Abstract
PURPOSE
To examine race/ethnic specific patterns of association between neighborhood socioeconomic status (NSES) and a cumulative biological risk index in a nationally representative population.
METHODS
The study sample included 13,199 non-Hispanic white, non-Hispanic black and Mexican American men and women, ages 20 and older, who attended the National Health and Examination Survey examination 1988 and 1994. Neighborhoods were defined as census tracts and linked to US Census measures from 1990 and 2000, interpolated to the survey year; the NSES score included measures of income, education, poverty and unemployment and categorized into quintiles, with the highest indicating greater NSES. A summary biological risk score, allostatic load (AL; range 0-9), was created from nine biological indicators of elevated risk, including serum levels of C-reactive protein, albumin, glycated hemoglobin, total and HDL cholesterol, waist-to-hip ratio, systolic and diastolic blood pressure, and resting heart rate. Regression models stratified by race/ethnicity examined AL as a continuous and dichotomous (high (>=3) vs. low AL) outcome.
RESULTS
For both outcomes, we found strong inverse associations between NSES and AL for blacks, after adjusting for age, gender, US birth, urbanicity and individual SES. These associations were weaker and less consistent for Mexican Americans and whites.
CONCLUSIONS
Our results indicate that living in low NSES neighborhoods is most strongly associated with greater cumulative biological risk profiles in the black US population.
Keywords: Socioeconomic status, Residence characteristics, Race, Ethnicity
INTRODUCTION
Race, Neighborhood Socioeconomic Status and Health
Numerous studies have shown that living in low socioeconomic status (SES) neighborhoods is associated with negative health outcomes, including cardiovascular disease (1-3) and mortality (4) and that these effects are independent of individual SES. Less well examined, however, is the extent to which substantial racial/ethnic differences in levels of neighborhood deprivation intersect with observed neighborhood relationships to health, resulting in persisting questions regarding the extent of likely confounding effects of race (5,6). As several United States (US) population samples have shown, African American and Hispanic individuals live in predominantly deprived areas, while whites are more heavily represented in the highest socioeconomic areas (6-8). Race and neighborhood socioeconomic status (NSES) are, in fact, so intertwined that it is often difficult to tease apart their separate effects on health (5). For example, previous analyses of data from the National Health and Nutrition Examination Survey (NHANES), a nationally representative sample of the US population, reveal that there is limited overlap between white and minority populations with regard to NSES, with relatively few whites in the lowest SES neighborhoods and few blacks in the highest SES neighborhoods (6).
Given the vastly different NSES distributions in different race/ethnicity groups and the fact that the associations of individual SES with health outcomes are also different by race/ethnicity (9-11), it is important to examine NSES-health associations separately in the different race/ethnicity groups. The large, nationally representative NHANES population sample offers a unique opportunity to investigate the possibly different race/ethnic specific patterns of relationships between neighborhood characteristics and health as a result of the large sample, with over-sampling of both African Americans and Mexican Americans. (12).
Neighborhood socioeconomic status and cumulative biological risk profiles
Researchers have suggested that multiple pathways are involved in a neighborhood’s influence on negative health outcomes. These include fewer physical resources, such as recreational facilities (13,14) and limited access to healthy and affordable food (15-17). In addition, individuals living in low SES areas are less likely to obtain adequate and preventive health care (18). Moreover, exposure to violence and stressful life events are greater in more disadvantaged neighborhoods (19). These factors, individually and synergistically, operate through multiple biological pathways to negatively influence health in disadvantaged neighborhoods.
Psychosocial adversity is known to affect multiple regulatory physiological systems, and cumulative, multi-system indices of physiologic dysregulation, such as allostatic load (AL), are able to comprehensively capture psychosocial influences on biology, better than individual biomarkers (20). Previous research, including recent analyses of NHANES III data (21), has shown that lower individual SES is associated with greater AL, as indexed by a count of biological parameters (representing multiple biological systems) in high-risk zones (22). Similar findings have also been reported from the Normative Aging Study (23), the Wisconsin Longitudinal Study (24), and a national sample in Taiwan (25). To date, however, there have been no studies examining the association between AL and neighborhood SES. Prior work has focused on individual biological parameters, including BMI (7), cholesterol (7), blood pressure (7,26) and C-reactive protein (27). While useful in elucidating neighborhood relationships to various biological pathways, such analyses likely fail to capture the total scope of the biological impact of neighborhoods, and thus likely underestimate the impact of neighborhood characteristics on health risks.
Health risks accrue from changes in multiple biological systems; for instance, cardiovascular risk accrues from changes in blood pressure, blood glucose, lipids, body fat, and chronic inflammation (20). Hence, to assess the full scope of neighborhood influences on health risks, it is likely important to move beyond examination of neighborhood associations with individual biomarkers. A cumulative, multi-system index, reflecting multiple biological factors that contribute to health risks, may better capture the global biological impact of living in disadvantaged neighborhoods.
Objective
Our objective was to evaluate the association between AL and NSES separately in the 3 major race/ethnic groups.
METHODS
The study sample included participants in the NHANES III survey of a nationally representative sample of the US population with interview, clinical exam, and laboratory components (12), conducted between 1988 and 1994.
NHANES III data were geocoded based on home address and merged with select US Census variables. Data on neighborhood characteristics were derived from 1990 and 2000 Decennial Census data and interpolated to the corresponding years that participants were surveyed in NHANES III, assuming a constant rate of change in neighborhood conditions between decennial census years (with the exception of the1988-1989 survey that was directly linked to 1990 Census data). These census measures were linked to individual respondents in the NHANES III sample via census tract identifiers.
Selection Criteria
We initially included all NHANES participants, ages >=20 (n=18,825). From this adult sample, we excluded those whose addresses could not be geocoded directly to census tracts (n=2,626), and those who were pregnant and who did not attend the NHANES Mobile Examination Center (MEC) exam (n=2,232). In addition, we excluded those missing AL score, US birth, and education information (n=129). NSES categories were created from this sample (n=13,838). For the stratified analyses we excluded those whose race/ethnicity was coded as “other” (n=639), since this group represented a mixture of various other race and ethnic groups (as well as those classified as “unknown”). The total remaining sample size was 13,199 (65.8% of the adult sample).
Outcome
Data based on nine biomarkers were used to create an overall multi-system summary index of risk, to reflect the cumulative extent of physiological dysregulation across multiple systems, or allostatic load (20). Biomarkers included inflammatory, metabolic and cardiovascular indicators: serum levels of C-reactive protein, albumin, glycated hemoglobin, total cholesterol, and high-density lipoprotein (HDL) cholesterol, waist-to-hip ratio, systolic blood pressure, diastolic blood pressure, and resting heart rate. For each of the variables, a dichotomous indicator was assigned reflecting high and low risk (1 or 0, respectively), based on clinically accepted “high risk” criteria (see Table 1) (28-35). These indicator variables were then summed to create the total AL score. Additional details describing this score, including information on missing variables and imputations, have been recently published (21). This approach parallels the approach to other count-based indices, including assessments of the metabolic syndrome (28), and cumulative indices of health behaviors (36,37). In these analyses, AL was examined both as a continuous and a dichotomous outcome (AL>=3 vs. AL<3, corresponding to the top quartile vs. the rest).
Table 1.
Clinically-defined “high risk” criteria for biologic risk factors used to create Allostatic Load Index
| Variable | High Risk Clinical |
|---|---|
| Albumin (g/dL) | <3.8a |
| C-reactive protein (mg/dL) | >=0.3b |
| Waist to hip ratio | >0.90 for men; >0.85 for womenc |
| Total cholesterol (mg/dL) | >=240d |
| HDL cholesterol (mg/dL) | <40d |
| Glycated hemoglobin (%) | >=6.4e |
| Resting heart rate (bt/min) | >=90f |
| Systolic blood pressure (mm Hg) | >=140g |
| Diastolic blood pressure (mm Hg) | >=90g |
HDL, high-density lipoprotein
Reference #29
Reference #30
Reference #31
Reference #28
Reference #32,33
Reference #34
Reference #35
Neighborhood Socioeconomic Status
An index of neighborhood socioeconomic status was created based on US Census variables linked to census tracts in which participants resided. We utilized factor analysis to select 6 census variables for the NSES index, including: percentage of family households with children not headed only be a female, percentage of male population ages 16 and older that is employed, percentage of households that do not receive public assistance income, percentage of households with income higher than the poverty threshold, median household income, and percentage of population ages 25 and older with high school diploma or higher education. A summary measure of NSES was then constructed by summing z scores for the six variables, a higher score indicating higher SES, with scores ranging from −7.7 to 2.0.. Our study sample included 1,772 neighborhoods. Quintiles of this summary score were created based on its distribution in the study sample (including the “other” race group). We used NSES quintiles as primary predictor in all analyses, to allow for non-linear associations between NSES and AL. The quintile ranges and percent distributions can be found in Table 2.
Table 2.
Characteristics of the National Health and Nutrition Survey (NHANES), study sample by race/ethnicity, from 1988-1994a
| Variables | Total n=13,199 |
White n=5,225 |
Black n=4,005 |
Mexican American n=3,969 |
|---|---|---|---|---|
| % | % | % | % | |
| Age (median) | 41.0 | 42.0 | 38.0b | 34.0b |
|
Male
Neighborhood SES |
48.1 | 48.1 | 44.8b | 53.9b |
| Number of neighborhoods | 1,772 | 1,059 | 779 | 763 |
| Participants per neighborhood (mean; median) | 7.4; 6.0 | 4.9; 4.0 | 5.1; 3.0 | 5.2; 4.0 |
| Total Score | 0.24 | 0.34 | −0.88b | −0.57b |
| Quintiles of Score (Range) | ||||
| Q1 (<=−0.66) | 19.2 | 11.1 | 56.5b | 47.8b |
| Q2 (−0.66 to −0.02) | 19.7 | 19.8 | 17.8 | 21.6 |
| Q3 (−0.02 to 0.39) | 20.1 | 21.8 | 12.0b | 14.0b |
| Q4 (0.39 to 0.81) | 20.4 | 22.9 | 9.8b | 10.8b |
| Q5 (>0.81) | 20.6 | 24.4 | 3.8b | 5.8b |
| Components of Score | ||||
| Percent of family households with children not headed by female |
93.4 | 94.2 | 85.1b | 90.0b |
| Percentage of male population 16+ that is employed | 94.7 | 95.2 | 91.0b | 91.8b |
| Percentage of households that do not receive public assistance income |
95.3 | 96.0 | 88.6b | 89.8b |
| Percentage of households with income higher than poverty threshold |
91.6 | 92.6 | 80.1b | 85.4b |
| Median household income | 33,000 | 35,000 | 24,000b | 28,000b |
| Percentage of 25+ population with high school diploma or higher |
79.6 | 81.5 | 65.9b | 64.5b |
| Education | ||||
| Grade School | 9.8 | 7.0 | 12.7b | 41.1b |
| Some High School | 12.8 | 11.4 | 18.8b | 17.4b |
| Complete High School | 33.1 | 33.1 | 37.5b | 23.6b |
| Some College | 21.8 | 22.7 | 20.5 | 12.7b |
| >=Complete College | 22.6 | 25.8 | 10.5b | 5.2b |
| Poverty Income Ratio | ||||
| <1.0 | 12.0 | 7.6 | 28.3b | 35.5b |
| 1.0-1.99 | 19.8 | 17.3 | 29.4b | 32.6b |
| 2.0-2.99 | 20.1 | 20.6 | 19.0 | 15.3b |
| 3.0-3.99 | 18.3 | 20.2 | 11.4b | 8.1b |
| 4.0-4.99 | 11.5 | 12.9 | 6.0b | 3.5b |
| >=5.0 | 18.4 | 21.3 | 6.0b | 5.0b |
| Allostatic Summary Score | 1.6 (1; 0,2) | 1.5 (1; 0,2) | 1.6 (1; 0,3)c | 1.6 (1; 1,2) |
| Mean (Median; 25th percentile, 75th percentile) | ||||
| High vs. Low (AL>=3 vs. <3) | 23.1 | 22.8 | 25.4c | 21.9 |
Weighted by NHANES Mobile Examination Center (MEC) weight (WTPFEX6). Exclusions were: ages<20, pregnant, those who did not attend the MEC exam, and whose addresses could not be geocoded, missing the neighborhood score and those missing US birth information, PIR and education.
p-value<0.01 compared to whites
p-value<0.05 compared to whites
Individual Socioeconomic Status
Individual level SES variables included education and income. Education was defined in terms of highest level completed, including grade school, some high school, complete high school, some college, complete college or more. Income was measured using the poverty income ratio (PIR), a ratio of household income to the household poverty level determined by area of residence and household size. (38).
PIR values were classified into five categories (<1, 1-1.99, 2-2.99, 3-3.99, 4-4.99 and 5+). About 2,150 observations were missing a PIR value. The PIR category for these observations was imputed using a single imputation method (39) based on age, gender, race/ethnicity, US birth, education, marital status, employment status, and neighborhood characteristics: median household income, percent non-Hispanic White, percent foreign born, percent renter-occupied housing units, and percent urban population.
Analysis
All analyses were stratified by race/ethnicity, using as categories: non-Hispanic whites, non-Hispanic blacks and Mexican Americans.
Mixed effects models were used to examine differences in the continuous AL score by quintiles of neighborhood SES score. We initially ran empty models to determine intraclass correlation coefficients (ICC); the ICC was 0.15 for neighborhoods, 0.01 for counties and 0.01 for the NHANES survey design PSU/strata combinations. Random intercepts for census counties and tracts were subsequently included in the mixed effects models, with the understanding that ICCs were low for both NHANES PSU and counties, and that most NHANES PSU are indeed counties (12). The models were initially adjusted for age, age squared, gender, US birth, urban/rural location, and then additionally adjusted for individual SES (education and PIR). A qu-adratic term for age was included based on previous analyses of NHANES data that determined this term the best fit when examining the relationship between age and allostatic load (40). Urban/rural status was adjusted for considering previous work that has shown NSES-health effects to be stronger in urban settings (41). Generalized estimating equation (GEE) models were used to model the log odds of high AL (AL >=3) by quintiles of neighborhood SES score. In sensitivity analyses, we also considered alternate definitions of high AL, defined as >=2 and >=4. We used an exchangeable correlation structure to account for within-neighborhood correlation.
All analyses were weighted using NHANES MEC weights, and used robust (empirical) error variance estimation to account for heteroskedasticity. Analyses were performed at the secure Research Data Center at the National Center for Health Statistics in Hyattsville, MD, and were conducted using SAS version 8.2.
RESULTS
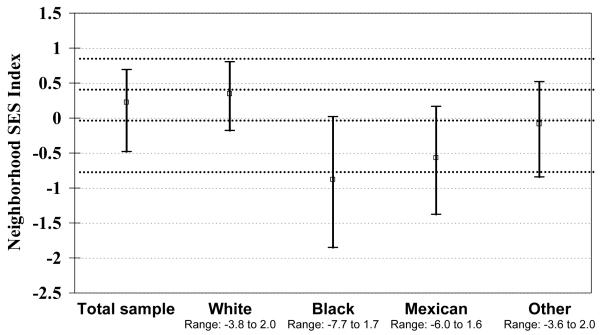
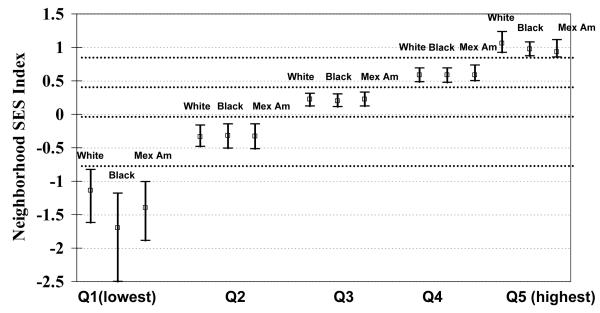
Figure 1a illustrates the starkly differing neighborhood SES distributions by race/ethnicity, with the most striking differences seen in the lower range of SES scores for whites versus blacks and Mexican Americans. Indeed, the median NSES score for whites bordered the 2nd NSES quintile (marked by the dashed lines) while the median for the black and Mexican American populations corresponded to the lowest two NSES quintiles. Figure 1b provides further details regarding these racial/ethnic differences, showing the race/ethnic-specific distribution of NSES scores within each NSES quintile. As shown, the greatest differences are evident in the bottom quintile (Q1), where the distribution of neighborhoods in which blacks live reflect a much lower range of NSES scores than for either Mexican Americans or whites.
Figure 1a.
“Interquartile Ranges of Neighborhood Socioeconomic Status Index by Race/Ethnic Group: NHANES 1988-1994”
aDashed lines indicate quintile cutpoints.
Figure 1b.
“Interquartile Ranges of Neighborhood Socioeconomic Status Index by Neighborhood SES Quintiles and Race/Ethnic Group: NHANES 1988-1994
aDashed lines indicate quintile cutpoints.
Table 2 presents the weighted distributions for other major characteristics of the study sample by race/ethnicity. The white participants were slightly older, more educated, had higher income, and higher NSES scores overall. Consistent with this latter finding, whites had higher scores for each of the neighborhood SES characteristics. These differences were statistically significant. Consistent with the graphical displays in Figures 1a & b, Table 2 shows that only 11.1% of whites lived in the lowest NSES quintile, compared to 56.5% of blacks and 47.8% of Mexican Americans. By contrast, 24.4% of whites lived in neighborhoods in the highest NSES quintile whereas only 3.8% and 5.8% of blacks and Mexican Americans, respectively, lived in these types of neighborhoods. Neighborhoods where black participants lived had lower total NSES scores than those of Mexican Americans, although blacks had slightly higher individual-level education and income. Differences in AL between black/Mexican Americans and whites were not statistically significant. Those excluded from the analyses for reasons described in the Methods, had lower average NSES score, were worse off with regard to education and PIR, and had slightly higher AL scores.
For each of the race/ethnic strata, analyses revealed statistically significant associations between average AL scores and NSES, with increasing average AL score associated with decreasing NSES quintiles, after adjustment for age, gender, and US birth (see Table 3, Model 1). After additional adjustment for individual-level SES (i.e., education and PIR; Model 2) and urban location, these trends remained significant for blacks and Mexican Americans. Blacks had the largest difference in AL between neighborhoods at the lowest and highest NSES quintiles. A slightly smaller difference was apparent between the lowest and highest NSES quintiles for Mexican Americans and differences were much smaller and not significant for whites.
Table 3.
Adjusted Differences of Allostatic Load by Quintiles of Neighborhood Socioeconomic Status in the United States Population, 1988-1994.
| White | Model 1: age, age2, gender US birth |
Model 2: plus urban location,
education, PIR |
||
|---|---|---|---|---|
| β | 95% CI | β | 95% CI | |
| Q1 (Low) | 0.301 | 0.154, 0.447 | 0.114 | −0.055, 0.283 |
| Q2 | 0.170 | 0.045, 0.294 | −0.004 | −0.146, 0.139 |
| Q3 | 0.194 | 0.083, 0.305 | 0.077 | −0.043, 0.197 |
| Q4 | 0.0658 | −0.030, 0.162 | 0.005 | −0.093, 0.103 |
| Q5 (High) | Reference | p trend: <0.0001 | Reference | p trend: 0.3 |
| Black | ||||
| Q1 (Low) | 0.483 | 0.269, 0.697 | 0.400 | 0.189, 0.611 |
| Q2 | 0.313 | 0.081, 0.545 | 0.256 | 0.040, 0.473 |
| Q3 | 0.210 | −0.061, 0.480 | 0.168 | −0.097, 0.433 |
| Q4 | 0.383 | 0.079, 0.687 | 0.355 | 0.060, 0.650 |
| Q5 (High) | Reference | p trend: 0.0001 | Reference | p trend: 0.005 |
| Mexican Am | ||||
| Q1 (Low) | 0.400 | 0.146, 0.654 | 0.302 | 0.051, 0.552 |
| Q2 | 0.311 | 0.047, 0.575 | 0.239 | −0.016, 0.493 |
| Q3 | 0.358 | 0.094, 0.621 | 0.286 | 0.037, 0.536 |
| Q4 | 0.201 | −0.103, 0.505 | 0.159 | −0.128, 0.446 |
| Q5 (High) | Reference | p trend: 0.0001 | Reference | p trend: 0.01 |
CI, confidence interval; PIR, poverty to income ratio; US, United States.
Consistent with these findings, examination of the relative odds of having a “high AL”, defined as a score of 3 or more, revealed that the strongest trend across NSES quintiles was for blacks (p-trend=0.02 in fully adjusted model; see Table 4). As shown in Table 4, blacks living in the lowest NSES neighborhoods had over twice the odds of a high AL score as compared with those living in the highest NSES quintile (OR: 2.2, 95%CI: 1.1, 4.1). Non-significant trends were seen for both whites and Mexican Americans. The odds of high AL were 30% higher for whites in the lowest NSES quintile compared to the highest (OR: 1.4, 95% CI: 1.0, 2.0), and 70% higher for Mexican Americans, though that measure was not statistically significant (OR: 1.7, 95% CI: 0.8, 3.3).
Table 4.
Adjusted Odds Ratios and 95% Confidence Intervals for High Allostatic Load (3+) by Quintiles of Neighborhood Socioeconomic Status in the United States Population, 1988-1994.
| White |
Fully Adjusted Model
a
High AL (3+) |
|
|---|---|---|
| OR | 95% CI | |
| Q1 (Low) | 1.3 | 0.9, 1.8 |
| Q2 | 0.8 | 0.6, 1.1 |
| Q3 | 1.1 | 0.8, 1.5 |
| Q4 | 1.0 | 0.7, 1.3 |
| Q5 (High) | Reference p trend: 0.7 |
Reference |
| Black | ||
| Q1 (Low) | 2.2 | 1.1, 4.1 |
| Q2 | 2.1 | 1.1, 4.1 |
| Q3 | 1.7 | 0.8, 3.4 |
| Q4 | 1.9 | 0.9, 3.7 |
| Q5 (High) | Reference p trend: 0.02 |
Reference |
| Mexican Am | ||
| Q1 (Low) | 1.7 | 0.8, 3.3 |
| Q2 | 1.6 | 0.8, 3.2 |
| Q3 | 1.8 | 0.9, 3.6 |
| Q4 | 1.2 | 0.6, 2.7 |
| Q5 (High) | Reference p trend: 0.2 |
Reference |
AL, allostatic load; CI, confidence interval; OR, odds ratio.
Fully adjusted model includes adjustment for age, age2, gender, US birth, urban location, education, and poverty income ratio.
Sensitivity analyses of the main results using alternative definitions of “high” AL (i.e., AL>=4 and AL>=2) revealed parallel findings for the former (i.e., AL>=4) with a statistically significant trend for blacks, and similar, though weaker, trends for the latter (i.e., AL>=2) (data not shown). Fully adjusted models in tables 3 and 4 were also re-fit considering only original PIR values (without any imputations) and the results were similar to the main analyses (data not shown). Parallel sets of sub-analyses for each of the 3 major subscales comprising the AL index (inflammation, metabolism and cardiovascular risks) revealed similar patterns in each case to those observed for the overall index, supporting the argument that multiple systems are similarly, negatively impacted by residence in a lower SES neighborhood (data not shown).
To further explore the possibility that NSES may impact AL differently, depending on whether you live in an urban vs. rural area, we also ran exploratory analyses, testing for potential interactions of urban/rural status and NSES. Only one significant interaction was found (p=0.04) for Mexican Americans, when considering risk of high AL (>=3 vs. <3). Models stratified by urban status for Mexican Americans revealed a significant negative association only in urban neighborhoods (OR for Q1 [lowest NSES] vs. Q5 [highest NSES] was 2.1, 95% CI: 1.0-4.3, and p-value for trend across NSES levels=0.02); there was no statistically significant risk and no apparent gradient for Mexican Americans in rural areas (p-value for trend=0.2).
DISCUSSION
These results show that those living in neighborhoods in the lowest NSES quintiles had higher levels of AL, compared to those living in neighborhoods at the highest NSES quintile, after adjusting for age, gender, US birth, urban location, education and income. This pattern was found in all 3 race/ethnic groups, although it was strongest and statistically significant only for the black population. This pattern of results was found to be robust across alternative measures of AL. For Mexican Americans this trend was statistically significant only in urban locations.
The pathways that might link low NSES to higher AL include factors that are associated with deprived neighborhoods that have also been shown associated with higher health risks represented in the AL index, including fewer physical activity resources, such as recreational facilities (13,14), limited access to healthy and affordable food (15-17), inadequate preventive health care (18) and exposure to violence and stressful life events (19).
The statistically significant risks and trend for blacks contrasts with previous studies that found only weak NSES-health associations in that population (1,4,42,43). Those studies, however, had fewer African Americans, and only included people from a few select counties in the US. Consistent with our findings, Cubbin et al examined the role of NSES using the same data (7) and found that it is associated inversely with diabetes and body mass index in black women (but not in white or Mexican American women) and with non-HDL cholesterol in black men (but not in white or Mexican American men). By using a multi-system biological index of risk, we were able to demonstrate NSES effects on cumulative biological dysregulation in all race/ethnic groups, with the largest and most consistent effects among blacks.
There are several possible reasons why AL scores may be most elevated in the lowest NSES quintile among blacks and less so for Mexican Americans and even less for whites. Although the quintiles were defined identically for all three race/ethnic groups, the characteristics of the actual neighborhoods in which the different groups live are quite different, with the starkest differences seen among those living in the lowest SES neighborhoods. Indeed, as Figure 1b clearly illustrates, within the lowest NSES quintile, the range of NSES scores is lower for blacks than for either Mexican Americans or whites. Thus, the significantly worse AL scores seen for blacks living in the lowest NSES quintile neighborhoods may reflect the fact that at least a portion of those blacks are living in neighborhoods of notably lower SES than those of whites in the lowest NSES quintile. Likewise, Mexican Americans in the lowest NSES quintile live in neighborhoods of lower SES compared to whites, though the SES range of their neighborhoods does not go as low as that of the black population. Thus, the greater differentials in AL by NSES seen for blacks and Mexican Americans may reflect the fact that the most deprived neighborhoods in which blacks and Mexican Americans live are worse off than the lowest SES neighborhoods for whites. The stronger association between NSES and AL for Mexican Americans living in urban areas was not predicted and requires future replication and elucidation of reasons for such effects in Mexican Americans versus other race/ethnic groups. Possible explanations that require further investigation include more detailed evaluation of the types of urban vs. rural neighborhoods inhabited by Mexican Americans versus other race/ethnic groups and whether this results in greater differentials in relevant neighborhood characteristics in the urban vs. rural settings, including availability of various resources such as food choices or liquor.
Strengths and Limitations
The strengths of this study include a study sample that is representative of the general US population, racially and ethnically diverse, as well as large enough to explore NSES-health relationships separately within the major race/ethnic groups. Moreover, the range of biological data allowed us to create a summary index of cumulative biological risk that captures information about multiple major biological systems.
A significant limitation of this study is the cross-sectional nature of the data. The biological and demographic data were only available at one point in time. We were thus unable to establish with certainty the temporal association between place of residence and onset of biological risk. We were also not able to assess contextual socioeconomic factors (substandard housing, lack of health clinics, lack of recreational facilities etc); the NSES measure we used was entirely compositional (i.e., based on SES of individuals in the neighborhood). While many neighborhood studies rely on such compositional measures (1,4,8,42,43), future studies should consider contextual measures that would more specifically describe a neighborhood’s SES, independent of its residents’ individual means.
Conclusions and Policy Implications
National data indicate strong associations for blacks between living in low NSES neighborhoods and greater cumulative biological risk profiles. These data suggest that such associations are apparent, although weaker, for Mexican Americans and even weaker for whites. Consistent with this finding, the low SES neighborhoods where blacks live are characterized by worse socioeconomic conditions than the low SES neighborhoods of whites and Mexican Americans. These findings confirm previous studies (7,44) and highlight the degree to which economic segregation impacts the health risks of those living in the lowest NSES neighborhoods. Clearly, future policy and research should direct its attention to these economic and racial disparities in light of the growing evidence of their fundamental impacts on our public health.
ACKNOWLEDGMENTS
This work was supported by grants from the national Institute on Aging (R01 AG023347, and P30-AG17265) and the National Institute on Environmental Health Sciences (P50 ES012383) We would like to thank the staff at the National Center for Health Statistics (NCHS) as well as the Research Data Center (RDC). Data from this study were presented in part at the Annual Meeting of the Society for Epidemiologic Research, Boston MA, June 2007.
ABBREVIATIONS
- AL
Allostatic load
- CI
confidence interval
- GEE
generalized estimating equation
- HDL
high-density lipoprotein
- MEC
mobile examination center
- NHANES
National Health and Nutrition Examination Survey
- NSES
neighborhood socioeconomic status
- OR
odds ratio
- PIR
poverty income ratio
- SES
socioeconomic status
- US
United States
REFERENCES
- 1.Diez-Roux AV, Merkin S Stein, Arnett D, Chambless L, Massing M, Nieto FJ, et al. Neighborhood of residence and incidence of coronary heart disease. N Eng J Med. 2001;345:99–10. doi: 10.1056/NEJM200107123450205. [DOI] [PubMed] [Google Scholar]
- 2.Winkelby M, Sundquist K, Cubbin C. Inequities in CHD incidence and case fatality by neighborhood deprivation. American Journal of Preventive Medicine. 2007;32(2):97–106. doi: 10.1016/j.amepre.2006.10.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Chaix B, Rosvall M, Merlo J. Recent increase of neighborhood socioeconomic effects on ischemic heart disease mortality: a multilevel survival analysis of two large Swedish cohorts. Am J Epidemiol. 2007;165:22–26. doi: 10.1093/aje/kwj322. [DOI] [PubMed] [Google Scholar]
- 4.Roux AV Diez, Borrell LN, Haan M, Jackson SA, Schultz R. Neighborhood environments and mortality in an elderly cohort: results from the cardiovascular health study. J Epidemiol Community Health. 2004 Nov;58(11):917–23. doi: 10.1136/jech.2003.019596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.LaVeist TA. Disentangling race and socioeconomic status: A key to understanding health inequalities. Journal of Urban Health. 2005;82(2):iii26–iii34. doi: 10.1093/jurban/jti061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hadden WC, Maury BB. The limits of contextual or multi-level analysis of health surveys. 1999 Federal Committee on Statistical Methodology Research Conference; Statistical Policy Office. Office of Management and Budget; 1999. Statistical Policy Working Paper 30. http://www.fcsm.gov/99papers/hadden.pdf. [Google Scholar]
- 7.Cubbin C, Hadden WC, Winkleby MA. Neighborhood context and cardiovascular disease risk factors: the contribution of material deprivation. Ethn Dis. 2001 Fall;11(4):687–700. [PubMed] [Google Scholar]
- 8.Roux AV Diez, Kiefe CI, Jacobs DR, Jr, Haan M, Jackson SA, Nieto FJ, et al. Area characteristics and individual-level socioeconomic position indicators in three population-based epidemiologic studies. Ann Epidemiol. 2001;11:395–405. doi: 10.1016/s1047-2797(01)00221-6. [DOI] [PubMed] [Google Scholar]
- 9.Karlamangla A, Singer BS, Williams DR, Schwartz J, Matthews K, Kiefe CI, et al. Impact of socio-economic status on longitudinal accumulation of cardiovascular risk in young adults: The CARDIA Study. Social Science & Medicine. 2005;60:999–1015. doi: 10.1016/j.socscimed.2004.06.056. [DOI] [PubMed] [Google Scholar]
- 10.Watkins LO, Neaton JD, Kuller LH. Racial differences in high density lipoprotein cholesterol and coronary heart disease incidence in the usual-care group of the multiple risk factor intervention trial. The American Journal of Cardiology. 1986;57:538–545. doi: 10.1016/0002-9149(86)90831-3. [DOI] [PubMed] [Google Scholar]
- 11.Kraus JF, Borhani NO, Franti CE. Socioeconomic status, ethnicity, and risk of coronary heart disease. American Journal of Epidemiology. 1980;111(4):407–414. doi: 10.1093/oxfordjournals.aje.a112915. [DOI] [PubMed] [Google Scholar]
- 12.National Center for Health Statistics Plan and operation of the Third National Health and Nutrition Examination Survey, 1988-94. Series 1: programs and collection procedures. Vital and Health Statistics. Series 1, Programs and Collection Procedures. 1994;(32):1–407. [PubMed] [Google Scholar]
- 13.Gordon-Larsen P, Nelson MC, Page P, Popkin BM. Inequality in the built environment underlies key health disparities in physical activity and obesity. Pediatrics. 2006;117:417–424. doi: 10.1542/peds.2005-0058. [DOI] [PubMed] [Google Scholar]
- 14.Powell LM, Slater S, Chaloupka FJ, Harper D. Availability of physical activity-related facilities and neighborhood demographic and socioeconomic characteristics: A national study. American Journal of Public Health. 2006;96(9):1676–1680. doi: 10.2105/AJPH.2005.065573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Horowitz CR, Colson KA, Hebert PL, Lancaster K. Barriers to buying healthy foods for people with diabetes: evidence of environmental disparities. AJPH. 2004;94(9):1549–1554. doi: 10.2105/ajph.94.9.1549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Moore LV, Roux AV Diez. Associations of neighborhood characteristics with the location and type of food stores. American Journal of Public Health. 2006;96:325–331. doi: 10.2105/AJPH.2004.058040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Powell LM, Slater S, Mirtcheva D, Bao Y, Chaloupka FJ. Food store availability and neighborhood characteristics in the United States. Preventive Medicine. 2007 Mar;44(3):189–95. doi: 10.1016/j.ypmed.2006.08.008. [DOI] [PubMed] [Google Scholar]
- 18.Pappas G, Hadden WC, Kozak LJ, Fisher GF. Potentially avoidable hospitalizations: inequalities in rates between US socioeconomic groups. American Journal of Public Health. 1997;87(5):811–816. doi: 10.2105/ajph.87.5.811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Attar BK, Guerra NG, Tolan PH. Neighborhood disadvantage, stressful life events, and adjustment in urban elementary-school children. Journal of Clinical Child Psychiatry. 1994;23:391–400. [Google Scholar]
- 20.McEwen BS, Stellar E. Stress and the individual. Mechanisms leading to disease. Archives of Internal Medicine. 1993;153(18):2093–2101. [PubMed] [Google Scholar]
- 21.Seeman TE, Merkin SS, Crimmins E, Koretz B, Karlamangla A. Education, Income and Ethnic Differences in Cumulative Biological Risk Profiles in a National Sample of US Adults: NHANES III (1988-1994) Social Science and Medicine. 2008 Jan;66(1):72–87. doi: 10.1016/j.socscimed.2007.08.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Seeman TE, Crimmins E, Huang MH, Singer B, Bucur A, Gruenewald T, et al. Cumulative biological risk and socio-economic differences in mortality: MacArthur studies of successful aging. Social Science & Medicine. 2004;58(10):1985–1997. doi: 10.1016/S0277-9536(03)00402-7. [DOI] [PubMed] [Google Scholar]
- 23.Kubzansky L, Kawachi I, Sparrow D. Socioeconomic status and risk factor clustering in the normative aging study: Any help from the concept of allostatic load? Annals of Behavioral Medicine. 1999;21(4):330–338. doi: 10.1007/BF02895966. [DOI] [PubMed] [Google Scholar]
- 24.Singer B, Ryff CD. Hierarchies of life histories and associated health risks. Ann N Y Acad Sci. 1999;896:96–115. doi: 10.1111/j.1749-6632.1999.tb08108.x. [DOI] [PubMed] [Google Scholar]
- 25.Hu P, Wagle N, Goldman N, Weinstein M, Seeman TE. The associations between socioeconomic status, allostatic load and measures of health in older Taiwanese persons: Taiwan social environment and biomarkers of aging study. J Biosoc Sci. 2007 Jul;39(4):545–56. doi: 10.1017/S0021932006001556. Epub 2006 Oct 20. [DOI] [PubMed] [Google Scholar]
- 26.Roux AV Diez, Chambless L, Merkin SS, Arnett D, Eigenbrodt M, Nieto FJ, Szklo M, Sorlie P. Socioeconomic disadvantage and change in blood pressure associated with aging. Circulation. 2002 Aug 6;106(6):703–10. doi: 10.1161/01.cir.0000025402.84600.cd. [DOI] [PubMed] [Google Scholar]
- 27.Petersen KL, Marsland AL, Flory J, Votruba-Drzal E, Muldoon MF, Manuck SB. Community socioeconomic status is associated with circulating Interleukin-6 and C-reactive protein. Psychosomatic Medicine. 2008;70:646–652. doi: 10.1097/PSY.0b013e31817b8ee4. [DOI] [PubMed] [Google Scholar]
- 28.National Cholesterol Education Program (NCEP) Expert Panel Report of the National Cholesterol Education Program Expert Panel on Detection, Evaluation and Treatment of High Blood Cholesterol in Adults. JAMA. 2001;285(19):2486–2497. doi: 10.1001/jama.285.19.2486. 2001. [DOI] [PubMed] [Google Scholar]
- 29.Visser M, Kritchevsky SB, Newman AB, Goodpaster BH, Tylavsky FA, Nevitt MC, et al. Lower serum albumin concentration and change in muscle mass: The Health, Aging and Body Composition Study. The American Journal of Clinical Nutrition. 2005;82(3):531–537. doi: 10.1093/ajcn.82.3.531. [DOI] [PubMed] [Google Scholar]
- 30.Ridker PM. C-Reactive protein: A simple test to help predict risk of heart attack and stroke. Circulation. 2003;108:81–85. doi: 10.1161/01.CIR.0000093381.57779.67. [DOI] [PubMed] [Google Scholar]
- 31.Alberti KG, Zimmet PZ. Definition, diagnosis and classification of diabetes mellitus and its complications. Part I: Diagnosis and classification of diabetes mellitus provisional report of a WHO consultation. Diabetic Medicine. 1998;15:539–553. doi: 10.1002/(SICI)1096-9136(199807)15:7<539::AID-DIA668>3.0.CO;2-S. [DOI] [PubMed] [Google Scholar]
- 32.Golden S, Boulware LE, Berkenblit G, Brancati F, Chander G, Marinopoulos S, et al. Use of glycated hemoglobin and microalbuminuria in the monitoring of diabetes mellitus. Evidence Report/Technology Assessment. 2003;84:1–6. [PMC free article] [PubMed] [Google Scholar]
- 33.Osei K, Rhinesmith S, Gaillard T, Schuster D. Is glycosylated hemoglobin A1c a surrogate for metabolic syndrome in nondiabetic, first-degree relatives of African-American patients with type 2 diabetes? The Journal of Clinical Endocrinology and Metabolism. 2003;88(10):4596–4601. doi: 10.1210/jc.2003-030686. [DOI] [PubMed] [Google Scholar]
- 34.Seccareccia F, Pannozzo F, Dima F, Minoprio A, Menditto A, Lo Noce C, et al. Heart rate as a predictor of mortality: the MATISS project. American Journal of Public Health. 2001;91(8):1258–1263. doi: 10.2105/ajph.91.8.1258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL, Jr., et al. Seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. Hypertension. 2003;42(6):1206–1252. doi: 10.1161/01.HYP.0000107251.49515.c2. [DOI] [PubMed] [Google Scholar]
- 36.Khaw KT, Wareham N, Bingham S, Welch A, Luben R, Day N. Combined impact of health behaviours and mortality in men and women: the EPIC-Norfolk prospective population study. PLoS Med. 2008 Jan 8;5(1):e12. doi: 10.1371/journal.pmed.0050012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Berkman LF, Breslow F, Wingard D. Health practices and mortality risk. In: Berkman LF, Breslow L, editors. Health and Ways of Living. Oxford University Press; New York, NY: 1983. pp. 61–112. [Google Scholar]
- 38.National Center for Health Statistics (CHS) [Accessed, 11-12-06];National Health and Nutrition Examination Survey III: Household Adult Data File Documentation. 1996 http://www.cdc.gov/nchs/data/nhanes/nhanes3/ADULT-acc.pdf.
- 39.Donders AJT, Van der Heijden GJMG, Stijnen T, Moons KGM. Review: A gentle introduction to imputation of missing values. Journal of Clinical Epidemiology. 2006;59:1087–1091. doi: 10.1016/j.jclinepi.2006.01.014. [DOI] [PubMed] [Google Scholar]
- 40.Crimmins EM, Johnston M, Hayward M, Seeman T. Age differences in allostatic load: an index of physiological dysregulation. Experimental Gerontology. 2003;38(7):731–734. doi: 10.1016/s0531-5565(03)00099-8. [DOI] [PubMed] [Google Scholar]
- 41.Chaix B, Rosvall M, Merlo J. Assessment of the magnitude of geographical variations and socioeconomic contextual effects on ischaemic heart disease mortality: a multilevel survival analysis of a large Swedish cohort. J Epidemiol Community Health. 2007;62:349–355. doi: 10.1136/jech.2006.047597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Merkin SS, Coresh J, Roux AV, Taylor HA, Powe NR. Area socioeconomic status and progressive CKD: the Atherosclerosis Risk in Communities (ARIC) Study. Am J Kidney Dis. 2005 Aug;46(2):203–13. doi: 10.1053/j.ajkd.2005.04.033. [DOI] [PubMed] [Google Scholar]
- 43.Merkin SS, Roux AV Diez, Coresh J, Fried LF, Jackson SA, Powe NR. Individual and neighborhood socioeconomic status and progressive chronic kidney disease in an elderly population: The Cardiovascular Health Study. Social Science and Medicine. 2007;65:809–821. doi: 10.1016/j.socscimed.2007.04.011. [DOI] [PubMed] [Google Scholar]
- 44.Winkelby MA, Cubbin C. Influence of individual and neighborhood socioeconomic status on mortality among black, Mexican-American, and white women and men in the United States. J Epidemiol Community Health. 2003;57:444–452. doi: 10.1136/jech.57.6.444. [DOI] [PMC free article] [PubMed] [Google Scholar]