Abstract
There is significant support for exposure therapy as an effective treatment for posttraumatic stress disorder (PTSD) across a variety of populations, including veterans; however, there is little empirical information regarding how veterans of different war theaters respond to exposure therapy. Accordingly, questions remain regarding therapy effectiveness for treatment of PTSD for veterans of different eras. Such questions have important implications for the dissemination of evidence based treatments, treatment development, and policy. The current study compared treatment outcomes across 112 veterans of the Vietnam War, the first Persian Gulf War, and the wars in Afghanistan and Iraq. All subjects were diagnosed with PTSD and enrolled in Prolonged Exposure (PE) treatment. Veterans from all three groups showed significant improvement in PTSD symptoms, with veterans from Vietnam and Afghanistan/Iraq responding similarly to treatment. Persian Gulf veterans did not respond to treatment at the same rate or to the same degree as veterans from the other two eras. Questions and issues regarding the effectiveness of evidence based treatment for veterans from different eras are discussed.
Keywords: posttraumatic stress disorder, veterans, prolonged exposure, treatment effectiveness, exposure therapy
Since the inclusion of posttraumatic stress disorder (PTSD) in the third edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM–III; APA, 1980), there have been a number of studies evaluating interventions for PTSD in combat veterans, as well as for a range of other traumatized patient populations (Bradley, Greene, Russ, Dutra, & Westen, 2005, meta-analysis; Cloitre, 2009, review; IOM, 2007). These studies generally support the use of exposure-based interventions for this population. In fact, the most recent VA/Department of Defense (DoD) Clinical Practice Guidelines identified exposure therapy as one of four evidence-based psychotherapies for veterans with PTSD (U.S. Department of Veterans Affairs & U.S. Department of Defense, 2010), and the Institute of Medicine (IOM) recognized exposure therapies as the only treatment approach with sufficient efficacy data for the treatment of combat-related PTSD (IOM, 2007).
Although the PTSD treatment outcome literature is fairly robust for both veteran and civilian patient populations, it is generally recognized in the trauma field, albeit not fully understood, that combat veterans do not fare as well in treatment as other traumatized groups (Cason, Grubaugh, & Resick, 2002). More specifically, a 2005 meta-analysis on psychotherapies for PTSD found that type of trauma was a significant predictor of preversus posttreatment effect size, with combat veterans demonstrating the least change after treatment, followed by a mixed trauma group, and then sexual assault survivors (Bradley et al., 2005). Worth noting, the above studies on combat related PTSD were based largely on Vietnam era veteran samples and on interventions with varying levels of therapeutic exposure to trauma-related stimuli.
Between 2002 and 2008 alone, tens of thousands of veterans returning from Operation Enduring Freedom (OEF) and Operation Iraqi Freedom (OIF) received combat-related PTSD services within the VA (Seal et al., 2010). As this number has increased, so have efforts to formally include OEF/OIF and Operation New Dawn (OND) veterans in treatment outcome studies. Due to the recent nature of the current conflicts in the Middle East, however, few of these PTSD treatment outcome studies have included representative samples of this new generation of veterans (Cigrang, Peterson, & Schobitz, 2005; Rauch et al., 2009; Tuerk, Yoder, Ruggiero, Gros, & Acierno, 2010; Tuerk et al., 2011). Although few in number, these studies demonstrate better pre- to posttreatment effect sizes than previous studies using samples composed predominantly of Vietnam era veterans (e.g., Cooper & Clum, 1989; Glynn et al., 1999; Keane, Fairbank, Caddell, & Zimering, 1989) suggesting that OEF/OIF/OND veterans may fare better in PTSD treatment than their predecessors. However, to date, we know very little about potential group differences between cohorts of veterans who served in different wars, especially when using manualized treatments that standardize clinical procedures and amount/session dose of therapeutic exposure.
The purpose of the current study is to compare PTSD and related outcomes in veterans from various combat theaters, OEF/OIF/OND, Gulf War, Vietnam, receiving a manualized Prolonged Exposure (PE) intervention for PTSD (PE; Foa, Hembree, & Rothbaum, 2007) in a southeastern VA Medical Center. To date, only a few studies have specifically compared PTSD treatment response by theater. Chard and colleagues (2010) compared Vietnam to OEF/OIF/OND veterans and found that OEF/OIF/OND veterans had lower PTSD severity scores post treatment once pretreatment severity and number of sessions attended were taken into account. Another study found that an OEF/OIF/OND cohort had lower PTSD symptoms at initial assessment compared to Vietnam veterans and that OEF/OIF/OND veterans had more protective factors in place when enrolling in PTSD treatment (Fontana & Rosenheck, 2008). Given the chronic and severe nature of PTSD among Vietnam veterans, these findings are not altogether surprising. However, more data along this theme are needed in order to make definitive conclusions regarding variability in treatment response across different cohorts of veterans. Such data will be informative as our public and private health care systems will be tasked with treating an aging cohort of older veterans with chronic PTSD while simultaneously responding to the needs of a new generation of combat veterans who may have unique symptom presentations and preferences.
Method
Study Overview
Participants were veterans receiving outpatient treatment for PTSD at a Veterans Affairs Medical Center (VAMC) between September, 2008 and August, 2010. All participants had a diagnosis of PTSD via a standardized clinical interview. The intake interview employed by the PTSD clinic consists of meeting with clinic staff to complete self-report measures (demographics form, PCL, BDI, Life Events Checklist), the Clinician Administered PTSD Scale (CAPS), and a semistructured clinical interview. The clinician completing the intake creates a report based on the data obtained in the interview and presents the case to the entire PTSD clinic team at a weekly staffing. If a patient is deemed to meet criteria for PTSD and be appropriate for individual, trauma-focused treatment, they are assigned to a clinician at that staff meeting. The current investigation is a post hoc, nonrandomized effectiveness study using archival data from patients treated by a PTSD Clinical Team (PCT). The archival data were obtained from a program evaluation database kept within the clinic. Assessment measures (PCL, BDI-II) completed by patients as part of evidence-based treatments are entered into the database by clinic staff. Outcome data included in this manuscript were taken from all patients receiving PE from three clinicians over the time period noted above. All veterans were treated with PE as part of their routine clinical care. Veterans were not subject to any protocol-driven exclusion criteria or given incentives to participate in treatment. This archival study was conducted with full approval from relevant Institutional Review Boards (IRBs).
Participants
The sample consisted of 61 OEF/OIF/OND, 34 Vietnam, and 17 Gulf War veterans. The majority of the sample was white (n = 64, 57%) and male (n = 103, 92%). Sixty-nine participants (60%) had a service-connection disability rating for PTSD. The mean age of the sample was 41 and the modal age was 34. Table 1 displays patient characteristics including military branch and PTSD service connection status, as well as distribution across therapists. Patients were identified for treatment through referrals from primary care providers, general mental health providers, and case managers to the PCT. All patients completed either the Clinician Administered PTSD-Scale (CAPS; Blake et al., 1995) or the PTSD and depression modules of the Structured Clinical Interview for the Diagnostic and Statistical Manual of Mental Disorders (4th ed., SCID-IV; First, Spitzer, Gibbon, & Williams, 1996) upon entry into PCT. Therapist assignment was based on provider availability in line with standard operating procedures of an outpatient psychotherapy clinic. All patients were treated by one of two clinical psychologists or a social worker (MSW) with specialized training in trauma related issues and PE (see Table 1). Treatment sessions were not coded for treatment fidelity; however, therapists participated in weekly group supervision as part of routine clinical practice to guard against therapist drift in skills. A portion (n = 28, 46%) of the subsample of OEF/OIF/OND veterans reported in this study are considered in greater detail in a previously published study (Tuerk et al., 2011); however, the foci of the two articles is sufficiently different to warrant the overlap.
Table 1.
Participant Demographics and Characteristics
| Theater | OIF/OEF/OND | Vietnam | Gulf War | Total |
|---|---|---|---|---|
| Ethnicity | ||||
| Caucasian | 38 (62%) | 21 (62%) | 6 (35%) | 65 (58%) |
| African-American | 20 (33%) | 13 (38%) | 10 (59%) | 43 (38%) |
| Hispanic | 3 (5%) | 0 (0%) | 1 (6%) | 4 (4%) |
| Military Branch | ||||
| Army | 37 (61%) | 18 (53%) | 9 (53%) | 64 (57%) |
| Marines | 14 (23%) | 7 (21%) | 5 (29%) | 26 (23%) |
| National Guard | 5 (8%) | 2 (6%) | 1 (6%) | 8 (7%) |
| Air Force | 3 (5%) | 4 (12%) | 1 (6%) | 8 (7%) |
| Navy | 2 (3%) | 3 (9%) | 1 (6%) | 6 (5%) |
| PTSD Service Connection | ||||
| 0% | 20 (33%) | 15 (44%) | 9 (53%) | 46 (41%) |
| 10% | 3 (5%) | 2 (6%) | 0 (0%) | 5 (4%) |
| 30% | 20 (33%) | 4 (12%) | 4 (24%) | 28 (25%) |
| 50% | 11 (18%) | 9 (26%) | 2 (12%) | 22 (20%) |
| 70% | 4 (7%) | 1 (3%) | 0 (0%) | 5 (4%) |
| 100% | 3 (5%) | 3 (9%) | 2 (12%) | 8 (7%) |
| Therapist | ||||
| 1 | 31 (51%) | 25 (74%) | 10 (59%) | 66 (59%) |
| 2 | 26 (43%) | 6 (18%) | 4 (24%) | 36 (32%) |
| 3 | 4 (7%) | 3 (9%) | 3 (18%) | 10 (9%) |
| Total N (%) | 61 (100%) | 34 (100%) | 17 (100%) | 112 (100%) |
Intervention
Prolonged Exposure (PE; Foa et al., 2007) is a manualized, 90-min, weekly, treatment protocol that consists of the following major components: (a) psycho-education regarding common reactions to trauma and a detailed rationale for treatment; (b) self assessment of anxiety using subjective units of distress (SUDs); (c) repeated in vivo exposure to situations avoided due to distress; and (d) repeated, prolonged imaginal exposure to traumatic memories followed by processing or discussion of the memories. In Vivo exposure involves having the patient approach a hierarchy of feared, but safe, trauma-related situations as homework between sessions. Imaginal exposure involves assisting patients to repeatedly recount their traumatic event(s) in detail, while vividly imagining the event(s). Treatment sessions are audio-taped for patients to review between sessions for additional exposure. Because the current investigation is an effectiveness study of PE conducted with veterans in the ecological context of a PCT clinic, the length of treatment varied by patient and was informed by ongoing psychometric assessment and collaborative evaluation of progress. The nature of the results offered below are exploratory with no a priori hypothesis testing.
Measures
PTSD Checklist—Military Version
The PCL-M (PCL-M; Blanchard, Jones-Alexander, Buckley, & Forneris, 1996) is a 17-item self-report measure of PTSD symptoms based on DSM–IV criteria. Scores on the PCL-M range from 17 to 85 with higher scores reflecting greater PTSD severity. The instrument has been shown to have excellent internal consistency (αs > .94) and test–retest reliability (r = .96; for review see Orsillo, 2001). In addition, the PCL-M has demonstrated excellent convergent validity with alternative measures of PTSD (rs range from .77 to .93; Orsillo, 2001).
Beck Depression Inventory-II
The BDI-II (BDI-II; Beck, Steer, & Brown, 1996) is a 21-item self report measure that assesses behavioral and affective symptoms of depression experienced over the past 2 weeks. Scores on the BDI-II range from 0 to 63 with higher scores reflecting greater depression severity. The BDI-II demonstrates adequate convergent validity, discriminant validity, test–retest reliability (r = .93), and good internal consistency (α < .92; Beck et al., 1996; Steer & Clark, 1997).
Data Analysis
The data for the current study were assessed using a mixed design 2 × 3 ANOVA (Time × Theater) and hierarchical linear modeling (HLM). The ANOVA was used to compare first session and final session scores on the PCL-M and BDI-II across Vietnam, OEF/OIF/OND, and Gulf War Veterans. An intent-to-treat (ITT) sample was used in which missing posttreatment data on the PCL-M and BDI-II were addressed using multiple imputation to address missing posttreatment data (MI; Rubin, 1987). MI involves the generation of multiple separate data sets (five for the current study) in which missing data are estimated from other variables. For the present study, pretreatment scores (PCL-M and BDI-II) and demographic variables (age, sex, ethnicity, and combat theater) were used. Each data set is then analyzed using a separate 2 × 3 ANOVA. Parameter estimates from each data set are combined using SAS Macro MIANALYZE. Approximately 19% (n = 21) of the current sample had missing data for posttreatment measures (nGulf War = 2 or 2% nOEF/OIF/OND = 18 or 16% nVietnam = 1 or 1%), including participants that were identified as noncompleters (n = 18). MI has been show to provide more accurate estimates of standard errors, and thus more accurate estimates overall, for incomplete data as compared to alternative methods such as last observation carried forward (LOCF) or mean replacement (Allison, 2001). HLM was used to examine differences in linear change trajectories across veterans from the different theaters. Time was scaled in weeks. The model used for the current study included a level one fixed effect for intercept and slope during the course of treatment and a level two fixed effect for theater of war (OEF/OIF/OND and Gulf War). Finally, Cohen’s d effect sizes were calculated from paired sample t tests for each theater to allow for comparison across studies.
Results
Descriptive statistics can be found in Table 2. A 2 × 3 (Time × Theater) ANOVA was conducted to assess changes in symptoms across time and theater of war. Noncompleters were defined as veterans that completed fewer than 6 sessions of treatment and had less than a 1 standard deviation change in PCL scores (to distinguish these veterans from those who received fewer than six sessions of treatment because they experienced rapid improvement; i.e., resolved cases were considered completers). Using these criteria, 18 participants were classified as noncompleters (nGulf War = 2 or 12% nOEF/OIF/OND = 15 or 26% nVietnam = 1 or 3%). The treatment completion rate differed by theater [χ2(2) = 8.50, p < .05]. However, a one way ANOVA indicated that there was not a significant difference in the number of sessions attended by OEF/OIF/OND (M = 8.20), Vietnam (M = 10.2), and Gulf War (M = 9.71) veterans [F(2, 109) = 1.66, p = .19]. Also, pretreatment severity did not differ as a function of theater on the PCL-M [F(1, 107 = 0.13, p = .72] or BDI-II [F(1, 107) = 0.46, p = .50]. Additionally, there was no difference in pretreatment PCL-M [F(1, 105) = 0.67, p = .42] or BDI-II scores [F(1, 105) = 0.03, p = .86] between those noncompleters and completers. Pretreatment scores also did not vary as a function of theater. Based on these findings, noncompleters appeared not to be quantitatively different from those that completed treatment. As such, data from these cases (n = 18) were included in the MI procedures to compute posttreatment scores on the PCL-M and BDI-II.
Table 2.
Descriptive Statistics for PCL-M and BDI-II Across Theater of War
| OEF/OIF/OND | Vietnam | Gulf War | |
|---|---|---|---|
| PCL - M | |||
| First Session | 62.13 (10.41)A | 64.44 (10.95)A | 66.53 (6.06)A |
| Final Session | 33.31 (12.54)B | 39.63 (16.24)B | 47.94 (14.36)C |
| d | 3.05 | 2.07 | 1.81 |
| BDI-II | |||
| First Session | 28.42 (9.80)A | 30.67 (10.53)A | 29.93 (10.10)A |
| Final Session | 15.73 (10.62)B | 15.00 (9.54)B | 18.71 (10.04)B |
| d | 1.27 | 1.91 | 1.42 |
| N | 61 | 34 | 17 |
Note. PCL-M = Posttraumatic Symptom Checklist–Military. BDI-II = Beck Depression Inventory, 2nd edition. d = Cohen’s D based on pairwise t-test within each theater. Subscripts indicate significant differences within each measure.
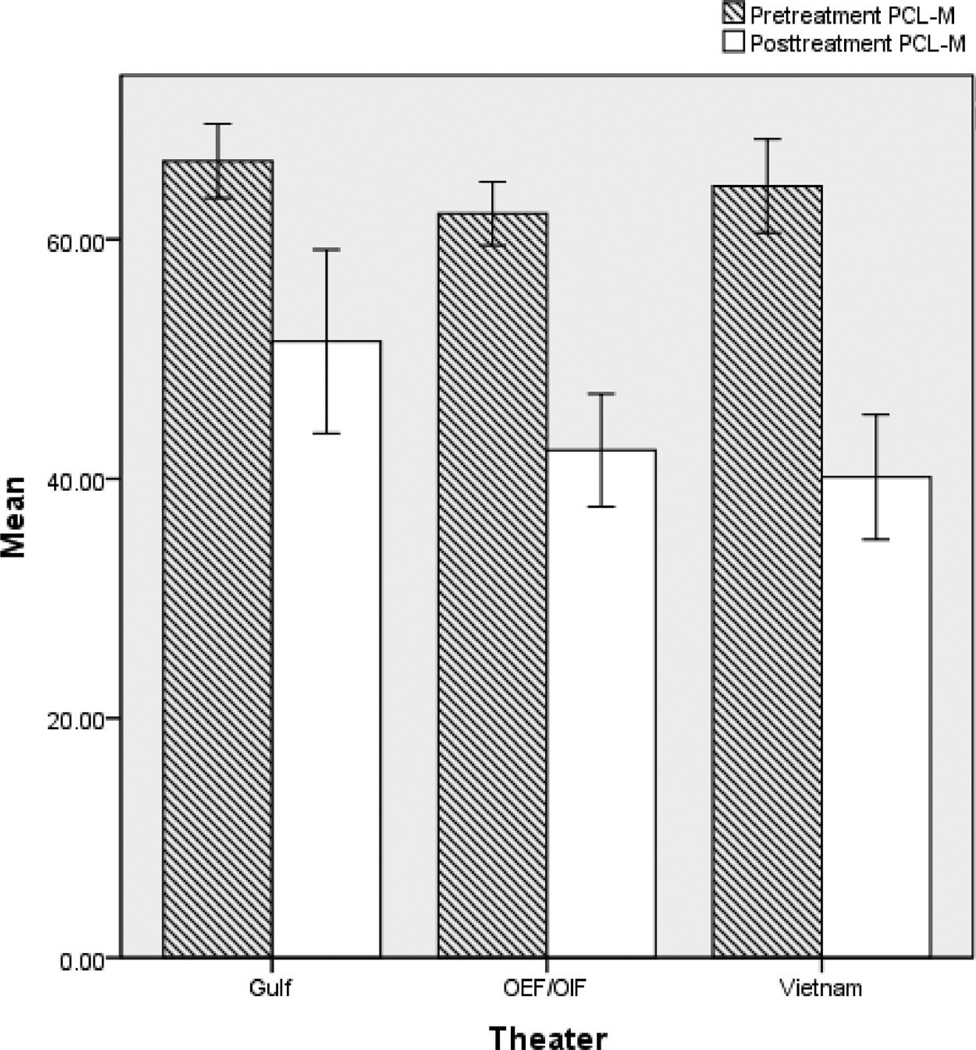
The results of the 2 × 3 ANOVA indicated a significant main effect on the PCL-M for both Time [F(1, 109) = 227.91, p < .01, partial η2 = 0.67] and Theater [F(2, 109) = 8.12, p < 0.01, partial η2 = 0.12]. However, the interaction between Time and Theater was also significant, [F(2, 109) = 3.35, p < .05, partial η2 = 0.06] and attention was thus directed to simple effects analyses split across Time. These analyses indicated that there was not a significant difference in PCL-M scores between Vietnam (M = 64.44, SD = 11.21), OEF/OIF/OND (M = 62.13, SD = 10.41), and Gulf War Veterans (M = 66.53, SD = 6.06) for the first session [F(2, 109) = 1.46, p = .24]. However, there was a significant difference in PCL-M scores for the final session, [F(2, 109) = 8.44, p < .01]. Pairwise post hoc comparisons using the Tukey-Kramer method with a harmonic mean sample size of 22.16 were used to determine significant differences in final session scores. The findings suggested that PTSD severity for Vietnam (M = 39.63, SD = 16.24) and OEF/OIF/OND (M = 33.31, SD = 12.54) veterans did not differ, but both groups scored significantly lower on the PCL-M than Gulf War veterans (M = 47.94, SD = 14.36; see Table 2 & Figure 1).
Figure 1.
First and final session mean scores on PCL-M across theater. Error bars represent 95% confidence intervals.
For the BDI-II, there was a significant main effect for Time [F(1, 109) = 102.06, p < .01)] but not for Theater [F(2, 109) = 0.37, p = .69]. The Theater × Time interaction was also not significant [F(2, 109) = 1.00, p = .37]. Taken together, these findings suggest that BDI scores decreased as a result of treatment and that scores obtained during the first and final treatment sessions were not significantly different by theater. In addition, PTSD service connection did not significantly influence outcomes on either the PCL-M or the BDI-II [F(1, 108) = 0.75, p = .39; F(1, 108) = 1.89, p = .17, respectively]. Finally, a 3 × 2 ANOVA (Therapist × Time) was run to examine whether therapist effects differed. The results suggested that there were no differences in outcomes across therapists [F(2, 107) = .085, p = .36].
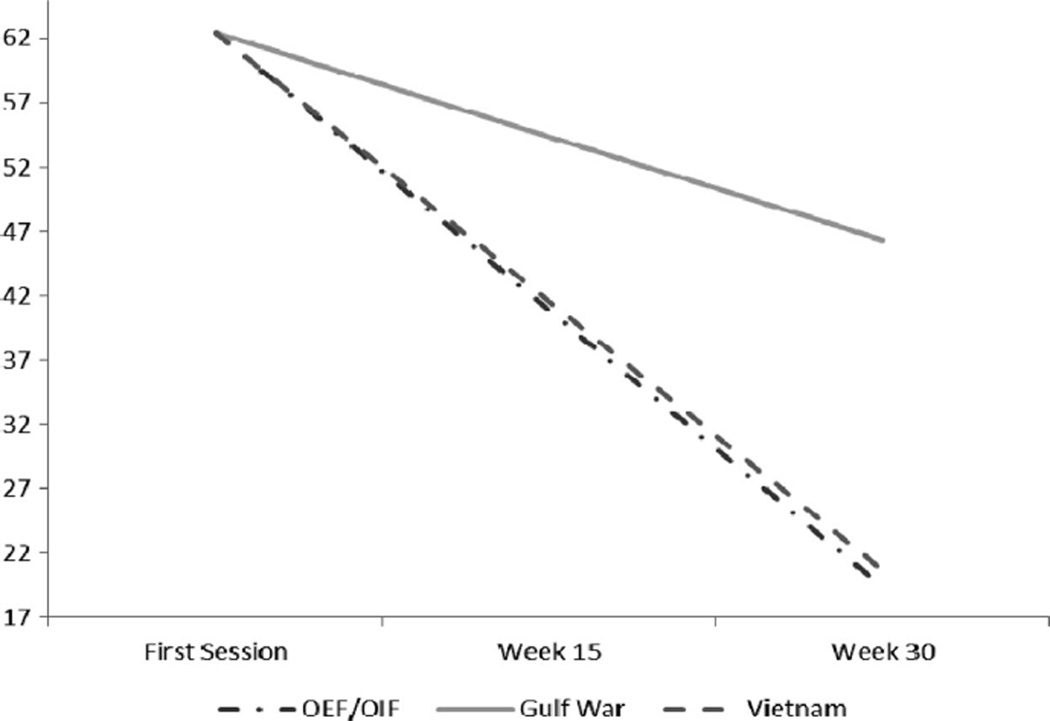
To further examine the degree to which treatment response varied as a function of theater, a multilevel model was fitted to the data that used PCL-M and BDI-II scores obtained at every other session over the course of treatment. To account for variability in treatment length and spacing of sessions, time was scaled in weeks. A two-level model was fitted to the PCL-M data that included a level one fixed effect for Time and a level two fixed effect for slope for Gulf War veterans and OEF/OIF/OND veterans (see Table 3). The findings suggested that OEF/OIF/OND veterans did not differ from Vietnam veterans (β11 = −0.04, p = .86), but Gulf War veterans’ PTSD symptoms declined at a significantly lower rate than Vietnam veterans symptoms (β12 = 0.92, p < .01; Figure 2). Another model was run in which OEF/OIF/OND and Vietnam veterans were collapsed into a single group and compared to Gulf War veterans. These findings suggested that Gulf War veterans’ symptoms decreased at a significantly lower rate than veterans of other theaters (β11 = 0.95, p < .01). Furthermore, Theater accounted for 15% of the variance in rate of change, suggesting that theater membership had a “medium” size of effect on rate of change.
Table 3.
Fixed and Random Effects for Linear Change Model Across Theater
| Parameter | PCL-M | BDI-II | ||
|---|---|---|---|---|
| Fixed Effects | ||||
| Intercept (First Session) | β00 | 62.05** (0.99) | 28.51** (1.08) | |
| Treatment rate of change | β10 | −1.50** (0.20) | −0.86** (0.12) | |
| OEF/OIF/OND | β11 | −0.05 (0.27) | 0.09 (0.16) | |
| Gulf War | β12 | 0.92** (0.29) | 0.45** (0.16) | |
| Random Effects | ||||
| Level 1 | e2 | 61.62 | 33.08 | |
| Level 2 | 50.93** (7.13) | 84.68** (9.21) | ||
| 0.78** (0.88) | 0.29** (0.54) |
Note. PCL-M = Posttraumatic Symptom Checklist–Military. BDI-II = Beck Depression Inventory, 2nd edition.
= p < .01.
Figure 2.
Change trajectories for OEF/OIF/OND, Vietnam, and Gulf War veterans from first session to 30 weeks of treatment for PCL-M.
A similar model was fitted to the BDI-II data. Similar results were obtained with OEF/OIF/OND not significantly differing from Vietnam veterans (β11 = 0.09, p = .58), but Gulf War veterans’ symptoms declining at a significantly lower rate (β12 = 0.45, p < .01). Additionally, when collapsing Vietnam and OEF/OIF/OND veterans, Gulf War veterans’ symptoms declined at a significantly lower rate relative to the other two cohorts (β11 = 0.40, p < .01). Gulf War status accounted for 13% of the variance in the rate of change.
Paired sample t tests were conducted across each theater of war to obtain a Cohen’s d measure of effect size. The t tests yielded statistically significant results suggesting that all groups benefited from treatment. The prepost PCL-M effect size for Gulf War veterans (d = 1.81) was lower than that of OEF/OIF/OND (d = 3.05) and Vietnam era veterans (d = 2.07). The BDI effect size for Gulf War veterans (d = 1.42) was comparable to that of OEF/OIF/OND veterans (d = 1.27), but less than that of Vietnam veterans (d = 1.91).
Discussion
There are several notable findings of this study. First, the effect sizes of PE for the three cohorts were large, ranging from 1.81 to 3.05, with an overall effect size of 2.73 across the three groups. Thus, in this, one of the largest effectiveness studies to date investigating the impact of PE on PTSD in combat veterans, further evidence was found for the robust nature of the intervention. Second, we found notable differences in treatment response by combat theater. The treatment effect size for Gulf War era veterans was lower than the treatment effect sizes for Vietnam and OEF/OIF/OND veterans, and Gulf War era veterans’ symptoms declined at significantly slower rates than those of the other two cohorts.
Several factors, in addition to the robust nature of PE, may have contributed to the large effect sizes found in this study. First, all three therapists who treated the veterans in this study received specialized training in PE. More specifically, all three completed a week-long training in PE as part of the Department of Veterans Affairs national PE rollout initiative, and two of the three are national level consultants and/or trainers for the initiative. Second, the majority of veterans completed a three to four session PTSD orientation class in which they were educated about the nature of PTSD and available treatment options. Importantly, veterans who started the group were required to attend the majority of the class sessions prior to being assigned a therapist for individual treatment—a requirement which selects for motivated, conscientious participants. Each of these factors likely augmented the robust nature of PE resulting in the notably large effect sizes found in this study. Unfortunately, information about those who drop out of the orientation class, and the attrition rates was not available for this report.
While all groups improved over the course of treatment, specific comparisons of the three groups yielded interesting results. First, the noncompletion rate varied significantly across Theater, with OEF/OIF/OND veterans completing the treatment at a lower rate than veterans from the Gulf War or Vietnam—74% (45), 88% (15), & 97% (33), respectively. PCL-M and BDI-II scores in the three cohorts were not significantly different at pre- or posttreatment and multilevel models suggested the rate of improvement in the Vietnam and OEF/OIF/OND groups did not differ significantly during the course of treatment. Two previous studies informally compared treatment outcomes between recently returning veterans and Vietnam era veterans. In one study, after controlling for pretreatment severity and number of sessions, OEF/OIF veterans had lower PTSD scores at posttreatment following a course of Cognitive Processing Therapy (CPT) for PTSD than Vietnam veterans (Chard, Owens, & Cottingham, 2010). In a small (n = 10) pilot study, PE was found to be similarly effective on PTSD severity across theaters of combat (Rauch et al., 2009). Although Rauch et al. was not powered to make substantial conclusions regarding the relative treatment effectiveness of PE, results from the current study suggest that treatment seeking veterans returning from the wars in Iraq and Afghanistan with PTSD do not differ significantly from Vietnam veterans either in their initial symptom presentation or in their response to PE.
A surprising finding, however, was that Gulf War veterans responded differently to PE than did veterans from other theaters. That is, while their symptoms did not differ significantly at the initial assessment, Gulf War veterans had higher symptoms at the final session than both OEF/OIF/OND and Vietnam era veterans (see Table 2, Figure 1) and the slope of their symptom improvement over the course of treatment was not as steep as that of the other two cohorts (see Table 3, Figure 2). One possible explanation for this finding is the difference in the specific combat experiences of Gulf War veterans. In the current study we did not formally assess trauma characteristics related to combat exposure, but anecdotally, this cohort of veterans was more likely to report chronic fear of death by biological agents, rather than active combat, as their most distressing traumatic memories. Specifically, a number of the Gulf War veterans in this sample described traumatic memories of hearing air raid sirens, putting on chemical protective suits, and waiting in Conex box-type bunkers in the dark for hours—a maneuver that was sometimes repeated several times in a 24-hr period. These patients reported fearing for their lives and a of sense helplessness, perceptions which qualify the events as traumatic according to the DSM–IV, but are qualitatively different than traumatic events typically reported by combat veterans. It is unlikely that the type of trauma reported, in and of itself, differentially influences treatment responses because PE has been found to be effective across a variety of different traumatic contexts (i.e., rape, motor vehicle accidents, and general combat). Accordingly, if the difference in treatment response for Gulf-war veterans reported here is replicable and accurate, it may be due to population differences related to variable stress-diathesis selection processes for chronic fear experiences versus acute types of trauma or to variable self-selection pressures and concurrent treatment seeking behaviors that may vary in some important, though unmeasured, ways among war-zone cohorts. These potential explanations are based on clinical judgment not data and are offered here only as potential avenues for future research.
Limitations
It is important to qualify the findings reported with several limitations. First, the study employed post hoc, nonrandomized, observational methodology which makes it impossible to draw definitive conclusions about causes of the differences found between the three groups. There are multiple possible confounding factors that may have influenced the results, including patient distribution across therapist, number of sessions completed, and patient comorbidity. Many of these issues are inherent in effectiveness research where concessions are made in order to approximate the effects of a treatment in more of a “real world” setting. As such, the data reported here are from patients moved through our PCT clinic in the standard operating procedure currently in place. Second, therapist fidelity to the PE protocol and patient compliance were not assessed. While fidelity checks are also less crucial in effectiveness research, all therapists were trained in PE as part of the VA national dissemination initiative and participated in weekly group and individual supervision. Supervision was conducted by the second author (P.T.) who is a national trainer in the PE initiative and included occasional tape review and problem solving regarding patient compliance. This level of supervision is part of the standard operating procedure in our clinic. There were no differences in treatment outcomes between therapists.
Future Directions
It may be worthwhile for researchers and clinicians in other PCTs to examine their clinic databases to assess whether Gulf War veterans in their clinics are responding differently to PTSD treatment than other cohorts. If the finding is replicated, future, more tightly controlled, research that attempts to parse out the relevant variables behind the finding will be a valuable addition to the field of PTSD treatment. In addition, future studies that attempt to control for the limitations noted above may help elucidate the results reported here. For example, randomizing randomizing patients to therapists, and assessing treatment fidelity will allow for firmer conclusions to be drawn about possible differences between cohorts in response to treatment. The current study also found that service connection did not affect participants’ symptom improvement over the course of treatment. This finding is consistent with what was reported by Tuerk et al., (2011) and provides further suggestion that PE can be effective for veterans despite service connection disability for PTSD. More investigation about the impact of service connection on treatment gains will help address longstanding concerns about the role of secondary gains in Veterans Health Administrations settings.
Overall, the present study found further support for the effectiveness of PE with combat veterans, as treatment effect sizes were large across cohorts, with veterans of the Gulf War benefiting but responding at a slower rate than veterans from other wars. Interestingly, Vietnam-era veterans who have had chronic PTSD symptoms for decades self-reported similar levels of improvement as veterans from more recent wars. Variables potentially associated with treatment response, such as initial chief complaint, specific combat trauma characteristics, and potential predisposing characteristics associated with veterans from different cohorts need to be formally identified and tested in future studies.
References
- Allison PD. Missing data. Thousand Oaks, CA: Sage; 2001. [Google Scholar]
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 3rd ed., text revision. Washington, DC: Author; 1980. [Google Scholar]
- Beck AT, Steer RA, Brown GK. BDI-II Manual. San Antonio, TX: The Psychological Corporation; 1996. [Google Scholar]
- Blake DD, Weathers FW, Nagy LM, Kaloupek DG, Gusman FD, Charney DS, Keane TM. The development of a clinician-administered PTSD scale. Journal of Traumatic Stress. 1995;8:75–90. doi: 10.1007/BF02105408. [DOI] [PubMed] [Google Scholar]
- Blanchard EB, Jones-Alexander J, Buckley TC, Forneris CA. Psychometric properties of the PTSD checklist (PCL) Behaviour Research and Therapy. 1996;34:669–673. doi: 10.1016/0005-7967(96)00033-2. [DOI] [PubMed] [Google Scholar]
- Bradley R, Greene J, Russ E, Dutra L, Westen D. A multidimensional meta-analysis of psychotherapy for PTSD. American Journal of Psychiatry. 2005;162:214–227. doi: 10.1176/appi.ajp.162.2.214. [DOI] [PubMed] [Google Scholar]
- Cason D, Grubaugh A, Resick P. Gender and PTSD treatment: Efficacy and effectiveness. In: Kimerling R, Ouimette P, Wolfe J, editors. Gender and PTSD. New York, NY: Guilford Press; 2002. pp. 305–334. [Google Scholar]
- Chard KM, Schumm JA, Owens GP, Cottingham SM. A comparison of OEF and OIF veterans and Vietnam veterans receiving cognitive processing therapy. Journal of Traumatic Stress. 2010;23:25–32. doi: 10.1002/jts.20500. [DOI] [PubMed] [Google Scholar]
- Cigrang J, Peterson A, Schobitz R. Three American troops in Iraq: Evaluation of brief exposure therapy treatment for the secondary prevention of combat-related PTSD. Pragmatic Case Studies in Psychotherapy. 2005;1:1–25. [Google Scholar]
- Cloitre M. Effective psychotherapies for posttraumatic stress disorder: A review and critique. CNS Spectrum. 2009;14:32–43. [PubMed] [Google Scholar]
- Cooper NA, Clum BA. Imaginal flooding as a supplemental treatment for PTSD in combat veterans: A controlled study. Behavior Therapy. 1989;20:381–391. [Google Scholar]
- First MB, Spitzer RL, Gibbon M, Williams JBW. Structured clinical interview for DSM–IV Axis I disorders–Patient edition (SCIDI-I/P, Version 2.0) New York, NY: Biometrics Research Department, New York State Psychiatric Institute; 1996. [Google Scholar]
- Foa EB, Hembree EA, Rothbaum BO. Prolonged Exposure Therapy for PTSD: Therapist Guide. New York, NY: Oxford University Press; 2007. [Google Scholar]
- Fontana A, Rosenheck R. Treatment-seeking veterans of Iraq and Afghanistan: Comparison with veterans of previous wars. Journal of Nervous and Mental Disease. 2008;196:513–521. doi: 10.1097/NMD.0b013e31817cf6e6. [DOI] [PubMed] [Google Scholar]
- Glynn SM, Eth S, Randolph ET, Foy DW, Urbaitis M, Boxer L, Crothers J. A test of behavioral family therapy to augment exposure for combat-related posttraumatic stress disorder. Journal of Consulting and Clinical Psychology. 1999;67:243–251. doi: 10.1037//0022-006x.67.2.243. [DOI] [PubMed] [Google Scholar]
- Institute of Medicine. [Retrieved February 20, 2010];Treatment of PTSD: An assessment of the evidence. Report Brief, October, 2007. 2007 from http://www.iom.edu/~/media/Files/Report%20Files/2007/Treatment-of-PTSD-An Assessment-of-The-Evidence/PTSDReportBriefFINAL2.ashx. [Google Scholar]
- Keane TM, Fairbank JA, Caddell JM, Zimering RT. Implosive (flooding) therapy reduces symptoms of PTSD in Vietnam combat veterans. Behavior Therapy. 1989;20:245–260. [Google Scholar]
- Orsillo SM. Measures for acute stress disorder and posttraumatic stress disorder. In: Anthony MM, Orsillo SM, Roemer L, editors. Practitioner’s guide to empirically based measures of anxiety. New York, NY: Springer; 2001. pp. 255–307. [Google Scholar]
- Rauch SAM, Defever E, Favorite T, Duroe A, Garrity C, Martis B, Liberzon I. Prolonged exposure for PTSD in a veteran’s health administration PTSD clinic. Journal of Traumatic Stress. 2009;22:60–64. doi: 10.1002/jts.20380. [DOI] [PubMed] [Google Scholar]
- Rubin DB. Multiple imputation for nonresponse surveys. New York, NY: Wiley; 1987. [Google Scholar]
- Seal KH, Maguen S, Cohen B, Gima KS, Metzler TJ, Ren L, Marmar CR. VA Mental Health services utilization in Iraq and Afghanistan veterans in the first year of receiving new mental health diagnoses. Journal of Traumatic Stress. 2010;23:5–16. doi: 10.1002/jts.20493. [DOI] [PubMed] [Google Scholar]
- Steer RA, Clark DA. Psychometric characteristics of the Beck Depression Inventory-II with college students. Measurement and Evaluation in Counseling and Development. 1997;30:128–136. [Google Scholar]
- Tuerk PW, Yoder M, Grubaugh AL, Myrick H, Hamner M, Acierno R. Prolonged exposure therapy for combat-related posttraumatic stress disorder: An examination of treatment effectiveness for veterans of the wars in Afghanistan and Iraq. Journal of Anxiety Disorders. 2011;25:397–403. doi: 10.1016/j.janxdis.2010.11.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tuerk PW, Yoder M, Ruggiero KJ, Gros DF, Acierno R. A pilot study of prolonged exposure therapy for posttraumatic stress disorder delivered via telehealth technology. Journal of Traumatic Stress. 2010;23:116–123. doi: 10.1002/jts.20494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- U.S. Department of Veterans Affairs, & U.S. Department of Defense. VA/DoD clinical practice guidelines for the management of post-traumatic stress. Washington, DC: U.S. Department of Veterans Affairs & U.S. Department of Defense; 2010. [Google Scholar]