ± 5.0 | 0.664 |
| Gender | |||
| Male | 35 | 33 | 0.749 |
| Female | 45 | 47 | |
| Shape of the tear | |||
| L-shaped | 15 | 14 | 0.819 |
| Inverted L-shaped | 11 | 10 | |
| U-shaped | 8 | 12 | |
| Crescent | 46 | 44 | |
| Mean area (mm2) | 25.3 ± 8.3 | 26.2 ± 7.4 | 0.465 |
| Coded area (mm2) | |||
| N (%) | |||
| 10–30 | 51 (49) | 53 (51) | 0.740 |
| 30–50 | 29 (51.8) | 27 (48.2) | |
In group 2 there were 33 men and 47 women. The mean age was 55.21 ± 5.0. The rotator cuff tear was small (ten to 30 mm) in 53 patients and large (30–50 mm) in 27 patients with a total mean size of 26.2 ± 7.4 mm. There were 44 crescent lesions, 14 L-shaped lesions, ten inverted L-shaped lesions and 12 U-shaped lesions (Table 1).
There were no statistically significant differences between group 1 and group 2 in these parameters.
Surgical technique
The three surgeons performed the same technique. Patients underwent brachial plexus block associated with general anaesthesia and were placed in a lateral decubitus position. The arm was suspended at approximately 30–45° of abduction and 20° of forward flexion. Distraction of the shoulder joint was accomplished with four kilograms of traction. To control bleeding we used radiofrequency, adrenalin admixture to the irrigation fluid and asked the anesthesiologist to lower the systolic blood pressure to 90 mm Hg if possible. We worked with an arthroscopic pump to maintain fluid pressure at 50 mmHg, increasing it temporally on demand up to 75 mmHg.
The arthroscope was inserted into the glenohumeral joint to evaluate the extent of the rotator cuff tear, any lesions of the biceps tendon and other associated lesions. The arthroscope was then redirected into the subacromial space. After complete bursectomy, arthroscopic subacromial decompression was performed to create a flat acromial undersurface in all patients. Osteophytes in the inferior part of the acromioclavicular joint were also removed, because not only an anterolateral subacromial spur but also medial subacromial spur and inferior clavicular spur were suspected as a cause of subacromial impingement. Tear size, pattern and mobility were evaluated. The edges of the tendon were debrided until strong healthy tissues were seen. For reattachment of the rotator cuff tendons, a cancellous bone bed was prepared in the footprint of the greater tuberosity with a bur until bleeding occurred. If mobility of a tendon was insufficient for repair, procedures to mobilise the tendon, such as release of the coracohumeral ligament and detachment of the rotator cuff from the bursal and articular sides, were performed.
The standard operating portals included the lateral portal for instrumentation, an accessory superior portal for anchor placement, and the previously established anterior and posterior portals. Frequently anterolateral and posterolateral portals were used.
The anchors used were Bio-Corkscrew double-loaded with No. 2 FiberWire sutures (Arthrex, Naples, FL, USA). These anchors were used by the three surgeons in both techniques.
For single-row repairs, anchors were placed along the lateral edge of the greater tuberosity within the footprint of the rotator cuff and spaced at five to ten millimetre increments. After placement of the anchors through the superior portal, sutures were individually passed from the double-loaded anchors into the lateral edge of the tendon, taking a ten to 15-mm bite of tissue using an antegrade suture passer or other instruments as deemed necessary to place a simple suture. When sutures had been placed, they were sequentially tied using a locking, sliding knot with backup half hitches (Figs. 1 and 2).
Fig. 1.
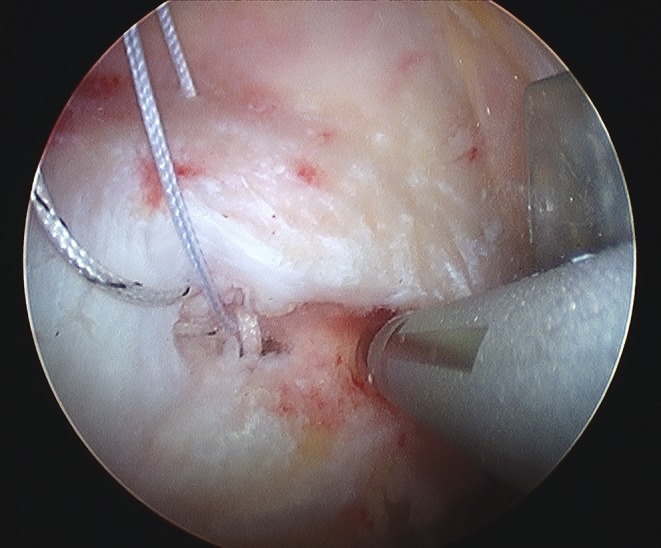
Single row: placement of anchors
Fig. 2.
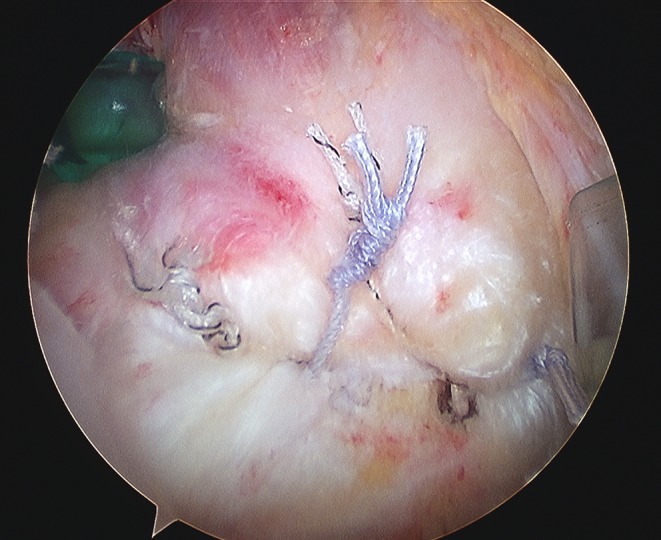
Single row: rotator cuff after arthroscopic repair
For double-row repairs, one row of anchors was placed in the medial aspect of the footprint, just lateral to the articular surface of the humeral head. Both sutures were passed through the tendon in a mattress fashion. A lateral row of anchors was then placed in the lateral aspect of the footprint, slightly proximal to the greater tuberosity. The lateral row sutures were passed in a simple suture fashion. Just one of the two sutures was passed through the tendon (Figs. 3 and 4).
Fig. 3.
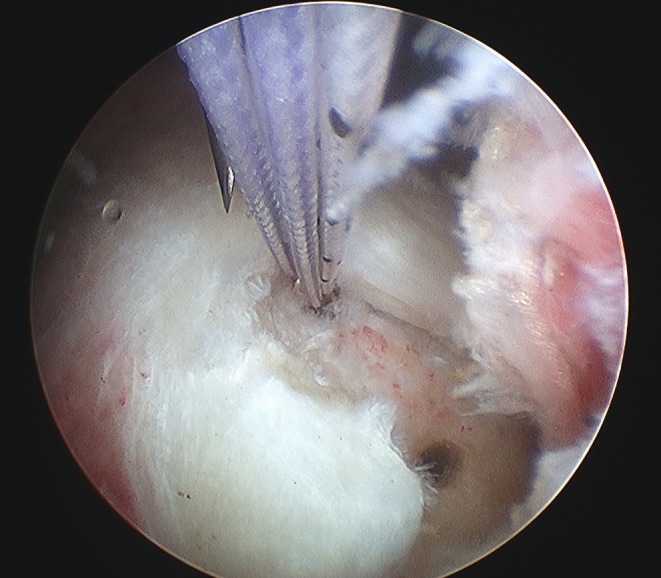
Double row: placement of anchors
Fig. 4.
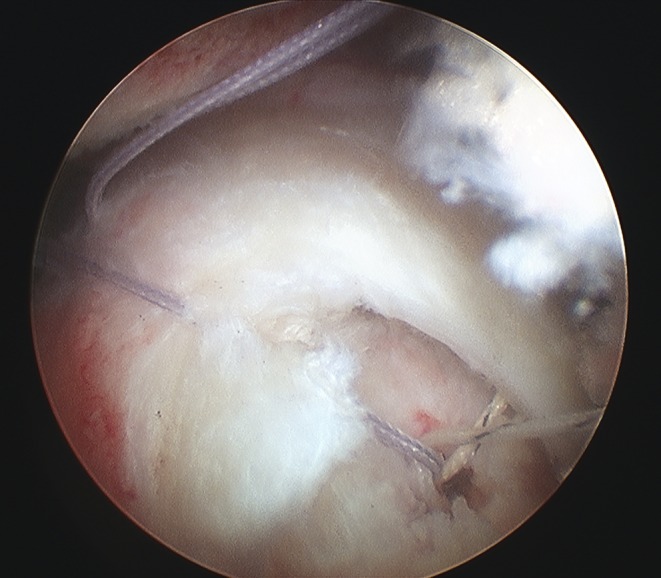
Surgical arthroscopic image
The L-shaped and U-shaped tears were first repaired with a side-to-side suture, providing margin convergence of the two edges of the cuff, before fixation of the cuff to the bone.
The number of anchors varied with the size of the tear and with the type of repair technique; we used 1.83 (range 1–3) anchors in group 1 and 2.99 anchors (range 2–4) in group 2.
Postoperative management
Postoperative management was the same for both groups. The arm was supported using an abduction sling. Under supervision, passive ROM was started in the first week. Active assisted ROM was typically started in a supine position starting at four to six weeks postoperatively, and full active ROM was commenced at six to eight weeks. Strengthening exercises were typically delayed for ten to 12 weeks.
Statistical methods
Student’s t test was used to compare the differences between preoperative UCLA score, Constant score, ASES index score, muscle strength and ROM in both groups.
The Mann–Whitney U test was used to compare the postoperative cuff integrity of the single-row and double-row groups. The significance level was set at P = 0.05.
All statistical analyses were performed by an independent statistician with the SPSS version 11.0.
Results
In the single-row and double-row groups, there was no significant difference in pre-surgical values in strength, ROM and scales (UCLA, ASES and Constant).
All measures at final follow-up in both groups showed a significant improvement compared with preoperative status.
The single-row and double-row groups showed no significant differences at final follow-up evaluation in ASES index (P = 0.269) and Constant score (P = 0.447), but the double-row group showed superior results compared with the single-row group in UCLA score (P < 0.023). When the analysis was limited to the group of ten to 30 mm, there were no significant differences in comparing both groups (Table 2). However, comparing single-row and double-row groups with over 30-mm tears, the double-row technique showed superior results compared with the single-row technique in UCLA score (P < 0.019) and in ASES index (P < 0.032) (Table 3).
Table 2.
Two-year results in 10–30 mm tears
| Mean ± SD | P | ||
|---|---|---|---|
| Single row | Double row | ||
| UCLA (0–35) | 28.9 ± 2.4 | 29.5 ± 1.6 | 0.359 |
| Constant (0–100) | 79.8 ± 6.6 | 79.7 ± 3.2 | 0.875 |
| ASES (0–100) | 84.6 ± 6.1 | 85.2 ± 3.2 | 0.940 |
| External rotation, ° | 59.0 ± 6.7 | 58.6 ± 4.0 | 0.774 |
| Internal rotation, ° | 55.7 ± 6.6 | 55.8 ± 4.3 | 0.722 |
| Flexion, ° | 153.9 ± 10.2 | 159.2 ± 6.8 | 0.003 |
| Abduction, ° | 154.3 ± 10.0 | 159.3 ± 6.8 | 0.007 |
| Flexion SSI | 0.75 ± 0.06 | 0.78 ± 0.04 | 0.027 |
| Abduction SSI | 0.76 ± 0.06 | 0.78 ± 0.04 | 0.358 |
| Internal rotation SSI | 0.79 ± 0.05 | 0.81 ± 0.04 | 0.009 |
| External rotation SSI | 0.80 ± 0.05 | 0.81 ± 0.03 | <0.001 |
Mann–Whitney U test
Table 3.
Two-year results in 30–50 mm tears
| Single row | Double row | P | |
|---|---|---|---|
| UCLA (0–35) | 27.1 ± 1.9 | 28.2 ± 1.4a | 0.019 |
| Constant (0–100) | 75.2 ± 7.0 | 77.0 ± 2.4b | 0.137 |
| ASES (0–100) | 80.3 ± 6.2 | 83.2 ± 3.1a | 0.032 |
| External rotation, ° | 54.2 ± 6.6 | 56.3 ± 3.8b | 0.002 |
| Internal rotation, ° | 51.0 ± 5.5 | 52.9 ± 3.7b | 0.007 |
| Flexion, ° | 145.8 ± 9.8 | 153.1 ± 7.0a | 0.002 |
| Abduction, ° | 146.3 ± 9.7 | 153.1 ± 7.0a | 0.004 |
| Flexion SSI | 0.70 ± 0.05 | 0.74 ± 0.03a | 0.002 |
| Abduction SSI | 0.72 ± 0.05 | 0.74 ± 0.03b | 0.100 |
| Internal rotation SSI | 0.76 ± 0.04 | 0.78 ± 0.02a | 0.026 |
| External rotation SSI | 0.76 ± 0.05 | 0.78 ± 0.02b | 0.091 |
aStudent’s t test
bMann–Whitney U test
Comparing the ROM, there were significant differences in flexion (153.9 ± 10.2° in group 1 and 159.2 ± 6.8° in group 2; P < 0.003) and abduction (154.3 ± 10° in group 1 and 159.3 ± 6.3° in group 2; P < 0.007). However, when comparing over 30-mm tears, the double-row technique showed superior results compared with the single-row technique in flexion (P < 0.002), abduction (P < 0.004), internal rotation (P < 0.007) and external rotation (P < 0.002) (Table 3).
The differences in SSI were significant comparing the single-row group and double-row group showing superior results in the double-row group in flexion (P < 0.001), abduction (P < 0.002), internal rotation (P < 0.01) and external rotation (P < 0.04). Results in ten to 30-mm tears (Table 2) and in over 30-mm tears (Table 3) were similar.
MRI studies at final follow-up showed an intact rotator cuff in 137 patients, partial-thickness defects in 15 patients and full-thickness defects in eight patients. There were no significant differences in rates of healing between group 1 and group 2 patients when assessed by MRI studies (P > 0.05) (Table 4).
Table 4.
Imaging
| MRI | Intact | Partial-thickness defect | Full-thickness defect |
|---|---|---|---|
| Single row | 65 | 10 | 5 |
| Double row | 72 | 5 | 3 |
| Total | 137 | 15 | 8 |
Discussion
Recent arthroscopic repair techniques for rotator cuff tears have emphasised the potential for a double-row repair to add strength to the repair and hopefully decrease the anatomical failure rate [1, 11, 13, 14, 24, 25]. Several studies have indicated that results in cases of anatomical failure, although clinically improved, are not as good as those that are anatomically intact, especially if strength measurements are made [1, 2]. Therefore, trying to achieve and maintain an intact cuff is a paramount goal in cuff repair. Biomechanical studies have emphasised the potential improvement of outcomes by the double-row repair technique [12, 16, 23]. However, clinical studies have not yet validated this idea [7, 17, 21, 22].
Franceschi et al. [7] completed a randomised controlled trial providing Level I evidence comparing the single-row repair technique and the double-row repair technique. Sixty patients were evaluated. Patients were reassessed at two years of intervention by their functional status with the UCLA scale and follow-up imaging by MRI. There were no significant differences in functional assessment, postoperative ROM and pattern of healing with MRI. Burks et al. [4] conducted a prospective randomised study comparing repair with the single-row and double-row techniques, including 40 patients in each group. For the functional outcome they used the UCLA, ASES, Constant, Western Ontario Rotator Cuff Index (WORC) and Single Assessment Numeric Evaluation (SANE) scales, and for the imaging outcome three postoperative MRI studies. The follow-up was 12 months. The postoperative MRI showed no difference in the insertion area, the tendon thickness or its signal. Postoperative strength and mobility were also similar. The authors concluded that there were no significant differences between the two techniques. In a recent study yielding Level I evidence, Grasso et al. [10] studied 80 patients. At the two year follow-up no significant differences were found in the Disabilities of the Arm, Shoulder and Hand (DASH) scale, Work-DASH, Constant and the measurement of muscle strength.
Charousset et al. [5] conducted a non-randomised comparative study including 31 patients in the double-row group and 35 in the single-row group. No significant differences were found regarding clinical outcomes measured by the Constant scale with a follow-up of approximately 28 months. Although no differences were found with computed tomographic arthrography whether the repair was partial or complete, a significantly higher rate for return of the tendon to its anatomical position was found with the double-row technique. Park et al. [19] conducted a study in which 40 consecutive patients were treated with the single-row technique and the following 38 with the double-row technique. At two years after surgery, no significant improvements were found in the two groups in ASES, Constant and SSI. When a comparison was made regarding the size of the rupture, functional assessment was significantly better with the double-row in large and massive tears (>3 cm) (P < 0.05). A new evaluation method, the SSI, only used in the Park et al. article [19], was introduced to reflect patients’ subjective judgement about the operation as well as their rehabilitation status. Because patients will always compare the operated shoulder with the unaffected shoulder, the only standard function of the shoulder will be that of the unaffected shoulder. Using the SSI, clinicians can more easily explain the goals of surgery and rehabilitation to the patient.
The number of anchors used for surgical repair depends on the size and shape of the lesion, as well as technique. In our study the number of anchors used was 1.83 in the single-row technique (1–3) and 2.99 in the double-row (2–4). An important fact is that most biomechanical laboratory studies compared the double-row technique with the single-row technique used twice in the double-row technique [12, 16, 23]. However, the number of anchors in recent clinical studies is not as high as in the laboratory [1, 7, 11, 25]. In fact, Franceschi et al. [7] used a mean of 1.9 and 2.3 anchors, respectively, and Burks et al. [4] 2.25 and 3.2. It may be that it is more difficult to place the anchors in vivo than in the laboratory and this may explain why fewer anchors are placed in clinical studies. Or maybe these extra anchors implanted in the laboratory are not required [18, 20].
In our study, the failure rate on MRI is 14.4 %, representing a total of 23 patients (eight with a full-thickness tear and 15 with a partial-thickness tear). It should be noted that functional and clinical outcomes in patients with a partial-thickness tear on MRI control are similar to those without a tear on MRI, whereas in patients with a full-thickness tear there does appear to be a greater clinical and functional impact.
The failure rate in other studies similar to ours is around 15 % in most [4, 10, 19, 24]. Follow-up time is also an important aspect for evaluation of these results, but it is a fact about which there is no clear consensus. Some studies say that the failures appear late in large and massive tears [8], while in the open repair technique, improvements appear over time. In other studies, these failures appear in very early stages after repair [9], while others appear in later stages of evolution [4]. In our study we followed up for 24 months because we have observed that it is long enough to assess the functional recovery of the shoulder and problems with the surgery appear early after surgery.
The strength of our study includes the fact that we had 100 % follow-up in a randomised study. Three different shoulder scoring systems were used to evaluate the groups. The study included 160 patients, which is the highest number of patients included in this kind of study as far as we know. In addition, we also used a new method to evaluate the strength that is more objective than previous methods.
A limitation of this study is that we only did one MRI after surgery, but because of the high demand for this imaging study in our hospital, it was not possible to do one every three or six months, which should be a more complete study. Perhaps the follow-up time is long, but as explained previously we decided on two years of follow-up time.
Conclusions
This prospective randomized evaluation of single-row compared with double-row rotator cuff fixation shows a significant improvement with the double-row technique in clinical evaluation. In over 30-mm tears the improvement appears in more measurements than in ten to 30-mm tears, but the MRI results did not reveal a significant difference between the single- and double-row groups.
Footnotes
Level of evidence: Level I.
References
- 1.Anderson K, Boothby M, Aschenbrener D, Holsbeeck M. Outcome and structural integrity after arthroscopic rotator cuff repair using 2 rows of fixation: minimum 2-year follow-up. Am J Sports Med. 2006;34:1899–1905. doi: 10.1177/0363546506290187. [DOI] [PubMed] [Google Scholar]
- 2.Boileau P, Brassart N, Watkinson DJ, Carles M, Hatzidakis AM, Krishnan SG. Arthroscopic repair of full-thickness tears of the supraspinatus: does the tendon really heal? J Bone Joint Surg Am. 2005;87(6):1229–1240. doi: 10.2106/JBJS.D.02035. [DOI] [PubMed] [Google Scholar]
- 3.Brady PC, Arrioni P, Burkhart SS. Evaluation of residual rotator cuff defects after in vivo single- versus double-row rotator cuff repairs. Arthroscopy. 2006;22:1070–1075. doi: 10.1016/j.arthro.2006.05.007. [DOI] [PubMed] [Google Scholar]
- 4.Burks RT, Crim J, Brown N, Fink B, Greis PE. A prospective randomized clinical trial comparing arthroscopic single- and double-row rotator cuff repair: magnetic resonance imaging and early clinical evaluation. Am J Sports Med. 2009;37:674–682. doi: 10.1177/0363546508328115. [DOI] [PubMed] [Google Scholar]
- 5.Charousset C, Grimberg J, Duranthon LD, Bellaiche L, Petrover D. Can a double-row anchorage technique improve tendon healing in arthroscopic rotator cuff repair? A prospective, nonrandomized, comparative study of double-row and single-row anchorage techniques with computed tomographic arthrography tendon healing assessment. Am J Sports Med. 2007;35:1247–1253. doi: 10.1177/0363546507301661. [DOI] [PubMed] [Google Scholar]
- 6.Curtis AS, Burbank KM, Tierney JJ, Scheller AD, Curran AR. The insertional footprint of the rotator cuff: an anatomic study. Arthroscopy. 2006;22(6):609.e1. doi: 10.1016/j.arthro.2006.04.001. [DOI] [PubMed] [Google Scholar]
- 7.Franceschi F, Ruzzini L, Longo UG, Martina FM, Zobel BB, Maffulli N, Denaro V. Equivalent clinical results of arthroscopic single-row and double-row suture anchor repair for rotator cuff tears: a randomized controlled trial. Am J Sports Med. 2007;35(8):1254–1260. doi: 10.1177/0363546507302218. [DOI] [PubMed] [Google Scholar]
- 8.Galatz LM, Ball CM, Teefey SA, Middleton WD, Yamaguchi K. The outcome and repair integrity of completely arthroscopically repaired large and massive rotator cuff tears. J Bone Joint Surg Am. 2004;86:219–224. doi: 10.2106/00004623-200402000-00002. [DOI] [PubMed] [Google Scholar]
- 9.Gerber C, Fuchs B, Hodler J. The results of repair of massive tears of the rotator cuff. J Bone Joint Surg Am. 2000;82(4):505–515. doi: 10.2106/00004623-200004000-00006. [DOI] [PubMed] [Google Scholar]
- 10.Grasso A, Milano G, Salvatore M, Falcone G, Deriu L, Fabbriciani C. Single-row versus double-row arthroscopic rotator cuff repair: a prospective randomized clinical study. Arthroscopy. 2009;25(1):4–12. doi: 10.1016/j.arthro.2008.09.018. [DOI] [PubMed] [Google Scholar]
- 11.Huijsmans PE, Pritchard MP, Berghs BM, Rooyen KS, Wallace AL, Beer JF. Arthroscopic rotator cuff repair with double-row fixation. J Bone Joint Surg Am. 2007;89(6):1248–1257. doi: 10.2106/JBJS.E.00743. [DOI] [PubMed] [Google Scholar]
- 12.Kim DH, ElAttrache NS, Tibone JE, et al. Biomechanical comparison of a single-row versus double-row suture anchor technique for rotator cuff repair. Am J Sports Med. 2006;34(3):407–414. doi: 10.1177/0363546505281238. [DOI] [PubMed] [Google Scholar]
- 13.Koh K, Kang KC, Lim TK, Shon MS, Yoo JC. Prospective randomized clinical trial of single- versus double-row suture anchor repair in 2- to 4-cm rotator cuff tears: clinical and magnetic resonance imaging results. Arthroscopy. 2011;27(4):453–462. doi: 10.1016/j.arthro.2010.11.059. [DOI] [PubMed] [Google Scholar]
- 14.Lafosse L, Brozska R, Toussaint B, Gobezie R. The outcome and structural integrity of arthroscopic rotator cuff repair with use of the double-row suture anchor technique. J Bone Joint Surg Am. 2007;89:1533–1541. doi: 10.2106/JBJS.F.00305. [DOI] [PubMed] [Google Scholar]
- 15.Lo IK, Burkhart SS. Double-row arthroscopic rotator cuff repair: re-establishing the footprint of the rotator cuff. Arthroscopy. 2003;19:1035–1042. doi: 10.1016/j.arthro.2003.09.036. [DOI] [PubMed] [Google Scholar]
- 16.Meier SW, Meier JD. The effect of double-row fixation on initial repair strength in rotator cuff repair: a biomechanical study. Arthroscopy. 2006;22(11):1168–1173. doi: 10.1016/j.arthro.2006.07.004. [DOI] [PubMed] [Google Scholar]
- 17.Papalia R, Franceschi F, Buono A, Zampogna B, Malffulli N, Denaro V. Double row repair: is it worth the hassle? Sports Med Arthrosc. 2011;19(4):342–347. doi: 10.1097/JSA.0b013e3182394215. [DOI] [PubMed] [Google Scholar]
- 18.Park MC, ElAttrache NS, Tibone JE, Ahmad CS, Jun BJ, Lee TQ. Part I: footprint contact characteristics for a transosseous-equivalent rotator cuff repair technique compared with a double-row repair technique. J Shoulder Elbow Surg. 2007;16:461–468. doi: 10.1016/j.jse.2006.09.010. [DOI] [PubMed] [Google Scholar]
- 19.Park JY, Lhee SH, Choi JH, Park HK, Yu JW, Seo JB. Comparison of the clinical outcomes of single- and double-row repairs in rotator cuff tears. Am J Sports Med. 2008;36:1310–1316. doi: 10.1177/0363546508315039. [DOI] [PubMed] [Google Scholar]
- 20.Park MC, Tibone JE, ElAttrache NS, Ahmad CS, Jun BJ, Lee TQ. Part II: biomechanical assessment for a footprint-restoring transosseous-equivalent rotator cuff repair technique compared with double-row repair technique. J Shoulder Elbow Surg. 2007;16(4):469–476. doi: 10.1016/j.jse.2006.09.011. [DOI] [PubMed] [Google Scholar]
- 21.Pennington WT, Gibbons DJ, Bartz BA, Dodd M, Daun J, Klinger J, Popovich M, Butler B. Comparative analysis of single-row versus double-row repair of rotator cuff tears. Arthroscopy. 2010;26(11):1419–1426. doi: 10.1016/j.arthro.2010.03.013. [DOI] [PubMed] [Google Scholar]
- 22.Reardon DJ, Maffulli N. Clinical evidence shows no difference between single- and double-row repair for rotator cuff tears. Arthroscopy. 2007;23(6):670–673. doi: 10.1016/j.arthro.2007.01.031. [DOI] [PubMed] [Google Scholar]
- 23.Smith CD, Alexander S, Hill AM, et al. A biomechanical comparison of single and double-row fixation in arthroscopic rotator cuff repair. J Bone Joint Surg Am. 2006;88(11):2425–2431. doi: 10.2106/JBJS.E.00697. [DOI] [PubMed] [Google Scholar]
- 24.Sugaya H, Maeda K, Matsuki K, Moriishi J. Repair integrity and functional outcome after arthroscopic double-row rotator cuff repair: a prospective outcome study. J Bone Joint Surg Am. 2007;89:953–960. doi: 10.2106/JBJS.F.00512. [DOI] [PubMed] [Google Scholar]
- 25.Sugaya H, Maeda K, Matsuki K, Moriishi J. Functional and structural outcome after arthroscopic full-thickness rotator cuff repair: single-row versus dual-row fixation. Arthroscopy. 2005;21(11):1307–1316. doi: 10.1016/j.arthro.2005.08.011. [DOI] [PubMed] [Google Scholar]


