Abstract
Study design: Systematic review
Objective: To compare the safety and effectiveness of fusion versus denervation for chronic sacroiliac joint pain after failed conservative management.
Summary of background: Methods of confirming the sacroiliac joint as a pain source have been extensively studied and reported in the literature. After confirmation of the origin of the pain by positive local anesthetic blocks, chronic sacroiliac joint pain is usually managed with a combination of medication, physical therapies, and injections. We have chosen to compare two alternative treatments for sacroiliac pain that was refractory to conservative therapies.
Methods: A systematic review of the English-language literature was undertaken for articles published between 1970 and June 2010. Electronic databases and reference lists of key articles were searched to identify studies evaluating fusion or denervation for chronic sacroiliac joint pain after failed conservative management. Studies involving only conservative treatment or traumatic onset of injury were excluded. Two independent reviewers assessed the level of evidence quality using the grading of recommendations assessment, development and evaluation (GRADE) system, and disagreements were resolved by consensus.
Results: We identified eleven articles (six fusion, five denervation) meeting our inclusion criteria. The majority of patients report satisfaction after both treatments. Both treatments reported mean improvements in pain and functional outcome. Rates of complications were higher among fusion studies (13.7%) compared to denervation studies (7.3%). Only fusion studies reported infections (5.3%). No infections were reported among denervation patients. The evidence for all findings were very low to low; therefore, the relative efficacy or safety of one treatment over another cannot be established.
Conclusions: Sacroiliac joint fusion or denervation can reduce pain for many patients. Whether a true arthrodesis of the joint is achieved by percutaneous techniques is open to question and whether denervation of the joint gives durable pain relief is not clear. Further comparative studies of these two techniques may provide the answers.
STUDY RATIONALE AND CONTEXT
The sacroiliac joint as a source of low back pain has been extensively studied and reported in the literature. Pathological conditions which can affect a sacroiliac joint include degenerative and inflammatory arthritis, posttraumatic and postpartum instability, infection and neoplastic disease. Various other conditions which might cause sacroiliac joint pain include leg-length discrepancy, hip arthritis, and lumbosacral fusions for low back pain, as well as iatrogenic violation of the joint following autologous posterior iliac crest bone graft harvest. Numerous physical tests have been described to isolate the sacroiliac joint as the source of low back pain but none have proved reliable. The most accepted test for sacroiliac pain is temporary relief of the pain after injection of local anaesthetic agents into the joint under fluoroscopic* control. Conservative treatment of chronic sacroiliac pain has consisted of analgesic and antiinflammatory medication, physical therapies and several types of injection techniques. More invasive techniques involve fusion of the joint or denervation by ablative therapy. We have chosen to focus our review on these two techniques of long-term pain relief after failure of conservative treatment.
OBJECTIVES
To compare the effectiveness and safety of fusion versus denervation for chronic sacroiliac joint pain after failed conservative management.
MATERIALS AND METHODS
Study design: Systematic review
Sampling:
Search: PubMed, Cochrane Collaboration Database, and National Guideline Clearinghouse Databases; bibliographies of key articles
Dates searched: 1970–June 2010.
Inclusion criteria: (1) chronic sacroiliac joint pain, (2) adults 18 years and older, (3) studies involving initial failed conservative treatment
Exclusion criteria: (1) conservative treatment only, (2) unclear whether subjects had first undergone conservative treatment, (3) trauma, (4) less than five subjects per treatment, (5) less than 6-month follow-up
Outcomes: patient satisfaction, pain, functional outcomes, wound infection, and complications (health related or surgery specific)
Analysis: descriptive statistics pooling rates across studies
Details about methods can be found in the web appendix at www.aospine.org/ebsj
RESULTS
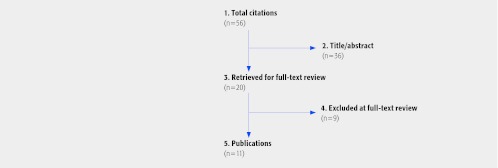
We identified eleven articles meeting our inclusion criteria (Fig 1). Six studies evaluated fusion for sacroiliac joint pain (n = 95 patients). Five studies evaluated denervation for sacroiliac joint pain (n = 68 patients). All studies were case series evaluating a single treatment. No cohort studies comparing one treatment to the other in the same patient population was identified, making statements regarding relative efficacy impossible. Further, follow-up times for denervation studies (6–12 months) were much shorter than fusion studies (17–69 months). All studies involved subjects who had failed other conservative management. A diagnosis of sacroiliac joint pain in all studies was confirmed by injection. Most often an injection with a solution used to reproduce exact pain pattern was followed by a local anesthetic for pain relief. Prior to their denervation treatment all patients in the denervation cohort underwent physical therapy and medical therapy. Some patients also underwent injection therapy or had previous back surgery. Many patients in the fusion cohort had previously undergone lumbar fusion and other types of back surgery.
Fig 1.
Flow chart showing results of literature search
Outcomes associated with fusion versus denervation for treatment of chronic sacroiliac pain (Tables 1,2,3, Figs 2,3)
Table 1. Common outcomes of studies evaluating fusion versus denervation for treatment for sacroiliac joint pain.
| N = 163 | Fusion N = 95 |
Denervation N = 68 |
||||||
|---|---|---|---|---|---|---|---|---|
| Outcomes | Studies (n) | Patients (n) | Results (mean) | Results (range) | Studies (n) | Patients (n) | Results (mean) | Results (range) |
| Patient satisfaction | 4 | 59 | 57.6% | 18%–100% | 1 | 9 | 89% | 89% |
| Infection | 4 | 57 | 5.3% | 0%–11% | 5 | 68 | 0% | 0% |
| All complications* | 6 | 95 | 13.7% | 0%–41% | 5 | 68 | 7.3% | 0%–33% |
Excluding infection
Table 2. Characteristics of studies of fusion for sacroiliac joint pain.
| Author (year) |
Study design | Study population |
Previous treatment n (%) |
Confirmed diagnosis | Fusion description | Follow-up mean (range) | Outcomes |
|---|---|---|---|---|---|---|---|
| Wise (2008) | Case series | N = 13 patients Unilateral (n = 7) Bilateral (n = 6) Age: 53.1 (45–62) Male: 7.7% |
Failed conservative therapy: 13 (100) Lumbar fusion: 8 (62) Open sacroiliac arthrodesis on contralateral side: 1 (8) |
Fluoroscopically guided intraarticular injections of local anesthetic and corticosteroid resulting in 2 or more hours of pain relief. | Percutaneously inserted fusion cages filled with morphogenic protein | 29.5 months (24–35) |
Fusion rate: n = 17/19 (89%) VAS* for low back pain: improved average 4.9 VAS for leg pain: improved average 2.4 VAS for dyspareunia: improved average 2.6 Satisfaction: n = 10/13 (77%) Complications: No infections No neurovascular complications |
| Schütz (2006) | Case series | N = 17 patients Unilateral (n = 0) Bilateral (n = 17) Age: 43.2 (22–76) Male: 29.4% |
Failed conservative therapy: 17 (100) Previous lumbar surgery: 10 (59) Previous sacroiliac joint surgery: 1 (6) |
Fluoroscopically guided selective anesthetic infiltration:14 (82%). Technetium bone-scan: 5 (29%). For further differentiation of lumbosacral and sacroiliac origin of pain, selective immobilization of lumbar, lumbosacral, sacroiliac segments using temporary external fixator: 4 (24%) |
Internal fixation and decortication of the sacroiliac joint, using a separate approach to each joint. Local bone grafting performed | 39 months (NR†) |
Fusion rate: – Definite bony fusion: n = 6 (35.3%) – Questionable fusion: n = 4 (23.5%) – Nonunion with instability: 7 (41.2%) Pain at follow-up: – Pain free: 1 (5.8%) – Mild, intermittent: 2 (11.8%) – Marked: 8 (47.0%) –Severe, intolerable: 6 (35.3%) Further surgery: n = 11 (64.7%) Satisfaction: n = 3 (17.6%) Complications: NR |
| Khurana (2009) | Case series | N = 15 patients Unilateral (n = 11) Bilateral (n = 4) Age: 48.7 (37–62) Male: 26.7% |
Previous spinal surgery: 6 (40) | Injection of local anesthetic and steroid under image intensifier control | Percutaneously inserted hollow modular anchorage screws filled with demineralized bone matrix | 17 months (9–39) |
Fusion rate: n = 15/15 (100%) SF-36 physical function: improved from 37 (23–51) to 80 (67–92) SF-36 general health: improved from 53 (34-73) to 86 (70-98) Majeed score: improved from 37 (18–54) to 79 (62–96) Majeed score excellent results: 13 (86.7) Further surgery: n = 0 (0) Complications: – No infections – No neurological complications – No cases of implant failure |
| Al-khayer (2008) | Case series | N = 9 patients Unilateral (n = 6) Bilateral (n = 3) Age: 42.4 (35–56) Male: 0% |
Failed rigorous conservative therapy: 9 (100) | Temporary pain relief with sacroiliac joint block | Percutaneously inserted hollow modular anchorage screws filled with demineralized bone matrix | 40 months (24–70) |
Fusion rate: n = 9/9 (100%) Owestry disability index: improved from 59 (34–70) to 45 (28–60) VAS for low back pain: improved from 8.1 (7–9) to 4.6 (3–7) VAS for overall satisfaction: 6.8 (5–8) Satisfaction with procedure: n = 9 (100) Complications: –Deep wound infection: n = 1 (11%) – No loosening, screw failure, or breakage – No nonunion |
| Buchowski (2005) | Case series | N = 20 patients Unilateral (NR) Bilateral (NR) Age: 45.1 (21–66) Male: 15.0% |
Failed conservative therapy (physical therapy, pain meds, lifestyle modification): 20 (100) Previous spine surgery: 15 (75) Previous fusion of sacrum: 8 (40) |
Pain relief with intraarticular sacroiliac joint injections under fluoroscopic guidance | Used modified Smith-Petersen technique | 69 months (24–108) |
Fusion rate: n = 17/20 (85%) Revision surgery for nonunion: n = 3 (15%) Satisfaction with procedure: n = 12 (60%) SF-36: statistically significant improvement made in 8 of 10 outcome categories AAOS modems instrumentscores: statistically significant improvement found in satisfaction with symptoms, neurogenic symptoms index, and pain/disability index Complications: – Deep wound infection: n = 2 (10%) – Pseudarthrosis: n = 3 (15%) – Painful hardware: n = 1 (5%) |
| Waisbrod (1987) | Case series | N = 21 patients Unilateral (n = 20) Bilateral (n = 1) Age: 42.0 (20–58) Male: 14.3% |
Previous operations for complaints: – discectomy: 2 (10) – posterolateral spinal fusion: 5 (24) – bilateral total hip replacement: 2 (10) |
Injection of 10% NaCl solution reproducing exact pain pattern patient complains of. Further injection of local anesthetic relieves pain for duration of drug’s effect. | Articular surfaces completely excised. Corticocancellous bone graft taken from iliac crest and/or tricalcium-phosphate ceramic blocks interposed under pressure between denuded cancellous bone. | 30 months (12–55) |
Satisfactory results (pain reduced at least 50%): n = 11/22 (50.0%) Nonunion: n = 2/22 (9.1%) Complications: NR |
VAS = visual analog scale
NR = not reported
Table 3. Characteristics of studies of denervation for sacroiliac joint pain.
| Author (year) |
Study design | Study population |
Previous treatment | Confirmed diagnosis | Denervation description |
Follow-up mean (range) | Outcomes |
|---|---|---|---|---|---|---|---|
| Cohen (2008) | Randomized controlled trial | N = 14 patients Unilateral (n = 13) Bilateral (n = 1) Age: 51.9 (27–75) Male: 35.7% n = 14 placebo denervation |
Physical therapy, pharmacotherapy, back surgery | Injections containing 2 mL of 0.5% bupivacaine and 1 mL of 40 mg/mL of depo-methylprednisolone | Cooled radiofrequency (RF) denervation of L4–5 primary dorsal rami and S1–3 lateral branches performed only after + 75% pain relief with L4–5 and S1–3 lateral branch blocks. | 6 months (NR*) |
Numerical rating score (NRS) for pain: improved average of 3.5 points from baseline (6.1 ± 1.8) to (2.6 ± 2.2) Oswestry disability index: improved average of 14.5 points from baseline (37.1 ± 10.6) to (22.6 ± 10.6) Global perceived effect: 7/14 (50%) at 6 months Medication reduction: 5/14 (36%) at 6 months Complications: – Only procedure-related pain and/or temporary neuritis reported – Transient non-painful buttock parasthesias (n = 1) |
| N = 11/14 of placebo patients crossed over to radiofrequency denervation after failed placebo denervation at 3 months Age: 51.8 (31–74) Male: 42.8% |
Physical therapy, pharmacotherapy, back surgery, placebo denervation | Injections containing 2 mL of 0.5% bupivacaine and 1 mL of 40 mg/ mL of depo-methylprednisolone | Conventional (non-cooled) RF denervation of L4–5 primary dorsal rami and S1–3 lateral branches performed only after failed placebo denervation | 6 months (NR) |
NRS for pain: improved average of 3.4 points from baseline (6.5 ± 1.9) to 6 months post-denervation (3.1 ± 2.1) Oswestry disability index: improved average of 23.6 points from baseline (47.9 ± 9.3) to 6 months post denervation (24.3 ± 21.0) Global perceived effect: 5/11(46%) at 6 months Medication reduction: 3/11 (27%) at 6 months |
||
| Cohen (2003) | Randomized controlled trial | N = 9 patients Unilateral (NR) Bilateral (NR) Age: 50.0 (31–81) Male: 53.9% |
Physical therapy, previous blocks, back surgery, pain medicine management | Injections performed with 80 mg triamcinolone acetonide steroid and 1 to 3 mL 0.5% ropivacaine or 0.5% bupivacaine | RF denervation of L4–5 primary dorsal rami and S1–3 lateral branches performed only after >50% pain relief with L4–5 and S1–3 lateral branch blocks | 9 months (NR) |
Visual analog scale (VAS) for pain: improved average of 4.1 points from baseline (6.3) to 9 months post denervation (2.2) Complications: No complications with any of the procedures |
| Yin (2003) | Case series | N = 14 patients Unilateral (NR) Bilateral (NR) Age: 53.7 (35–79) Male: 28.6% |
Physical therapy, medical therapy, manual therapy, home-based flexibility and exercise programs, TENS, anesthetic injections, back surgery (lumbar discectomy, fusion or laminectomy) | Two separate deep interosseous ligamentous injections with 5 mL of 0.5% bupivacaine containing 4 mg/mL of triamcinolone | Sensory stimulation-guided RF denervation of L5 posterior sensory branch and the lateral branches of S1–3 | 6 months (NR) |
Visual integer pain score (VIPS): 64% successful outcome (defined as 60%
consistent subjective relief and greater than a 50% consistent decrease in VIPS,
maintained for at least 6 months) Complications: – No identifiable surgical complications – Cutaneous numbness over one buttock lasting 6 months (n = 1) – Most patients with transient buttock cutaneous dysesthesia – No bowel or bladder dysfunction – No postprocedure infections |
| Burnham (2007) | Case series | N = 9 patients Unilateral (n = 8) Bilateral (n = 1) Age: 54.6 (38–82) Male: 22.2% |
Back exercises, manual therapy, physical therapy, medical therapy, injections | Local anesthetic joint block | RF denervation of posterior sensory nerves | 12 months (NR) |
Patient satisfaction: 8/9 (89%) NRS for pain: improved average of 3.5 points from baseline (mean = 8) to 12 months post-denervation (mean = 4.5) Revised Oswestry disability index: improved average of 18 points from baseline (mean = 56) to 12 months postdenervation (mean = 38) Complications: – Numbness and itchiness of skin overlying treated sacroiliac joint (n = 3) |
| Vallejo (2006) | Case series | N = 22 patients Unilateral (NR) Bilateral (NR) Age: 55.9 ( ± 14) Male: 18.2% |
Physical therapy, medical therapy | Two or more fluoroscopically guided injections of corticosteroid/local anesthetic | Pulsed RF denervation of medial branch of L4, posterior rami of L5, and the lateral branches of S1–2. | 6 months (NR) |
VAS pain score: improved average of 4.9 points from baseline (7.6 ± 1.7) to 6 months postdenervation (2.7 ± 1.8) (P < .0001) FACIT quality of life scores: – Physical well-being: baseline (1.6 ± 0.7) and 6 months post-denervation (1.1 ± 0.5) (P< .0001) – Social-well being: baseline (3.1 ± 0.9) and 6 months post-denervation (3.2 ± 0.9) (P = .039) – Emotional well-being: baseline (1.3 ± 0.5) and 6 months post-denervation (1.0 ± 0.4) (P = .014) – Functional well-being: baseline (1.4 ± 0.8) and 6 months post-denervation (2.1 ± 1.0) (P < .0001) Complications: No complications directly or indirectly related to procedure |
NR = not reported
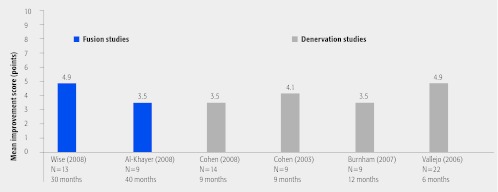
Fig 2.
Mean visual analog scale or numeric rating scale improvements after fusion (blue) or denervation (grey) among all studies measuring these outcomes
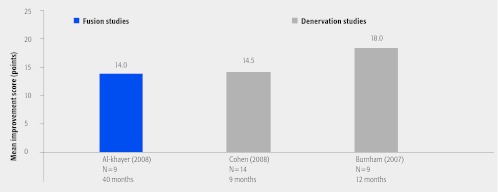
Fig 3.
Oswestry disability index improvements after fusion (blue) or denervation (grey) among all studies measuring these outcomes
The majority of fusion studies (n = 4) reported patient satisfaction as an outcome 1,2,3,4. The mean rate of patient satisfaction was 57.6% (range, 18%–100%) among 59 subjects. Only one denervation study reported patient satisfaction. There was an 89% patient satisfaction rate out of nine subjects 5 (Table 1).
The majority of denervation studies (n = 4) and two fusion studies reported pain improvement as an outcome using a visual analog or numeric rating scale to measure change from pre to posttreatment 1,3,5,6,7,8. All studies reported a mean improvement (range, 3.5–4.9 points) among subjects (Fig 2).
Two denervation studies and one fusion study reported a change in Oswestry disability index scores from pre to posttreatment 3,5,6. All studies reported a mean improvement (range, 14–18 points) (Fig 3).
Complications and infections associated with fusion and denervation for treatment of chronic sacroiliac pain (Table 1)
The pooled infection rate among fusion studies (n = 57 patients) was 5.3% and denervation studies (n = 68 patients) was 0% 1,3,4,5,6,7,8,9,10 (Table 1).
All studies reported general health or treatment specific complications 1,2,3,4,5,6,7,8,9,10,11 (Table 1). The pooled complication rate (excluding infections) among fusion studies (n = 95 patients) was 13.7% and denervation studies (n = 68 patients) was 7.3%. Fusion studies reported nonunion, pseudarthrosis and painful hardware as complications (excluding infection) while denervation studies reported transient buttock parasthesias, temporary neuritis, and numbness and itchiness of skin overlying treated sacroiliac joint.
EVIDENCE SUMMARY
Table 4.
| Outcomes | Strength of evidence | Conclusions/comments | |
|---|---|---|---|
| Question 1: To compare the effectiveness of fusion versus denervation for chronic sacroiliac joint pain after failed conservative management | |||
| 1. Patient satisfaction | Fusion | The majority of patients report satisfaction after both treatments. The rate was higher among denervation subjects; however, this was based on one study with nine subjects. | |
| Denervation | |||
| 2. Improvement in pain | Fusion | Both treatments rendered mean improvements in pain of 3.5–4.9 points on a 10-point scale among studies reporting this outcome; however, only two studies reported this outcome for fusion. | |
| Denervation | |||
| 3. Improvement in functional outcome | Both treatments rendered an improvement in functional outcome based on the Oswestry disability score of 14.0–18.0 points; however, only one fusion study and two denervation studies reported this outcome. | ||
| Question 2: To compare the safety of fusion versus denervation for chronic sacroiliac joint pain after failed conservative management | |||
| 4. Complications | Rates of complications were higher among fusion studies (13.7%) compared to denervation studies (7.3%); however, it is important to note that these are different study populations and the follow-up times are much shorter among denervation studies. | ||
| 5. Infections | Only fusion studies reported infections (5.3%). No infections were reported among denervation patients. | ||
DISCUSSION (Table Table 4)
The majority of subjects report satisfaction after either treatment. Both treatments appear to demonstrate improvement in outcomes from pre to posttreatment during their follow-up period.
Complication rates and infection rates are higher among those undergoing fusion compared to those undergoing denervation.
The existing literature is limited to case series. No studies were identified that compared treatments in the same patient population. Given these limitations, pooled rates from these studies must be taken with caution. The open fusion studies reported poorer results and higher complication rates than the percutaneous studies. However, the concept of ‘fusion’ of the sacroiliac joint after percutaneous fixation with hollow screws or cages filled with bone-graft substitute was based on the absence of loosening on plain x-rays or confirmation of trabecular continuity across the implants on CT scanning. Also, many of the patients in the fusion series had undergone previous spinal surgery, suggesting that a positive response to sacroiliac blocks does not predict successful pain relief after sacroiliac fusion in patients with chronic pain syndromes.
All of the denervation studies have short follow-up periods, raising the question of duration of effect given that many reported studies of lumbar facet joint denervation show loss of efficacy after about 2 years.
There is a clear need for more properly constructed comparative studies to establish whether chronic sacroiliac joint pain can be better managed with invasive pain relieving techniques than conventional conservative therapies.
EDITORIAL STAFF PERSPECTIVE
Our reviewers were unanimously in favor of publication of this review, despite the controversial nature of a number of aspects of this condition—starting with uncertainty surrounding physical examination, continuing with diagnostic confirmation and finally treatment. The results of this systematic review point out a commonly encountered conundrum: while there seems to be some evidence suggesting a ‘positive treatment effect’ as reported by patients, closer inspection of the data at hand produces more questions than answers. In summary, the role of the sacro-iliac joint in low back pain and its management remain very much unclear to the present date and is, perhaps, somewhat overemphasized by some. Identification of pathologic entities such as presented by the authors—clear instability, severe degeneration, infection, neoplasia—remains a helpful contribution to patient care by an informed practitioner. Should surgical stabilization be chosen for a sufferer of SI-joint pain, the current state of the literature unfortunately allows little or no real insights due to unclear handling of several confounding variables (ie, previous spine fusion, osteoporosis, obesity, pelvic alignment, physical fitness levels) and inconsistent definition of desired surgical outcomes—are true fusions actually achieved in a large number of the described techniques? That said, are solid fusions actually necessary for a satisfactory outcome? Do the outcomes justify the means? Many questions, few real answers, much to do in the future.
This systematic review was founded by AOSpine
Fluoroscopic image intensification control
References
- 1.Wise C L, Dall B E. Minimally invasive sacroiliac arthrodesis: outcomes of a new technique. J Spinal Disord Tech. 2008;21(8):579–584. doi: 10.1097/BSD.0b013e31815ecc4b. [DOI] [PubMed] [Google Scholar]
- 2.Schutz U, Grob D. Poor outcome following bilateral sacroiliac joint fusion for degenerative sacroiliac joint syndrome. Acta Orthop Belg. 2006;72:296–308. [PubMed] [Google Scholar]
- 3.Al-Khayer A, Hegarty J, Hahn D. et al. Percutaneous sacroiliac joint arthrodesis: a novel technique. J Spinal Disord Tech. 2008;21(5):359–363. doi: 10.1097/BSD.0b013e318145ab96. [DOI] [PubMed] [Google Scholar]
- 4.Buchowski J M Kebaish K M Sinkov V et al. 2005Functional and radiographic outcome of sacroiliac arthrodesis for the disorders of the sacroiliac joint Spine J 55520–528.discussion 529 [DOI] [PubMed] [Google Scholar]
- 5.Burnham R S, Yasui Y. An alternate method of radiofrequency neurotomy of the sacroiliac joint: a pilot study of the effect on pain, function, and satisfaction. Reg Anesth Pain Med. 2007;32(1):12–19. doi: 10.1016/j.rapm.2006.08.008. [DOI] [PubMed] [Google Scholar]
- 6.Cohen S P, Hurley R W, Buckenmaier C C. et al. Randomized placebo-controlled study evaluating lateral branch radiofrequency denervation for sacroiliac joint pain. Anesthesiology. 2008;109(2):279–288. doi: 10.1097/ALN.0b013e31817f4c7c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Cohen S P, Abdi S. Lateral branch blocks as a treatment for sacroiliac joint pain: a pilot study. Reg Anesth Pain Med. 2003;28(2):113–119. doi: 10.1053/rapm.2003.50029. [DOI] [PubMed] [Google Scholar]
- 8.Vallejo R, Benyamin R M, Kramer J. et al. Pulsed radiofrequency denervation for the treatment of sacroiliac joint syndrome. Pain Med. 2006;7(5):429–434. doi: 10.1111/j.1526-4637.2006.00143.x. [DOI] [PubMed] [Google Scholar]
- 9.Khurana A, Guha A R, Mohanty K. et al. Percutaneous fusion of the sacroiliac joint with hollow modular anchorage screws: clinical and radiological outcome. J Bone Joint Surg Br. 2009;91(5):627–631. doi: 10.1302/0301-620X.91B5.21519. [DOI] [PubMed] [Google Scholar]
- 10.Yin W, Willard F, Carreiro J. et al. Sensory stimulation-guided sacroiliac joint radiofrequency neurotomy: technique based on neuroanatomy of the dorsal sacral plexus. Spine. 2003;28(20):2419–2425. doi: 10.1097/01.BRS.0000085360.03758.C3. [DOI] [PubMed] [Google Scholar]
- 11.Waisbrod H, Krainick J U, Gerbershagen H U. Sacroiliac joint arthrodesis for chronic lower back pain. Arch Orthop Trauma Surg. 1987;106(4):238–240. doi: 10.1007/BF00450461. [DOI] [PubMed] [Google Scholar]