Abstract
Little is known about the immunological and virological impact of diagnosis disclosure among HIV-positive children and adolescents. The current cross-sectional study examined medication hiding as a mediator of the relationship between disclosure to friends and three medical outcomes: CD4+ absolute count, CD4+ percentage, and viral load. Participants included 25 perinatally-infected, HIV-positive children and adolescents ages 11 to 18 years from the U.S. Diagnosis disclosure and medication hiding were self-reported by participants and medical markers were derived from blood samples drawn during the same clinic visit. Bootstrapping analyses revealed that disclosure to at least one friend (versus no friends) was associated with less medication hiding, which was associated with higher CD4+ absolute counts and percentages but not viral load. Further, among the subset of participants who had disclosed to at least one friend (n=19), those who reported disclosing to 11 or more versus 1–10 friends were less likely to hide medication taking, which was associated with higher CD4+ absolute counts. Findings suggest HIV-positive children and adolescents’ diagnosis disclosure to friends corresponds to less medication hiding, ultimately yielding better immune functioning. Health care providers should be cognizant of these potential medical benefits associated with disclosure when offering support around disclosure decision-making.
Keywords: pediatric HIV, disclosure, HAART, medical functioning
Introduction
Due to the negative stigma attached to being HIV-positive and consequent risks associated with serostatus disclosure, many HIV-positive people are selective about revealing their diagnosis, sometimes concealing it even from family and friends (Rao, Kekwaletswe, Hosek, Martinez, & Rodriguez, 2007). Unlike disclosure decisions faced by people with behaviorally-acquired HIV disease, disclosure by perinatally-infected, HIV-positive children and adolescents (PHCA) is uniquely embedded in a familial context. These PHCA may face family pressure to maintain secrecy, given that diagnosis disclosure simultaneously exposes the serostatus of their biological mother and raises questions about other family members’ serostatus if mode of infection is revealed or assumed (Vreeman et al., 2010). Thus, PHCA may lack full autonomy over the decision to share their diagnosis. Consequently, PHCA may disclose to fewer friends than their behaviorally-infected counterparts (Abramowitz et al., 2009).
Maintenance of serostatus secrecy requires not only verbal self-restraint but also behavioral accommodations, such as concealing medication and medication-taking activities. In a U.S. sample of HIV-positive youth, Rao et al. (2007) found that many participants reported skipping doses and hiding their medication for fear friends or family might discover their serostatus. Such behavior has dangerous implications for disease management. Highly active antiretroviral therapy (HAART) necessitates strict adherence to slow disease progression (Kitahata et al., 2004) and involves not only medication dosage, but also dose timing. To the extent that patients’ efforts to conceal their serostatus alter dose taking and timing, such behavior could be detrimental to their health. Thus, opting not to disclose to friends could indirectly compromise PHCA’s medical functioning.
To date, research examining peer disclosure among PHCA relative to medical outcomes is limited and has yielded mixed results (e.g., Lam, Naar-King, & Wright, 2007; Wiener & Battles, 2006; Sherman, Bonanno, Wiener, & Battles, 2000). The current study sought to examine medication hiding as a mediator of the relationship between peer disclosure and multiple markers of medical functioning among PHCA. We hypothesized that participants who had disclosed their serostatus to 1+ friend(s) would report less medication hiding, which would relate to better medical functioning (see Table 1). A secondary objective, contingent on finding a significant indirect effect, was to explore the implications of number of friends disclosed to for medication hiding and medical functioning.
Table 1.
Sociodemographic and Medical Characteristics of Sample (N=25)
| Characteristic | n (%) |
|---|---|
| Sex | |
| Male | 13 (52%) |
| Female | 12 (48%) |
| Age | |
| 11–14 years | 13 (52%) |
| 15–18 years | 12 (48%) |
| Race | |
| African American | 14 (56%) |
| White | 8 (32%) |
| Hispanic | 1 (4%) |
| Native American | 1 (4%) |
| Other | 1 (4%) |
| Preferred Language | |
| English | 25 (100%) |
| Recency of HAART initiation | |
| 5 years ago | 3 (12%) |
| 6 years ago | 8 (32%) |
| 7 years ago | 14 (56%) |
| HAART Dosing Schedule | |
| 2 doses/day | 22 (88%) |
| 3 doses/day | 3 (12%) |
| Caregiver Educationa | |
| Less than high school diploma (<12 years) | 2 (8%) |
| Completed high school or trade school (12 years) | 7 (29%) |
| Some college (13–15 years) | 9 (28%) |
| Completed college (16 years) | 5 (21%) |
| Graduate education (17+ years) | 1 (4%) |
| Caregiver HIV Statusb | |
| Positive | 6 (24%) |
| Negative | 19 (76%) |
| Caregiver Relationship | |
| Biological | 9 (36%) |
| Non-biological | 16 (64%) |
Reported for subset of participants for whom data were available (n=24); In 2-parent households (n=11), years of education were averaged
In 2-parent households (n=11), caregiver HIV status was considered positive if at least one parent was HIV-positive
Methods
Participants
The sample was comprised of 25 PHCA from across the U.S. who were enrolled on a medical protocol at a government research institute via referral by their local medical providers. Patients were eligible for this substudy if they were aware of their serostatus and actively being prescribed HAART.
Measures
Diagnosis disclosure
Participants’ disclosure of their serostatus to friends was assessed with one item: “How many of your friends are aware of your HIV diagnosis?” Response options were “None,” “1–3,” “4–10,” and “11 or more.” For the primary analyses with the full sample, the latter three options were combined to form an “any disclosure” subgroup that was compared to the “no disclosure” subgroup. Alternate category combinations were used to dichotomize the variable (1–3 vs. 4+ and 1–10 vs. 11+) in subsequent exploratory analyses.
Medication hiding
The extent to which participants concealed medication-taking from friends was assessed with one item: “Do you hide the fact that you take medication from your friends?” Response options ranged from “Not at all” (1) to “Very much” (4), with higher scores indicating greater hiding.
Medical functioning
Medical markers of HIV disease status included HIV1 RNA copies/ml (viral load), CD4+ absolute cell counts, and CD4+ percentages.
Background characteristics
Patients and caregivers completed a background form regarding sociodemographic and medical characteristics.
Procedure
Eligible patients and their caregivers were approached during outpatient clinic visits for their primary medical protocol and invited to participate in this substudy. Questionnaire and medical data were obtained during the same visit. All study procedures received IRB approval.
Analyses
Analyses were performed using SPSS (PASW 18.0.3). Pearson correlations were conducted to explore bivariate relationships between medication hiding and medical variables. Bootstrapping was used to test medication hiding as a mediator between disclosure and medical functioning. Preacher and Hayes’ (2011) INDIRECT macro was used to generate 5000 bootstrapped samples, from which bias-corrected and accelerated confidence intervals were established to estimate indirect effects.
Results
Sample Characteristics
Of the 38 patients invited to participate, 30 enrolled and 25 completed the questionnaire and blood draw. The final sample was comprised of 25 PHCA (Mage=15.08 years, SD=1.82). Additional characteristics are presented in Tables 1–3.
Table 3.
Amount of Medication Hiding Reported by Sample (N=25)
| n (%) | |
|---|---|
| Not at all | 10 (40%) |
| A little | 2 (8%) |
| Somewhat | 5 (20%) |
| Very much | 8 (32%) |
Descriptive and Correlational Analyses
Medians, means, and standard deviations of all medical functioning variables are presented in Table 2. PCR analyses revealed that seven patients (28%) had an undetectable viral load (HIV-1 RNA PCR <50 copies/ml). Among the remainder (n=18), viral loads ranged from 1.69–6.07 log10 copies/ml. CD4+ absolute counts ranged from 96-2734 cells/µl and CD4+ percentages ranged from 7–45%. Medication hiding was significantly correlated with CD4+ counts and percentages, but not viral load. (See Table 4.)
Table 2.
Disclosure Characteristics Reported by Sample (N=25)
| Number of Friends Disclosed To | n (%) |
|---|---|
| 0 friends | 6 (24%) |
| 1–3 friends | 8 (32%) |
| 4–10 friends | 3 (12%) |
| 11+ friends | 8 (32%) |
Table 4.
Summary of Intercorrelations, Means, and Standard Deviations for Medication Hiding and Medical Functioning Variables
| 1 | 2 | 3 | 4 | Mdn | M | SD | ||
|---|---|---|---|---|---|---|---|---|
| 1 | Medication Hiding | 1.00 | 0.25 | −0.41** | −0.65*** | 3.00 | 2.44 | 1.33 |
| 2 | Viral Load (log10 copies/ml) | - | 1.00 | −0.32 | −0.52** | 3.41 | 3.29 | 1.44 |
| 3 | CD4+ Count (cells/µl) | - | - | 1.00 | .61** | 571.00 | 654.52 | 592.97 |
| 4 | CD4+ Percentage | - | - | - | 1.00 | 25.00 | 27.64 | 11.73 |
p < 0.05.
p < 0.01.
p < 0.001.
Testing for Indirect Effects
Bootstrapping analyses indicated significant indirect effects of disclosure on medical functioning via medication hiding for both CD4+ absolute counts and percentages (95% CIs [70.07, 929.92], [3.58, 18.38], respectively) but not viral load. These results suggested that disclosure to 1+ friend(s) versus none was associated with less medication hiding, which was associated with higher CD4+ absolute counts and percentages.
Follow-up analyses were conducted with the 19 participants who had disclosed their diagnosis to 1+ friend(s) to explore the implications of number of friends disclosed to. A significant indirect effect emerged when disclosure was dichotomized as 1–10 versus 11+ friends; participants who reported disclosing to 11+ friends (n=8) were less likely to hide medication-taking, which was associated with higher CD4+ absolute counts (95% CIs [51.14, 1313.93]). No other significant indirect effects emerged.
Discussion
Despite HIV disease’s evolution towards a more mainstream, manageable illness, PHCA continue to maintain secrecy surrounding their diagnosis; most of our participants reported some degree of medication hiding and nearly a quarter refrained from disclosing to any friends. PHCA who disclosed their serostatus to 1+ friend(s) were less likely to hide taking medication, which was associated with better immunological status (higher CD4+ absolute counts and percentages). Further, disclosing to 11+ versus 1–10 friend(s) was linked to less medication hiding, which was related to higher CD4+ absolute counts.
These findings lend support to others’ recommendations for openness with friends and families given reported psychosocial benefits (e.g., peer social support; Battles & Wiener, 2002). Further, diagnosis concealment becomes increasingly difficult for older adolescents as their time and intimacy with peers intensifies (Kang, Mellins, Ng, Robinson, & Abrams, 2008). Thus, healthcare providers should consider the potential psychosocial and medical benefits associated with disclosure and patients’ developmental stage when offering support. However, providers should also recognize the persistence of HIV-related stigma and the psychological risks associated with disclosure, particularly to acquaintances (Lam et al., 2007) or the public (Battles & Wiener, 2002). Our results suggest that disclosing to a larger circle of friends (11+) corresponds to less medication hiding, which could offer immunological benefit. A more detailed investigation is needed to determine whether this effect holds with disclosure to larger social circles or whether an optimal, intermediary level of disclosure exists for physical wellbeing as it does for psychological wellbeing. In the interim, providers should encourage PHCA to disclose to friends, but to do so selectively.
Despite the indirect effect found between disclosure and CD4+ values, we did not find a parallel effect with viral load as an outcome; thus, our hypothesis was only partially supported. Also, medication hiding and viral load were not significantly correlated. This may suggest that certain aspects of medical functioning (e.g., immune status) are more sensitive to dose timing than others (e.g., viral suppression).
Given the cross-sectional nature and small sample size of the current study, we present these findings as preliminary support for the relationship of peer disclosure to medication hiding and medical functioning. Limitations include vulnerability to social desirability bias, the term “friends” being subject to participants’ interpretation, and disclosure being operationalized as friends’ awareness versus participants’ own willful action (friends could be “aware of” diagnosis due to caregiver’s disclosure). Additionally, we were unable to include medication adherence in the hypothesized pathway. While we speculate that low medication-hiding implies better adherence since patients could take medications at scheduled times regardless of their company, it also may correspond to worse adherence, since non-adherent individuals have nothing to hide. Finally, given our small, U.S.-based sample, the generalizability of our findings to other PHCA nationally and internationally is limited.
Future research is warranted to establish causality within the hypothesized pathway and to investigate viral load more fully as an outcome. To support our behavioral explanation for the link between disclosure and medical functioning, adherence should be measured directly and examined as a mediator between medication hiding and medical outcomes using a larger sample. Additionally, quantitative and qualitative methods assessing other dimensions of disclosure besides number of friends disclosed to (e.g., closeness and duration of friendships, proportion of friends disclosed to, circumstances surrounding disclosure act, other persons disclosed to) would allow for a richer understanding of the association between disclosure and medication-related behavior.
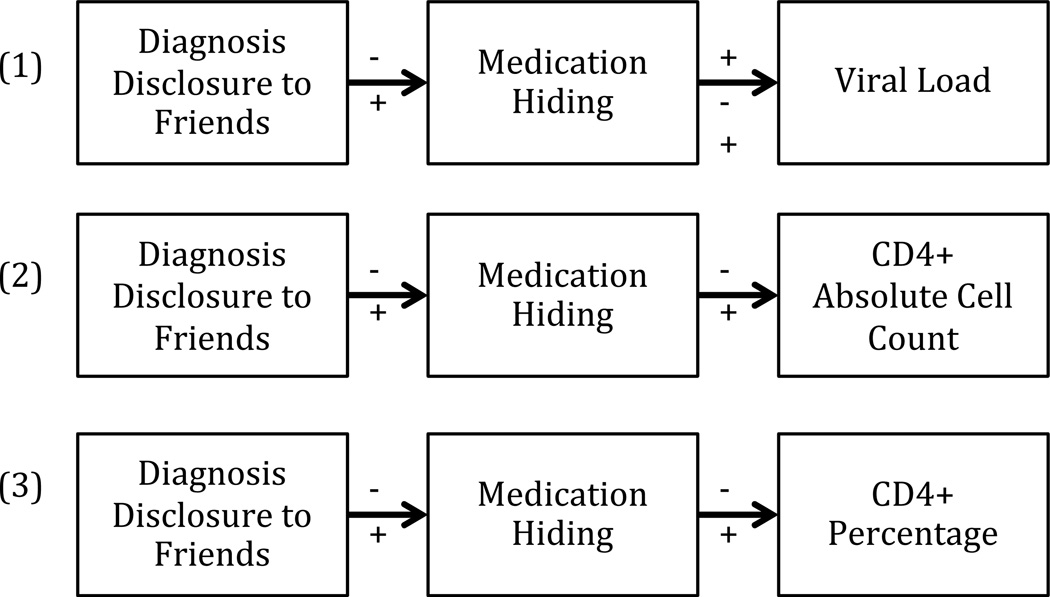
Figure 1.
Hypothesized model of the indirect effects of diagnosis disclosure to friends on medical functioning via medication hiding. Medical functioning was operationalized in three different ways: (1) Viral load (HIV1 RNA log10 copies/ml), (2) CD4 + absolute cell count (cells/µl), and (3) CD4 + percentage of total lymphocytes.
Acknowledgements
This research was supported by the Intramural Research Program of the National Institutes of Health, National Cancer Institute, Center for Cancer Research, as well as Federal Contracts HHSN261200477004C with the Medical Illness Counseling Center and HHSN261200800001E with SAIC-Frederick, Inc. Sarah K. Calabrese was supported by Grant Number F31-MH085584 from the National Institute of Mental Health. The content of this publication does not necessarily reflect the views or policies of the Department of Health and Human Services, nor does mention of trade names, commercial products, or organizations imply endorsement by the U.S. Government. The authors report no proprietary or commercial interest in any product mentioned or concept discussed in this article.
References
- Abramowitz S, Koenig LJ, Chandwani S, Orban L, Stein R, LaGrange R, Barnes W. Characterizing social support: Global and specific social support experiences of HIV-infected children and adolescents. AIDS Patient Care STDS. 2009;23(5):323–330. doi: 10.1089/apc.2008.0194. [DOI] [PubMed] [Google Scholar]
- Battles HB, Wiener LS. From adolescence through young adulthood: Psychosocial adjustment associated with long-term survival of HIV. Journal of Adolescent Health. 2002;30:161–168. doi: 10.1016/s1054-139x(01)00341-x. [DOI] [PubMed] [Google Scholar]
- Kang E, Mellins CA, Ng WYK, Robinson L, Abrams EJ. Standing between two worlds in Harlem: A developmental psychopathology perspective of perinatally acquired human immunodeficiency virus and adolescence. Journal of Applied Developmental Psychology. 2008;29:227–237. [Google Scholar]
- Kitahata MM, Reed SD, Dillingham PW, Van Rompaey SE, Young AA, Harrington RD, Holmes KK. Pharmacy-based assessment of adherence to HAART predicts virologic and immunologic treatment response and clinical progression to AIDS and death. International Journal of STD & AIDS. 2004;15(12):803–810. doi: 10.1258/0956462042563666. [DOI] [PubMed] [Google Scholar]
- Lam PK, Naar-King S, Wright K. Social support and disclosure as predictors of mental health in HIV-positive children and adolescents. AIDS Patient Care STDS. 2007;21(1):20–29. doi: 10.1089/apc.2006.005. [DOI] [PubMed] [Google Scholar]
- Preacher KJ, Hayes AF. INDIRECT macro (indirect.sps) 2011 Retrieved from http://www.afhayes.com/spss-sas-and-mplus-macros-and-code.html. [Google Scholar]
- Rao D, Kekwaletswe TC, Hosek S, Martinez J, Rodriguez F. Stigma and social barriers to medication adherence with urban children and adolescents living with HIV. AIDS Care. 2007;19(1):28–33. doi: 10.1080/09540120600652303. [DOI] [PubMed] [Google Scholar]
- Sherman BF, Bonanno GA, Wiener LS, Battles HB. When children tell their friends they have AIDS: Possible consequences for psychological well-being and disease progression. Psychosomatic Medicine. 2000;62:238–247. doi: 10.1097/00006842-200003000-00016. [DOI] [PubMed] [Google Scholar]
- Vreeman RC, Nyandiko WM, Ayaya SO, Walumbe EG, Marrero DG, Inui TS. The perceived impact of disclosure of pediatric HIV status on pediatric antiretroviral therapy adherence, child well-being, and social relationships in a resource-limited setting. AIDS Patient Care and STDS. 2010;24(10):639–649. doi: 10.1089/apc.2010.0079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wiener L, Battles H. Untangling the web: A close look at diagnosis disclosure among HIV-infected adolescents. Journal of Adolescent Health. 2006;38:307–309. doi: 10.1016/j.jadohealth.2005.03.024. [DOI] [PMC free article] [PubMed] [Google Scholar]