Abstract
Previous studies of pediatric intracerebral hemorrhage have investigated isolated intraparenchymal hemorrhage. We investigated whether detailed assessment of intraventricular hemorrhage enhanced outcome prediction after intracerebral hemorrhage. We prospectively enrolled 46 children, full-term to 17 years, median age 2.7 years with spontaneous intraparenchymal hemorrhage and/or intraventricular hemorrhage. Outcome was assessed with the King’s Outcome Scale for Childhood Head Injury. Twenty-six (57%) had intraparenchymal hemorrhage, 10 (22%) had pure intraventricular hemorrhage, and 10 (22%) had both. There were 2 deaths, both with intraparenchymal hemorrhage + intraventricular hemorrhage volume ≥4% of total brain volume. Presence of intraventricular hemorrhage was not associated with poor outcome, but hydrocephalus showed a trend (p=0.09) toward poor outcome. In receiver operating characteristic curve analysis, combined intraparenchymal hemorrhage + intraventricular hemorrhage volume also showed a trend toward better outcome prediction than intraparenchymal hemorrhage volume alone. Although not an independent outcome predictor, future studies should assess intraventricular hemorrhage qualitatively and quantitatively.
Keywords: intracerebral hemorrhage, pediatric hemorrhage, intraparenchymal hemorrhage, intraventricular hemorrhage
Introduction
Stroke occurs in 2 to 13 per 100,000 children per year in the developed world.1,2 In a large pediatric study from a northern California health system, intracerebral hemorrhage had an incidence of 1.4 per 100,000 person-years.3 Spontaneous intracerebral hemorrhage accounts for about 50% of stroke in children whereas in adults it accounts for only about 15%. Intracerebral hemorrhage is comprised of intraparenchymal hemorrhage, intraventricular hemorrhage, and subarachnoid hemorrhage. In contrast to adults, intraparenchymal hemorrhage in children is rarely due to long standing hypertension and most often is due to vascular malformations.4 Given the distinct etiologies compared to adults and limited pediatric studies, intraparenchymal hemorrhage and intraventricular hemorrhage are incompletely understood in children. Additionally, intraventricular hemorrhage is rarely studied in children who are not premature infants. The strongest associations with outcome in pediatric intracerebral hemorrhage are intraparenchymal component of intracerebral hemorrhage ≥2% of total brain volume resulting in moderate disabilities and ≥4% resulting in severe disability.4,5 It is important to note that measures of hemorrhage volume in these studies only included intraparenchymal hemorrhage volume, therefore the relation of total hemorrhage (intraparenchymal hemorrhage + intraventricular hemorrhage) volume to outcome has not yet been studied. Additionally, previous pediatric studies categorized intraventricular hemorrhage as either present or absent and found no association of intraventricular hemorrhage with outcome. In adults with intracerebral hemorrhage the presence or absence of intraventricular hemorrhage, the intraventricular hemorrhage volume, and scores rating the severity of intraventricular hemorrhage have all been shown to add to outcome prediction models after intracerebral hemorrhage.6 In the current study, intraventricular hemorrhage was systematically analyzed by manual volumetric analysis. We also used an intraventricular hemorrhage scoring system developed by Hijdra7 et al. Since previous retrospective5 and prospective4 pediatric studies on outcome prediction in pediatric intracerebral hemorrhage did not assess intraventricular hemorrhage volume, intraventricular hemorrhage distribution, or investigate intraventricular hemorrhage scores, an association of intraventricular hemorrhage with outcome may not have been appreciated. Our primary goal was to investigate whether the inclusion of intraventricular hemorrhage volume and/or an intraventricular hemorrhage score, rather than simply dichotomizing intraventricular hemorrhage as present or absent, enhanced our ability to predict poor outcome.
Methods
Participants
Children, full-term newborns, 37 weeks to 17 years, with spontaneous intraparenchymal hemorrhage with or without concomitant IVH or with isolated IVH confirmed on CT or MRI were included. With parental informed consent, subjects were prospectively enrolled from 2007–2009 in an Institutional Review Board approved study at two large tertiary care centers. Exclusion: trauma; isolated subarachnoid hemorrhage; intracerebral hemorrhage due to brain tumor; hemorrhagic transformation of arterial ischemic stroke or cerebral venous sinus thrombosis.
Intraventricular Hemorrhage Assessments
Volumetric analysis of total brain volume, intraparenchymal hemorrhage volume, and IVH volume was performed by 2 raters using ImageJ as previously described (http://rsb.info.nih.gov/ij/download.html) on the initial imaging study.5, 8 Total brain volume included the cerebral hemispheres, cerebellum, and brainstem. Ventricular volume was not subtracted from the total brain volume so that total brain volume would not vary with hydrocephalus. Values obtained by manual segmentation tracing were the reference criterion. Both intracerebral hemorrhage and intraventricular hemorrhage volume were expressed as a percent of total brain volume.4, 5, 8 We used the intraventricular hemorrhage score to estimate intraventricular hemorrhage severity for use as a possible bedside method for aiding outcome prediction.8, 9 An intraventricular hemorrhage score was assigned independently by 2 raters using the Hijdra scheme to quantify intraventricular hemorrhage size in the right lateral, left lateral, 3rd, and 4th ventricles.7 Hemorrhage in each ventricle was scored as 0 points for no blood, 1 point for posterior sedimentation of blood, 2 points for a partly filled ventricle, and 3 points for a completely filled ventricle (total score range 0–12 points).
Outcome assessment
Children were assessed at follow-up by a pediatric stroke neurologist with the King’s Outcome Scale for Childhood Head Injury (KOSCHI).10 The KOSCHI incorporates functional impairments as well as periodic symptoms like headaches and seizures. Scores are 1 for death, 2 for vegetative state, 3a and 3b for severe disability (3a worse), 4a and 4b for moderate disability (4a worse), and 5a and 5b for good recovery (5b full recovery, no residual symptoms). Poor outcome was defined as KOSCHI <4.
Statistical Analysis
Inter-rater reliability for intraventricular hemorrhage score estimation was measured with a weighted kappa statistic. A kappa >0.8 is considered excellent.11 Linear regression was performed to determine the correlation of the estimated measure of intraventricular hemorrhage, the intraventricular hemorrhage score, with the volumetric measures. Since values were not normally distributed, data were log transformed. The regression analysis was clustered by patient since the two ratings for each patient were not independent, and the parameter R2 was reported as the result. The intraventricular hemorrhage score was added to a logistic regression model for prediction of poor outcome. Outcome prediction using intraparenchymal hemorrhage volume was compared to intraparenchymal hemorrhage + intraventricular hemorrhage volume using receiver operating characteristic curves. Categorical comparisons were performed using χ2. A two-sided p-value of <0.05 was considered statistically significant. Statistical analysis was performed using STATA version 11.0 (Stata Corp, College Station, TX).
Results
We enrolled 46 children, mean age 6.2 ± 6.4 years and median age 2.7 years (range 0–17.3 years). Twenty-four (52%) were male. Fifteen participants (33%) were less than one year of age, including 10 (22%) neonates (<30 days old). Racial distribution was 31 (67%) Caucasian, 14 (31%) Black or African American, and 1 (2%) South Asian. One Caucasian child was Hispanic. All children were neurologically normal before the hemorrhage. Mean intraparenchymal hemorrhage was 1.59% of total brain volume, mean intraventricular hemorrhage was 0.77% of total brain volume, and mean intraparenchymal hemorrhage + intraventricular hemorrhage volume was 2.33% of total brain volume. Patient characteristics and follow-up KOSCHI scores are presented in Table 1.
Table 1.
Demographics
| Demographics and Patient Characteristics | Full patient population N=46 (mean ± std) | Patients with KOSCHI 1 (N=2) | Patients with KOSCHI 3 (N=2) | Patients with KOSCHI 4 (N=21) | Patients with KOSCHI 5 (N=21) |
|---|---|---|---|---|---|
| Age in years | 6.2 ± 6.4 | 0 years & 15.2 | 0.4 & 14.2 | 6.3 ± 6.0 | 5.8 ± 6.6 |
| Intracerebral hemorrhage volume as a % of total brain volume | 1.6% ± 2.6% | 0% % 14.49% | 8.74% & 2.28 | 1.23% ±1.41% | 0.83% ± 1.15% |
| Intraventricular hemorrhage volume as a % of total brain volume | 0.77% ± 1.84% | 4.29% & 0.68% | 0% & 0% | 0.59% ± 1.55% | 0.85% ± 2.13% |
| Total Hemorrhage volume as a % of total brain volume | 2.33% ± 2.98% | 4.29% & 15.17% | 8.74% & 2.28 | 1.94% ±2.01% | 1.72% ± 2.20% |
| Hydrocephalus | 30% (N=14) | 50% (N=1) | 50% (N=1) | 43% (N=9) | 14% (N=3) |
| Ethnicity | |||||
| Caucasian | 65% | ||||
| African American | 30% | ||||
| Hispanic | 2% | ||||
| South Asian | 2% | ||||
| Herniation (N=11) | 24% | ||||
| Transtentorial or Uncal 73% (N=8) | 17% | 100% | 100% | 19% | 0% |
| Cinculate 27% (N=3) | 7% | 0% | 0% | 9% | 5% |
| Locations | |||||
| Supratentorial (N=44) | 93% | 100% | 100% | 86% | 100% |
| Infratentorial (N=3) | 7% | 0% | 0% | 14% | 0% |
| Altered Mental Status at presentation | 41% | 50% | 50% | 48% | 33% |
The full cohort is shown in column one, additional colums are the characteristics (mean ± SD) of patients based on their final outcome [KOSCHI 1 (death) to KOSCHI 5 (good outcome)]. One patient had both supratentorial and infratentorial intraparenchymal hemorrhage.
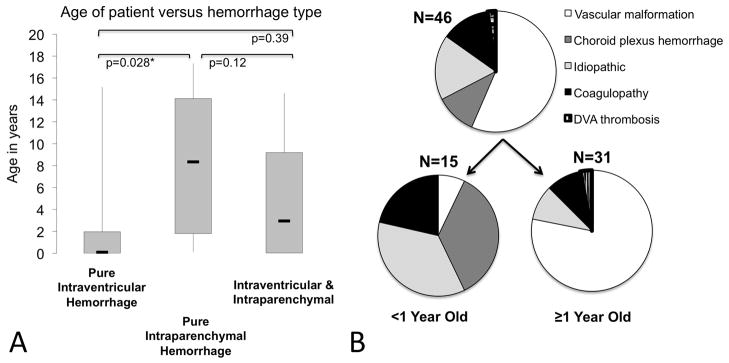
Intraventricular Hemorrhage Characteristics
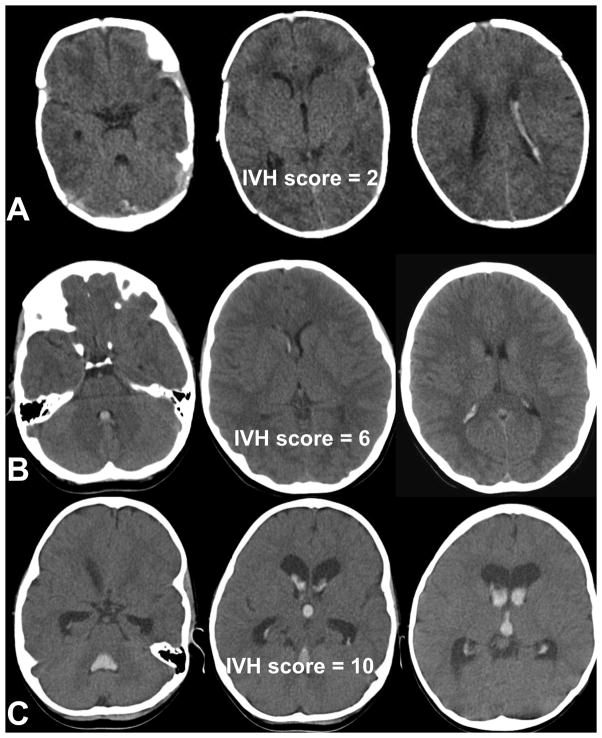
Isolated intraparenchymal hemorrhage occurred in 26 (56%) patients, 10 (22%) had isolated intraventricular hemorrhage, and 10 (22%) had both. The mean and median ages at presentation among children with isolated intraventricular hemorrhage (2.8 ± 5.3 years, median 0.1 year), isolated intraparenchymal hemorrhage (mean 8.3 ± 6.7 years, median 8.4 years), and concomitant intraventricular hemorrhage and intraparenchymal hemorrhage (4.7 ± 5.2 years, median 2.95 years) are shown in Figure 2A. Using analysis of variance a difference was found between groups (p=0.05). Using t-tests, patients with pure intraventricular hemorrhage were younger than those with pure intraparenchymal hemorrhage [Figure 2A] mean 2.8 ± 5.3 years, median 0.1 year versus mean 8.3 ± 6.7 years, median 8.4 years, p=0.03). Those with both intraparenchymal hemorrhage and intraventricular hemorrhage were of intermediate age (mean 4.7 ± 5.2 years, median 2.95 years) but not statistically different from either group. Patients younger than one-year-old primarily had choroid plexus or idiopathic hemorrhages (72%), whereas children older than one year primarily had hemorrhages related to vascular malformations (75%) (Figure 2B, χ2 =16.89, p<0.0001). Three patients (7%) had some infratentorial hemorrhage. Intraventricular hemorrhage volumes ranged from 0.1–63.8cm3, corresponding to 0.3–19% of total brain volume, and intraventricular hemorrhage scores ranged from 0–11 (Figure 1). Weighted kappa statistic for intraventricular hemorrhage score agreement between raters was 0.84 (95%CI: 0.77 – 0.86), and absolute agreement was 94.5%. Intraventricular hemorrhage score and manual intraventricular hemorrhage volume correlation was fair, R2=0.42 (β=1.11, 95%CI: 0.04– 2.19, p=0.04). Presence of hydrocephalus was associated with a trend for poorer outcome (p=0.09).
Figure 2.
Age of patients versus hemorrhage type (A), hemorrhage etiology of the cohort and separated by age of subject (B).
Figure 1.
Representative IVH scores of 2 (A), 6 (B), and 10 (C).
Intraventricular hemorrhage score was added to a logistic regression model for predicting poor outcome. The only statistically significant predictor of poor outcome was intraparenchymal hemorrhage volume in both univariate and multivariate analysis. In our multivariate model, we attempted to adjust for age >1, presence of intraventricular hemorrhage, high intraventricular hemorrhage score, and high intraventricular hemorrhage volume, but these were not statistically significant. Since only 20 of the 46 children in this sample had intraventricular hemorrhage, a power calculation was performed. Overall, we had only 54% power to detect a difference in good versus poor outcome for those with a large intraparenchymal hemorrhage (≥4% of total brain volume) compared to those with intraparenchymal hemorrhage <4% of total brain volume. Power increased to 59% when the presence of intraventricular hemorrhage was added to large intraparenchymal hemorrhage (7 of 20 children with intraventricular hemorrhage also had a large intraparenchymal hemorrhage). We did detect a difference in outcome between children with intraparenchymal hemorrhage volume ≥4% of total brain volume versus <4% of total brain volume, but our power to detect the additive effect of intraventricular hemorrhage was limited.
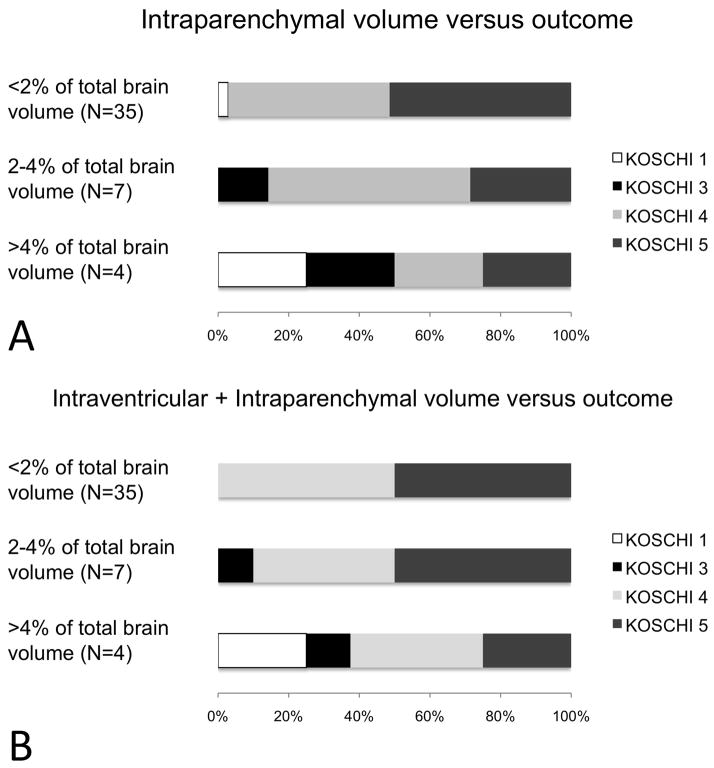
Patient Outcomes
Patient outcomes are presented in Figure 3. As previously shown,4, 5 patients with larger hemorrhages did poorly. In our cohort, 11 (24%) had intraparenchymal hemorrhage ≥2% of total brain volume and 4 had intraparenchymal hemorrhage ≥4% of total brain volume. When total hemorrhage volume (intraparenchymal hemorrhage + intraventricular hemorrhage) was analyzed, 18 (39%) had hemorrhage ≥2% of total brain volume and 8 had hemorrhage ≥4% of total brain volume. Four children had KOSCHI <4 at their last follow-up, at a median of 10 months (range 1–28 months) from the acute hemorrhage (Figure 2). There were 2 deaths, both in children with intraparenchymal hemorrhage + intraventricular hemorrhage volume ≥4% of total brain volume, intraventricular hemorrhage scores were both 9, and each had herniation. Most children with intraparenchymal hemorrhage volume ≥2% of total brain volume have moderate disabilities and those with ≥4% have severe disability.4.5 When placing children in this cohort into 3 categories of hemorrhage volume (intraparenchymal hemorrhage <2%, ≥2%−4%, or ≥4% total brain volume), a volume-dependent relationship with outcome is apparent (Figure 3A). However, some patients predicted to have good outcomes based on intraparenchymal hemorrhage volume alone had poor outcomes (Figure 3A). For example, patients with small intraparenchymal hemorrhage volumes <2% of total brain volume but large intraventricular hemorrhage ≥4% of total brain volume are classified as having large hemorrhage when both intraparenchymal hemorrhage + intraventricular hemorrhage volume are considered (Figure 3B). Using the combined intraparenchymal hemorrhage + intraventricular hemorrhage volume, these children are predicted to have poor outcome, whereas they are predicted to have good outcome if only the smaller intraparenchymal hemorrhage volume were taken into account (Figure 3A versus 3B). The point estimate and 95% confidence interval in receiver operating characteristic curves analysis was higher for predicting poor outcome (KOSCHI <4) using intraparenchymal hemorrhage + intraventricular hemorrhage versus intraparenchymal hemorrhage volume alone (area under curve 0.88, 95% CI: 0.74–1.00 versus 0.74, 0.37–1.0, p=0.81). Intermediate outcomes could not be predicted with both high sensitivity and specificity using either intraparenchymal hemorrhage volume or intraparenchymal hemorrhage + intraventricular hemorrhage volume.
Figure 3.
KOSCHI score versus hemorrhage volume (A) intraparenchymal hemorrhage as a percent of total brain volume (B) intraparenchymal hemorrhage + intraventricular hemorrhage as a percent of total brain volume.
Discussion
This study offers a detailed analysis of intraventricular hemorrhage in a prospectively enrolled pediatric population with intraparenchymal and intraventicular hemorrhage. Including intraventricular hemorrhage volume in addition to intraparenchymal hemorrhage volume may provide additional prognostic information. To illustrate this point, one patient with intraparenchymal hemorrhage with intraventricular hemorrhage would have been categorized as having hemorrhage ≤2% total brain volume when only accounting for the intraparenchymal hemorrhage, and one would expect a good outcome. However, when the intraventricular hemorrhage was taken into account, the intraparenchymal hemorrhage +intraventricular hemorrhage volume was ≥4% of total brain volume, and total hemorrhage volume correctly predicted a poor outcome since this patient subsequently died (Figure 3A vs B). Additional studies with larger sample size are needed to clarify whether presence of intraventricular hemorrhage, degree of intraventricular hemorrhage, and/or presence of hydrocephalus are independent predictors of poor outcome. Additionally, the method in which hemorrhage intraventricular hemorrhage is assessed is critical to consider for future studies. The correlation between the intraventricular hemorrhage score and manual intraventricular hemorrhage volume was only fair, likely because the intraventricular hemorrhage score values blood in each ventricle equally. For example, a small volume of blood completely filling the 3rd or 4th ventricle is weighted the same as a larger volume of blood completely filling a lateral ventricle, both have an intraventricular hemorrhage score of three. Logically, a small volume of blood in the 3rd and/or 4th ventricles may be clinically relevant in children, as it may rapidly produce hydrocephalus. At the present time, both the intraventricular hemorrhage score and the intraventricular hemorrhage volume are worthy of further study in children. Our study suggests that younger children are most likely to present with isolated intraventricular hemorrhage (not due to vascular malformations), a finding that has not been reported outside of the preterm neonatal population. 12, 13
In comparison to adult studies, this sample is small, yet it represents the largest prospective pediatric spontaneous intracerebral hemorrhage study to date. Despite collaboration between two large tertiary children’s medical centers, we still faced sample size issues however, with only a 59% power to detect a statistically significant difference in outcome, we saw a trend for poorer outcome in patients with hydrocephalus.
Conclusions
In this cohort, presence of intraventricular hemorrhage, volume of intraventricular hemorrhage, and intraventricular hemorrhage score were not independent predictors of poor outcome. Methodologically, intraventricular hemorrhage volume and intraventricular hemorrhage score can be systematically assessed in prospective studies since intraventricular hemorrhage may contribute to poor outcome through the appearance of hydrocephalus. Hemorrhage etiologies exist in different proportions based upon age. Our data may provide a helpful model for future studies investigating intraventricular hemorrhage in children although further research is needed to characterize intraventricular hemorrhage and to refine outcome prediction models.
Acknowledgments
This work was conducted at the Johns Hopkins Hospital and the Children’s Hospital of Philadelphia. This study was presented as an abstract at the International Stroke Conference in February, 2011.
Funding:
JTK is supported by the Stanford School of Medicine Medical Scholars program. LAB is supported by the National Institutes of Health (T32-NS007413) and by the L. Morton Morley Funds of The Philadelphia Foundation. RNI is supported by the National Institute of Neurologic Disease and Stroke (NINDS; R01-NS050488, K23-NS062110). DJL is supported by the NINDS (K23-NS052380), Dana Foundation, and Wolfson Fund for Neurologic Research. SES is supported by a grant from the NINDS (K12-NS049453). LCJ is supported by a grant from the NINDS (K23-NS062110).
This study was approved by each local institutional review board, and patients’ guardians provided written informed consent for the above study.
This work was performed at The Johns Hopkins University School of Medicine, Stanford University School of Medicine, and The Children’s Hospital of Philadelphia. These data were presented in abstract form at the 2011 International Stroke Conference.
Footnotes
Conflicts of Interest/Disclosures:
Drs. Ichord and Jordan are members of the Clinical Event Committee for the Berlin Heart trial for pediatric ventricular assist devices. None of the other authors has any financial disclosures related to the current study.
Author Contributions:
Jonathan Kleinman conceived the idea, analyzed data, drafted the manuscript, and interpreted the results. Kyle Englemann, Lauren Beslow, Sabrina Smith, Daniel Licht, and Rebecca Ichord collected data and critically revised the manuscript. Lori Jordan conceived the idea, collected and analyzed data, drafted the manuscript, and critically revised the manuscript. All authors had access to the data prior to submission.
References
- 1.Fullerton H, Wu Y, Zhao S, Johnston S. Risk of stroke in children: Ethnic and gender disparities. Neurology. 2003;61:189–194. doi: 10.1212/01.wnl.0000078894.79866.95. [DOI] [PubMed] [Google Scholar]
- 2.Giroud M, Lemesle M, Nivelon J, Milan C, Dumas R. Cerebrovascular disease in children under 16 years of age in the city of dijon, france: A study of incidence and clinical features from 1985 to 1993. Journal of Clinical Epidemiology. 1995;48:1343–1348. doi: 10.1016/0895-4356(95)00039-9. [DOI] [PubMed] [Google Scholar]
- 3.Jordan LC, Johnston S, Wu Y, Sidney S, Fullerton H. The importance of cerebral aneurysms in childhood hemorrhagic stroke: A population-based study. Stroke. 2009;40:400–405. doi: 10.1161/STROKEAHA.108.518761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Beslow L, Lintracerebral hemorrhaget DJ, Smith SE, Storm PB, Heuer GG, Zimmerman RA, Feiler AM, Kasner SE, Intracerebral hemorrhageord RN, Jordan LC. Predictors of outcome in childhood intracerebral hemorrhage: A prospective consecutive cohort study. Stroke. 2010;41:313–318. doi: 10.1161/STROKEAHA.109.568071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Jordan LC, Kleinman JT, Hillis AE. Intracerebral hemorrhage volume predicts poor neurologic outcome in children. Stroke. 2009;40:1666–1671. doi: 10.1161/STROKEAHA.108.541383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hallevi H, Albright K, Aronowski J, Barreto AD, Martin-Schild S, Khaja A, Gonzales NR, Illoh K, Noser E, Grotta JC. Intraventricular hemorrhage: Anatomic relationships and clinical implications. Neurology. 2008;70:848–852. doi: 10.1212/01.wnl.0000304930.47751.75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hijdra A, Brouwers P, Vermeulen M, van Gijn J. Grading the amount of blood on computed tomograms after subarachnoid hemorrhage. Stroke. 1990;21:1156–1161. doi: 10.1161/01.str.21.8.1156. [DOI] [PubMed] [Google Scholar]
- 8.Kleinman JT, Hillis AE, Jordan LC. Abc/2: Estimating intracerbral haemorrhage volume and total brain volume, and predicting outcome in children. Developmental Medicine and Child Neurology. 2011;53:281–284. doi: 10.1111/j.1469-8749.2010.03798.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Beslow L, Intracerebral hemorrhageord RN, Kasner SE, Mullen M, Lintracerebral hemorrhaget DJ, Smith SE, Storm PB, Jordan LC, Messé S. Abc/xyz estimates intracerebral hemorrhage volume as a percent of total brain volume in children. Stroke. 2010;41:691–694. doi: 10.1161/STROKEAHA.109.566430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Crouchman M, Rossiter L, Colaco T, Forsyth R. A practical outcome scale for paediatric head injury. Archives of Disease in Childhood. 2001;84:120–124. doi: 10.1136/adc.84.2.120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Landis RJ, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1977;33:159–174. [PubMed] [Google Scholar]
- 12.Rosenthal R. The “file drawer problem” and tolerance for null results. Psychological bulletin. 1979;86:638–641. [Google Scholar]
- 13.Dickersin K, Min Y. Publication bias: The problem that won’t go away. Annals of the New York Academy of Science. 1993;703:135–146. doi: 10.1111/j.1749-6632.1993.tb26343.x. [DOI] [PubMed] [Google Scholar]