Abstract
Objective
The objective of this research was to identify top dietary sources of energy, solid fats, and added sugars among 2–18 year olds in the United States.
Methods
Data from the National Health and Nutrition Examination Survey (NHANES), a cross-sectional study, were used to examine food sources (percentage contribution and mean intake with standard errors) of total energy (2005–06) and calories from solid fats and added sugars (2003–04). Differences were investigated by age, sex, race/ethnicity, and family income, and the consumption of empty calories—defined as the sum of calories from solid fats and added sugars—was compared with the corresponding discretionary calorie allowance.
Results
The top sources of energy for 2–18 year olds were grain desserts (138 kcal/day), pizza (136 kcal), and soda (118 kcal). Sugar-sweetened beverages (soda and fruit drinks combined) provided 173 kcal/day. Major contributors varied by age, sex, race/ethnicity, and income. Nearly 40% of total calories consumed (798 kcal/day of 2027 kcal) by 2–18 year olds were in the form of empty calories (433 kcal from solid fat and 365 kcal from added sugars). Consumption of empty calories far exceeded the corresponding discretionary calorie allowance for all sex-age groups (which range from 8–20%). Half of empty calories came from six foods: soda, fruit drinks, dairy desserts, grain desserts, pizza, and whole milk.
Conclusion
There is an overlap between the major sources of energy and empty calories: soda, grain desserts, pizza, and whole milk. The landscape of choices available to children and adolescents must change to provide fewer unhealthy foods and more healthy foods with fewer calories. Identifying top sources of energy and empty calories can provide targets for changes in the marketplace and food environment. However, product reformulation alone is not sufficient—the flow of empty calories into the food supply must be reduced.
Introduction
In the United States (US) today, over 23 million children and adolescents are overweight or obese (1,2). Excess body weight, poor diet, and sedentary behavior have been associated with an increased risk of many chronic diseases, including hypertension, dyslipidemia, type 2 diabetes, as well as depression, poor self-esteem, and associated quality of life issues (3,4). Although overweight and obesity are found in all subpopulations, the burden is particularly striking among children, adolescents, and underserved populations. Children and adolescents are now experiencing weight-related chronic diseases once seen only among adults. Additionally, the prevalence of overweight is higher among adolescents compared to younger children, Mexican-American boys compared to non-Hispanic black or white boys, and Mexican-American and Non-Hispanic black girls compared to non-Hispanic white girls (2).
Multiple factors influence overweight and obesity rates, but ultimately, an imbalance between energy consumed and energy expended is the determining factor. The current environment (including food stores, restaurants, schools, and worksites) and customs surrounding food in the US have been labeled “obesogenic” and “toxic” due to the contributions made to this imbalance by large portion sizes, snacking, away-from-home meals, and consumption of sugar-sweetened beverages (5–7). Ironically, in a food environment that supplies an overabundance of energy, there are too few vegetables, whole grains, fruits, and milk products (8). Therefore, US children and adolescents do not always consume the types and amounts of food they need to support an active, healthy lifestyle (9).
Recommendations for fruits, vegetables, whole grains and other nutrient-bearing food groups are available in the 2005 Dietary Guidelines for Americans and MyPyramid (10, 11). These resources also define the concept of a “discretionary calorie allowance” to provide limits for excess calories from consumption of food groups beyond recommended amounts and all calories from solid fats, alcoholic beverages, and added sugars (SoFAAS). These SoFAAS represent empty calories, or sources of energy with virtually no nutritional value, and have been examined previously in relation to discretionary calorie allowances (12). Although the discretionary calorie allowance should be considered an upper bound on consumption of calories from SoFAAS, such intakes far exceed the recommended discretionary calorie allowances across all sex-age groups in the US population (13). The purpose of this paper is to identify the top as-eaten food sources of energy, solid fats, and added sugars among US children and adolescents. “As-eaten” food sources include composite foods (e.g., cookies), and mixed dishes (e.g., pizza), as well as discrete foods (e.g., milk or apples).
Methods
Data source and sample
Data from the National Health and Nutrition Examination Survey (NHANES), a cross-sectional study, were used to examine food sources of total energy (2005–06) and calories from solid fats and added sugars (2003–04). NHANES is a nationally representative survey with a complex multistage, stratified probability sample. Trained interviewers conducted in-person 24-hour dietary recalls with all eligible persons, using automated data collection systems that included multiple passes. Survey participants ages 12 years and older completed the dietary interview on their own, proxy-assisted interviews were conducted with children ages 6 to 11 years, and proxy respondents reported for children younger than age 5 years (14). The NHANES protocol was approved by the National Center for Health Statistics Research Ethics Review Board, Hyattsville, Maryland, and all participants provided informed consent. Further information regarding the design of the NHANES, including sampling and weighting procedures, can be found at http://www.cdc.gov/nchs/nhanes.htm.
Defining a list of specific foods
NHANES dietary intake data are catalogued according to discrete codes representing foods as eaten. For this analysis, food codes representing similar foods were combined to provide an indication of the contribution of distinct foods as-eaten to the consumption of energy, solid fats, and added sugars. That is, the food codes reported by 2–18 year olds during any of the years examined were sorted into 96 mutually exclusive food categories, which are hereafter referred to as specific foods. The list of specific foods (Figure 1) was adapted from earlier analyses (15–17) and has been used in a previous project (18).
Figure 1.
List of specific foods: Result of grouping like foods reported in 2003–2004 and 2005–2006 NHANESa
Defining energy from solid fats and added sugars
USDA’s MyPyramid Equivalents Database (MPED) Version 2.0 (19) was used to estimate energy from solid fats and added sugar (MPED values for grams of solid fat and teaspoons of added sugars were converted based on 9 kcal/gram and 16 kcal/teaspoon, respectively). To capture how well diets conform to current guidance, the MPED incorporates data from a “recipe” file, which disaggregates all foods reported in the survey to individual ingredients, and assigns those ingredients to MyPyramid groupings. For example, yogurt with fruit is separated into yogurt, fat, fruit, and caloric sweetener in the recipe file and assigned corresponding cup-equivalents of milk and fruit, grams of solid fat, and teaspoons of added sugar. Because MPED is currently available only through NHANES 03–04, energy from solid fats and added sugars were calculated for those years.
Statistical analysis
Dietary recalls (Day 1 only) for all 2–18 years olds with data deemed reliable by the study developers were included in this analysis. Appropriate weighting factors were applied to adjust for differential probabilities of selection and various sources of non-response. Mean intakes of total energy, energy from solid fats, and energy from added sugars were calculated. The percentage contribution and mean intake (with standard errors) of specific foods to total energy, energy from solid fats, and energy from added sugars were also estimated. Differences were examined by age (using age groups featured in current guidance (10, 11): 2–3, 4–8, 9–13, and 14–18 years old), sex, race/ethnicity (Non-Hispanic Whites, Non-Hispanic Blacks, Mexican Americans), and family income based on the federal poverty income ratio (PIR) (using three PIR categories: less than 130% of PIR, 131% to 185%, and greater than 185%). The PIR is the ratio of income to the designated poverty threshold for the family’s composition as defined by the US Census Bureau; family income less than 185% of PIR is considered low-income and qualifies for the Special Supplemental Program for Women, Infants, and Children and reduced-price school meals, and income less than 130% qualifies for the Supplemental Nutrition Assistance Program (formerly the Food Stamp Program) and free school meals.
Finally, the contribution of “empty calories”—defined as the sum of energy from solid fats and added sugars—was calculated and put side by side with the corresponding discretionary calorie allowance for each sex-age group (11). Low activity levels were assumed, because most children and adolescents do not achieve the 60 minutes per day of cardiorespiratory activity recommended in national physical activity guidelines (20). Data analyses were conducted using SAS (version 9.1, SAS Institute Inc, Cary, NC) and SUDAAN (version 9.0,Research Triangle Institute, Research Triangle Park, NC).
Results
Mean intakes of energy, solid fats, and added sugars, along with the contributions (percentage and absolute intake) of specific foods contributing at least 2%, are available online at www.riskfactor.cancer.gov/foodsources/energy. Data are provided for persons 2–18 years and by age, sex, race/ethnicity, and income level. For ease of presentation in this paper, mean intakes of energy, solid fats, and added sugars, and results from the top five sources are summarized in Tables 1 and 2 and Figure 2.
Table 1.
Mean intake and major sources of energy, solid fats and added sugars among children and adolescents in the United States (2–18 years old)
| Top five sources | ||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Age Group |
#1 | % | Mean (kcal) |
SE | #2 | % | Mean (kcal) |
SE | #3 | % | Mean (kcal) |
SE | #4 | % | Mean (kcal) |
SE | #5 | % | Mean (kcal) |
SE |
| Energy a | ||||||||||||||||||||
| All | Grain dessertsb | 6.8 | 138 | 6.7 | Pizza | 6.7 | 136 | 8.5 | Sodac | 5.8 | 118 | 8.7 | Yeast breads | 5.6 | 114 | 6.8 | Chickend | 5.6 | 113 | 8.1 |
| 2–3 | Whole milk | 7.1 | 104 | 8.2 | 100% fruit juicee | 6.3 | 93 | 9.4 | Reduced fat milk | 6.2 | 91 | 10.7 | Pastaf | 5.9 | 86 | 9.4 | Grain dessertsb | 4.6 | 68 | 6.6 |
| 4–8 | Grain dessertsb | 7.6 | 136 | 10.8 | Yeast breads | 5.4 | 98 | 5.1 | Pastaf | 5.4 | 97 | 11.4 | Reduced fat milk | 5.3 | 95 | 7.2 | Pizza | 5.3 | 95 | 12.3 |
| 9–13 | Grain dessertsb | 7.1 | 145 | 15.6 | Pizza | 6.3 | 128 | 9.5 | Chickend | 6.0 | 122 | 13.1 | Yeast breads | 5.4 | 109 | 5.8 | Sodac | 5.2 | 105 | 12.1 |
| 14–18 | Sodac | 9.3 | 226 | 18.2 | Pizza | 8.8 | 213 | 24.5 | Grain dessertsb | 6.5 | 157 | 8.4 | Yeast breads | 6.2 | 151 | 14.5 | Chickend | 5.9 | 143 | 16.6 |
| Solid Fats g | ||||||||||||||||||||
| All | Pizza | 11.5 | 50 | 3.6 | Grain dessertsb | 9.8 | 43 | 2.4 | Whole milk | 8.2 | 35 | 3.2 | Regular cheese | 7.9 | 34 | 2.9 | Fatty meatsh | 6.7 | 29 | 2.5 |
| 2–3 | Whole milk | 16.7 | 58 | 5.6 | Fatty meatsh | 11.1 | 39 | 5.0 | Regular cheese | 8.6 | 30 | 6.0 | Reduced fat milk | 8.1 | 28 | 3.8 | Grain dessertsb | 7.2 | 25 | 2.4 |
| 4–8 | Whole milk | 11.3 | 45 | 5.6 | Pizza | 10.2 | 41 | 6.0 | Grain dessertsb | 9.0 | 36 | 2.6 | Regular cheese | 7.0 | 28 | 4.5 | Reduced fat milk | 6.9 | 28 | 3.6 |
| 9–13 | Grain dessertsb | 11.4 | 51 | 6.0 | Pizza | 11.2 | 50 | 5.2 | Regular cheese | 8.9 | 40 | 5.3 | Whole milk | 6.7 | 30 | 4.4 | Fatty meatsh | 6.5 | 29 | 2.9 |
| 14–18 | Pizza | 14.7 | 70 | 9.3 | Grain dessertsb | 9.7 | 46 | 2.8 | Regular cheese | 7.6 | 36 | 3.2 | Fried potatoes | 6.9 | 33 | 2.3 | Fatty meatsh | 5.7 | 27 | 3.0 |
| Added Sugars i | ||||||||||||||||||||
| All | Sodac | 31.8 | 116 | 5.3 | Fruit drinks | 15.0 | 55 | 3.1 | Grain dessertsb | 10.9 | 40 | 2.3 | Dairy desserts | 7.9 | 29 | 3.4 | Candy | 6.8 | 25 | 2.2 |
| 2–3 | Fruit drinks | 19.3 | 38 | 3.7 | Sodac | 11.4 | 22 | 3.3 | Grain dessertsb | 11.3 | 22 | 1.7 | Candy | 8.5 | 17 | 2.5 | Cold cereals | 8.3 | 16 | 1.6 |
| 4–8 | Sodac | 19.9 | 65 | 7.5 | Fruit drinks | 17.0 | 56 | 5.9 | Grain dessertsb | 11.2 | 37 | 2.8 | Dairy desserts | 10.4 | 34 | 5.9 | Cold cereals | 8.3 | 27 | 1.9 |
| 9–13 | Sodac | 30.7 | 117 | 11.7 | Fruit drinks | 13.6 | 52 | 5.7 | Grain dessertsb | 12.4 | 47 | 5.6 | Dairy desserts | 8.8 | 33 | 5.2 | Candy | 7.8 | 30 | 3.1 |
| 14–18 | Sodac | 44.5 | 197 | 9.7 | Fruit drinks | 14.1 | 63 | 5.6 | Grain dessertsb | 9.4 | 42 | 2.9 | Candy | 5.6 | 25 | 4.1 | Dairy desserts | 5.5 | 24 | 2.7 |
Data Source: Energy data from NHANES 2005–2006, Solid Fats and Added Sugars data from NHANES 2003–2004.
NHANES 2005–2006: Sample size by group by group: Ages 2–18 (n=3778), 2–3 (n=497), 4–8 (n=899), 9–13 (n=1047), 14–18 (n=1335).
NHANES 2003–2004: Sample size by group by group: Ages 2–18 (n=3553), 2–3 (n=424), 4–8 (n=781), 9–13 (n=1001), 14–18 (n=1347).
SE: Standard Error.
Energy mean intake (kcal) by group: Ages 2–18 (2027), 2–3 (1471), 4–8 (1802), 9–13 (2035), 14–18 (2427).
Includes cakes, cookies, donuts, pies, crisps, cobblers, granola bars.
Includes sodas, energy drinks, sports drinks, and sweetened bottled water including vitamin water.
Includes chicken and chicken mixed dishes.
Excludes orange and grapefruit juice.
Includes pasta and pasta dishes.
Solid fats mean intake (kcal) by group: Ages 2–18 (433), 2–3 (350), 4–8 (401), 9–13 (450), 14–18 (476).
Includes sausage, franks, bacon, and ribs.
Added sugars mean intake (kcal) by group: Ages 2–18 (365), 2–3 (197), 4–8 (329), 9–13 (381), 14–18 (444).
Table 2.
Mean intake and major sources of energy, solid fats and added sugars among children and adolescents in the United States (2–18 years old), by Race/Ethnicity and Family Income
| Top five sources | |||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Groupa | #1 | % | Mean (kcal) |
SE | #2 | % | Mean (kcal) |
SE | #3 | % | Mean (kcal) |
SE | #4 | % | Mean (kcal) |
SE | #5 | % | Mean (kcal) |
SE | |
| Energy b | |||||||||||||||||||||
| NHW | Grain dessertsc | 7.2 | 152 | 9.3 | Pizza | 7.0 | 148 | 12.8 | Sodad | 6.4 | 134 | 13.4 | Yeast breads | 6.1 | 129 | 10.5 | Chickene | 5.2 | 109 | 11.3 | |
| NHB | Chickenn | 8.4 | 163 | 13.8 | Grain dessertsl | 6.3 | 123 | 9.3 | Pizza | 6.1 | 119 | 8.6 | Fruit drinks | 5.1 | 100 | 13.8 | Pastaf | 4.7 | 90 | 11.2 | |
| Mex-Am | Mexican dishes | 7.1 | 136 | 8.5 | Grain dessertsl | 5.9 | 114 | 10.8 | Pizza | 5.5 | 105 | 19.2 | Whole milk | 5.1 | 99 | 8.3 | Sodam | 4.8 | 92 | 4.6 | |
| <=130% | Grain dessertsl | 6.1 | 117 | 9.4 | Chickenn | 6.0 | 116 | 13.7 | Pizza | 5.9 | 114 | 9.6 | Sodam | 5.3 | 101 | 12.8 | Yeast breads | 5.1 | 99 | 4.7 | |
| 131–185% | Pizza | 10.1 | 203 | 62.7 | Sodam | 7.0 | 142 | 48.6 | Grain desserts | 6.9 | 138 | 13.4 | Yeast breads | 6.5 | 131 | 32.7 | Pastao | 5.2 | 104 | 19.0 | |
| >=186% | Grain dessertsl | 7.1 | 148 | 9.2 | Pizza | 6.5 | 135 | 12.4 | Sodam | 5.9 | 122 | 7.8 | Yeast breads | 5.7 | 119 | 7.7 | Chickenn | 5.5 | 114 | 9.0 | |
| Solid Fats g | |||||||||||||||||||||
| NHW | Pizza | 13.0 | 57 | 5.3 | Grain dessertsl | 9.4 | 41 | 3.5 | Regular cheese | 8.9 | 39 | 4.1 | Reduced fat milk | 7.2 | 32 | 3.4 | Whole milk | 6.7 | 30 | 4.0 | |
| NHB | Pizza | 11.4 | 49 | 3.2 | Grain dessertsl | 10.4 | 45 | 4.1 | Fatty meatsh | 10.1 | 44 | 7.5 | Whole milk | 8.8 | 38 | 3.0 | Fried potatoes | 6.2 | 27 | 1.7 | |
| Mex-Am | Whole milk | 12.0 | 52 | 4.5 | Grain dessertsl | 10.6 | 45 | 3.2 | Mexican dishes | 9.8 | 42 | 5.9 | Pizza | 8.3 | 36 | 3.9 | Regular cheese | 7.1 | 31 | 4.1 | |
| <=130% | Whole milk | 12.7 | 56 | 5.1 | Pizza | 10.0 | 44 | 6.9 | Grain dessertsl | 9.7 | 43 | 3.0 | Fatty meatsq | 8.4 | 37 | 5.2 | Regular cheese | 7.1 | 31 | 2.7 | |
| 131–185% | Pizza | 13.7 | 59 | 13.8 | Regular cheese | 10.5 | 46 | 16.7 | Whole milk | 9.0 | 39 | 8.8 | Grain dessertsl | 8.5 | 37 | 2.9 | Fried potatoes | 8.4 | 36 | 10.4 | |
| >=186% | Pizza | 12.2 | 52 | 5.7 | Grain dessertsl | 10.2 | 43 | 3.3 | Regular cheese | 7.9 | 34 | 2.2 | Reduced fat milk | 6.3 | 27 | 3.2 | Pastao | 6.3 | 27 | 3.5 | |
| Added Sugars i | |||||||||||||||||||||
| NHW | Sodam | 34.7 | 130 | 8.8 | Fruit drinks | 12.2 | 46 | 4.3 | Grain dessertsl | 10.3 | 39 | 3.2 | Dairy desserts | 8.4 | 31 | 4.7 | Cold cereals | 6.5 | 24 | 2.1 | |
| NHB | Fruit drinks | 24.3 | 89 | 3.9 | Sodam | 21.8 | 80 | 6.5 | Grain dessertsl | 12.1 | 45 | 3.7 | Candy | 9.4 | 35 | 4.9 | Dairy desserts | 7.2 | 26 | 4.4 | |
| Mex-Am | Sodam | 31.5 | 111 | 14.0 | Fruit drinks | 19.0 | 67 | 6.1 | Grain dessertsl | 11.5 | 40 | 3.0 | Candy | 6.1 | 21 | 2.0 | Dairy desserts | 5.8 | 20 | 2.4 | |
| <=130% | Sodam | 30.4 | 110 | 6.0 | Fruit drinks | 15.0 | 54 | 4.2 | Grain dessertsl | 11.4 | 41 | 4.2 | Cold cereals | 7.7 | 28 | 2.9 | Dairy desserts | 7.3 | 27 | 3.4 | |
| 131–185% | Sodam | 32.7 | 110 | 8.7 | Grain dessertsl | 12.3 | 41 | 4.9 | Fruit drinks | 11.9 | 40 | 6.8 | Cold cereals | 8.0 | 27 | 3.8 | Dairy desserts | 7.2 | 24 | 3.4 | |
| >=186% | Sodam | 32.6 | 122 | 9.2 | Fruit drinks | 15.5 | 58 | 4.4 | Grain dessertsl | 10.2 | 38 | 2.3 | Dairy desserts | 8.5 | 32 | 4.7 | Candy | 6.8 | 25 | 3.1 | |
Data Source: Energy data from NHANES 2005–2006, Solid Fats and Added Sugars data from NHANES 2003–2004.
NHANES 2005–2006: Sample size by group by group: Non-Hispanic Whites (n=1018), Non-Hispanic Blacks (n=1161), Mexican-Americans (n=1253), <= 130% POV (n=1457), 131–185% POV (n=451), >=186% POV (n=1707).
NHANES 2003–2004: Sample size by group by group: Non-Hispanic Whites (n=980), Non-Hispanic Blacks (n=1229), Mexican-Americans (n=1062), <= 130% POV (n=1536), 131–185% POV (n=465), >=186% POV (n=1401).
SE: Standard Error.
Race/Ethnicity groups being reported are: Non-Hispanic Whites (NHW), Non-Hispanic Blacks (NHB), and Mexican-Americans (Mex-Am). Family Income groups being reported on are: families with incomes at or below 130% of the poverty level, those between 131–185% of the poverty level, and those at or above 186% of poverty level.
Energy mean intake (kcal) by group: Non-Hispanic Whites (2101), Non-Hispanic Blacks (1941), Mexican-Americans (1930), <= 130% POV (1923), 131–185% POV (2009), >=186% POV (2087).
Includes cakes, cookies, donuts, pies, crisps, cobblers, granola bars.
Includes sodas, energy drinks, sports drinks, and sweetened bottled water including vitamin water.
Includes chicken and chicken mixed dishes.
Includes pasta and pasta dishes.
Solid fats mean intake (kcal) by group: Non-Hispanic Whites (442), Non-Hispanic Blacks (433), Mexican-Americans (430), <= 130% POV (444), 131–185% POV (433), >=186% POV (425).
Includes sausage, franks, bacon, and ribs.
Added sugars mean intake (kcal) by group: Non-Hispanic Whites (376), Non-Hispanic Blacks (368), Mexican-Americans (351), <= 130% POV (361), 131–185% POV (336), >=186% POV (374).
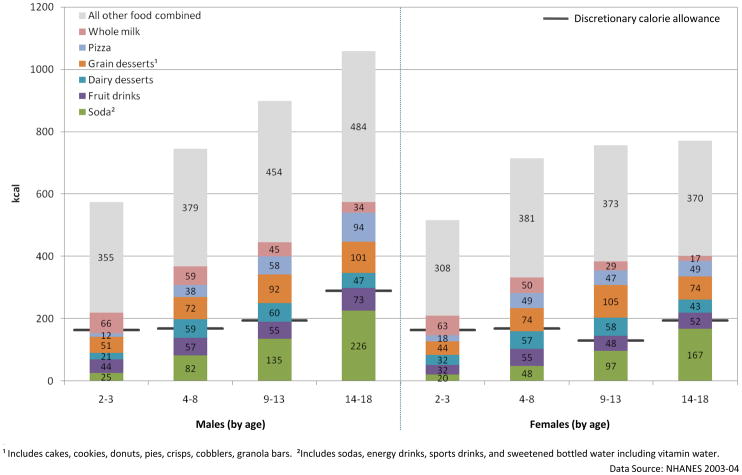
Figure 2.
Food sources and mean intake of empty calories for male and female children and adolescents in the United States, relative to discretionary calorie allowance
Among 2–18 year olds, about half of empty calories came from six specific foods: soda, fruit drinks, dairy desserts, grain desserts, pizza, and whole milk.
The discretionary calorie allowance for each sex/age group is based on low activity levels, because most children and adolescents do not achieve the 60 minutes per day of cardio-respiratory activity recommended in national physical activity guidelines (21).
Energy
The top five sources of energy for 2–18 years olds were grain desserts (cakes, cookies, donuts, pies, crisps, cobblers, and granola bars) (138 kcal/day), pizza (136 kcal), soda (118 kcal), yeast breads (114 kcal), and chicken and chicken mixed dishes (113 kcal) (Table 1). These foods each contributed more than 5% to energy intake, or more than 100 kcal per child per day. Combining related specific foods within the beverage category, children and adolescents consumed 173 kcal from sugar-sweetened beverages (combining soda and fruit drinks) and 146 kcal from milk (combining whole and reduced-fat versions) (data for fruit drinks and reduced fat milk do not always appear in the top five sources, so these data are available online).
These major contributors varied by age group. For example, the top five sources of energy for 2–3 years olds included whole milk (104 kcal/day), fruit juice (93 kcal), reduced-fat milk (91 kcal), and pasta and pasta dishes (86 kcal). Pasta and reduced-fat milk were also among the top five sources of energy for 4–8 years olds (97 and 95 kcal, respectively).
The top contributors of energy also varied by race/ethnicity (Table 2). For example, major contributors for 2–18 year old Non-Hispanic Blacks included fruit drinks (100 kcal/day) and pasta and pasta dishes (90 kcal), while Mexican-Americans’ top sources included Mexican mixed dishes (136 kcal) and whole milk (99 kcal). Non-Hispanic Blacks and Whites consumed more energy from sugar-sweetened beverages (combining soda and fruit drinks) than from milk (combining all milks), whereas Mexican-Americans consumed more energy from milk than from sugar-sweetened beverages (Table 2 and online tables). The top five sources of energy by income were consistent across income levels, but varied in ranking order.
Solid Fats
The average daily intake of energy from solid fats among 2–18 year olds is 433 kcal (Table 1). The major sources of solid fat were pizza (50 kcal/day from solid fat), grain desserts (43 kcal), whole milk (35 kcal), regular cheese (34 kcal), and fatty meats (29 kcal). This list varied by age group, with younger children obtaining a greater share of their solid fat from both whole and reduced-fat milk and 14–18 year olds getting more from fried potatoes. Major contributors also included fried potatoes among non-Hispanic Blacks and persons with PIR between 131% and 185%, Mexican dishes among Mexican-Americans, reduced-fat milk among non-Hispanic Whites and persons with PIR greater than 185%, and pasta among persons with PIR greater than 185% (Table 2).
Added Sugars
The average daily intake of energy from added sugars among all 2–18 year olds was 365 kcal (Table 1). The major sources of added sugars were soda (116 kcal/day from added sugars), fruit drinks (55 kcal), grain desserts (40 kcal), dairy desserts (29 kcal), and candy (25 kcal). The list does not vary markedly by age and demographic groups, but cold cereals were among the top sources for 2–8 year old children, Non-Hispanic Whites, and low-income groups (Table 2).
Sugar-sweetened beverages (soda and fruit drinks) represented the top two sources of calories from added sugars among nearly all age and demographic groups (Tables 1 and 2). The consumption of added sugar from sugar-sweetened beverages was 60 kcal/day for 2–3 year olds, 121 kcal for 4–8 year olds, 169 kcal for 9–13 year olds, and 260 kcal for 14–18 year olds. Among all racial/ethnic and income groups, sugar-sweetened beverages contributed about 45–50% of added sugars. Non-Hispanic Blacks obtained more added sugars from fruit drinks and less from soda than other groups.
Empty Calories
Empty calories represented the sum of calories from solid fat and added sugars. Nearly 40% of total calories consumed (798 kcal/day of 2027 kcal) by 2–18 year olds were in the form of empty calories (433 kcal from solid fat and 365 kcal from added sugars, as shown in Table 1). This contrasts markedly with the discretionary calorie allowances, which range from 8% to 20% of total calories. As shown in Figure 2, consumption of empty calories far exceeded the corresponding discretionary calorie allowance for all sex-age groups.
Among 2–18 year olds, about half of these empty calories came from six specific foods: soda, fruit drinks, dairy desserts, grain desserts, pizza, and whole milk (Figure 2). Solid fats and added sugars found in all other foods combined supplied the remainder. Sugar-sweetened beverages were the largest contributor, providing 22% of empty calories (data available online). In fact, among both males and females 9–13 and 14–18 years old, the empty calories consumed from soda and fruit drinks alone effectively “used up” or exceeded the discretionary calorie allowance.
Discussion
To our knowledge, this is the first paper to provide data on sources of solid fats and added sugars (collectively, empty calories) as well as total energy, among diets of children and adolescents, examined by race/ethnicity, income, and age groups. The variables examined are based on the most recent available data on a nationally representative sample of US children and adolescents.
Several previously published analyses laid the foundation for this work (15–18,21–25). Subar et al. examined data from the 1989–1991 Continuing Survey of Food Intakes by Individuals (15) and found 2–18 year olds in the US consumed 11.7% of energy from milk and 4.3% of total energy from soda (and 6.5% from all sugar-sweetened beverages). A higher proportion of energy consumption from soda and all sugar-sweetened beverages (5.8% and 8.5%, respectively) and a lower proportion of milk (7.1%) were identified in the current study. These trends regarding an increase in total energy from soda and fruit drinks are consistent with previous research (24–25). More recently, Wang et al. found that 2–19 years olds consumed 10–15% of energy intake from sugar-sweetened beverages and 100% fruit juice (25). Although the food groupings and age groupings were slightly different, our results are consistent with their findings (2–18 year olds consumed 11.1% of energy intake from sugar-sweetened beverages and 100% fruit juice) (25).
A notable overlap was found between the major sources of energy and major sources of empty calories: soda, grain desserts, pizza, and whole milk. Soda is made up solely of empty calories; grain desserts can provide some nutrients but are generally rich in both solid fats and added sugars; and pizza and whole milk supply needed nutrients but are also rich in solid fats. Whole milk has more nutrient-dense alternatives: fat-free milk and/or reduced-fat milk. Pizza and grain desserts are generally made commercially; these foods could benefit from reformulation to reduce the empty calories and make them healthier.
The landscape of choices available to children and adolescents must change to provide fewer unhealthy foods and more healthy foods with fewer calories. Several analyses have attempted to quantify the existing “energy gap,” or energy imbalance that contributes to overweight and obesity among children and adolescents (26–27). Whether the energy gap is 150 (26) or 350 kcal/day (27), identifying sources of energy and empty calories can provide targets for changes in the marketplace and the food environment. Dietitians, nutritionists, and other health professionals can work to promote healthier food environments for children and adolescents at multiple levels—at the macro-, community-, school-, and individual-levels.
Groups such as the Healthy Weight Commitment Foundation, a partnership among major food and beverage manufacturers, trade associations, retailers, and others, have formed around the common goal of reducing childhood obesity by 2015 (28). Given recent weight status trends, this is an ambitious goal, but one that the food industry is uniquely positioned to influence through the use of product innovation, portion control, and promotions. For example, a major cereal manufacturer has committed to reducing to single digits the grams of sugar per serving in sugar-sweetened breakfast cereals advertised to children (29), and other companies participating in this new initiative may consider smaller-portion packages. However, such steps will not reduce obesity if they do not significantly reduce the flow of empty calories into the nation’s food supply, limit unhealthy foods, and provide consistent messaging about healthy foods. Future studies may investigate links between changes in empty calories in the food supply and changes in dietary intake.
Limitations
Several caveats are worth noting, to aid in interpretation of the data. First, decisions regarding how to group or separate foods influenced the rankings. Fat-free milk, reduced-fat milk and whole milk were analyzed separately, as were soda, fruit drinks, and fruit juices, to allow for meaningful differences to be seen where they existed (for example, whole milk was a top source among younger children compared to adolescents). Although it was informative to examine these as discrete foods, it was also useful to combine them to see their additive contribution to energy intakes.
Second, the rankings for the specific foods also depended in part on how ubiquitously a given food was consumed. Foods that contained the most calories, solid fats, and/or added sugars were not necessarily the major contributors to population intake. Because some foods were commonly consumed in the population, they contributed more to total intake than foods that contained more energy (or solid fats or added sugars) per portion. Similarly, because adolescents require and consumed more energy than smaller children, the rankings for all ages considered together were heavily influenced by those of older children and teenagers.
Third, the mean contribution represents the average per capita rather than per user. For example, all persons age 2–18 consumed an average of 116 kcal/day from soda. If the analysis was restricted to only those children and adolescents who reported drinking soda on a given day, average caloric intake from soda would be higher.
Finally, these analyses make use of data from NHANES 2003–04. Although more recent NHANES data are available, MPED updates have not kept up with NHANES releases. It is not expected that substantial shifts in sources of energy, saturated fat or added sugars occurred in the relatively short span between these survey cycles. However, updated databases for MyPyramid equivalents are necessary to enable monitoring of trends. More current MPED data also are necessary for any other analysis requiring that food intake be evaluated in relation to dietary guidance.
Conclusion
The epidemic of obesity among children and adolescents is now widely regarded as one of the most important public health problems in the US. Most experts agree that the solution will involve changes in both diet and physical activity, in order to affect energy balance. For diet, this means a reduction in energy from current consumption levels. Although reduction in energy intake from any source could lead to weight change, it would seem imprudent to advise children to cut down on key nutrient-bearing food groups, such as fruits, vegetables, whole grains, fat-free milk, and lean meats. This is especially true given that solid fats and added sugars are consumed in amounts far in excess of allowance levels. This paper identifies the major sources of overall energy and empty calories, providing context for dietary guidance that could specifically focus on limiting calories from these sources and for changes in the food environment.
Acknowledgments
The authors gratefully acknowledge the contributions of Lisa Kahle, Information Management Systems, Inc, for SAS programming and data analysis, Carmita Signes, NOVA Research, for table and figure preparation, and Anne Rodgers for thoughtful review.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Jill Reedy, Division of Cancer Control and Population Sciences, National Cancer Institute, Bethesda, MD.
Susan M. Krebs-Smith, Division of Cancer Control and Population Sciences, National Cancer Institute, Bethesda, MD.
References
- 1.Ogden CL, Carroll MD, Flegal KM. High body mass index for age among US children and adolescents, 2003–2006. JAMA. 2008;299:2401–2405. doi: 10.1001/jama.299.20.2401. [DOI] [PubMed] [Google Scholar]
- 2.Ogden CL, Carroll MD, Curtin LR, Lamb MM, Flegal KM. Prevalence of high body mass index in US children and adolescents, 2007–2008. JAMA. 2010 Jan 13; doi: 10.1001/jama.2009.2012. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 3.Dietz WH. Health consequences of obesity in youth: childhood predictors of adult disease. Pediatrics. 1998;101:518–25. [PubMed] [Google Scholar]
- 4.Schwimmer JB, Burwinkle TM, Varni JW. Health-related quality of life of severely obese children and adolescents. JAMA. 2003;289:1813–9. doi: 10.1001/jama.289.14.1813. [DOI] [PubMed] [Google Scholar]
- 5.Nielsen SJ, Siega-Riz AM, Popkin BM. Trends in energy intake in US between 1977 and 1996: Similar shifts seen across age groups. Obesity Research. 2002;10:370–378. doi: 10.1038/oby.2002.51. [DOI] [PubMed] [Google Scholar]
- 6.Nielsen SJ, Popkin BM. Patterns and trends in food portion sizes, 1977–1998. JAMA. 2003;289:450–3. doi: 10.1001/jama.289.4.450. [DOI] [PubMed] [Google Scholar]
- 7.Brownell KD, Schwartz MB, Puhl RM, Henderson KE, Harris JL. The need for bold action to prevent adolescent obesity. J Adolesc Health. 2009;45:S8–17. doi: 10.1016/j.jadohealth.2009.03.004. Epub 2009 Jun 11. [DOI] [PubMed] [Google Scholar]
- 8.Krebs-Smith SM, Reedy J, Bosire C. Healthfulness of the U.S. food supply: little improvement despite decades of dietary guidance. Am J Prev Med. 2010;38:472–7. doi: 10.1016/j.amepre.2010.01.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.National Cancer Institute. [Accessed on December 17, 2009];Usual Dietary Intakes: Food Intakes, US Population, 2001–04. http://riskfactor.cancer.gov/diet/usualintakes/pop/
- 10.US Department of Agriculture. [Accessed on December 17, 2009];MyPyramid. http://www.mypyramid.gov.
- 11.US Department of Health and Human Service and US Department of Agriculture. Dietary Guidelines for Americans, 2005. 6. Washington D.C: US Government Printing Office; Jan, 2005. [Google Scholar]
- 12.Guenther PM, Reedy J, Krebs-Smith SM. Development of the Healthy Eating Index-2005. J Am Diet Assoc. 2008;108:1896–1901. doi: 10.1016/j.jada.2008.08.016. [DOI] [PubMed] [Google Scholar]
- 13.Basiotis PP, Guenther PM, Lino M, Britten P Center for Nutrition Policy and Promotion. Nutrition Insight 33, June 2006. [Accessed December 17, 2009];Americans consume too many calories from solid fat, alcohol, and added sugar. http://www.cnpp.usda.gov/Publications/NutritionInsights/Insight33.pdf.
- 14.National Center for Health Statistics. Dietary Interview, NHANES 2003–2006. [Accessed December 17, 2009];Public Data General Release File Documentation. http://www.cdc.gov/nchs/nhanes/about_nhanes.htm.
- 15.Subar AF, Krebs-Smith SM, Cook A, Kahle LL. Dietary sources of nutrients among US children, 1989–1991. Pediatrics. 1998;102:913–923. doi: 10.1542/peds.102.4.913. [DOI] [PubMed] [Google Scholar]
- 16.Subar AF, Krebs-Smith SM, Cook A, Kahle LL. Dietary sources of nutrients among US adults, 1989 to 1991. J Am Diet Assoc. 1998;98:537–547. doi: 10.1016/S0002-8223(98)00122-9. [DOI] [PubMed] [Google Scholar]
- 17.Cotton PA, Subar AF, Friday JE, Cook A. Dietary sources of nutrients among US adults, 1994 to 1996. J Am Diet Assoc. 2004;104:921–930. doi: 10.1016/j.jada.2004.03.019. [DOI] [PubMed] [Google Scholar]
- 18.Bachman JL, Reedy J, Subar AF, Krebs-Smith SM. Sources of food group intakes among the US population, 2001–2002. J Am Diet Assoc. 2008;108:804–814. doi: 10.1016/j.jada.2008.02.026. [DOI] [PubMed] [Google Scholar]
- 19. [Accessed December 17, 2009];MyPyramid Equivalents Database, version 2.0. http://www.ars.usda.gov/Services/docs.htm?docid=8498.
- 20.Troiano RP, Berrigan D, Dodd KW, Mâsse LC, Tilert T, McDowell M. Physical activity in the United States measured by accelerometer. Med Sci Sports Exerc. 2008;40:181–8. doi: 10.1249/mss.0b013e31815a51b3. [DOI] [PubMed] [Google Scholar]
- 21.Thompson FE, Dennison BA. Dietary sources of fats and cholesterol in US children aged 2 through 5 years. Am J Public Health. 1994;84:799–806. doi: 10.2105/ajph.84.5.799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Troiano RP, Briefel RR, Carroll MD, Bialostosky K. Energy and fat intakes of children and adolescents in the United States: data from the National Health and Nutrition Examination Surveys. Am J Clin Nutr. 2000;72:1343S–1353S. doi: 10.1093/ajcn/72.5.1343s. [DOI] [PubMed] [Google Scholar]
- 23.Guthrie JF, Morton JF. Food sources of added sweeteners in the diets of Americans. J Am Diet Assoc. 2000;100:43–51. doi: 10.1016/S0002-8223(00)00018-3. [DOI] [PubMed] [Google Scholar]
- 24.Nielsen S, Popkin B. Changes in beverage intake between 1977 and 2001. Am J Prev Med. 2004;27:205–210. doi: 10.1016/j.amepre.2004.05.005. [DOI] [PubMed] [Google Scholar]
- 25.Wang YC, Bleich SN, Gortmaker SL. Increasing caloric contribution from sugar-sweetened beverages and 100% fruit juices among US children and adolescents, 1988–2004. Pediatrics. 2008;121:e1604–e1614. doi: 10.1542/peds.2007-2834. [DOI] [PubMed] [Google Scholar]
- 26.Wang YC, Gortmaker SL, Sobol AM, Kuntz KM. Estimating the energy gap among US children: A Counterfactual Approach. Pediatrics. 2006;118:e1721–e1733. doi: 10.1542/peds.2006-0682. [DOI] [PubMed] [Google Scholar]
- 27.Swinburn B, Sacks G, Ravussin E. Increased food energy supply is more than sufficient to explain the US epidemic of obesity. Am J Clin Nutr. 2009;90:1453–6. doi: 10.3945/ajcn.2009.28595. [DOI] [PubMed] [Google Scholar]
- 28.Healthy Weight Commitment Foundation. [Accessed December 17, 2009]; http://www.healthyweightcommit.org/about.
- 29.General Mills Announces Plans to Reduce Sugar Content of Children's Cereals. [Accessed December 17, 2009]; http://www.rwjf.org/childhoodobesity/digest.jsp?id=26422.