Abstract
Purpose
Selection of the correct femoral stem size is crucial in total hip arthroplasty for an uncomplicated implantation and good initial stability. Pre-operative templating has been shown to be a valuable tool in predicting the correct implant size. For short-stem total hip arthroplasty (SHA), which recently is increasingly used, it is unknown if templating can be performed as reliable as conventional total hip arthroplasty (THA).
Methods
A total of 100 hip arthroplasties, 50 with SHA and 50 with THA, were templated by four orthopaedic surgeons each. The surgeons had different levels of professional experience and performed a digital template of the acetabular and femoral component on the pre-operative radiographs. The results were compared with the truly inserted implant size.
Results
For the femoral stems the average percentage of agreement (±1 size) was 89.0 % in SHA and 88.5 % in THA. There was no significant difference among surgeons in the accuracy of templating the correct stem size and no significant difference between templating SHA and THA. For the acetabular component the average percentage of agreement (±1 size) was 75.8 %. However, the more experienced surgeons showed a significant higher accuracy for templating the correct cup size than the less experienced surgeons.
Conclusion
Digital templating of SHA can predict the stem sizes as accurately as conventional THA. Therefore digital templating is also recommendable for SHA, as it helps to predict the implant size prior to surgery and thereby might help to avoid complications.
Introduction
Pre-operative templating is considered an important step prior to hip arthroplasty in order to anticipate problems and prevent complications [1]. It also helps to identify the optimal sizes of the components and thereby avoid limb discrepancies, insufficient offset reconstructions, femoral fractures and implant failures due to a lack of stability [2–6]. Templating on radiographs has shown to be a reliable and accurate way to determine the size of the components prior total hip arthroplasty (THA) [5, 7–12]. For short-stem total hip arthroplasty (SHA), which was introduced several years ago [13] and recently is increasingly used, only little is known about the accuracy of pre-operative templating [10].
This appears important, as the design and anchorage of most short-stem total hip implants are different compared to conventional total hip implants [13]. This applies particularly to the wedged and doubled-tapered SHA designs which are metaphyseal anchored by multiple-point contact [13]. Furthermore, the position of those short-stem implants is more variable and also depends on the femoral resection level and the anatomy of the femoral neck [14]. Undersizing of short stems might lead to an early stem migration with a higher rate of failure, whereas oversizing of the implants might lead to a higher femoral fracture rate.
For those reasons this study assessed: (1) how accurately digital templating can be performed for a metaphyseally anchored SHA implant, (2) if it is as accurate as for a conventional THA implant and (3) if the accuracy of templating is dependent on the professional experience of the surgeon. The main hypothesis of this study was that templating of SHA is not significantly different compared to THA.
Materials and methods
Study design
Digital templating was performed retrospectively for a total of 100 hips, with 50 accounting for SHA and 50 accounting for conventional THA. Pairs of pre-operative and postoperative radiographs were consecutively selected from the digital files of our orthopaedic department and were acquired between January 2009 and August 2011. Inclusion criteria were primary hip replacement, a pre-operative pelvic-overview with a calibration object and a postoperative radiograph showing components which were adequate in size and position. Only one type of implant was included for the SHA and THA group respectively. Exclusion criteria were severe dysplasia (Crowe II–IV) or a missing calibration object. The study was approved by the ethics committee of the University.
All pelvic-overviews were taken as an antero-posterior image (film-focus distance 110 cm), centred on the pubis and taken in the supine position with both legs in 10–15° of internal rotation. As a calibration object, either a metallic ball of 10-mm diameter which was positioned between the legs of the patient at the anteroposterior level of the great trochanter or, if available, the implant head of a contralateral hip arthroplasty was used.
Templating was performed by four orthopaedic surgeons from one academic medical centre with different levels of professional experience: attending physician (AF), fifth year resident (R-5) (AS), third year resident (R-3) (FS) and first year resident (R-1) (LWJ). Each of the observers performed a template on the pre-operative digital radiograph for the acetabular and femoral component. The planning was done in a blinded fashion and random order, at a minimum of two months after surgery. Templating was performed with a digital radiograph planning software (EndoMap, Siemens, Nürnberg, Germany), which is routinely used in our clinic and all surgeons are trained in using this software. Radiographs are first calibrated with the help of the calibration object and then digital templating was performed for the acetabular and femoral component according to the protocol for digital templating in THA as described by Bono [15].
Implants and patients
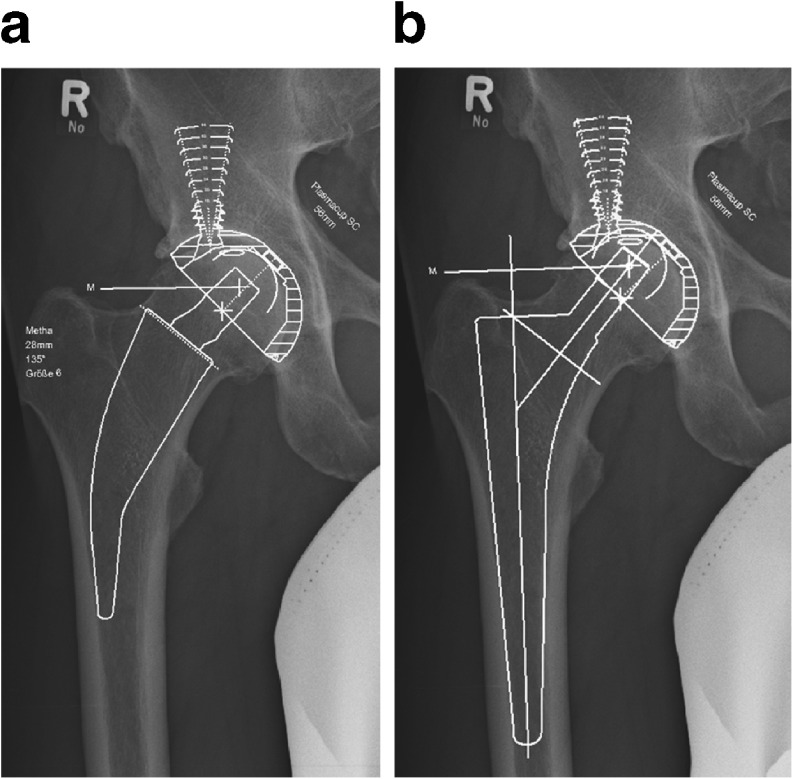
Short-stem hip implant
Patients with SHA all received the same double-tapered short-stem (Metha, Aesculap, Tuttlingen, Germany) (Fig. 1a). The implant sizes range from 0 to 7 and are available with a monoblock (CCD-angle 120°,130°, 135°) or as a modular implant with cone adapters (CCD-angle 130°, 135°, 140° with 7.5° ante-, retro-version and neutral). In this study, only implants with a neutral neck were templated. The median stem size used in SHA was 3.0 ± 1.4 (range 0–6). From the 50 SHAs, 60 % (n = 30) were from males and 40 % (n = 20) were from females, which had a mean age of 55.1 ± 11.6 years (range 24–71) at the time of implantation. The right hip was involved in 54 % (n = 27) and the left hip was involved in 46 % (n = 23) of the cases. Reasons for SHA were osteoarthritis in 80 % (n = 40), avascular necrosis in 16 % (n = 8) and acetabular dysplasia in 4 % (n = 2).
Fig. 1.
Digital template of short-stem hip arthroplasty (SHA) (a) and conventional total hip arthroplasty (THA) (b)
Conventional hip implant
Patients with THA all received the same conventional stem (CR-Stem, Implantcast, Buxtehude, Germany) (Fig. 1b). The implant sizes range from 1 to 7 and have a CCD-angle of 140°. The median stem size used in THA was 4.0 ± 1.6 (range 1–7). From the 50 THAs, 52 % (n = 26) were from males and 48 % (n = 24) were from females, which had a mean age of 65.0 ± 6.0 years (range 24–71) at the time of implantation. The right hip was involved in 50 % (n = 25) and the left hip was involved in 50 % (n = 25) of the cases. Reasons for THA were osteoarthritis in 88 % (n = 44), avascular necrosis in 4 % (n = 2) and acetabular dysplasia in 8 % (n = 4).
Acetabular component
In both groups, either a threaded 88 % (n = 88) or a press-fit 12 % (n = 12) acetabular cup (Screwcup or Plasmacup, both Aesculap, Tuttlingen, Germany) were used and templated according to the truly implanted cup. Both cups are available in 2-mm increments, with sizes ranging from 44 to 64 mm and can be used with a polyethylene or a ceramic liner. In all patients a ceramic femoral head was used which is available in the sizes small, medium, large and extra-large with 4-mm increments respectively. The median cup size used in SHA was 52 ± 3.9 (range 44–62) and the median cup size used in THA was 52 ± 3.1 (range 44–56).
Statistics
The accuracy of templating was reported as a percent agreement between the implanted size and the templated size for each component and surgeon. Interpretation of inter-observer agreement was performed by weighted kappa (κ) analysis for the acetabular and femoral component. Inter-observer comparison included: (1) the two more experienced surgeons, attending vs. R-5; (2) the two less experienced surgeons, R-3 vs. R-1; (3) the more experienced surgeons (attending/R-5) vs. the less experienced surgeons (R-3/R-1). There were two possible combinations for the latter: attending/R-5 vs. R-3/R-1 and attending/R-5 vs. R-1/R-3. According to the guideline by Landis and Koch, the strength of agreement for κ values was considered as "slight" between 0.00 and 0.20, as "fair" between 0.21 and 0.40, as "moderate" between 0.41 and 0.60, as "substantial" between 0.61 and 0.80 and as "almost perfect" between 0.81 and 1.00 [16]. Chi-square analysis was performed to evaluate the effect of experience (attending/R-5 vs. R-3/R-1) and the comparison between SHA and THA on the accuracy of templating. A p < 0.05 was considered to be significant.
Results
Femoral stem
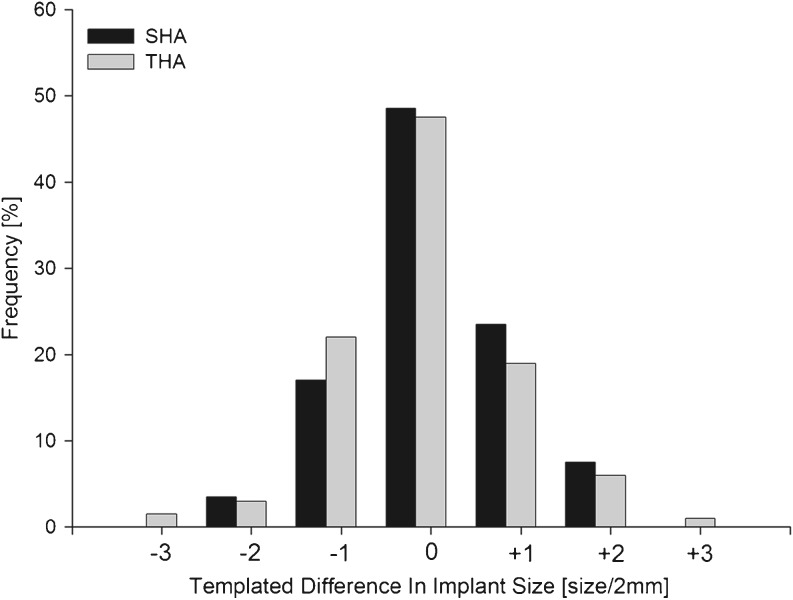
Short-stem total hip arthroplasty
Among all observers, the pre-operative template accurately (±0) predicted SHA stem size in 48.5 % (n = 97/200) of attempts. In 89.0 % (n = 178/200) the stem was predicted within one size difference (±1), 100 % (n = 200/200) were within two size difference (±2) and 0.0 % (n = 0/200) were more than two sizes different (> ±2) (Fig. 2, Table 1). Inaccurately planned sizes were larger in 31.0 % (n = 62/200) and smaller in 20.5 % (n = 41/200) (Table 1).
Fig. 2.
Differences between templated and truly implanted stems in SHA (Metha-stem) and THA (CR-stem). Positive values indicate templating of a larger component and negative values indicate templating of a smaller component
Table 1.
Accuracy of component templating for the different surgeons [%]
| Surgeons | SHA ± 0 | SHA ± 1 | THA ± 0 | THA ± 1 | Cup ± 0 | Cup ± 1 |
|---|---|---|---|---|---|---|
| Total | 48.5 | 89.0 | 47.5 | 88.5 | 34.8 | 75.8 |
| Attending | 48.0 | 82.0 | 52.0 | 92.0 | 44.0 | 78.0 |
| R-5 | 50.0 | 94.0 | 54.0 | 94.0 | 40.0 | 81.0 |
| R-3 | 48.0 | 94.0 | 48.0 | 90.0 | 32.0 | 82.0 |
| R-1 | 48.0 | 86.0 | 36.0 | 78.0 | 23.0 | 62.0 |
R- year of residency, SHA short-stem total hip arthroplasty,THA conventional total hip arthroplasty
Inter-observer agreement for SHA was substantial between the more experienced surgeons (kappa 0.67), moderate between the less experience surgeons (kappa 0.57) and moderate between more and less experienced surgeons (kappa 0.57 and 0.53). Templating of SHA was not significantly different (p = 0.89) between the more and the less experienced surgeons.
Conventional total hip arthroplasty
Among all observers, pre-operative template accurately (±0) predicted conventional THA stem size in 47.5 % (n = 95/200) of attempts. In 88.5 % (n = 177/200) the stem was predicted within one size difference (±1), 97.5 % (n = 195/200) were within two sizes different (±2) and 2.5 % (n = 5/200) were more than two sizes different (> ±2) (Fig. 2, Table 1). Inaccurately planned sizes were larger in 26 % (n = 52/200) and smaller in 26.5 % (n = 53/200).
Inter-observer agreement for conventional THA was substantial between the more experienced surgeons (kappa 0.79), moderate between the less experienced surgeons (kappa 0.58) and moderate to substantial between more and less experienced surgeons (kappa 0.59 and 0.63). Templating of SHA between the more and the less experienced surgeons was not significantly different (p = 0.09).
Comparison of short-stem and conventional total hip arthroplasty
No significant difference was observed in the accuracy of digital templating between SHA and THA for all observers (p = 0.76). Similarly, no significance was observed between templating SHA and THA for the attending (p = 0.69), the R-5 (p = 0.69), the R-3 (p = 1.00) and the R-1 (p = 0.15).
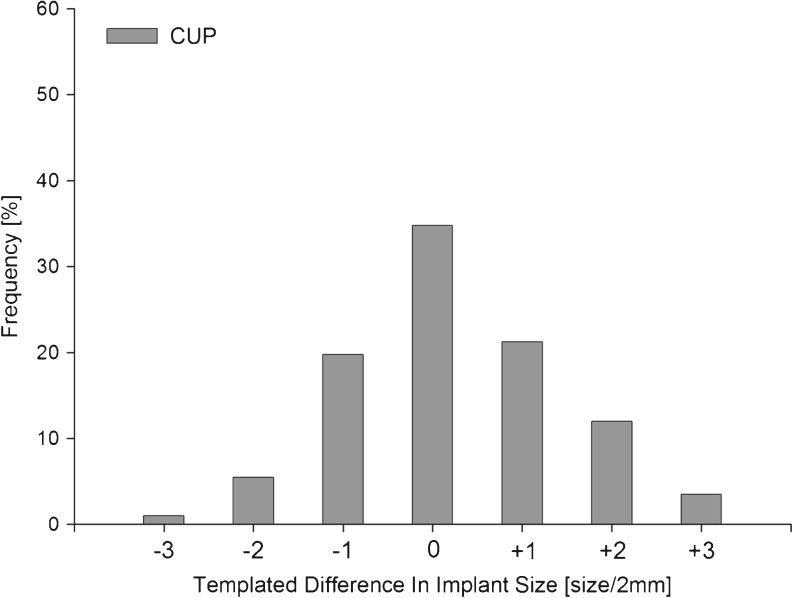
Acetabular cup size
Among all observers, pre-operative template accurately (±0) predicted acetabular size in 34.8 % (n = 139/400) of attempts. In 75.8 % (n = 303/400) the cup was predicted within one size difference (±1), 93.3 % (n = 373/400) were within two sizes different and 6.8 % (n = 27/400) were more than two sizes different (> ±2) (Fig. 3, Table 1). Inaccurately planned sizes were smaller in 26.5 % (n = 106/400) and larger in 38.8 % (n = 155/400).
Fig. 3.
Differences between templated and truly implanted acetabular cups. Positive values indicate templating of a larger component and negative values indicate templating of a smaller component
Inter-observer agreement for the acetabular cup was substantial between the more experienced surgeons (kappa 0.63), fair between the less experienced surgeons (kappa 0.29) and moderate between more and less experienced surgeons (kappa 0.45 and 0.44). Templating of the acetabular cup was significantly different (p = 0.002) between more and less experienced surgeons.
Discussion
Pre-operative templating is considered an important step in hip arthroplasty. Short-stem total hip arthroplasty has rapidly increased over recent years and shown good clinical short-term results [17, 18]. However, little is known about the value and accuracy of pre-operative templating in SHA.
This study shows that the accuracy of digital templating for the metaphyseally anchored SHA stem was not significantly different compared to that of a conventional THA stem. The accuracy obtained for prediction of the exact stem size in conventional THA was 47.5 %, which is in line with several studies reporting about an accuracy for digital templating of cementless THA between 31 % and 58 % [5, 12, 19, 20]. Similarly, within one size, an accuracy of 71–94 % has been reported in other THA studies [5, 9, 11, 12, 19, 20] and matches our result of 88.5 %. For SHA, only one retrospective study has evaluated the accuracy of digital templating. Wedemeyer et al. [10] reported for the Mayo short-stem (Zimmer, Warsaw, Indiana, USA), which also is a metaphyseally anchored SHA design, an accuracy of about 38 % for the exact size. This finding corresponds to our results of 49 % for the Metha stem. Moreover, within one size of margin they reported about an accuracy of 95 %, compared to 89 % in this study [10].
Comparison of the accuracy between THA and SHA was not significantly different and revealed similar results for both groups (88.5 % vs. 89.0 % within one stem size). This indicates that the stem size for SHA can as accurately be templated as the stem size for THA. This finding is relevant, as it had been discussed that SHA may cause a higher rate of femoral neck fractures during insertion [21]. However, a biomechanical study could demonstrate that the fracture risk with a proper implant size is equal for SHA and THA [22]. Therefore, it can be speculated that some of the reported intra-operative fractures might be related to the use of an oversized SHA implant. This is underscored by a study of Zeh et al. [21] who reported a high rate of femoral neck fractures during the learning curve for implantation of the Mayo stem. As the present study demonstrates that the stem size for SHA can exactly be determined in about 50 % of the cases and within one size margin in 89 %, this shows that a pre-operative templating is a useful tool to predict the proper implant size and thereby might be able to reduce intra-operative complications.
The acetabular components used for SHA and THA are basically the same. In both procedures, the acetabular component is placed first, which means the cup position and size is not influenced by the different stem design. Templating of cementless acetabular components has already been studied extensively by others [5, 9–12, 19, 20]. Those which evaluated digital templating of the acetabular component reported about an exact cup size in 25–40 % [5, 10, 12, 19, 20], compared to 34.8 % in our study. Within one size, these studies reported about an accuracy of 60–85 % [5, 9–12, 19, 20], which meets our finding of 75.8 %.
The influence of the professional experience on the accuracy of templating was also evaluated in this study. In the current literature this is controversial and contradictory results have been reported. While two studies found a significant influence of the professional experience on templating the components for THA [23, 24], two recently published studies did not find a significant influence [19, 25]. However, it should be noted that in all studies different types of observers were evaluated and some of the studies also included cemented as well as uncemented components and had small numbers in some of the subgroups [23, 25]. In the present study, a significant difference was found for the acetabular component for the surgeons having longer professional experience (attending/R-5) compared to the surgeon with a shorter experience (R-3/R-1). The finding goes along with most previous studies, which describe that templating of the acetabular cup is more challenging and usually shows a lower accuracy compared to the femoral stem [5, 9–11, 20]. No significant difference was found between the surgeons in templating the femoral stems, which indicates that templating of SHA is not only accurate, but also can reliably be performed by surgeons with a short professional experience.
Templating in hip arthroplasty can be performed by digital or analogue techniques. In this study, all radiographs were templated digitally, as conventional radiographs are no longer available in our and most other institutions. Controversy exists whether digital or acetate templating is the more precise one. Most studies reported about a higher accuracy for acetate templating [5, 11], whereas two other studies reported a higher accuracy for digital templating [7, 9]. Still, all studies demonstrate that both techniques are appropriate to determine the implant size [5, 7, 9, 11].
Overall, the accuracy of templating the correct implant for SHA was found to be good. However, it has to be noticed that templating of a 3-dimensional procedure is performed on plain 2-dimensional radiographs. Although the exact stem size can reliably be determined in about half of the hips, most of the remaining stems are determined within one size margin. Therefore, an intra-operative verification of the correct implant size, as for example by fluoroscopy, appears to be still recommended [25].
This study has limitations. The experienced and less experienced group only consisted of two surgeons each. And secondly, we did not take into account the severity of the pre-operative disease of the templated hips, which might have affected the accuracy of templating the components.
In conclusion, this study shows that digital templating for a metaphyseally anchored SHA hip implant can be performed as accurately as for a conventional THA hip implant and also can reliably be performed by surgeons with a short professional experience. Therefore, pre-operative templating offers a useful tool in SHA to predict the femoral stem size prior to surgery and should routinely be performed pre-operatively.
Acknowledgment
The authors thank Michael Lauseker from the Institute of Medical Informatics Biometry Epidemiology (IBE) for the expert advice in statistics.
Conflict of interest
The authors declare that they have no conflict of interest.
References
- 1.Eggli S, Pisan M, Muller ME. The value of preoperative planning for total hip arthroplasty. J Bone Joint Surg Br. 1998;80(3):382–390. doi: 10.1302/0301-620X.80B3.7764. [DOI] [PubMed] [Google Scholar]
- 2.Haddad FS, Masri BA, Garbuz DS, Duncan CP. The prevention of periprosthetic fractures in total hip and knee arthroplasty. Orthop Clin North Am. 1999;30(2):191–207. doi: 10.1016/S0030-5898(05)70074-2. [DOI] [PubMed] [Google Scholar]
- 3.Suh KT, Cheon SJ, Kim DW. Comparison of preoperative templating with postoperative assessment in cementless total hip arthroplasty. Acta Orthop Scand. 2004;75(1):40–44. doi: 10.1080/00016470410001708070. [DOI] [PubMed] [Google Scholar]
- 4.Della Valle AG, Padgett DE, Salvati EA. Preoperative planning for primary total hip arthroplasty. J Am Acad Orthop Surg. 2005;13(7):455–462. doi: 10.5435/00124635-200511000-00005. [DOI] [PubMed] [Google Scholar]
- 5.Della Valle AG, Comba F, Taveras N, Salvati EA. The utility and precision of analogue and digital preoperative planning for total hip arthroplasty. Int Orthop. 2008;32(3):289–294. doi: 10.1007/s00264-006-0317-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Fottner A, Steinbruck A, Sadoghi P, Mazoochian F, Jansson V. Digital comparison of planned and implanted stem position in total hip replacement using a program form migration analysis. Arch Orthop Trauma Surg. 2011;131(7):1013–1019. doi: 10.1007/s00402-010-1256-3. [DOI] [PubMed] [Google Scholar]
- 7.The B, Verdonschot N, Horn JR, Ooijen PM, Diercks RL. Digital versus analogue preoperative planning of total hip arthroplasties: a randomized clinical trial of 210 total hip arthroplasties. J Arthroplasty. 2007;22(6):866–870. doi: 10.1016/j.arth.2006.07.013. [DOI] [PubMed] [Google Scholar]
- 8.Zhao X, Zhu ZA, Zhao J, Li MQ, Wang G, Yu DG, Yu B. The utility of digital templating in total hip arthroplasty with Crowe type II and III dysplastic hips. IntOrthop. 2011;35(5):631–638. doi: 10.1007/s00264-010-0991-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Whiddon DR, Bono JV, Lang JE, Smith EL, Salyapongse AK. Accuracy of digital templating in total hip arthroplasty. Am J Orthop (Belle Mead NJ) 2011;40(8):395–398. [PubMed] [Google Scholar]
- 10.Wedemeyer C, Quitmann H, Xu J, Heep H, Knoch M, Saxler G. Digital templating in total hip arthroplasty with the Mayo stem. Arch Orthop Trauma Surg. 2008;128(10):1023–1029. doi: 10.1007/s00402-007-0494-5. [DOI] [PubMed] [Google Scholar]
- 11.Iorio R, Siegel J, Specht LM, Tilzey JF, Hartman A, Healy WL. A comparison of acetate vs digital templating for preoperative planning of total hip arthroplasty: is digital templating accurate and safe? J Arthroplasty. 2009;24(2):175–179. doi: 10.1016/j.arth.2007.11.019. [DOI] [PubMed] [Google Scholar]
- 12.Gamble P, Beer J, Petruccelli D, Winemaker M. The accuracy of digital templating in uncemented total hip arthroplasty. J Arthroplasty. 2010;25(4):529–532. doi: 10.1016/j.arth.2009.04.011. [DOI] [PubMed] [Google Scholar]
- 13.Morrey BF, Adams RA, Kessler M. A conservative femoral replacement for total hip arthroplasty. A prospective study. J Bone Joint Surg Br. 2000;82(7):952–958. doi: 10.1302/0301-620X.82B7.10420. [DOI] [PubMed] [Google Scholar]
- 14.Kamada S, Naito M, Nakamura Y, Kiyama T. Hip abductor muscle strength after total hip arthroplasty with short stems. Arch Orthop Trauma Surg. 2011;131(12):1723–1732. doi: 10.1007/s00402-011-1350-1. [DOI] [PubMed] [Google Scholar]
- 15.Bono JV. Digital templating in total hip arthroplasty. J Bone Joint Surg Am. 2004;86-A(Suppl 2):118–122. doi: 10.2106/00004623-200412002-00016. [DOI] [PubMed] [Google Scholar]
- 16.Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1977;33(1):159–174. doi: 10.2307/2529310. [DOI] [PubMed] [Google Scholar]
- 17.Briem D, Schneider M, Bogner N, Botha N, Gebauer M, Gehrke T, Schwantes B. Mid-term results of 155 patients treated with a collum femoris preserving (CFP) short stem prosthesis. Int Orthop. 2011;35(5):655–660. doi: 10.1007/s00264-010-1020-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lerch M, Haar-Tran A, Windhagen H, Behrens BA, Wefstaedt P, Stukenborg-Colsman CM. Bone remodelling around the Metha short stem in total hip arthroplasty: a prospective dual-energy X-ray absorptiometry study. Int Orthop. 2012;36(3):533–541. doi: 10.1007/s00264-011-1361-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hsu AR, Kim JD, Bhatia S, Levine BR. Effect of training level on accuracy of digital templating in primary total hip and knee arthroplasty. Orthopedics. 2012;35(2):e179–e183. doi: 10.3928/01477447-20120123-15. [DOI] [PubMed] [Google Scholar]
- 20.Crooijmans HJ, Laumen AM, Pul C, Mourik JB. A new digital preoperative planning method for total hip arthroplasties. Clin Orthop Relat Res. 2009;467(4):909–916. doi: 10.1007/s11999-008-0486-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Zeh A, Radetzki F, Diers V, Bach D, Rollinghoff M, Delank KS. Is there an increased stem migration or compromised osteointegration of the Mayo short-stemmed prosthesis following cerclage wiring of an intrasurgical periprosthetic fracture? Arch Orthop Trauma Surg. 2011;131(12):1717–1722. doi: 10.1007/s00402-011-1342-1. [DOI] [PubMed] [Google Scholar]
- 22.Jakubowitz E, Seeger JB, Lee C, Heisel C, Kretzer JP, Thomsen MN. Do short-stemmed-prostheses induce periprosthetic fractures earlier than standard hip stems? A biomechanical ex-vivo study of two different stem designs. Arch Orthop Trauma Surg. 2009;129(6):849–855. doi: 10.1007/s00402-008-0676-9. [DOI] [PubMed] [Google Scholar]
- 23.Mittag F, Ipach I, Schaefer R, Meisner C, Leichtle U. Predictive value of preoperative digital templating in THA depends on the surgical experience of the performing physician. Orthopedics. 2012;35(2):e144–e147. doi: 10.3928/01477447-20120123-14. [DOI] [PubMed] [Google Scholar]
- 24.Carter LW, Stovall DO, Young TR. Determination of accuracy of preoperative templating of noncemented femoral prostheses. J Arthroplasty. 1995;10(4):507–513. doi: 10.1016/S0883-5403(05)80153-6. [DOI] [PubMed] [Google Scholar]
- 25.Efe T, El Zayat BF, Heyse TJ, Timmesfeld N, Fuchs-Winkelmann S, Schmitt J. Precision of preoperative digital templating in total hip arthroplasty. Acta Orthop Belg. 2011;77(5):616–621. [PubMed] [Google Scholar]