Abstract
Purpose
To evaluate the risk factors for overactive bladder (OAB) in a population aged 40 years and over in the community.
Materials and Methods
We conducted a community-based survey of OAB in a population aged 40 years and over in Guri City and Yangpyeong County, South Korea, by use of the overactive bladder symptom score (OABSS) questionnaire. A total of 926 subjects were included in the final analysis. The definition of OAB was more than 2 points for the urgency score and 3 points for the sum of scores. In addition, the subjects were asked about age, dwelling place, marital status, educational status, behavioral factors (smoking, drinking, etc), and medical history. Categorical variables were analyzed by using the logistic regression model and were adjusted for age by using the logistic regression model.
Results
Overall OAB prevalence was 14.1% (130/926), made up of 49/403 males (12.2%) and 81/523 females (15.5%). OAB prevalence increased with age (p<0.0001). Risk factors for OAB were educational status (age-adjusted p=0.0487), stroke (p=0.0414), osteoporosis (p=0.0208), asthma (p=0.0091), rhinitis (p=0.0008), and cataract. Other factors (dwelling place, marital status, smoking, drinking, hypertension, diabetes, hyperlipidemia, myocardial infarction, angina, tuberculosis, atopic dermatitis, hepatitis B, and depression) were not associated with OAB.
Conclusions
The prevalence of OAB in our study was about 14.1% and the risk factors for OAB were educational status, stroke, osteoporosis, asthma, rhinitis, and cataract. Knowledge of these risk factors may help in the diagnosis and treatment of OAB.
Keywords: Overactive bladder, Risk factors
INTRODUCTION
According to the International Continence Society (ICS), overactive bladder (OAB) is a condition characterized by frequency (>8 micturitions per day) and nocturia (waking one or more times at night to void) with or without urge incontinence (involuntary emptying of the contents of the bladder). Many epidemiological and clinical studies have shown that OAB affects the physical and mental health of patients and is an economic and social burden to patients [1,2]. Epidemiological and clinical studies have surveyed the symptoms and causes and the prevalence of OAB [3]. Estimates of OAB prevalence differ, but almost all studies have shown that its prevalence increases with age. There is also some evidence of an association with depression [1,2]. Many previous studies on OAB have been limited to the elderly or to subjects with incontinence [4-6]. We conducted a cross-sectional study of subjects aged over 40 years in an urban and a rural region to measure the prevalence of OAB in the community and assessed the risk factors for the condition.
MATERIALS AND METHODS
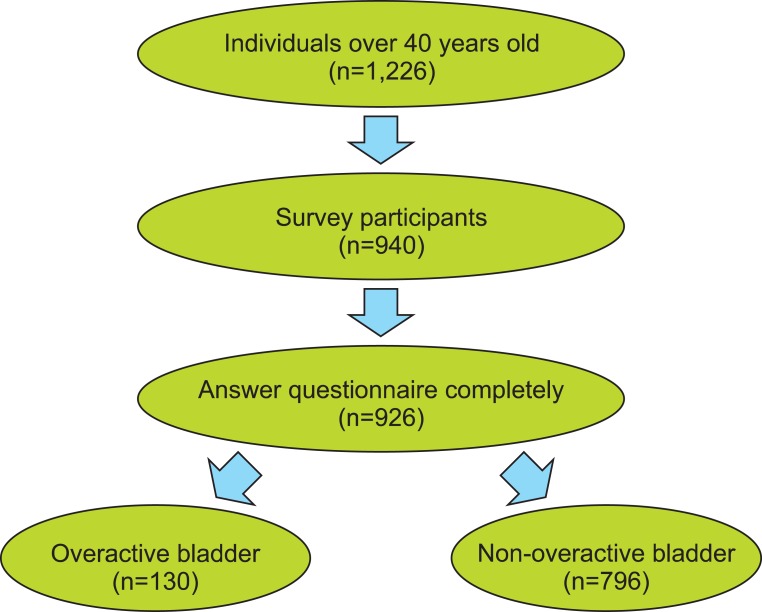
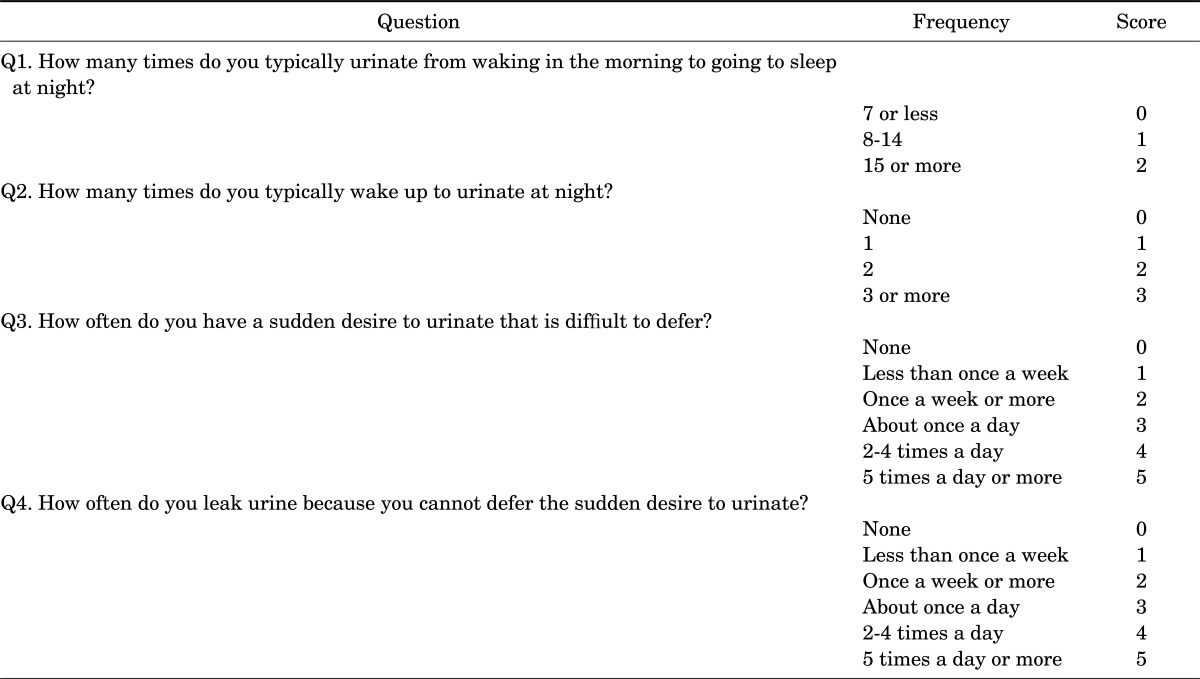
The study participants were 1,226 subjects aged over 40 years in Guri City and Yangpyeong County, South Korea, who were approached in October and November 2010. The response rate was 74.2% (940 responders out of 1,226), and a few participants with incomplete questionnaire were excluded (n=14). Therefore, a total of 926 subjects were included in the final analysis (Fig. 1). The survey involved face-to-face interviews, with fully informed consent. The protocol of this study was developed by the Department of Preventive Medicine, Hanyang University College of Medicine. The survey was conducted with the overactive bladder symptom score (OABSS) questionnaire (Table 1). OAB was defined according to the ICS as urgency with or without urge incontinence, and usually with frequency and nocturia. In this study, OAB was defined as over 2 points for the urgency score and 3 points for the sum of total scores in the OABSS questionnaire. The matters covered by the questionnaire are listed in Table 2. They included dwelling place (rural or urban area), marital status, education, behavioral factors (smoking, drinking, etc), and self-reported medical history, including hypertension, stroke, myocardial infarction, angina, hyperlipidemia, diabetes, osteoporosis, arthritis, tuberculosis, asthma, rhinitis, atopic dermatitis, cataract, hepatitis B, and depression. The individuals surveyed were divided into three groups in relation to smoking: a never smoking group (no history of smoking), an ex-smoking group, and a current smoking group. In the same way, individuals were classified in three categories with regard to drinking: the never-drinkers (no history of drinking), the ex-drinkers, and the current drinkers.
FIG. 1.
Flow diagram of the study.
TABLE 1.
Overactive bladder symptom score (OABSS)
OAB, sum score≥3 and score of Q2≥2; Mild-OAB, sum score≤5; Moderate-OAB, 6≤sum score≤11; Severe-OAB, sum score≥12.
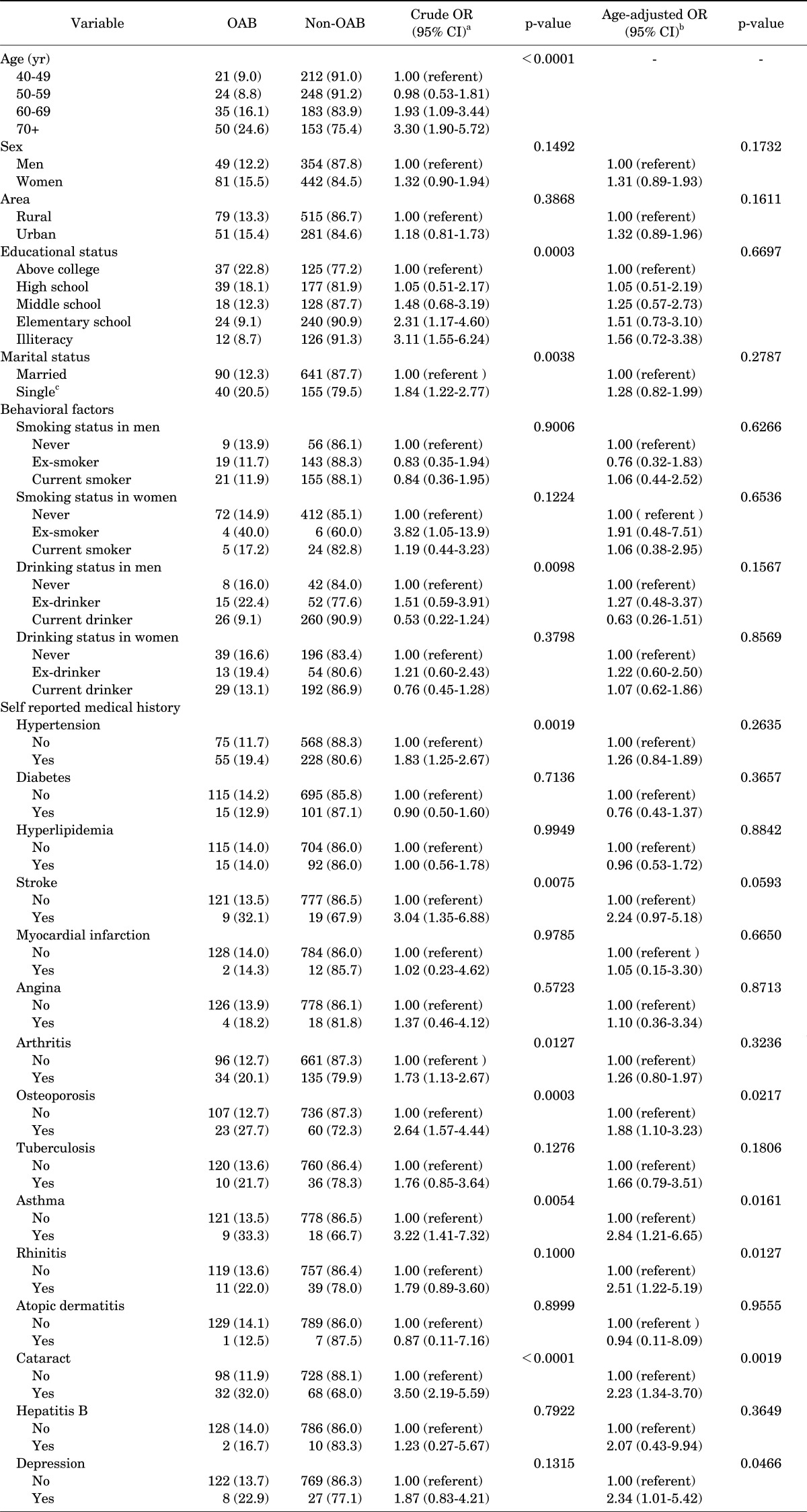
TABLE 2.
Risk factors for overactive bladder (OAB)
OAB, overactive bladder; OR, odds ratio; CI, confidence interval.
a:Logistic regression model, b:Logistic regression model adjusted for age (continuous), c:Single, widowed, divorced or separated, never married.
Categorical variables were analyzed by using a logistic regression model and were adjusted for age by using a logistic regression model. Statistical significance was considered established at the level of an alpha error of 0.05. Statistical analysis was performed with SAS ver. 9.1 (SAS Institute Inc., Cary, NC, USA).
RESULTS
The characteristics of the subjects are shown in Table 2. Of the 926 subjects, 403 subjects (43.52%) were male and 81 were female (15.5%). The subjects' mean age was 75.4±4.5 years. A total of 130 subjects (14.1%) were diagnosed with OAB, including 49 males (12.2%) and 81 females (15.5%). A total of 694 of the responders lived in the rural area (Yangpyeong County), and 79 of them were diagnosed with OAB; 332 responders lived in the urban area (Guri City), and 51 of them were diagnosed with OAB (p=0.20). The distribution of OAB among individuals with various other characteristics is presented in Table 2.
According to educational status, the prevalence of OAB was below 10% in those with an educational status of high school graduate or above; in those with less than a high school level of eduction, the prevalence of OAB was over 90%.
There were 28 people with a history of stroke, and the prevalence of OAB with a history of stroke was 9/28 (32.1%). There were 83 patients with a history of osteoporosis, and the prevalence of OAB with a history of osteoporosis was 23/83 (27.7%). There were 27 patients with a history of asthma, and the prevalence of OAB with a history of asthma was 9/27 (33.3%). There were 100 subjects with cataract, of whom 32 (32.0%) met the criteria for OAB. The prevalence of OAB was not related to other risk factors except for those mentioned above.
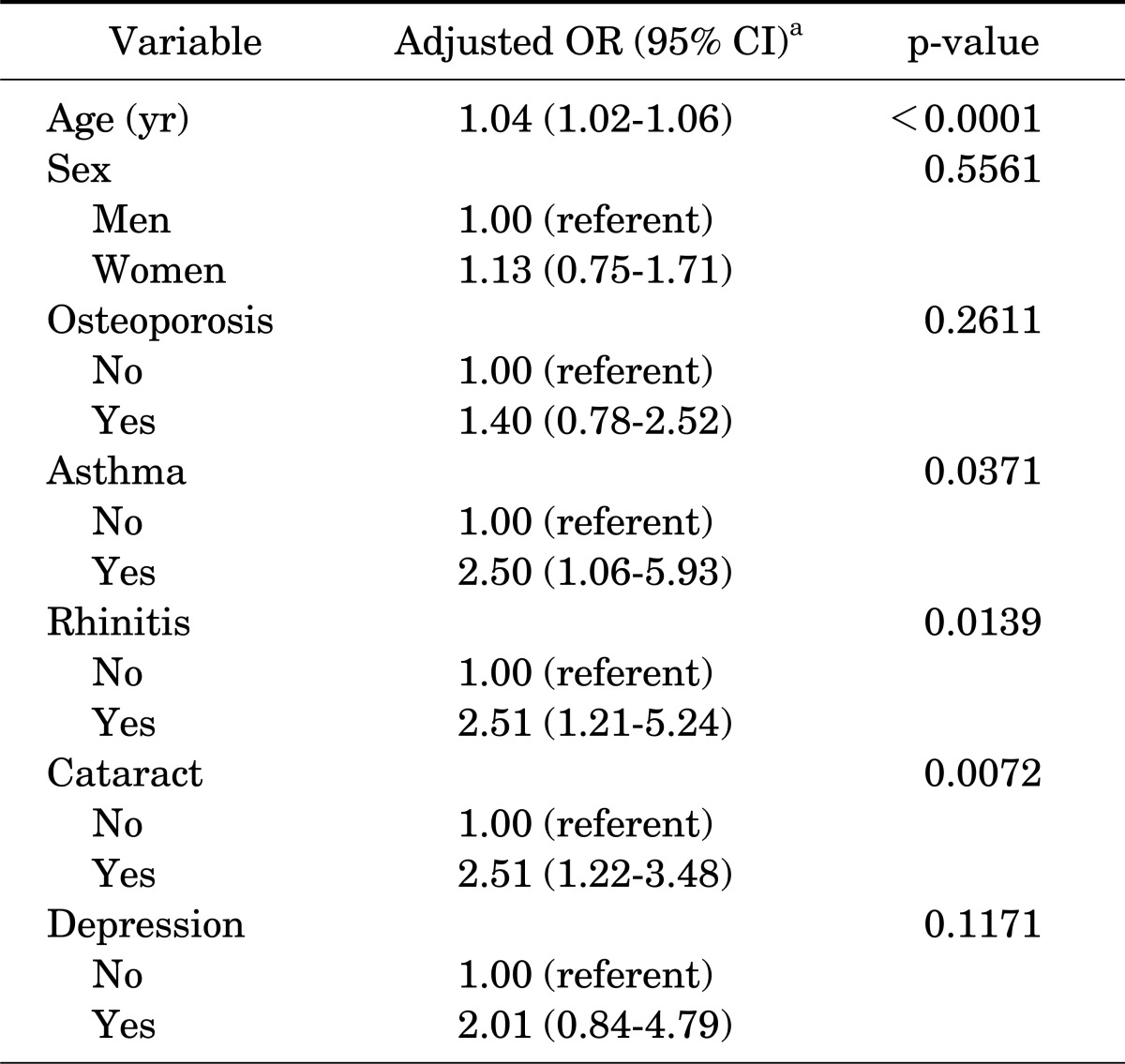
The risk of OAB increased with age (p<0.0001). We used age-adjusted p-values to assess the risk factors for OAB. Educational status (p<0.0487), stroke (p<0.0414), osteoporosis (p<0.0208), asthma (p<0.0091), rhinitis (p <0.0150), and cataract (p<0.0008) were significantly associated with OAB (Table 3). Other factors (dwelling place, marital status, smoking, drinking, hypertension, diabetes, hyperlipidemia, myocardial infarction, angina, tuberculosis, atopic dermatitis, hepatitis B, and depression) were not significantly associated with OAB.
TABLE 3.
Age adjusted risk factors for OAB
OAB, overactive bladder; OR, odds ratio; CI, confidence interval.
a:Logistic regression model adjusted for age (continuous), sex, medical history of osteoporosis, asthma, rhititis, cataract, and depression.
DISCUSSION
The prevalence of OAB varies from country to country. In Europe, the prevalence of OAB reaches 16.6%, and increases to 22.1 to 41.9% in people over 70 years of age [7-10]. As part of the National Overactive Bladder Evaluation Program in the United States, a large-scale telephone survey was conducted of 5,204 respondents of both sexes aged ≥18 years. The total prevalence of OAB reached 857/5204 (16.5%) and attained 25% or more in people aged over 65. The prevalence of OAB with urge incontinence was 319/857 (6.1%) and the prevalence of OAB without urge incontinence was 538/857 (10.4%) [2]. In addition, in Japan, many epidemiologic surveys and clinical studies have shown that the prevalence reaches 12.4%; in individuals aged 70 to 79 years, it reaches 22.6%, and in those over 80 it reaches 36.8% [11-13]. Other studies have also examined the risk factors for OAB. The prevalence of OAB was found to increase with age in countries including Korea [14-16]. In our study, OAB prevalence was a little higher than in the Korean European Prospective Investigation into Cancer and Nutrition (EPIC) study. However, the study populations differed slightly between the Korean EPIC study and our study; our study population consisted of community-based subjects. In particular, the Korean EPIC study showed that storage lower urinary tract symptoms (LUTS) were more prevalent than voiding or post-micturition LUTS. In our study also, storage LUTS were more prevalent than other voiding symptoms. We obtained the same result for age dependence and also identified other risk factors, though age was the most important risk factor. The differences in OAB prevalence between countries may be related to cultural factors including race and cultural circumstances [17].
Stewart et al. [2] showed that the prevalence of OAB without urge incontinence increased more steeply with age in men than in women and was significantly different by sex. In men, OAB without urge incontinence increased approximately three-fold, whereas OAB without urge incontinence gradually increased in women less than 44 years of age and reached a plateau in women over the age of 44 years. In our study, the prevalence of OAB by sex was not significantly different. This was probably because of differences between the populations studied in the United States and those studied in Korea.
Studies of other risk factors in Japanese persons over 70 found that depression (multiple adjusted odds ratio=2.07), a recent drinking history, and obesity (body mass index) were significantly linked to the prevalence of OAB [3]. In our study these variables were not risk factors, probably because of differences between the populations studied in Japan and in Korea, especially in terms of age. In our study, the age-adjusted p-value for depression was 0.0671. These data include only a history of diagnosis of depression. These data may therefore be an underestimate because they did not include depressed mood.
Other studies have examined the relationship between OAB and lifestyle, especially smoking, alcohol use, and diet, and reported that controlling these factors improved or prevented OAB [18,19]. In the present study, however, residential area, marital status, smoking, alcohol consumption, hypertension, diabetes, hyperlipidemia, myocardial infarction, angina, tuberculosis, atopic dermatitis, and hepatitis B were found to be unrelated to the risk of OAB. This difference may be due to differences in diet and national make-up between the groups surveyed [17].
Previous studies have, like ours, found a clear relationship between lower educational status and risk of OAB [1]. There is also a close relationship between socioeconomic status and educational level and it is the former that probably relates most directly to the risk of OAB. Persons with a higher educational level are more likely to seek better health behaviors and may have healthier lifestyles, whereas persons with a lower educational level may have a higher prevalence of smoking, poor diet, more labor, and exposure to toxins.
Our study had some limitations. The first was the small size of the study population. The prevalence of OAB in the general population is sizeable; considering the odd ratio, it could be over-estimated. Second, the OAB group identified by the questionnaire did not receive any clinical follow-up. Despite these limitations, however, our study has clarified the prevalence of OAB in Korea and has identified several associated risk factors.
This study aimed at surveying the prevalence of OAB in the community and the multiple risk factors for OAB. Analyzing the risk factors for OAB may help in the diagnosis of OAB. Use of these risk factors may be helpful for creating new criteria for OAB with multiple risk factors.
CONCLUSIONS
The prevalence of OAB in the community in Korea was 14.1% and the identified risk factors for OAB were age, educational status, stroke, osteoporosis, asthma, rhinitis, and cataract. Knowledge of these risk factors should facilitate the diagnosis and also the treatment of OAB.
ACKNOWLEDGEMENTS
This work was supported by the research fund of Hanyang University Institute of Aging Society in 2010.
Footnotes
The authors have nothing to disclose.
References
- 1.Wang Y, Xu K, Hu H, Zhang X, Wang X, Na Y, et al. Prevalence, risk factors, and impact on health related quality of life of overactive bladder in China. Neurourol Urodyn. 2011;30:1448–1455. doi: 10.1002/nau.21072. [DOI] [PubMed] [Google Scholar]
- 2.Stewart WF, Van Rooyen JB, Cundiff GW, Abrams P, Herzog AR, Corey R, et al. Prevalence and burden of overactive bladder in the United States. World J Urol. 2003;20:327–336. doi: 10.1007/s00345-002-0301-4. [DOI] [PubMed] [Google Scholar]
- 3.Ikeda Y, Nakagawa H, Ohmori-Matsuda K, Hozawa A, Masamune Y, Nishino Y, et al. Risk factors for overactive bladder in the elderly population: a community-based study with face-to-face interview. Int J Urol. 2011;18:212–218. doi: 10.1111/j.1442-2042.2010.02696.x. [DOI] [PubMed] [Google Scholar]
- 4.Ueda T, Tamaki M, Kageyama S, Yoshimura N, Yoshida O. Urinary incontinence among community-dwelling people aged 40 years or older in Japan: prevalence, risk factors, knowledge and self-perception. Int J Urol. 2000;7:95–103. doi: 10.1046/j.1442-2042.2000.00147.x. [DOI] [PubMed] [Google Scholar]
- 5.Grimby A, Milsom I, Molander U, Wiklund I, Ekelund P. The influence of urinary incontinence on the quality of life of elderly women. Age Ageing. 1993;22:82–89. doi: 10.1093/ageing/22.2.82. [DOI] [PubMed] [Google Scholar]
- 6.Diokno AC, Brock BM, Brown MB, Herzog AR. Prevalence of urinary incontinence and other urological symptoms in the noninstitutionalized elderly. J Urol. 1986;136:1022–1025. [PubMed] [Google Scholar]
- 7.Irwin DE, Milsom I, Hunskaar S, Reilly K, Kopp Z, Herschorn S, et al. Population-based survey of urinary incontinence, overactive bladder, and other lower urinary tract symptoms in five countries: results of the EPIC study. Eur Urol. 2006;50:1306–1314. doi: 10.1016/j.eururo.2006.09.019. [DOI] [PubMed] [Google Scholar]
- 8.Irwin DE, Milsom I, Kopp Z, Abrams P EPIC Study Group. Symptom bother and health care-seeking behavior among individuals with overactive bladder. Eur Urol. 2008;53:1029–1037. doi: 10.1016/j.eururo.2008.01.027. [DOI] [PubMed] [Google Scholar]
- 9.Irwin DE, Milsom I, Kopp Z, Abrams P, Cardozo L. Impact of overactive bladder symptoms on employment, social interactions and emotional well-being in six European countries. BJU Int. 2006;97:96–100. doi: 10.1111/j.1464-410X.2005.05889.x. [DOI] [PubMed] [Google Scholar]
- 10.Milsom I, Abrams P, Cardozo L, Roberts RG, Thuroff J, Wein AJ. How widespread are the symptoms of an overactive bladder and how are they managed? A population-based prevalence study. BJU Int. 2001;87:760–766. doi: 10.1046/j.1464-410x.2001.02228.x. [DOI] [PubMed] [Google Scholar]
- 11.Homma Y, Yamaguchi O, Hayashi K Neurogenic Bladder Society Committee. An epidemiological survey of overactive bladder symptoms in Japan. BJU Int. 2005;96:1314–1318. doi: 10.1111/j.1464-410X.2005.05835.x. [DOI] [PubMed] [Google Scholar]
- 12.Homma Y, Yamaguchi O, Hayashi K Neurogenic Bladder Society Committee. Epidemiologic survey of lower urinary tract symptoms in Japan. Urology. 2006;68:560–564. doi: 10.1016/j.urology.2006.03.035. [DOI] [PubMed] [Google Scholar]
- 13.Homma Y, Yoshida M, Seki N, Yokoyama O, Kakizaki H, Gotoh M, et al. Symptom assessment tool for overactive bladder syndrome: overactive bladder symptom score. Urology. 2006;68:318–323. doi: 10.1016/j.urology.2006.02.042. [DOI] [PubMed] [Google Scholar]
- 14.Yu HJ, Liu CY, Lee KL, Lee WC, Chen TH. Overactive bladder syndrome among community-dwelling adults in Taiwan: prevalence, correlates, perception, and treatment seeking. Urol Int. 2006;77:327–333. doi: 10.1159/000096337. [DOI] [PubMed] [Google Scholar]
- 15.Zhang W, Song Y, He X, Huang H, Xu B, Song J. Prevalence and risk factors of overactive bladder syndrome in Fuzhou Chinese women. Neurourol Urodyn. 2006;25:717–721. doi: 10.1002/nau.20293. [DOI] [PubMed] [Google Scholar]
- 16.Lee YS, Lee KS, Jung JH, Han DH, Oh SJ, Seo JT, et al. Prevalence of overactive bladder, urinary incontinence, and lower urinary tract symptoms: results of Korean EPIC study. World J Urol. 2011;29:185–190. doi: 10.1007/s00345-009-0490-1. [DOI] [PubMed] [Google Scholar]
- 17.Goldstein LB, Adams R, Alberts MJ, Appel LJ, Brass LM, Bushnell CD, et al. Primary prevention of ischemic stroke: a guideline from the American Heart Association/American Stroke Association Stroke Council: cosponsored by the Atherosclerotic Peripheral Vascular Disease Interdisciplinary Working Group; Cardiovascular Nursing Council; Clinical Cardiology Council; Nutrition, Physical Activity, and Metabolism Council; and the Quality of Care and Outcomes Research Interdisciplinary Working Group. Circulation. 2006;113:e873–e923. doi: 10.1161/01.STR.0000223048.70103.F1. [DOI] [PubMed] [Google Scholar]
- 18.Dallosso HM, Matthews RJ, McGrother CW, Donaldson MM, Shaw C Leicestershire MRC Incontinence Study Group. The association of diet and other lifestyle factors with the onset of overactive bladder: a longitudinal study in men. Public Health Nutr. 2004;7:885–891. doi: 10.1079/phn2004627. [DOI] [PubMed] [Google Scholar]
- 19.Dallosso HM, McGrother CW, Matthews RJ, Donaldson MM Leicestershire MRC Incontinence Study Group. The association of diet and other lifestyle factors with overactive bladder and stress incontinence: a longitudinal study in women. BJU Int. 2003;92:69–77. doi: 10.1046/j.1464-410x.2003.04271.x. [DOI] [PubMed] [Google Scholar]