ABSTRACT
Study design: Biomechanical study.
Objectives: To evaluate the compression strengths of various bone fillers used in treating vertebral compression fractures using a third-generation sawbone model and to evaluate the viability of this novel model as an alternative to actual human or animal vertebrae for biomechanical testing of vertebral-filling materials.
Methods: Cavities were created in the osteoporotic vertebral body sawbone models and filled with PMMA, SRS, MIIGX3 HiVisc, and BoneSource fillers. These were cured according to manufacturers' recommendations and then tested to failure in the compression model. Elastic modulus was calculated and compared with the control group which was not augmented.
Results: The mean modulus of elasticity for the control group vertebrae was 92.44 ± 19.28 MPa. The mean modulus of elasticity was highest in the polymethylmethacrylate (PMMA) group (195.47 ± 2.33 MPa) and lowest in the MIIG group (25.79 ± 4.77 MPa). The results for the SRS-tricalcium phosphate group (79.14 ± 20.20 MPa) were closest to the control group, followed by the BoneSource group (57.49 ± 8.35 MPa). Statistical analysis, for comparison of individual group means, identified significant differences between the control group and all other groups (P < .05), with the exception of the SRS-tricalcium phosphate group (P = .65, versus control). The modulus of elasticity for the PMMA group was significantly higher than all other groups (P < .001).
Conclusion: The third-generation osteoporotic sawbones model simulates in vitro physiological specimen function. It was effective for comparing which osteoconductive agents may provide adequate strength while minimizing potential adjacent level fracture. Increased stiffness was seen with PMMA compared with the unaugmented control as well as with calcium phosphate or calcium sulfate cements suggesting that these may reduce adjacent segment fractures.
STUDY RATIONALE AND CONTEXT
Despite documented pain relief following kyphoplasty and vertebroplasty for the treatment of vertebral compression fractures, one potential complication of these procedures is adjacent segment fracture in the osteoporotic spine. Substances used to reinforce the osteoporotic or diseased vertebrae include polymethylmethacrylate (PMMA) and others, such as calcium phosphate bone cements. Standardized evaluation of the biomechanical properties of different vertebral augmentation agents in a consistently reproducible vertebral body model which mimics physiological conditions in a reproducible fashion and, moreover, is readily available would enhance our ability to draw conclusions on the biomechanical effects of vertebral augmentation on the surrounding spinal column through comparative analysis.
OBJECTIVES
To compare the compression strengths of four different filler materials used in vertebral augmentation and to confirm the feasibility of the third-generation osteoporotic sawbone model as a viable alternative to human or animal vertebrae for biomechanical testing.
METHODS
Study design: Biomechanical study.
Materials and procedures
An anatomical, third-generation sawbone vertebral model (Pacific International) was utilized. Twenty upper lumbar replica vertebrae were allocated to five groups, with four vertebrae in each group. The first group, control, was tested before any augmentation and the remaining four groups were tested after augmentation with one of the four materials below.
To prepare the 16 vertebrae for augmentation, a drill press was used to drill a 5 mm hole through the pedicle into the anterior vertebral body, stopping approximately 5–8 mm before reaching the anterior wall. A Kyphon inflatable bone tamp system was used to create a defect within the cancellous portion of the vertebrae. To ensure that all vertebrae were augmented in a similar fashion, radiopaque dye was used in the insufflation liquid and x-rays of each augmented vertebrae were taken with the inflated balloons in place (Fig 1).
Once the bony defect had been created within the vertebral body, each side of the vertebrae was filled with one of the four different filler materials (Fig 2). After filling with the appropriate material, all of the vertebrae were placed in a water bath at 37°C for 24 hours to allow for complete polymerization. The materials were allowed adequate time to harden and were removed from the water bath.
Four different filler materials were used: (1) Simplex P, polymethylmethacrylate (PMMA) from Stryker Orthopaedics; (2) SRS-tricalcium phosphate cement from Norian Corp; (3) MIIG X3 HiVisc, calcium sulfate cement from Wright Medical; and (4) BoneSource, calcium phosphate cement from Stryker Orthopaedics. The same amount of liquid (5 mL) was used in each augmentation and each vertebra was augmented bilaterally via injection of two 2.5 mL volumes of the investigated material.
The vertebrae were then tested using specially fabricated end plates and the Instron screw-driven mechanical testing load frame (Fig 3). Each vertebra was compressed under a stroke-controlled loading regime to measure the construct's elastic modulus in compression. Mechanical testing of each sample was stopped when either a compressive displacement of 6 mm was achieved or mechanical failure was detected, as denoted by a rapid decrease in the measured compressive load that was greater than 15% of the current load.
Fig 1.
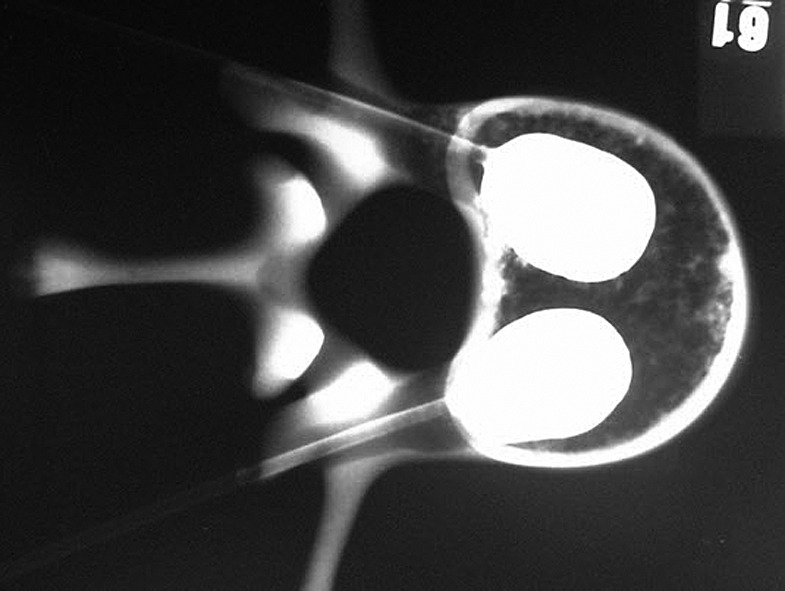
X-ray evaluation of the cement augmentation following cavity creation.
Fig 2.

View through vertebral body with cement augmentation in place.
Fig 3.
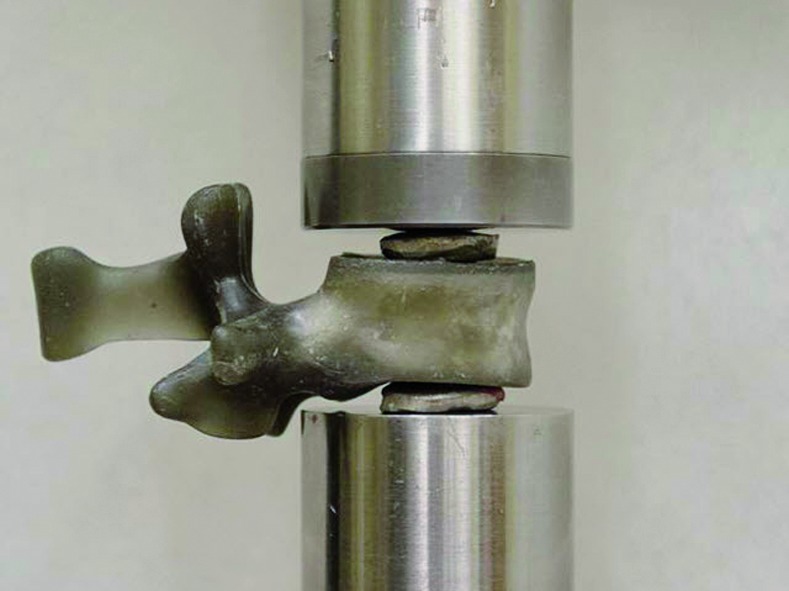
Specimen in testing position.
Outcomes: The modulus of elasticity (in megapascals) under compressive loading was obtained via standard stress/strain calculations, wherein stress is the applied compressive load divided by the surface area of the load-applying custom metallic discs and strain is the recorded axial compression divided by the initial vertical height of the sample.
Analysis: Load deformation and stress/strain curves were calculated using SPSS statistical software. The means across all groups were compared using one-way analysis of variance (ANOVA) and Tukey post hoc testing was used to compare all possible pairs of experimentally derived means, based on a studentized range distribution. Differences between groups were considered significant if P < .05.
Additional methodological and technical details are provided in the web appendices at www.aospine.org/ebsj.
RESULTS
Note: Load to failure was not an experimental parameter utilized in this study. As such, not all samples were loaded until catastrophic failure was observed. Individual test conclusion was achieved when conditions of maximum axial compressive displacement was met (Fig 4).
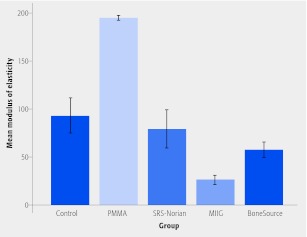
Fig 4.
Mean modulus of elasticity during vertebral compression test. Results are separated based on treatment groups with error bars representing±1 standard deviation. PMMA indicates polymethylmethacrylate.
The mean modulus of elasticity for the control group vertebrae was 92.44 ± 19.28 MPa.
The results for the SRS-tricalcium phosphate group (79.14 ± 20.20 MPa) were closest to the control group, followed by the BoneSource group (57.49 ± 8.35 MPa).
The mean modulus of elasticity was highest in the PMMA group (195.47 ± 2.33 MPa) and lowest in the MIIG group (25.79 ± 4.77 MPa).
Statistically significant differences between the control group and all other groups (P < .05) except the SRS-tricalcium phosphate group (P = .651) were seen.
The modulus of elasticity for the PMMA group was significantly higher than all other groups (P < .001), when group means were independently compared.
DISCUSSION
This study demonstrates the use of the third-generation sawbones vertebral model of osteoporotic bone for biomechanical testing of agents used for vertebral augmentation. This model demonstrated load characteristics similar to cadaveric specimens presented in Johnson and Keller's study 1. The presented model allows for consistent vertebral cavity filling and testing of various fixation strategies.
Concerns have been raised about adjacent level insufficiency fractures following kyphoplasty and vertebroplasty secondary to abnormal stresses from the creation of a “super vertebrae” within an environment of vertebrae with less structural integrity due to disease. Reports of up to 52% of osteoporotic spines treated with either vertebroplasty or kyphoplasty sustained adjacent level fractures within a 7-year period 2. Deramond and Mathis 3 report a slight but significant increase in the incidence of fracture of adjacent vertebrae which they attribute to a shift in the normal load transmission through the spine following vertebroplasty. Abnormal loading and motion have been established in vertebral segments treated with either kyphoplasty or vertebroplasty in the recent article by Lieberman et al 4. Farooq et al 5 found that vertebroplasty reduces stress concentrations in the annulus and neural arch resulting in a more even distribution of compressive stress on the intervertebral disc and adjacent vertebral bodies.
Based on the compression strength values obtained during testing in this biomechanical study, PMMA was significantly stiffer than the other agents tested. Calcium phosphate and calcium sulfate materials revealed a similar modulus of elasticity to the nonaugmented vertebrae; however, both were not as stiff as PMMA but could still withstand significant loading. These findings suggest that choice of agent may influence rates of adjacent segment fracture following augmentation procedures.
The strengths of this study include the use of a model for biomechanical testing that is readily available and provides a consistent loading and testing application.
Limitations of this study include a number of factors related to the potential for absence of clinical correlations, such as lack of adjustability for various degrees of osteoporosis and lack of preexistent kyphosis.
Additional research on the biomechanical properties of filling agents and the potential differential influence such agents may have on rates of adjacent segment fracture are needed. The study by Nouda et al 6 suggests the strength of bone filler may influence the rate of adjacent fracture but further studies are going to be needed for validation.
With regard to this biomechanical model, further testing and direct comparisons to anatomical models is required to validate it for widespread use. A similar model involving multiple vertebral levels should be evaluated to fully elucidate the effects of various filler materials on adjacent vertebrae.
SUMMARY AND CONCLUSION
PMMA was significantly stiffer than the other agents tested and exceeded the normal loading characteristics of osteoporotic vertebral bone.
Comparison of the calcium phosphate and calcium sulfate materials to the unaugmented vertebrae revealed a more similar modulus of elasticity. Calcium phosphate cement may be used as a filler to recreate a more normal elastic modulus vertebral body reconstruction.
The third-generation sawbones vertebral model of osteoporotic bone appears to be a viable option for biomechanical testing of agents used for vertebral augmentation. Further validation is needed.
EDITORIAL STAFF PERSPECTIVE
The reviewers found that this is a well-executed study, methodologically, in examining and comparing the compressive stiffness of vertebrae augmented with various bone-filler substances. The reviewers identified the following issues:
This study uses a third-generation sawbone model for greater consistency in mechanical testing. However, the study itself does not validate this model and there is no comparison of the model used to allow the reader to scale it a given severity of osteoporosis.
The actual desirable stiffness of a vertebral body to be augmented remains elusive. If it is made too stiff, which polymethylmethacrylate (PMMA) injected into a solid mold such as done with kyphoplasty may lead to, increased adjacent segment fractures may occur. If not stiff enough the resultant construct may not be sufficient in providing adequate support and inadequate pain relief. Fig 4 indeed suggests that augmentation with PMMA substantially increases the stiffness of the vertebra compared with the control. However, it also suggests that Norian, BoneSource, and MIIG augmentation result in a vertebra that is less stiff than a nonaugmented vertebra. Why would a physician want to inject a substance that (at least by this report) results in a less stiff vertebra?
Finally, the notion of a “super stiff” vertebra after cement augmentation potentially resulting in adjacent segment fracture is certainly reasonable and widely believe to be the case, though it is difficult to definitively prove. However, there is clinical concerns with “less stiff” bone fillers. There remains uncertainty that cements, which are injected as a not yet set suspension, may leak into blood circulation before curing, and may subsequently result in undesirable systemic effects. Specifically, Norian XR has not been approved for treatment of vertebral fractures in the United States and has been removed from the market for this indication 1. Clearly, the potential advantages of a “less stiff” construct (potentially reducing adjacent level fracture) must be balanced against the safety of the index procedure. As many of the cements are injected into a vulnerable and elderly population with damaged vertebral bodies, improved mechanical, rheological, and physiological understanding is desirable to assure patient safety prior to routine clinical implementation.
This study was funded in part by University of Mississippi Medical Center intramural funding.
REFERENCES
- 1.Johnson A E, Keller T S. Mechanical properties of open-cell foam synthetic thoracic vertebrae. J Mater Sci Mater Med. 2008;19:1317–1323. doi: 10.1007/s10856-007-3158-7. [DOI] [PubMed] [Google Scholar]
- 2.Grados F, Depriester C, Cayrolle G. et al. Long-term observations of vertebral osteoporotic fractures treated by percutaneous vertebroplasty. Rheumatology (Oxford) 2000;39:1410–1414. doi: 10.1093/rheumatology/39.12.1410. [DOI] [PubMed] [Google Scholar]
- 3.Deramond H, Mathis J M. Vertebroplasty in osteoporosis. Semin Musculoskelet Radiol. 2002;6:263–268. doi: 10.1055/s-2002-36724. [DOI] [PubMed] [Google Scholar]
- 4.Lieberman I H, Togawa D, Kayanja M M. Vertebroplasty and kyphoplasty: filler materials. Spine J. 2005;5:305S–316S. doi: 10.1016/j.spinee.2005.02.020. [DOI] [PubMed] [Google Scholar]
- 5.Farooq N, Park J C, Pollintine P. et al. Can vertebroplasty restore normal load-bearing to fractured vertebrae? Spine (Phila Pa 1976) 2005;30:1723–1730. doi: 10.1097/01.brs.0000171906.01906.07. [DOI] [PubMed] [Google Scholar]
- 6.Nouda S, Tomita S, Kin A. et al. Adjacent vertebral body fracture following vertebroplasty with polymethylmethacrylate or calcium phosphate cement: biomechanical evaluation of the cadaveric spine. Spine (Phila Pa 1976) 2009;34:2613–2618. doi: 10.1097/BRS.0b013e3181abc150. [DOI] [PubMed] [Google Scholar]